Introduction
Hidradenitis suppurativa (HS) is a chronic and relapsing inflammatory follicular disorder of the intertriginous areas.1 It is one of the most reported diseases associated with Crohn's disease (CD). Effective symptomatic management remains a therapeutic challenge for HS or CD. Acute symptomatic management for HS is limited to intralesional steroids and systemic steroids as rescue therapies.2 Herein, we report a unique case of aggressive/recalcitrant HS in the setting of CD rapidly stabilized following tumescent triamcinolone infiltration (TTI).
Case report
A 16-year-old African American female with a history of recalcitrant CD and HS, Hurley stage III, was admitted for a recurrent CD flare, severe HS flare, and headache.
Her history was notable for CD at the age of 8, which became aggressive such that she required a partial loop ileostomy with colostomy. Previous treatment failures for her CD included intravenous immunoglobulin, adalimumab, methotrexate, vedolizumab, ustekinumab, tacrolimus, 6-mercaptopurine, and infliximab. On admission, her CD regimen included methylprednisolone 10 mg and metronidazole 250 mg 3 times a day. Acute pain control for her headache and HS/CD was achieved with oxycodone-acetaminophen 5 mg-325 mg every 6 hours.
Her CD was complicated by the development of mild HS of her left axilla 4 years later, which has since progressed to involve both axillae. Prior treatments for her HS included hibiclens, clindamycin gel, metronidazole cream, doxycycline, adalimumab, and intralesional triamcinolone.
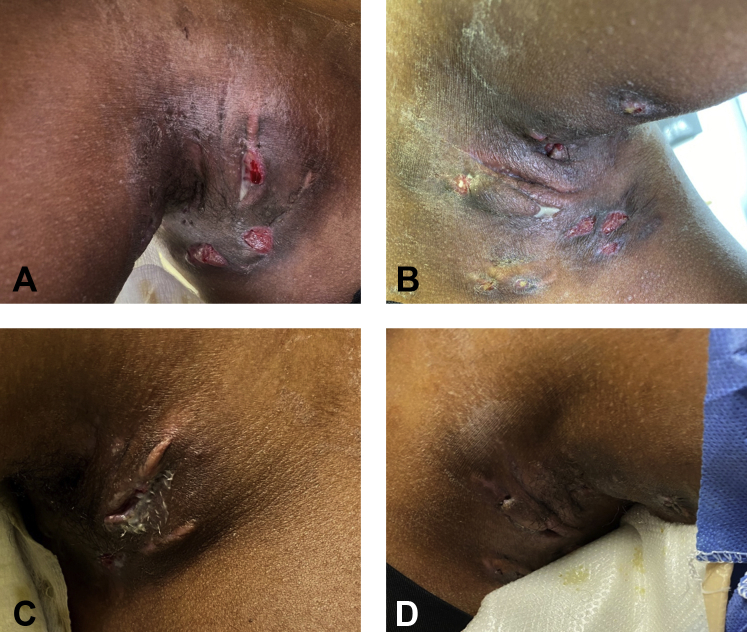
Physical examination revealed bilateral axillae with tender deep-seated erythematous nodules and draining sinuses (Fig 1, A and B), with limited range of motion of her shoulders to a few degrees. There was significant edema in her mons pubis and bilateral labia majora and labia minora, with linear fissures of her inguinal folds.
Fig 1.
Clinical images of the (A) right and (B) left axilla with tender, deep-seated erythematous nodules and hemorrhagic and purulent draining sinuses. Clinical images of the (C) right and (D) left axilla significantly improved, now non-tender, with no erythema, and minimal drainage 48 hours after TTI. TTI, Tumescent triamcinolone infiltration.
Due to the severity of her flare and degree of discomfort resulting in transient functional impairment of her shoulders, we sought a safe and acute alternative to decrease the inflammation for rapid relief. The addition of triamcinolone to tumescent anesthetic solution is well-documented as very effective in preventing inflammation and swelling.3 Tumescent anesthesia with triamcinolone solution was prepared with 250 mL of saline, 25 mL of 1% lidocaine with epinephrine, and 120 mg of triamcinolone in the form of a 40 mg/mL solution mixed into the saline bag. After conscious sedation performed using pediatric anesthesia, both axillae, and the inguinal folds, mons pubis, and labia majora were draped in a sterile manner. Several insertion points were marked at each lesional area and anesthetized with a total of 6 mL of 1% lidocaine with epinephrine to minimize the needle insertion pain. TTI was then performed using a 60-mL syringe with an 18-gauge needle at the aforementioned areas, with 60 mL infiltrated at each axilla and 158 mL infiltrated at the mons pubis, inguinal folds, and labia majora collectively. She tolerated the procedure with mild discomfort and agitation during injection, which she did not recall after the sedation wore off.
At the time of the TTI procedure, given the frequency of her flares and recalcitrance to prior treatments, multiple punch biopsies were performed at both axillae and the mons pubis and bilateral inguinal folds to delineate whether there was a clinical overlap between HS and CD. Biopsy of her left inguinal fold was consistent with CD, with no evidence of HS. Meanwhile, biopsies of the axillae supported HS, with no evidence of CD. The periodic acid–Schiff, Gram, acid-fast bacilli, and Grocott-Gomori methenamine silver stains were negative for microorganisms in all samples.
She experienced significant improvement of her HS in terms of edema, pain, and drainage within 48 hours of the procedure (Fig 1, C and D), which has sustained for about 7 months. She also experienced significant improvement of her CD, but that lasted about 4 weeks. Her current HS regimen includes hibiclens wash and topical clindamycin gel.
Discussion
Here, we describe the effective symptomatic management of HS in the setting of metastatic CD following TTI. Our patient presented a therapeutic challenge for several reasons. First, she was in a constant highly inflammatory state given her concomitant aggressive CD, potentially exacerbating her HS. Moreover, she developed toxicity to many recommended systemic medications for effective disease control of her HS and CD.4 She failed to develop therapeutic levels of several biologics after several months of treatment. Despite being on chronic systemic steroids for the management of her CD, she continued to experience frequent flares of her HS and CD, requiring several hospital admissions.
TTI was an excellent alternative that facilitated rapid improvement of patient-reported outcomes (pain and quality of life) and clinically relevant HS stabilization for a period of 7 months. Importantly, she was able to resume her activities of daily living, such as combing her hair and returning to school. Of note, she also experienced improvement of her CD but that response was short-lived. This underscores the difference in pathogenesis between HS and CD. She remains on 10 mg methylprednisolone 3 times a day for her CD, managed by her gastroenterologist.
TTI has the advantage of a larger volume being deposited precisely into scar tissue, deep dermis, and superficial fascia with less needle sticks and lengthens the period of disease stabilization, thereby minimizing any unwanted metabolic effects of long-term steroid use. The corticosteroid dose of 120 mg was arbitrarily chosen based on the extent of disease activity but may be titrated as on a case-by-case basis. We hypothesize that TTI produced a localized reservoir of triamcinolone in the superficial fascia and dermis, allowing for slow diffusion across the fibrous tissue and reducing peribulbar and intrafollicular inflammation. This is in contrast to intralesional triamcinolone injection, in which the small volume of triamcinolone remains localized to the intrafollicular space reducing only the inflammation within and not the perifollicular inflammation, which forms a significant component in the late stages of the disease. TTI is an easily performed alternative for patients with recalcitrant/aggressive HS in need of acute symptomatic management and disease stabilization. Based on this case and subsequent patients treated, sedation to control injection discomfort should be used when available; alternatively, a sublingual dose of a benzodiazepine might be used.5 Additional studies are needed to further standardize the protocol and characterize treatment efficacy.
Acknowledgments
We are grateful to Simon S. Rabinowitz, MD, PhD, for his contribution to the management of this case.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
References
- 1.Saunte D.M.L., Jemec G.B.E. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318(20):2019–2032. doi: 10.1001/jama.2017.16691. [DOI] [PubMed] [Google Scholar]
- 2.van der Zee H.H., Gulliver W.P. Medical treatments of hidradenitis suppurativa: more options, less evidence. Dermatol Clin. 2016;34(1):91–96. doi: 10.1016/j.det.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 3.Gholamali A., Sepideh P., Susan E. Hair transplantation: preventing post-operative oedema. J Cutan Aesthet Surg. 2010;3(2):87–89. doi: 10.4103/0974-2077.69018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Principi M., Cassano N., Contaldo A. Hydradenitis suppurativa and inflammatory bowel disease: an unusual, but existing association. World J Gastroenterol. 2016;22(20):4802–4811. doi: 10.3748/wjg.v22.i20.4802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kontinen V.K., Maunuksela E.L., Sarvela J. Premedication with sublingual triazolam compared with oral diazepam. Can J Anaesth. 1993;40(9):829–834. doi: 10.1007/BF03009253. [DOI] [PubMed] [Google Scholar]