Abstract
The aim was to determine whether there is a difference in the periodontal aspect (gingival recession, probing pocket depth) of the palatally displaced canine (PDC) compared to the contralateral canine. Also, from a surgical perspective, sought to determine whether there is a difference (surgical duration, postoperative pain) between the surgical techniques. The word combinations were adapted for each electronic database: PubMed, LILACS, Scopus, Web of Science, Cochrane Library and gray literature. Studies that met the following criteria were considered eligible: (P) Patients who received orthodontic-surgical treatment for correction of PDC; (I) Performing orthodontic-surgical treatment for traction of the PDC; (C) Comparison of the tractioned canine with its contralateral or between the two techniques; (O) Gingival recession, probing pocket depth, postoperative complications and surgical duration; (S) Randomized and nonrandomized clinical studies or observational studies. The overall prevalence of gingival recession was estimated to be 10.53% [95% CI, 3.87% - 25.59%; I2 = 88%]. No statistically significant difference (p > 0.05) was found between the means of the variables gingival recession, probing pocket depth and surgical duration. The evidence suggests that traction of palatally displaced canines can be considered a reliable and acceptable procedure.
Keywords: Canine, Tooth eruption, Ectopic, Oral surgical procedures, Systematic review
1. Introduction
Canines are of great importance in establishing and maintaining the shape, aesthetics and function of the dental arch. [1] After the third molars, they are the teeth that are most affected by impaction, reaching about 2% of the population [2,3]. They are more common in the maxilla [[4], [5], [6]] with a unilateral tendency [7] and in most cases located in the palatal region [8]. Numerous factors can cause impaction of the upper canine, but the exact etiology is not known [1].
The diagnosis of impaction is performed through clinical and radiographic examinations, in addition to determining the location, for correct planning and conduct of the treatment to be performed. [9,10] The prognosis of treatment depends on the position, angulation of the canine in relation to the adjacent teeth and the possibility of the presence of ankylosis [8]. Various treatment alternatives are considered, such as extraction of the canine and movement of the premolars to the position of the same; auto transplantation; prosthetic rehabilitation to obtain occlusal harmony or association of a surgical technique with orthodontic treatment to move the tooth to the line of occlusion [8,11,12].
Orthodontic-surgical treatment is commonly used to correct the palatally displaced canines (PDC), which can be performed using the open or closed surgical exposure method. The open technique involves lifting the flap and removing the bone and mucosa, where after removing the surgical pack, the spontaneous eruption of the tooth is expected. Once it has erupted sufficiently for an orthodontic accessory to be glued, its alignment above the mucosa is initiated. [13] The closed technique, on the other hand, involves elevation of the flap, limited bone removal and accessory bonding to the exposed crown with the palatine mucosa superimposed, allowing the alignment of the tooth below it [14]. However, regardless of the technique used, the treatment of PDC can lead to a variable amount of periodontal damage [15,16].
Researchers point out advantages and disadvantages of the techniques, and the choice between them is somewhat controversial. [[17], [18], [19], [20], [21], [22]] In 2018, Sampaziotis et al. [23] published the most recent systematic review on the subject and concluded that there is no difference between the open and closed technique in relation to periodontal and aesthetic aspects, with the shortest time of surgery in the PDC group exposed by the open technique, however, the conclusion of this review was based only on qualitative analysis, and quantification was not performed through meta-analysis. In addition, a comparison was made only of the PDCs exposed between the different techniques, with no comparison between the PDCs exposed in relation to their untractioned contralateral with normal eruption. Therefore, in order to update the cumulative knowledge on the subject, enable a quantitative analysis and perform a comparison of the tractioned teeth with the contralateral canine with normal eruption, a new systematic review is justified.
Thus, the objective of this meta-analysis was to determine whether there is a difference in the periodontal aspect (gingival recession, probing pocket depth) of the PDC compared to the contralateral canine with normal eruption. Also, the analysis sought to determine, from a surgical perspective, whether there is a difference (surgical duration, postoperative pain) between the open and closed technique.
2. Material and methods
2.1. Protocol and registration
This systematic review was conducted and reported using the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analysis checklist (PRISMA) [24], and was registered in the International Prospective Register of Systematic Reviews (PROSPERO).
2.2. Eligibility criteria
Studies that met the following criteria using the acronym “PICOS” were considered to be eligible for this systematic review:
Population (P): Patients who received orthodontic-surgical treatment for traction and correction of the PDC.
Intervention (I): Orthodontic-surgical treatment for traction of the PDC.
Comparison (C): Contralateral tooth with normal eruption or between different tractioned PDCs (comparison between different surgical exposure techniques).
Outcomes (O): Primary outcomes - Gingival recession (measured clinically from the visible cement enamel junction to the gingival margin on the buccal midpoint of the crown) and probing pocket depth (measured at six points with a millimeter-periodontal probe: DB – distobuccal; MidB – midbuccal; MB – mesiobuccal; DL – distolingual; MidL – midlingual; ML – mesiolingual); Secondary outcomes - Discomfort and postoperative pain assessed using postoperative questionnaires, and surgical duration (in minutes from incision to last suture).
Types of studies (S): Randomized and nonrandomized clinical studies or cohort, case-control, cross-sectional studies were included. There was no restriction when age, malocclusion, orthodontic mechanics were used for traction, publication time or language.
2.3. Inclusion criteria
Studies were included in which the sample consisted of patients who had PDC and were treated through orthodontic-surgical treatment for the traction of the impacted tooth, which may have been performed using the open or closed surgical technique. The studies must have compared the tractioned teeth with the contralateral tooth (untractioned and with normal eruption), or, performed the comparison between the open and closed surgical technique (between different tractioned PDCs) in the same study. The studies should have evaluated the outcome of interest and have an analytical design (interventional or observational).
2.4. Exclusion criteria
The following exclusion criteria were applied:
-
1)
Animal studies;
-
2)
Studies that included participants with craniofacial deformity or syndromic individuals;
-
3)
Studies that did not compare the open and closed surgical technique or that did not have separate statistical data for the open or closed surgical technique compared to the contralateral tooth;
-
4)
Studies that did not evaluate the PDC or that did not have separate statistical data for PDC;
-
5)
Studies that evaluated another impacted tooth, where there were no separate statistical data for the canine;
-
6)
Studies in which there was no assessment of the outcomes of interest;
-
7)
Studies with incomplete or missing data;
-
8)
Studies that did not use fixed orthodontic appliance for traction of the impacted canine;
-
9)
Reviews, letters, conference summaries, personal opinions or case reports;
2.5. Information sources and search strategy
The word combinations and the appropriate truncation were adapted for each electronic database, and the following databases were used: PubMed, LILACS, Scopus, Web of Science and CENTRAL of the Cochrane Library (Appendix A). Gray literature searches were also carried out using Google Scholar, Open Gray and Proquest. After searching the electronic databases, a manual search of the references of the included studies was carried out to avoid the risk of not including any relevant study. References have been managed, and duplicates have been removed using the EndNote® X7 reference manager (Thomson Reuters, Philadelphia, PA). The searches were carried out on 20 July 2018 and were updated on 11 February 2020.
2.6. Study selection
The selection of studies was carried out in two phases. In the first phase, the titles and abstracts of all electronic databases were selected by two independent reviewers. All articles that did not appear to meet the inclusion criteria were excluded at this stage. In phase 2, the entire text was read in full, and the same eligibility criteria were applied by the same reviewers. Disagreements or dissimilar results between the two reviewers in phase 1 and 2 were resolved by discussion until a mutual agreement between the two reviewers was reached, and if there was no consensus, a third reviewer was consulted for final decision making. The final selection was based solely on the evaluation of the full text of the studies.
2.7. Data items and data collection process
Two reviewers independently selected and extracted data from the included articles and compared the information extracted. Any disagreement regarding an item of data was discussed between them and the third reviewer, and, if necessary, an expert was consulted to make the final decision. The following data were extracted from the included articles: author; publication year; country; study objective, sample characteristics (sample size, age, sex, type of surgical exposure); study design, results and conclusion. In cases of missing or incomplete data in the article, three attempts were made to contact the authors to obtain this unpublished information.
2.8. Risk of Bias in individual studies
For the evaluation of the possible risk of methodological bias for interventional studies, the “Cochrane Collaboration tool for assessing the risk of bias” was used. This tool covers sequence generation, allocation concealment, blinding, incomplete outcome data (e.g. dropouts and withdrawals) and selective outcome reporting. For each domain in the tool, the procedures undertaken for each study were described, including the use of verbatim quotes. A judgement as to the possible risk of bias on each of the six domains was made from the extracted information and rated as ‘high risk’ or ‘low risk’. If there was insufficient detail reported in the study, the study was judged as ‘unclear’, and the original study investigators were contacted for more information.
The methodology of the selected observational studies was assessed using the Meta-Analysis of Statistics Assessment and Review Instrument (Mastari) bias risk tool. [25] The risk of bias was categorized as “high” when the study had a “yes” score of less than 49%; “moderate” when the study had between 50%–69% of “yes” scores; and “low” when the study had more than 70% of “yes” scores for bias risk questions.
These judgments were made independently by two reviewers. The disagreements were resolved first by discussion and then by consulting a third author for arbitration.
2.9. Synthesis of results
The prevalence estimates for the gingival recession variable were synthesized through a meta-analytical analysis with a randomized effect model with the inverse variance method and the DerSimonian and Laird estimator [26], with the heterogeneity being assessed using the inconsistency index (I2) [27]. The Freeman-Tukey double arcsine transformation method was used so that the data followed an approximately normal distribution [28]. 95% confidence intervals (95% CI) were used, calculated by the Clopper-Pearson method. The analyses and the forest plot were performed using the Rstudio statistical software version 1.2.1335 (Rstudio Inc, Boston, USA).
The estimate of the summary effect for the variables of probing pocket depth, surgical duration and gingival recession were calculated using the weighted difference of means (MD) between the two comparison groups. The calculation of heterogeneity was performed using the I2 index. [29] I2 values greater than 50% were considered an indicator of substantial heterogeneity between the studies, suggesting the need for random effect analysis models; on the other hand, for values less than 50%, fixed model analysis were used. The forest plot for these variables were generated with the software Review Manager 5.3 (RevMan 5.3, Copenhagen, Denmark) [29]. The level of significance for all assessments was set at 5% and for a better assessment of heterogeneity, the analyses were divided into subgroups.
2.10. Risk of bias across studies
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) [30] system was used to evaluate the quality of evidence. Risk of bias, inconsistency, indirectness, imprecision and publication bias were evaluated by two authors, and the quality of evidence was classified into four levels: high, moderate, low and very low.
3. Results
3.1. Studies selection
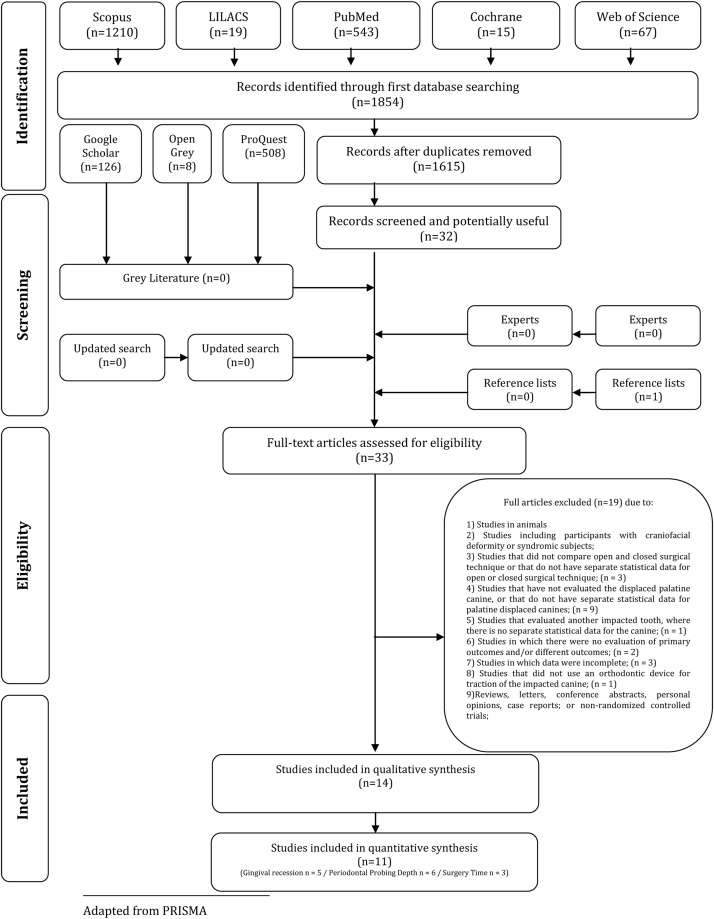
The final electronic search of the databases revealed 1854 records, and after removing the duplicates, 1615 records remained. A comprehensive evaluation of the titles and abstracts (phase 1) was carried out, and 1592 articles were excluded, resulting in a final number of 32 articles. The search in the gray literature was carried out in Google Scholar, Open Gray and Proquest, identifying 642 studies; however, no study was selected. A manual search was performed on the references of the 32 articles selected for phase 2, and an additional study was identified. Thus, 33 articles were selected to read the full text (phase 2), and nineteen of these were excluded (Appendix B). Thus, 14 studies remained and were included in the qualitative synthesis (Fig. 1). Kappa coefficient of agreement index was > 0.8, indicating excellent agreement between the reviewers.
Fig. 1.
Flowchart of search criteria and literature selection.
3.2. Study characteristics
The countries of origin of the included studies were Italy, Jordan, Lithuania, Norway, Sweden and United Kingdom.
The sample size ranged from 9 [31] to 293 [31] PDCs. The total sample of all included studies was composed of 68.7% women and 31.3% men, and of the total of included studies, two did not report the gender of the sample [32,33], and some studies were composed of the same sample [[34], [35], [36], [37]] evaluating different outcomes, so these samples were only counted once to estimate the proportion.
The 14 studies included were composed of 8 randomized clinical studies and 6 retrospective cohort studies. The year of publication ranged from 1976 [33,38] to 2019 [32]. The characteristics of the studies are available in Table 1.
Table 1.
Summary of descriptive characteristics and outcomes of interest of the included studies (n = 14).
| Author, year | Aim of the study | Sample size | Age/Sex | Study design | Outcomes of interest | Conclusions |
|---|---|---|---|---|---|---|
| Bjorksved, M., et al. 2018 | To compare surgery time, complications and patients’ perceptions between closed and open surgical techniques in palatally impacted maxillary canines. |
119/ 60CL 59OP |
13.4 ± 1.46 75F 44M |
Interventional/ Randomized clinical trial | Surgery time did not differ significantly between the interventions. Complications though were more severe in bilateral cases and the patients experienced more pain and impairment in the open group. | There were no statistically significant differences regarding surgery time between the groups. Postoperative complications were similar between the groups in unilateral PDCs, but more common in the open group in bilateral cases. More patients in the open group experienced pain and impairment compared to the closed group. |
| Blair, G. S., et al., 1998 | The records of 96 consecutively treated patients, were reviewed after orthodontic alignment of the exposed teeth (Open technique). The exposed canines, were critically assessed. And the assessment involved scoring for clinical impression, mobility, gingival condition and pocketing, oral hygiene, vitality, and radiographic appearances. | 25 patiens and 30 canines/ 30 OP |
10.1–30.2 22F 3M |
Observational/ Retrospective cohort | Pocket depth was greater in the exposed teeth in comparison with contralateral side. There was no clinically detectable difference in tooth color between the exposed teeth and the control groups. Vitality testing demonstrated that internal controls had a significantly lower response than the exposed canines. | The results indicate that the technique of surgical exposure and orthodontic alignment of ectopic maxillary canines provides a satisfactory method of treatment. |
| Bollero, P., et al., 2017 | 14CL | 13.5 ± 1.4 8F 6M |
Observational/ Retrospective cohort | |||
| Caprioglio, A., et al., 2019 | To evaluate and compare the existing correlations between periodontal health outcome of palatally impacted maxillary canines and their initial position identified according to the different rates of impaction severity in adolescent patients after their exposure (closed technique) and alignment. | 293CL | 13.8 ± 1.2 | Observational/ Retrospective cohort | α-Angle and d-distance showed no significant differences in the periodontal outcome of palatally impacted maxillary after treatment. The only tested variable showing significant differences was S, since canines with CEJ visible at the end of the treatment presented sectors with a mean score of 1.67, which was significantly different (P < 0.05) when compared to the S-sector for the canines that showed PD < 2 mm at the end of the treatment. | Radiographic variables as α Angle and d-distance seem to not influence the periodontal outcome of the treated impacted canine regardless of the amount of gravity. On the contrary, S sector might play a significant role when higher rates of gravity are present suggesting the possibility in few cases for periodontal damage at the end of treatment. |
| Caprioglio, A., et al., 2013 | The aim of the present study was to evaluate the long-term periodontal response of palatally impacted maxillary canines aligned compared with contralateral spontaneously erupted teeth. | 33CL | 16.3 ± 3.9 24F 9M |
Observational/ Retrospective cohort | The average probing depth values showed no significant clinical differences. Probing depths recorded at the vestibular surface of the lateral incisor (P < 0.05) and at the midpalatal/midlingual aspect of the first premolar were statistically significant in comparison with the control elements. | The use of a closed-flap surgical technique in association with a codified orthodontic traction system (Easy Cuspid) allowed alignment of palatally impacted canines without damage to the periodontium. |
| Gharaibeh et al, 2008 | Compare the duration of surgery and the patient’s perception of pain after closed and open surgical exposure of unilateral palatally impacted maxillary canines | 32/ 16CL 16OP |
17.3 ± 4.6/ 28F 4M |
Interventional/ Randomized clinical trial | The mean surgical duration for the open-eruption technique was 30.9 ± 10.1 min compared with 37.7 ± 8.4 min for the closed-eruption technique. This difference was statistically significant (p = .006) On the first postoperative day, 6 patients (33%) in the close-eruption group reported severe pain compared with 4 patients (22%) in the open-eruption group. This difference was not statistically significant (p = .123) |
The surgical duration was significantly shorter in the open-eruption exposure. Postoperative pain was similar after open- and closed-eruption surgical exposures. However, there was a faster disappearance of severe pain among patients in the closed-eruption groups. |
| Mummolo, S., et al. 2018 | This prospective observational study investigated differences in periodontal health parameters between BIMC and PIMC after surgical orthodontic treatment with open technique and compared the findings with those from contralateral physiologically erupted canines. | 9OP | 18.50 ± 1.96 5F 4M |
Observational/ Prospective Cohort | No signifcant differences were observed in the PIMC group. | The periodontal status of PIMC was not affected by surgical orthodontic treatment with open technique. |
| Parkin et al, 2013 | Investigate differences in the periodontal outcomes of palatally displaced canines exposed with either an open or a closed surgical technique. | 71 / 36CL 35OP | 14.1 ± 1.6/ 52F 29M |
Interventional/ Randomized clinical trial | When the clinical periodontal attachment level values for the unoperated teeth were subtracted from the clinical periodontal attachment level values for the operated teeth, the mean difference between open and closed groups was just 0.1 mm (open, 0.5 mm, SD, 0.8; closed, 0.6 mm, SD, 0.6); this difference was not statistically (independent t test, P = 0.782). The mean attachment loss for 3 of 4 sites was found to be marginally greater in the closed group compared with the open group; however, the difference was not statistically significant. On the midbuccal aspect of the operated canine, in the closed group, 9 subjects (31%) had recession of at least 1 mm (7 subjects had recession of 1 mm, 2 had recession of 2 mm). In the open group, 8 participants (24%) showed recession of a least 1 mm (5 had 1 mm, 3 had 2 mm. No significant difference was found between the 2 groups (chi-square test, P = 0.774) | The exposure and alignment of PDC has a small impact on periodontal health. The magnitude of this impact is not influenced by surgical technique (in terms of open vs closed exposure) and is so small that it is unlikely to influence the prognosis of a tooth in the long term in most patients. |
| Parkin et al, 2012 | Investigate differences in surgical outcomes (time spent in the operating room and 10-day postoperative patient questionnaire findings) between open and closed exposure for palatally displaced maxillary canines | 71 / 36CL 35OP | 14.1 ± 1.6/ 52F 29M |
Interventional/ Randomized clinical trial | The mean operating times for the open and closed techniques were 34.3 ± 11.2 min and 34.3 ± 11.9 min, respectively (p = 0.986) Six of the nine participants reporting that pain was still present after several days were in the open group. Three of the four participants reporting no pain were in the closed group; however, the difference in pain duration between groups was not significant (p = 0.161) |
There was no difference in the operating time between the open and closed surgical techniques for palatally displaced maxillary canines. There were no differences in any of the patient-reported outcomes between the 2 surgical procedures. Although most participants reported pain, discomfort, impairment to everyday activies, and the need for regular analgesia after surgical exposure, in most patients this was of short duration and subsided after a few days. |
| Smailiene et al, 2013 | Evaluate the posttreatment status (Radiological, periodontal and intraoral examination – visual assessment of the color and shape of the crown, inclination, position in the dental arch, function) of palatally impacted canines treated applying 2 different surgical methods (open and closed) and to compare it with the status of naturally erupted canines | 43 / 21CL 22OP |
15.81 ± 3.04/ 35F 8M |
Interventional/ Randomized clinical trial | The findings of tooth position, inclination, color, and shape did not differ between groups. No significant differences in the occlusal contacts were found between the groups. The measurements of the PPD did not significantly differ between the groups. The differences in the gingival recession between groups open and closed were not significant. | The posttreatment status of the palatally impacted and the adjacent teeth after the surgical-orthodontic treatment did not significantly differ between the groups treated with 2 different surgical methods, i.e., the open technique with free eruption (open) and the closed flap technique (closed). Both treatment methods can be considered as acceptable for the treatment of palatally impacted canines. |
| Smailiene et al, 2013 | Evaluate post-treatment periodontal status of palatally impacted canines treated by open or closed technique and compare it with naturally erupted canines | 43 / 21CL 22OP |
15.81 ± 3.04/ 35F 8M |
Interventional/ Randomized clinical trial | Measurements of the PPD did not differ significantly between groups open and closed but differed from those in the contralateral quadrants with normally erupted canines. Differences in gingival recession between groups were nonsignificant. Width of keratinized tissue was greater in the open technique group, these measurements did not differ significantly from those in the closed technique group. Bone support did not differ significantly. Mean orthodontic treatment time was 28.41 ± 4.96 in group open and 32.19 ± 11.73 months (p > 0.05) in group closed. | After surgical-orthodontic treatment of palatally impacted canines, either by open surgery with open or by closed technique, there were no significant differences in post-treatment periodontal status of the canines and adjacent teeth. Both treatment methods are acceptable for treatment of the palatally impacted canines; even if the mean time from exposure to eruption / extrusion is somewhat shorter in the open exposure technique. Post-treatment PPD and the level of bone support were not dependent on the patients’ age at the start of treatment, the duration of treatment, or the initial horizontal and vertical localization of impacted canine. |
| Wisth, P. J., et al. 1976 | The aim was to investigate the periodontal status of orthodontically-treated palatally-impacted maxillary canines by clinical and radiographic methods, and to compare it with the status of contralateral canines. | 34/ 34OP |
17.3 19F 15M |
Interventional/ Randomized clinical trial | A comparison of the hygienic condition and the Gingival Index did not reveal any considerable differences between the experimental and the control teeth at the time of examination. A comparison between pocket depth loss of attachment, and distance from the CEJ to the interdental bone showed that the pocket on the distal surface was significantly deeper in the experimental group (p < 0.05). Both de buccal and the palatal surfaces of the experimental teeth displayed significantly greater loss attachment than did the control teeth. | The treated canines displayed significantly more loss of periodontal support on the buccal and palatal surfaces than did the untreated teeth. |
| Wisth, P. J., et al. 1976 | The purpose was to compare the periodontal condition of orthodontically corrected impacted maxillary canines in two groups (open and closed techniques) of patients subjected to different surgical procedures. | 56/ 34OP 22CL | 15.9 | Interventional/ Randomized clinical trial | Oral hygiene and gingival inflammation were approximately the same in both groups. The palatal pocket was deeper on teeth subjected to moderate surgical exposure, and the depth also varied more. The loss of fiber attachment was not significantly different except on the palatal surface, where it was greater after radical exposure and also varied more. The interdental bone height, which was measured on radiographs, varied more after radical than after moderate surgical exposure. | It seems likely that the moderate surgical procedure (closed technique) causes the least periodontal damage. The mean differences were, however, small. If one desires to be able to inspect the position of the tooth regularly, or to reduce the duration of treatment the radical surgical exposure (open technique) can be used. |
| Zasciurinskiene et al., 2008 | To evaluate the impact of surgical-orthodontic (closed technique) treatment and the initial vertical and mesiodistal position of palatally impacted maxillary canines on the periodontal health of impacted canines and adjacent teeth. | 32CL | 18.2 ± 5.1/ 22F 10M |
Observational/Cross-Sectional | A significant increase in pocket depth was found at the canine mesiopalatal point after surgical-orthodontic treatment. Also, a correlation was found between the initial mesiodistal and vertical position of the impacted canine and the posttreatment periodontal status of the impacted canine, the adjacent lateral incisor, and the first premolar. | A combined surgical orthodontic approach in the treatment of impacted maxillary canines produces clinically acceptable periodontal conditions. The average increase in pocket depth was less than 4 mm and clinically unimportant for most patients. |
Legend: NA = Not applicable; CL = Closed surgery; OP = Open surgery; F = Female; M = Male; PDC = palatally displaced canine; PPD = periodontal pocket depth.
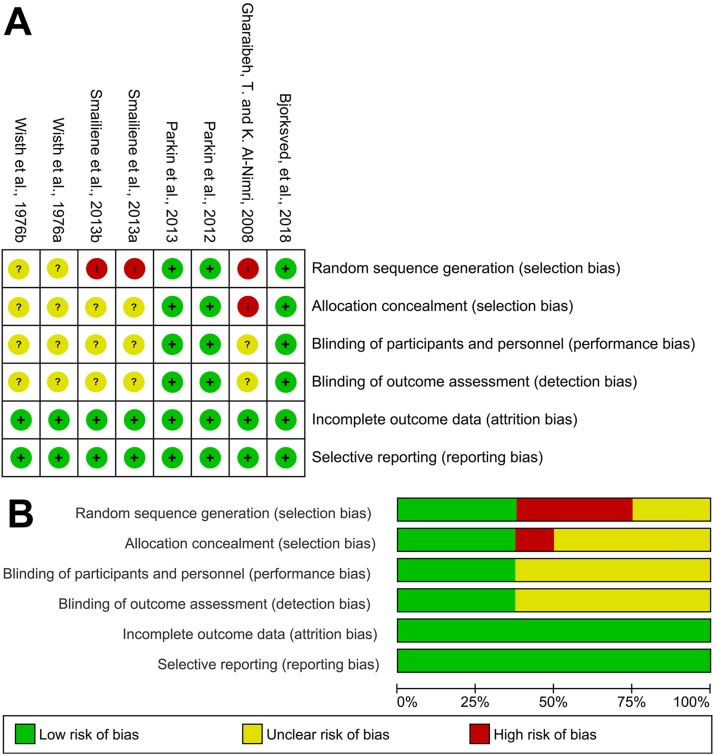
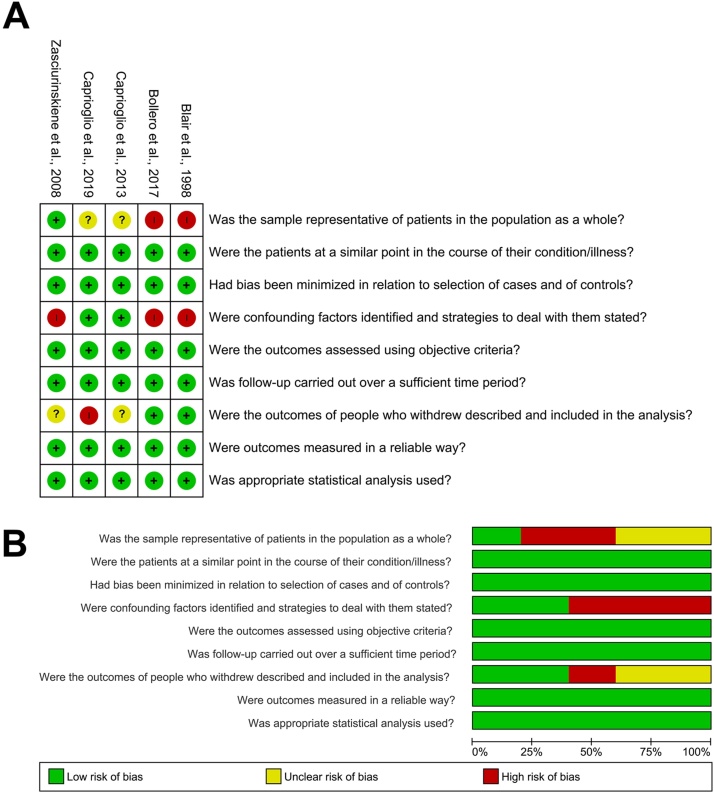
3.3. Risk of Bias within studies
Of the 8 randomized clinical studies included, 3 studies were low risk in all domains evaluated [34,35,39], and 5 were low risk in two of the six domains evaluated (Fig. 2). All included observational studies had a low risk of bias (Fig. 3).
Fig. 2.
Cochrane’s tool to assessed risk of bias in randomized controlled trials. Green indicates a low risk of bias, yellow indicates an unclear risk of bias, and red indicates a high risk of bias. a) Risk of bias summary; b) Graph.
Fig. 3.
Cohort studies assessed using Meta-Analysis of Statistics Assessment and Review Instrument (Mastari) critical appraisal tools. Green indicates a low risk of bias, yellow indicates an unclear risk of bias, and red indicates a high risk of bias. a) Risk of bias summary; b) Graph.
3.4. Results of individual studies
When comparing the periodontal aspect between the two surgical techniques, no study found statistically significant (p > 0.05) differences between the two techniques for the outcome of gingival recession [34,37] and probing pocket depth [36].
The level of complications resulting from surgery in the 4-week postoperative period were similar in both techniques [39]; however, patients undergoing the open surgical technique reported greater pain compared to the closed technique group, with a faster disappearance of severe pain in the group using the closed technique. [17]. On the other hand, the only article that used a validated questionnaire for measurement found no difference between the two techniques in any of the patients' postoperative reports, including pain [35].
In teeth operated by the open technique, vitality and periodontal status seem not to have been adversely affected [31,40] when compared to contralateral teeth. One study reported greater probing pocket depth in teeth operated by the open technique when compared to contralateral canines [38].
The evaluation of the probing pocket depth in PDCs and operated by the closed technique showed differences in results, where greater pocket depth was found in the mesiolingual region compared to contralateral canines, after the orthodontic treatment was completed (p < 0.05) [41]. However, one study reported that there was no difference in this aspect in relation to the contralateral canine [42]. The periodontal conditions of the impacted canine and adjacent teeth after surgical-orthodontic treatment in the closed technique seem to depend on the initial vertical and horizontal position of the impacted canine [43].
3.5. Synthesis of results
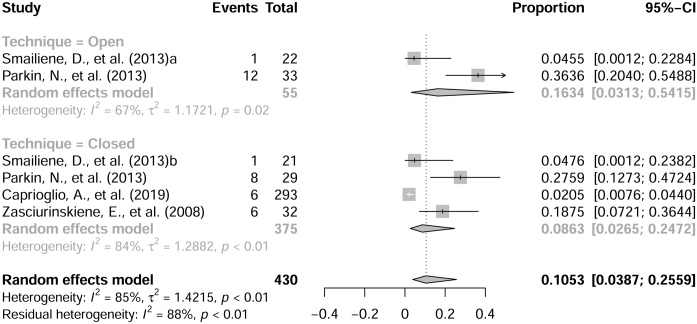
Of the total studies included, eleven studies were selected to perform the meta-analysis. The following outcomes were able to be quantitatively assessed by meta-analytical analysis: Gingival recession [32,34,36,43], probing pocket depth [32,36,38,41,43] and surgical duration [17,35,39].
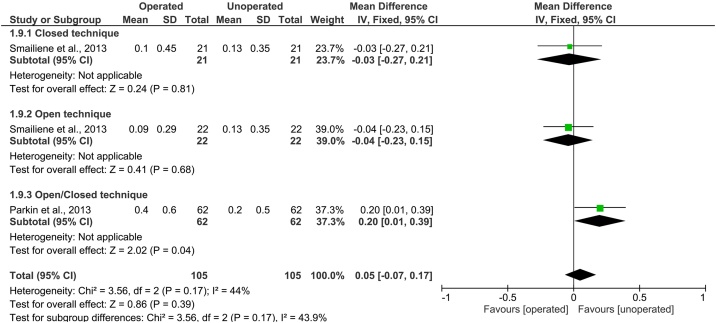
The combined global prevalence of gingival recession was based on 430 PDCs, with an estimated 10.53% [95% CI, 3.87 %–25.59 %; I2 = 88%] for the assessed outcome (Fig. 4). When comparing the difference between means of the variable gingival recession, the meta-analysis did not demonstrate a significant effect (p > 0.05) [MD = 0.05; 95% CI, -0.07 – 0.17; I2 = 44%] (Fig. 5).
Fig. 4.
Forest plot of the prevalence of canine gingival recession after orthodontic-surgical treatment.
Fig. 5.
Comparison between impacted canine versus contralateral canine, after orthodontic-surgical treatment, for the outcome of gingival recession.
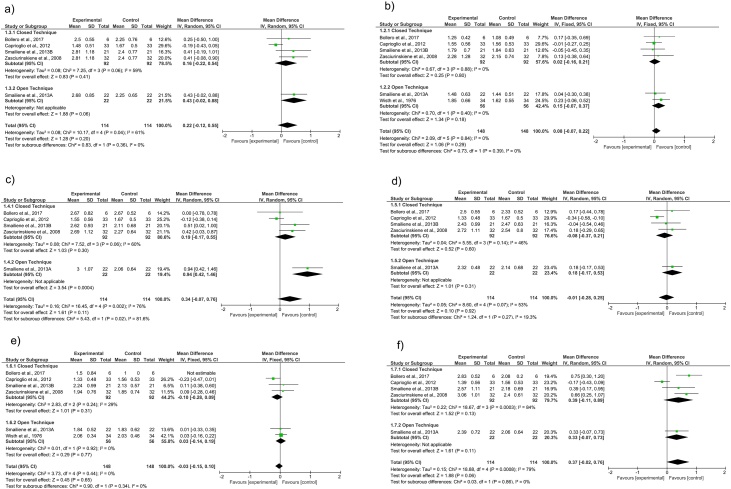
When comparing the probing pocket depth between the operated canines and the contralateral canine after the treatment was completed, there was no difference between the mean depth between the two groups in any of the evaluated sites (Fig. 6).
Fig. 6.
Comparison between the impacted canine versus the contralateral canine, after orthodontic-surgical treatment, for the probing pocket depth outcome: a) distobuccal; b) midbuccal; c) mesiobuccal; d) distolingual; e) midlingual; f) mesiolingual.
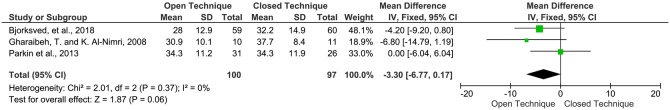
For the variable surgical duration, no significant difference was found between the open and closed techniques [MD = - 3.30; 95% CI, -6.77 – 0.17; I2 = 0%] (Fig. 7).
Fig. 7.
Comparison between open technique versus closed technique for the outcome time of surgery.
3.6. Risk of bias across studies
The overall quality of the evidence assessed by the GRADE tool was considered to be low and very low. The main factors responsible for the decrease in the level of evidence were methodological limitations (lack of randomization, confounding factors inherent in the included observational studies and individual studies with little clarity in the methodology for assessing bias), inconsistency (lack of control over confounding factors such as type of surgery, age, impacted canine position) and inaccuracy (wide confidence interval). (Table 2, Table 3).
Table 2.
GRADE summary of finding table for Periodontal aspects of the operated canine compared to the contralateral. Evidence level assessment for the following comparisons: Gingival Recession and Probing pocket depth.
| Outcomes | Anticipated absolute effects* (95% CI) |
Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
|---|---|---|---|---|---|---|
| Risk with Unoperated canine | Risk with Operated canine | |||||
| Gingival Recession | MD 0.05 higher (0.07 lower to 0.17 higher) | – | 210 (2 RCTs) | ⨁◯◯◯ VERY LOW a, b | The evidence is very uncertain about the effect of impacted canine traction on gingival Recession. | |
| Probing pocket depth - Canine (MidB) | MD 0.08 higher (0.07 lower to 0.22 higher) | – | 296 (6 observational studies) | ⨁◯◯◯ VERY LOW c | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (MidB). | |
| Probing pocket depth - Canine (DB) | MD 0.22 higher (0.12 lower to 0.55 higher) | – | 228 (5 observational studies) | ⨁◯◯◯ VERY LOW c, d | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (DB). | |
| Probing pocket depth - Canine (MB) | MD 0.34 higher (0.07 lower to 0.76 higher) | – | 228 (5 observational studies) | ⨁◯◯◯ VERY LOW c, d, e | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (MB). | |
| Probing pocket depth - Canine (DL) | MD 0.01 lower (0.28 lower to 0.25 higher) | – | 228 (5 observational studies) | ⨁◯◯◯ VERY LOW c, d | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (DL). | |
| Probing pocket depth - Canine (MidL) | MD 0.03 lower (0.15 lower to 0.1 higher) | – | 296 (6 observational studies) | ⨁◯◯◯ VERY LOW c | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (MidL). | |
| Probing pocket depth - Canine (ML) | MD 0.37 higher (0.02 lower to 0.76 higher) | – | 228 (5 observational studies) | ⨁◯◯◯ VERY LOW c, d, e | The evidence is very uncertain about the effect of impacted canine traction on probing pocket depth - Canine (ML). | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: Mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
The study by Smailiene et al. did not make clear some points of their assessment of risk of bias. Due to its weight in the analysis, it was classified as a serious risk of bias.
Few studies were included in the analysis; therefore, the analysis is not robust.
The analysis was composed mostly of observational studies.
Statistical heterogeneity across studies (I² between 50–80 %).
Wide confidence interval.
Table 3.
GRADE summary of finding table for surgery time of the operated canine comparing open and closed technique.
| Outcomes |
Anticipated absolute effects* (95% CI) |
Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
|---|---|---|---|---|---|---|
| Risk with Closed Technique | Risk with Open technique | |||||
| Surgery Time | MD 3.3 lower (6.77 lower to 0.17 higher) | – | 197 (3 RCTs) | ⨁⨁◯◯ LOWa, b | The evidence suggests that open technique results in little to no difference in surgery Time. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: Mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
The study by Gharaibeh et al, did not make clear some points of their assessment of risk of bias.
Few studies were included in the analysis; therefore, the analysis is not robust.
4. Discussion
The present meta-analysis aimed to answer whether there is a difference in the surgical-periodontal result (gingival recession, probing pocket depth, surgical duration and postoperative pain) for PDCs that were exposed and tractioned by open or closed surgical procedures. Based on the individual analysis of the included studies, both surgical techniques are reliable in relation to their periodontal surgical results. The meta-analytical analysis, likewise, demonstrated little impact on teeth submitted to this procedure, and both techniques seem to be acceptable to be performed.
Aesthetics compromised by gingival recession, in addition to the discomfort caused by root sensitivity, are common concerns of patients [44]. Diagnosis of periodontal conditions is essential to predict or prevent complications during the course of orthodontic treatment [45]. The overall proportion presented by the present meta-analysis, based on 430 impacted canines, showed an estimate of 10.53% [95% CI, 3.87% - 25.59%; I2 = 88%] for the presence of gingival recession in these post-traction teeth. Parkin et al. [34] found 20 cases of recession for a total of 62 operated canines (32.26%). On the other hand, Caprioglio et al. [32] found 6 cases for a sample of 293 operated canines (2.05%). These differences may occur due to confounding factors intrinsic to this evaluation, such as the chosen study model (observational studies have less control over these factors), post-orthodontic evaluation time, age, surgical technique for exposure of the impacted canine and its position. In addition, these data must be viewed with caution, as the study models of the articles included are not the best for assessing the prevalence of this variable. Despite these limitations, the meta-analytical method can be useful to obtain a more accurate estimate of the frequency of the disease, such as incidence rates and prevalence ratios [28]. However, despite the proportion estimate, with the scientific evidence available to date, it cannot be said that PDCs have a higher average of gingival recession (p > 0.05) [MD = 0.05; 95% CI, -0.07 – 0.17 I2 = 44%].
The choice of the method to be performed for surgical exposure of PDC is based on the prognosis in relation to the periodontal tissue that surrounds the tooth to be tractioned; thus, the orthodontic-surgical procedure must simulate the natural process of dental eruption [37]. When comparing the probing pocket depth between operated canines compared to the contralateral canine after an orthodontic treatment is completed, Caprioglio et al. [42] found no significant difference (p > 0.05) in any evaluated site. On the other hand, Smailiene et al. [37], found a significant difference (p < 0.05) for this outcome; however the authors did not consider a clinically important difference, as it did not exceed 3 mm. The overall effect presented by the present meta-analytical synthesis for the probing pocket depth outcome was not significant (p > 0.05) for all evaluated sites, thus demonstrating that there is no difference in this outcome between operated canines when compared to its contralateral.
The outcome surgical duration was the only one capable of quantitative analysis comparing the two techniques for exposure of the impacted canine, and the analysis of the results showed that there was no difference for this outcome between the two techniques [MD = -3.30; 95% CI, -6.77 – 0.17; I2 = 0%]. In this same sense, Parkin et al. [35] and Bjorksved et al. [39] found no difference in the surgical duration between the two techniques. On the other hand, Gharaibeh and Al-Nimri [17] reported shorter surgical durations for the open technique; however, items such as concealment of participants and staff (performance bias), allocation concealment (selection bias), generation of random sequence (selection bias) and concealment of the results evaluation (bias detection) were not clear in this study. In addition, confounding factors such as the position of the canine to be exposed and the surgeon's experience can influence the results. Despite this, no heterogeneity was detected in the results of the meta-analysis (I2 = 0%).
Heterogeneity was assessed in all analyses using the inconsistency index [27]. Based on this, for the meta-analytical analysis, we chose to use a randomized effect model for the outcomes: prevalence of gingival recession (I2 = 85%) and probing pocket depth (DB – I2 = 61%; MB - I2 = 76%; DL - I2 = 53%; ML - I2 = 79%), thus incorporating the influence of the heterogeneity verified in the weighting of the estimate of the effect. The limitations regarding the differences between the surgical technique, sample size of the included studies, in addition to the chosen study model, may be responsible for the heterogeneity presented in these analyses.
The results of this systematic review and meta-analysis show important data in relation to the surgical, periodontal and orthodontic aspects of PDCs, demonstrating the current stage of knowledge on the subject. These data are important to the orthodontist, surgeon and periodontist, facilitating communication with the patient regarding the predictability of the technique and stipulating the risks based on the current literature on the subject. However, some limitations should be pointed out, such as the number of included studies, the sample size of the included studies and the uncontrolled confounding factors in part of the included studies (observational studies). GRADE's evaluation shows that the quality of the evidence available on the subject is still low (surgical duration) and very low (probing pocket depth and gingival recession). Thus, the present study highlights the need for more prospective, multicenter, randomized clinical studies that are well conducted methodologically in order to make the analysis more robust.
5. Conclusion
The traction of PDCs can be considered a reliable and acceptable procedure, as there are no differences in relation to the periodontal aspect (recession, probing depth), and there are no differences regarding the time of surgery between the two surgical techniques. The available evidence is still uncertain to say whether the postoperative complications resulting from the surgery differ between the two techniques, so further studies should be performed to enable a quantitative analysis of the data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Thereare no study sponsors involved with the study.
Data availability statement
All the data associated with the study are presented within the manuscript.
Conflicts of interest
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jdsr.2020.10.001.
Contributor Information
Cristiano Miranda de Araujo, Email: cristiano.araujo@utp.br.
Pâmela Dias Trannin, Email: pamela.trannin@yahoo.com.br.
Angela Graciela Deliga Schroder, Email: angela.schroder@pucpr.edu.br.
José Stechman-Neto, Email: jose.stechmann@utp.br.
Bianca L. Cavalcante-Leão, Email: blcleao@gmail.com.
Natanael Henrique Ribeiro Mattos, Email: natanael.mattos@utp.br.
Bianca Simone Zeigelboim, Email: bianca.zeigelboim@utp.br.
Rosane Sampaio Santos, Email: rosane.santos2@utp.br.
Odilon Guariza-Filho, Email: odilongfilho@gmail.com.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Bishara S.E., Ortho D. Impacted maxillary canines: a review. Am J Orthod Dentofacial Orthop. 1992;101(2):159–171. doi: 10.1016/0889-5406(92)70008-X. [DOI] [PubMed] [Google Scholar]
- 2.Thilander B., Jakobsson S. Local factors in impaction of maxillary canines. Acta Odontol Scand Suppl. 1968;26(1-2):145–168. doi: 10.3109/00016356809004587. [DOI] [PubMed] [Google Scholar]
- 3.Ericson S., Kurol J. Longitudinal study and analysis of clinical supervision of maxillary canine eruption. Comm dent oral epid. 1986;14(3):172–176. doi: 10.1111/j.1600-0528.1986.tb01526.x. [DOI] [PubMed] [Google Scholar]
- 4.Mulick J.F., Dr. James F. Mulick on impacted canines. J Clin Orthod. 1979;13(12):824–834. [PubMed] [Google Scholar]
- 5.Jacoby H. The etiology of maxillary canine impactions. Am J orth. 1983;84(2):125–132. doi: 10.1016/0002-9416(83)90176-8. [DOI] [PubMed] [Google Scholar]
- 6.Ericson S., Kurol J. Resorption of incisors after ectopic eruption of maxillary canines: a CT study. Angle orth. 2000;70(6):415–423. doi: 10.1043/0003-3219(2000)070<0415:ROIAEE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Johnston W.D. Treatment of palatally impacted canine teeth. Am J Orth. 1969;56(6):589–596. doi: 10.1016/0002-9416(69)90194-8. [DOI] [PubMed] [Google Scholar]
- 8.Fournier A., Turcotte J.Y., Bernard C. Orthodontic considerations in the treatment of maxillary impacted canines. Am J Orth. 1982;81(3):236–239. doi: 10.1016/0002-9416(82)90056-2. [DOI] [PubMed] [Google Scholar]
- 9.Koutzoglou S.I., Kostaki A. Effect of surgical exposure technique, age, and grade of impaction on ankylosis of an impacted canine, and the effect of rapid palatal expansion on eruption: a prospective clinical study. Am J Orthod Dentofacial Orthop. 2013;143(3):342–352. doi: 10.1016/j.ajodo.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Pakbaznejad Esmaeili E. Minimum size and positioning of imaging field for CBCT scans of impacted maxillary canines. Clin Oral Investig. 2020;24(2):897–905. doi: 10.1007/s00784-019-02904-1. [DOI] [PubMed] [Google Scholar]
- 11.Bishara S.E. Clinical management of impacted maxillary canines. Semin Orthod. 1998;4(2):87–98. doi: 10.1016/s1073-8746(98)80006-6. [DOI] [PubMed] [Google Scholar]
- 12.Becker A., Chaushu S. Palatally impacted canines: the case for closed surgical exposure and immediate orthodontic traction. Am J Orthod Dentofacial Orthop. 2013;143(4):451. doi: 10.1016/j.ajodo.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Lewis P.D. Preorthodontic surgery in the treatment of impacted canines. Am J orth. 1971;60(4):382–397. doi: 10.1016/0002-9416(71)90150-3. [DOI] [PubMed] [Google Scholar]
- 14.Clark D. 11 the management of impacted canines: free physiologic eruption. JADA. 1971;82(4):836–840. doi: 10.14219/jada.archive.1971.0153. [DOI] [PubMed] [Google Scholar]
- 15.Oz A.Z., Ciǧer S. Health of periodontal tissues and resorption status after orthodontic treatment of impacted maxillary canines. Nig J Clin Pract. 2018;21(3):301–305. doi: 10.4103/njcp.njcp_419_16. [DOI] [PubMed] [Google Scholar]
- 16.Hansson C., Rindler A. Periodontal conditions following surgical and orthodontic treatment of palatally impacted maxillary canines - A follow-up study. Angle Orth. 1998;68(2):167–172. doi: 10.1043/0003-3219(1998)068<0167:PCFSAO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Gharaibeh T., Al-Nimri K. Postoperative pain after surgical exposure of palatally impacted canines: closed-eruption versus open-eruption, a prospective randomized study. Oral surg, oral med, oral path, oral rad end. 2008;106:339–342. doi: 10.1016/j.tripleo.2007.12.025. [DOI] [PubMed] [Google Scholar]
- 18.Woloshyn H. Pulpal and periodontal reactions to orthodontic alignment of palatally impacted canines. Angle orth. 1994;64(4):257–264. doi: 10.1043/0003-3219(1994)064<0257:PAPRTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Pearson M.H. Management of palatally impacted canines: the findings of a collaborative study. Eur J Orth. 1997;19(5):511–515. doi: 10.1093/ejo/19.5.511. [DOI] [PubMed] [Google Scholar]
- 20.Becker A., Chaushu S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2003;124(5):509–514. doi: 10.1016/s0889-5406(03)00578-x. [DOI] [PubMed] [Google Scholar]
- 21.Chaushu S. Patients’ perception of recovery after exposure of impacted teeth: a comparison of closed-versus open-eruption techniques. J oral max surg. 2005;63(3):323–329. doi: 10.1016/j.joms.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Zuccati G. Factors associated with the duration of forced eruption of impacted maxillary canines: a retrospective study. Am J Orthod Dentofacial Orthop. 2006;130(3):349–356. doi: 10.1016/j.ajodo.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 23.Sampaziotis D. Open versus closed surgical exposure of palatally impacted maxillary canines: comparison of the different treatment outcomes-a systematic review. Eur J Orthod. 2018;40(1):11–22. doi: 10.1093/ejo/cjw077. [DOI] [PubMed] [Google Scholar]
- 24.Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123–30. [PMC free article] [PubMed] [Google Scholar]
- 25.Institute J.B. 2014. Joanna Briggs institute reviewers’ manual: 2014 edition. [Google Scholar]
- 26.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 27.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 28.Barendregt J.J. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 29.Julian P.T.H. 2011. S.G., cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011] [Google Scholar]
- 30.GRADE, GRADE working group: the Grading of Recommendations Assessment, Development and Evaluation. 2014.
- 31.Mummolo S. Periodontal status of buccally and palatally impacted maxillary canines after surgical-orthodontic treatment with open technique. J Oral Sci. 2018;60(4):552–556. doi: 10.2334/josnusd.17-0394. [DOI] [PubMed] [Google Scholar]
- 32.Caprioglio A. Effects of impaction severity of treated palatally displaced canines on periodontal outcomes: a retrospective study. Prog Orthop Sci. 2019;20(1) doi: 10.1186/s40510-018-0256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wisth P.J., Norderval K., Bøe O.E. Comparison of two surgical methods in combined surgical-orthodontic correction of impacted maxillary canines. Acta Odontol Scand. 1976;34(1):53–57. doi: 10.3109/00016357609026558. [DOI] [PubMed] [Google Scholar]
- 34.Parkin N. Periodontal health of palatally displaced canines treated with open or closed surgical technique: a multicenter, randomized controlled trial. American journal of orthodontics and dentofacial orthopedics :tics. 2013;144:176–184. doi: 10.1016/j.ajodo.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Parkin N.A. No difference in surgical outcomes between open and closed exposure of palatally displaced maxillary canines. J Oral Max Surg. 2012;70(9):2026–2034. doi: 10.1016/j.joms.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 36.Smailiene D., Kavaliauskiene A., Pacauskiene I. Posttreatment status of palatally impacted maxillary canines treated applying 2 different surgical-orthodontic methods. Medicina-Lithuania. 2013;49(8):354–360. [PubMed] [Google Scholar]
- 37.Smailiene D. Palatally impacted maxillary canines: choice of surgical-orthodontic treatment method does not influence post-treatment periodontal status. A controlled prospective study. Eur J Orth. 2013;35(6):803–810. doi: 10.1093/ejo/cjs102. [DOI] [PubMed] [Google Scholar]
- 38.Wisth P.J., Norderval K., Boe O.E. Periodontal status of orthodontically treated impacted maxillary canines. Angle Orthod. 1976;46(1):69–76. doi: 10.1043/0003-3219(1976)046<0069:PSOOTI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 39.Bjorksved M. Closed vs open surgical exposure of palatally displaced canines: surgery time, postoperative complications, and patients’ perceptions: a multicentre, randomized, controlled trial. Eur J Orth. 2018;40(6):626–635. doi: 10.1093/ejo/cjy070. [DOI] [PubMed] [Google Scholar]
- 40.Blair G.S., Hobson R.S., Leggat T.G. Posttreatment assessment of surgically exposed and orthodontically aligned impacted maxillary canines. Am J Orthod Dentofacial Orthop. 1998;113(3):329–332. doi: 10.1016/s0889-5406(98)70305-1. [DOI] [PubMed] [Google Scholar]
- 41.Bollero P. Long-term periodontal status of palatally and buccally impacted canines after closed surgical-orthodontic approach. Oral Implantol. 2017;10(2):162–171. doi: 10.11138/orl/2017.10.2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caprioglio A., Vanni A., Bolamperti L. Long-term periodontal response to orthodontic treatment of palatally impacted maxillary canines. Eur J Orth. 2013;35(3):323–328. doi: 10.1093/ejo/cjs020. [DOI] [PubMed] [Google Scholar]
- 43.Zasciurinskiene E. Initial vertical and horizontal position of palatally impacted maxillary canine and effect on periodontal status following surgical-orthodontic treatment. Angle Orthod. 2008;78(2):275–280. doi: 10.2319/010907-8.1. [DOI] [PubMed] [Google Scholar]
- 44.Merijohn G.K. Management and prevention of gingival recession. Periodontol 2000. 2016;71(1):228–242. doi: 10.1111/prd.12115. [DOI] [PubMed] [Google Scholar]
- 45.D’Silva E. The association between gingival recession and buccal bone at maxillary anterior teeth. J Periodontol. 2019 doi: 10.1002/JPER.19-0375. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data associated with the study are presented within the manuscript.