Abstract
We present a case of metastatic prostate cancer with rare metastases involving the brain and orbit, in addition to liver, skeletal and nodal metastases. The patient had undergone prior hormonal therapy and chemotherapy and had disease progression despite 2 cycles of 177Lu-Prostate specific membrane antigen (177Lu-PSMA) based radioligand therapy. He had a partial response after 2 cycles of 225Ac-PSMA based targeted alpha therapy, as demonstrated on the 68Ga-PSMA PET/CT study. However, the patient had disease progression at the end of 4 cycles of 225Ac-PSMA therapy, evident by rising prostate specific antigen levels and imaging findings. The end of treatment 68Ga-PSMA PET/CT showed additional sites of metastases in the orbit and brain apart from overall disease progression. These are rare sites of distant spread in prostate cancer and require urgent evaluation and local treatment to prevent potential complications. The importance of detection of metastatic sites in closed cavities is because of the requirement for urgent intervention to avoid compression related complications.
Key Words: Prostate Specific Membrane Antigen, Prostate cancer, Ocular, CNS, PET/CT
Introduction
68Ga-PSMA PET/CT is a valuable diagnostic modality for initial staging of prostate cancer, as well as in recurrence evaluation and treatment response assessment. 68Ga-PSMA PET/CT is also performed for evaluating potential candidates for PSMA-based radioligand therapy or targeted alpha therapy. In the present case, 68Ga-PSMA PET/CT was useful in demonstrating rare metastatic sites involving the brain and orbit, in a patient refractory to 2 cycles of 177Lu-PSMA and 4 cycles of 225Ac-PSMA therapy. The importance of detecting orbital and brain metastases on PET/CT in this patient, is the additional requirement of regional radiation therapy to prevent local compression related complications.
Case Report
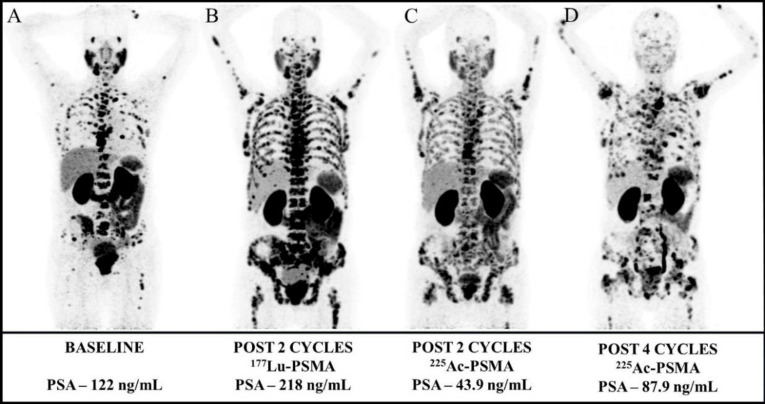
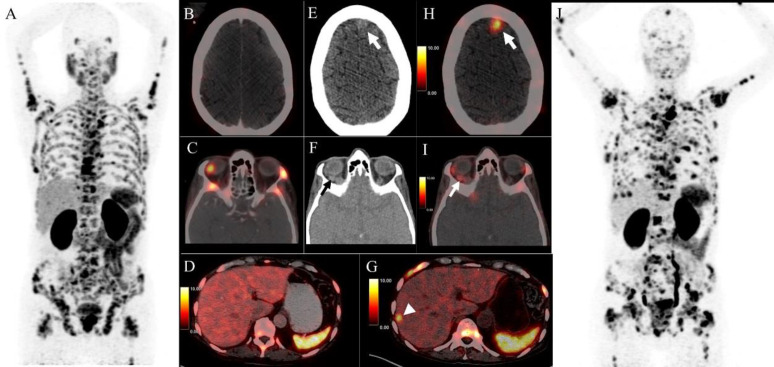
A 68-year-old man with metastatic castration resistant prostate cancer (mCRPC), involving multiple skeletal sites was found to have disease progression after docetaxel, cabazitaxel, enzalutamide therapy and two cycles of 177Lu-PSMA radioligand therapy. Figure 1 (A-D) shows the temporal sequence of 68Ga-PSMA-HBED-CC PET/CT maximum intensity projection (MIP) images at various time-points during therapy along with the relevant prostate specific antigen (PSA) values. The patient was considered for PSMA-based targeted alpha therapy and underwent 2 cycles of 225Ac-PSMA (each dose: 100 kBq/kg body weight) at 2-month interval. 68Ga-PSMA-HBED-CC PET/CT performed for response assessment (Figure 2-A) showed tracer avid lesions in the prostate and multiple skeletal metastases (without any visceral lesions; Figure 2-B, C, D) and reduction in tracer avidity of most of the lesions with a > 50% decline in PSA (218 ng/mL to 43.9 ng/mL) and significant improvement in pain due to osseous metastases.
Figure 1.
68Ga-PSMA-HBED-CC PET/CT maximum intensity projection images obtained at baseline (A), with disease progression after 2 cycles of 177Lu-PSMA therapy (B). Partial favourable treatment response along with a >50% decline in PSA was observed after 2 cycles of 225Ac-PSMA therapy (C). However, after completion of 4 cycles of 225Ac-PSMA, the patient had disease progression on imaging, as well as on biochemical analysis (D)
Figure 2.
68Ga-PSMA-HBED-CC PET/CT performed after initial two cycles of 225Ac-PSMA therapy for response assessment (A) showing tracer avid lesions in the prostate and multiple skeletal metastases (without any visceral lesions; B, C, D). 68Ga-PSMA PET/CT performed after completion of a total of 4 cycles of 225Ac-PSMA therapy showing extensive tracer avid skeletal lesions and interval appearance of new lesions in the brain, involving the left frontal cortex (E, H – thick arrow), soft tissue lesion in the right retro-ocular location (F, I – thin arrow) and the segment VII of liver (G, arrow-head) with overall scan representing disease progression (J)
The patient further received 2 additional cycles of 225Ac-PSMA therapy. 68Ga-PSMA PET/CT performed after completion of a total of 4 cycles of 225Ac-PSMA therapy showed extensive tracer avid skeletal lesions and interval appearance of new lesions in the brain, involving the left frontal cortex (Figure 2-E, H – thick arrow), soft tissue lesion in the right retro-ocular location (Figure 2-F, I – thin arrow) and the segment VII of liver (Figure 2-G, arrow-head) with overall scan representing disease progression (Figure 2-J). Additionally, the PSA values showed a rising trend from 43.9 ng/mL to 87.9 ng/mL. Next generation sequencing (NGS) performed for BRCA1/2 and ATM gene was positive for ATM gene mutation. Clinically, the patient did not have any neurologic or visual symptoms. The patient was advised an ophthalmologic and radiation oncology consult in view of the brain and orbital metastases.
Discussion
68Ga-PSMA PET/CT, despite its non-specificity to prostate cancer, has shown superior diagnostic performance in initial staging of high risk prostate cancer, recurrence assessment and has shown utility in patient selection for PSMA based radioligand therapy (177Lu-PSMA) or targeted alpha therapy (225Ac-PSMA) (1–6). The common sites of distant metastases include the non-regional lymph nodes (common iliac and more cranial lymph nodes) and bones (predominantly the axial skeleton) followed by lungs and liver as the relatively less common sites(4). The rare metastatic sites include the penis (7), testicles (8), kidneys, gastrointestinal tract, spleen, pancreas, thyroid, adrenals, brain/ meninges (4) and the orbit (9, 10). Commonly, these atypical metastatic sites appear in conjunction with an extensive nodal and skeletal metastatic disease, as seen in the present case.
Mutations in DNA repair genes have been associated with resistance to PSMA based alpha-therapy in prostate cancer (11). ATM is an activator of TP53 and acts as a sensor of DNA integrity prior to mitosis. Mutations involving ATM gene have been seen as one of the most common mutations in radioresistant prostate cancer and was also observed in our index patient (11). The addition of poly (ADP ribose) polymerase (PARP) inhibitor, Olaparib to 177Lu-DOTATATE based peptide receptor radionuclide therapy in neuroendocrine tumors, has shown improved tumoral toxicity (12). Additionally, Olaparib has specific anti-tumor activity in patients with ATM and BRCA1/2 gene mutations and thus may be beneficial as a combination treatment with alpha-therapy in the subgroup of patients with these identified genetic mutations (11). The expansion of genomics and metabolomics in patients with radioresistant prostate cancer can help us in identification of novel drug targets that may be added as combination treatments to improve outcomes of PSMA-based beta/alpha therapies.
Orbital metastases account for 1-13% of the diagnosed orbital tumors. The primary cancer sites with orbital metastases include the breast, lungs, melanoma, carcinoids, prostate and the gastrointestinal malignancies (13, 14). An orbital biopsy is commonly performed for confirmation of the metastasis, however in patients with extensive metastatic disease and a known primary, as in the present case, the risks of performing a biopsy quite often outweigh its potential benefits. Metastatic sites in the brain and orbit merit special attention as tumor expansion with/ without peri-tumoral edema in these closed cavities can quickly lead to compression of the vital structures, such as the globe and ocular muscles in the former, and the brain parenchyma in the latter. These patients have a rapid and non-remitting onset of symptoms and require urgent decompressive measures (13). Despite the extensive systemic involvement, as in the present case, the orbital and brain metastases need urgent attention to preserve the quality of life, including visual function and to avoid any rapidly developing local complications. Local radiation therapy is frequently the mainstay of treatment with the goal of achieving local tumor growth control (15). Interestingly, significant regression of cerebral metastases has been documented using 177Lu-PSMA and 225Ac-PSMA based therapies without any adverse local effects (16, 17). Thus, in a patient naïve to PSMA based radioligand or alpha-therapy, or with an effective prior treatment, 177Lu-/225Ac-PSMA therapies remain a viable option for treatment of brain metastases.
68Ga-PSMA PET/CT, in the present case proved useful in identification of the rare sites of metastases in the orbit and brain, enabling a prompt referral to an ophthalmologist and radiation oncologist, apart from documenting disease progression on the current therapeutic regimen.
Conflict of interest
Ashwin Singh Parihar, Kunal Ramesh Chandekar, Harpreet Singh, Ashwani Sood and Bhagwant Rai Mittal declare that they have no conflict of interest. There is no source of funding.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
The institutional review board of our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
References
- 1.Perera M, Papa N, Roberts M, Williams M, Udovicich C, Vela I, et al. Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer—Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta- Eur Urol. 2020;77:403–17. doi: 10.1016/j.eururo.2019.01.049. [DOI] [PubMed] [Google Scholar]
- 2.Rousseau C, Le Thiec M, Ferrer L, Rusu D, Rauscher A, Maucherat B, et al. Preliminary results of a 68Ga-PSMA PET/CT prospective study in prostate cancer patients with occult recurrence: Diagnostic performance and impact on therapeutic decision-making. Prostate. 2019;79:1514–22. doi: 10.1002/pros.23869. [DOI] [PubMed] [Google Scholar]
- 3.Parihar AS, Vadi SK, Mittal BR, Kumar R, Bal A, Singh SK. 68Ga-PSMA-HBED-CC-avid synchronous urinary bladder paraganglioma in a patient with metastatic prostate carcinoma. Clin Nucl Med. 2018;43:e329–30. doi: 10.1097/RLU.0000000000002172. [DOI] [PubMed] [Google Scholar]
- 4.Barbosa FG, Queiroz MA, Nunes RF, Viana PCC, Marin JFG, Cerri GG, et al. Revisiting prostate cancer recurrence with PSMA PET: Atlas of typical and atypical patterns of spread. Radiographics. 2019;39:186–212. doi: 10.1148/rg.2019180079. [DOI] [PubMed] [Google Scholar]
- 5.Parihar AS, Mittal BR, Sood A, Basher RK, Singh G. 68Ga-Prostate-Specific Membrane Antigen PET/CT and 18F-FDG PET/CT of Primary Signet Ring Cell Breast Adenocarcinoma. Clin Nucl Med. 2018;43:e414–6. doi: 10.1097/RLU.0000000000002265. [DOI] [PubMed] [Google Scholar]
- 6.Parihar AS, Sood A, Mittal BR, Kumar R, Singh H, Dhatt SS. 68Ga-PSMA-HBED-CC PET/CT and 18F-FDG PET/CT in Ewing Sarcoma. Clin Nucl Med. 2020;45:E57–8. doi: 10.1097/RLU.0000000000002764. [DOI] [PubMed] [Google Scholar]
- 7.Vadi SK, Kumar R, Mittal BR, Parihar AS, Singh SK. Unusual Case of Diffuse Penile Metastasis of Prostate Cancer on 68Ga PSMA PET/CT Imaging and 177Lu PSMA Posttherapy Scintigraphy. Clin Nucl Med. 2018;43:276–8. doi: 10.1097/RLU.0000000000002001. [DOI] [PubMed] [Google Scholar]
- 8.Weiberg D, Radner H, Derlin T, Thon WF. Early Detection of Bilateral Testicular Metastases From Prostatic Adenocarcinoma Using 68Ga-PSMA Ligand PET/CT. Clin Nucl Med. 2017:42. doi: 10.1097/RLU.0000000000001659. [DOI] [PubMed] [Google Scholar]
- 9.Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, et al. Distribution of metastatic sites in patients with prostate cancer: A population-based analysis. Prostate. 2014;74:210–6. doi: 10.1002/pros.22742. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed M, Begum T. Orbital metastasis from prostate cancer. BMJ Case Rep. 2015:bcr2015211447. doi: 10.1136/bcr-2015-211447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kratochwil C, Giesel FL, Heussel CP, Kazdal D, Endris V, Nientiedt C, et al. Patients resistant against PSMA-targeting α-radiation therapy often harbor mutations in DNA damage-repair-associated genes. J Nucl Med. 2020;61:683–8. doi: 10.2967/jnumed.119.234559. [DOI] [PubMed] [Google Scholar]
- 12.Nonnekens J, van Kranenburg M, Beerens CEMT, Suker M, Doukas M, van Eijck CHJ, et al. Potentiation of peptide receptor radionuclide therapy by the PARP inhibitor olaparib. Theranostics. 2016;6:1821–32. doi: 10.7150/thno.15311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol. 2007;18:405–13. doi: 10.1097/ICU.0b013e3282c5077c. [DOI] [PubMed] [Google Scholar]
- 14.Jain TK, Parihar AS, Sood A, Basher RK, Bollampally N, Shekhawat AS, et al. Orbital metastasis: Rare initial presentation of an occult gall bladder carcinoma. Clin Nucl Med. 2018;43:188–9. doi: 10.1097/RLU.0000000000001937. [DOI] [PubMed] [Google Scholar]
- 15.Boldt HC, Nerad JA. Orbital Metastases from Prostate Carcinoma. Arch Ophthalmol. 1988;106:1403–8. doi: 10.1001/archopht.1988.01060140567024. [DOI] [PubMed] [Google Scholar]
- 16.Wei X, Schlenkhoff C, Schwarz B, Essler M, Ahmadzadehfar H. Combination of 177Lu-PSMA-617 and external radiotherapy for the treatment of cerebral metastases in patients with castration-resistant metastatic prostate cancer. Clin Nucl Med. 2017;42:704–6. doi: 10.1097/RLU.0000000000001763. [DOI] [PubMed] [Google Scholar]
- 17.Sathekge MM, Bruchertseifer F, Lawal IO, Vorster M, Knoesen O, Lengana T, et al. Treatment of brain metastases of castration-resistant prostate cancer with 225Ac-PSMA-617. Eur J Nucl Med Mol Imaging. 2019;46:1756–7. doi: 10.1007/s00259-019-04354-z. [DOI] [PubMed] [Google Scholar]