Abstract
As a consequence of the COVID-19 pandemic, different measures have been implemented by governments from each affected country. Such measures usually involve restrictions on the movement of citizens, and have had a profound effect on usual activities and timetables. As a result of school closures and strict restrictions regarding going outside home, children have been one of the most disadvantaged population groups during the lockdown period. We therefore aimed to investigate potential health risk behaviors amongst isolated pre-school and school-aged children. We retrieved relevant articles from MEDLINE, Web of Science, PsycInfo, and Scopus databases to describe identified health-related behaviors (i.e. screen exposure, environmental influence, physical activity and fitness, sedentariness, sleep patterns, eating habits, psychological response, body composition, and injuries) in relation to social isolation and social deprivation of children without previous illness or conditions. This review depicts the potential health-related behaviors according to related literature, and put the focus on future short and long-term sequels of social isolation. Socio-affective complications and insufficient physical activity are underscored as two of the main concerns, particularly among socio-economic deprived children. Both issues could be effectively addressed with either adequate parental or community guidance.
Keywords: Coronavirus, COVID-19, Isolation, Confinement, Virus
1. Introduction
The pandemic of COVID-19 has rapidly spread worldwide since the first case was detected in Wuhan, China. Since then, more than two million diagnosed cases from more than two hundred countries have been documented, at the time of writing (World Health Organization, 2020). To date, there is no COVID-19 specific antiviral treatment recommended, no vaccine is available to prevent future infections, and prevention has been underscored to be the most effective measure to combat the spread of new contagions (Di Gennaro et al., 2020). Particularly elderly men and people exhibiting health risk behaviors or previous medical conditions (i.e. smoking history and underlying conditions such as chronic obstructive pulmonary disease, cardiovascular disease, cancer, hypertension and diabetes) have been observed to be the populations with higher risk of developing severe disease, need of medicalized intensive care, and mortality (Di Lorenzo and Di Trolio, 2020; Wang et al., 2020b). On the other hand, children do not seem to account for a large proportion of COVID-19 disease (i.e. 2% and 1.2% of the confirmed cases in respectively China and Italy), although a few severe cases and fatalities have been documented (Ong et al., 2020). The fact that most of the COVID-19 infected children were either asymptomatic or had mild to moderate disease (94.1%) put the focus of preventing spread of the disease on them in countries such as Italy and Spain, which were two of the first European countries to enact measures related to closuring schools (Ong et al., 2020). The rationale behind such decision could have been influenced by the higher percentages of children sharing households with elderly relatives in these countries (Lorenzo and Trolio, 2020), although this measure has been estimated to prevent substantially less deaths than other social distancing interventions (Viner et al., 2020). Furthermore, free-circulation of children outside households have been partially or totally restricted in several countries, with up to six or more weeks in a row holding this enacted measures (Spanish Government, 2020), although there is no certainty about potential collateral effects regarding this issue. Wang et al. (2020a) have raised the question about how COVID-19 lockdown might be affecting children, and they have suggested that both potential mental and physical health problems could be mitigated with higher parental and community involvement, whereas research on this issue is urgently required; many children, particularly those from lower socioeconomic backgrounds, might have been temporarily deprived of institutional educational environments, social contact with peers and, possibly, adequate cognitive, affective and physical stimuli for their age.
2. Methods
To inform this narrative review, we conducted a study search through four databases (MEDLINE, Web of Science, PsycInfo, and Scopus) using PRISMA procedures. The following search terms were used: confinement, isolation, solitude, children and truncated “psych” and “phys”. A more refined search of the literature comprised the following inclusion criteria: i) observational and review studies, ii) written in English language, iii) involving human subjects, iv) individuals aged 3 to 12 years, v) study population exposed to any type of either social isolation or deprivation, and vi) studies aiming to examine the influence of either social isolation or deprivation (i.e. from peers, relatives or both of them) over any type of health-related behaviors. Because there was no repetitive pattern regarding time or nature of the social isolation exposition in the examined studies, we adopted a conservative approach and considered social isolation and social deprivation as a situation in which children were separated from either peers, relatives or both of them during either a limited or unlimited period of time regardless the cause. Manually searched references derived from the articles consulted were also added to this search result. Given the lack of studies regarding isolated children, inclusion was broad and hinged on relevance of content and quality of evidence. Also, despite the scarce evidence for several health-related habits such as physical activity, eating habits, sleep patterns, or screen exposure in either socially isolated or socially deprived children, it was hypothesized that those will worsen during the confinement, which has been suggested in a novel study (López-Bueno et al., 2020). Therefore, information from relevant studies related to these health-related habits was also included in the present narrative review. On the other hand, the following exclusion criterion was used: i) articles involving population experiencing any previous condition or disease. Overall, evidence from more than 70 articles identified was classified by different health-related behaviors (i.e. screen exposure, sleep patterns, physical activity, physical fitness and sedentary behaviors, eating habits, psychological responses, body composition, environmental issues, and injuries) and used for the purpose of this study. There was a complete agreement among all authors upon which articles to include.
The present review aims to summarize the literature regarding health-related behaviors in isolated children without previous conditions with the objective to apply it to the current COVID-19 pandemic.
3. Health-related outcomes in isolated children
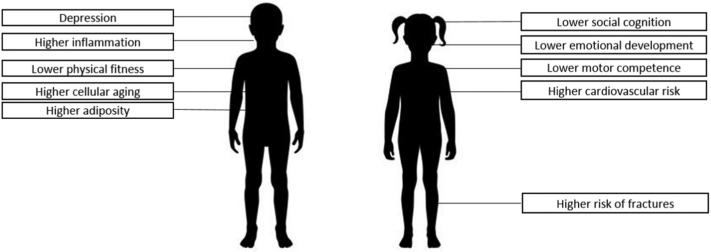
Social isolation during childhood has been independently linked to different conditions; connectedness has been observed to be a critical factor to increase the risk of post-traumatic stress disorders in a post-disaster context (McDermott et al., 2012). Being a socially isolated children was identified as an independent risk factor (i.e. apart from other well-stablished cardiovascular disease risk factors) for cardiovascular disease (i.e. elevated blood pressure, elevated total cholesterol level, overweight, low high-density lipoprotein level, low maximum oxygen consumption, and elevated glycated haemoglobin concentration) compared with non-isolated children even twenty years later; such childhood social isolation has been associated with higher inflammation (i.e. higher levels of C-reactive protein) which was partially due to subsequent lower education, less advantaged social class in adulthood, adult stress, and the tendency to obesity and to smoke (Caspi et al., 2006; Lacey et al., 2014). Early social deprivation has been linked to higher cellular aging (i.e. shorter telomere length) (Drury et al., 2012), and has profound effects over social cognition, and emotional development (Bick et al., 2017; Young et al., 2017). Further, early social deprivation had a negative effect on motor development, which was observed to be mediated by intelligence quotient, and could not be compensated with additional institutional measures (Levin et al., 2014). The main health areas identified through literature search in isolated pre-school and school-aged children are summarised in Table 1 .
Table 1.
Health-related areas identified in isolated pre-school and school-aged children.
| Screen exposure |
| Physical activity, physical fitness and sedentary behaviors |
| Eating habits |
| Psychological responses |
| Body composition |
| Environmental issues |
| Injuries |
4. Screen exposure
With the increase of time at home, TV viewing and use of PC, tablets and mobile phones is likely to increase; in fact, a recent study found that screen exposure increased by 4 h/day among children and adolescents during COVID-19 Lockdown in Italy (Pietrobelli et al., 2020). Because workers from many countries have been ordered to telework at home during the COVID-19 lockdown, the use of electronic devices may be seen as a useful tool to occupy children while parents work. In addition, ordinary school attendance has been widely substituted by digital homework or digital classes in many countries. Such screen-based behaviors (i.e. television viewing, computer use, and playing electronic games) have been linked to increased cardiovascular disease risk factors among children, although different effects have been detected among them (Robinson et al., 2015). For instance, online gaming and streaming activity have increased during the COVID-19 lockdown in different countries (King et al., 2020). This association seems to be mediated by adiposity, which might be favoured for both more snacks consumption and diet changes (Berentzen et al., 2014; Tsujiguchi et al., 2018). Several studies have suggested that children screen exposure is related to family behaviors regarding this issue, although this habit could be reduced with physical changes in the home environment and compensated with more physically active contents (De Decker et al., 2012; Faulkner et al., 2018; Niermann et al., 2018; Simons et al., 2015). Moreover, there is still a chance that high screen exposure increases depression among children (Kremer et al., 2014). Contrarily to expected, children from lower income households usually have easier access to TV, DVD and video games and less access to play equipment (i.e. jump ropes or bicycles) than their higher income counterparts (Tandon et al., 2014). There is mixed evidence on how such screen exposure might affect children's odds to develop myopia (Lanca and Saw, 2020).
5. Sleep patterns
Due to the fact that children are experiencing a change in their usual daily habits, it would be expected to find different sleep patterns; however, there is either moderate or insufficient evidence that daily habits such as higher screen time or fixed timetable substantially influence sleep, though higher physical activity and outdoor play have been directly associated with longer sleep in pre-schoolers (Belmon et al., 2019; Janssen et al., 2020). Overall, modifiable sleep patterns are per se normal among children between 3 and 7 years of age (Taylor et al., 2015). Particularly, longer sleep duration, which has been associated with lower body mass index, higher diet quality and higher levels of physical activity (Khan et al., 2015). Furthermore, sleep time increased by 0.65 h/day among children and adolescents during COVID-19 lockdown in Italy (Pietrobelli et al., 2020). This association between physical activity and sleep patterns has been observed to be bidirectional; thus, maintaining usual daily habits regarding physical activity and other usual activities might be useful in order to stimulate enough sleep time in younger children (Ávila-garcía et al., 2020; Sorić et al., 2015).
6. Physical activity, physical fitness and sedentary behaviors
The link between social isolation and lower physical activity levels and physical fitness in children was identified decades ago (Andersen et al., 1980), whereas the COVID-19 lockdown has now been observed to reduce by 2.30 h/week the exercise time among children and adolescents (Pietrobelli et al., 2020). High levels of moderate to vigorous physical activity and low levels of sedentary behavior are critical to achieve higher motor competence and higher health-related quality of life, with differences attributed to gender, socioeconomic status, sport club participation, and living areas for the second case (Adank et al., 2018; Wagner et al., 2014). Either physical activity or sports competitions have been observed to be associated with lower higher blood pressure, although that link was dependent of body mass index and cardiorespiratory fitness (Gaya et al., 2011). Besides, physical activity is generally a positive predictor of bone mineral density (Cardadeiro et al., 2014). Because many COVID-19 affected countries have closured ordinary school classes, effective physical activity might not be sufficiently applied to children outside school; school and physical education lessons usually make the difference and provide both adequate environments and support to encourage children to be physically active (Grao-Cruces et al., 2019; Gu et al., 2018; Hesketh et al., 2015; Eather et al., 2013; Wilkie et al., 2018). There might be a possibility that children will be able to intuitively compensate for higher sedentary behaviors with more physical activity at home, but the current evidence remains inconclusive, and it may further depend on the setting characteristics (Ridgers et al., 2018; Ridgers et al., 2014). Similarly, primary students might be more prone to elaborate strategies to be more physically active outside the school than their secondary counterparts (De Meester et al., 2014). Additionally, those with higher motor competence might be less affected by the COVID-19 lockdown, since they have usually exhibited higher physically active behaviors during the week (Foweather et al., 2015). A review by Xu et al. (Brouwer et al., 2018; Xu et al., 2015) found family roles to play an important role in promoting children physical activity, thus it might be a critical point to address when implementing health strategies aimed at them, particularly during this lockdown period. Besides, healthy lifestyle habits such as active commuting to schools (i.e walking or cycling), which has been linked to increasing both overall physical activity and physical fitness, and reducing sedentary behaviour (Aires et al., 2011; Aparicio-Ugarriza et al., 2020), have been partially or totally restricted due to COVID-19 governmental measures (i.e. measures vary depending on the country, although those most affected by COVID-19 have closured schools during, at least, several weeks, with some countries also restricting the ability to leave the home). Whether there is a link between higher levels of physical activity and an improvement of the immune function in children needs to be further investigated (Timmons, 2007).
7. Eating habits
Apparently, staying at home could improve eating habits since children and their families might consume less fast-food, which has been linked to higher risk for unhealthy dietary nutrient intake, obesity and coronary heart disease in children aged 9 to 10 years (Donin et al., 2018). In contrast, a recent study found that potato chip, red meat, and sugary drink intakes increased during the lockdown among obese children and adolescents in Italy (Pietrobelli et al., 2020). Furthermore, another recent study reviewing potential effect of Covid-19 quarantine over cardiovascular health suggested the lack of emotional support from both friends and relatives as a possible predictor for stress-driven eating and drinking behaviors which usually lead to poor eating habits (Mattioli et al., 2020). When reduced, food away from home consumption has been associated with lower body mass index and less body fat percentage, although this association is probably mediated by changes in diet quality (i.e. more fibre and less added sugars, and added fats). Although there are differences regarding eating habits and socioeconomic family status (i.e. families with higher socioeconomic status usually have healthier eating habits), knowledge and self-regulating behaviors still play an important role in this relationship (Pereira et al., 2019). The fact that food is usually eaten at convenience during COVID-19 lockdown may not importantly affect body mass index, since higher double breakfast eaters at school had more odds to exhibit a healthy weight (Wang et al., 2017). As suggested by Vissers et al. (2012) there seems to be no evidence between diet, physical activity, and sedentary behaviors in 9 to 10 year old children.
8. Psychological response
Early social isolation during primary school solely may not predict mental health problems later (Matthews et al., 2015). Concerning cognitive development, social isolated school children from farms were observed to perform worse in role-taking than rural children, but no differences were detected in logical operations (Cowan, 2016). Bi-directional associations between exclusion from school and mental health were identified among British children, although socioeconomic issues might mediate this relationship (Ford et al., 2018). Besides, psychosocial deprivation in children associates with higher levels of socio-emotional behavior problems later (McDermott et al., 2013). Since friends moderate young children's prospective associations between social isolation and adjustment problems, a controlled use of technology with these friend-connectivity purposes might be useful in this particular COVID-19 context of lockdown (Laursen et al., 2007; Williams et al., 2000). Particularly, School routines are important coping mechanisms for young people with mental health issues; a survey conducted by the mental health charity YoungMinds in participants up to age 25 years with mental illness history in the UK found that 83% of the sample worsened their condition during the pandemic and that 26% were unable to access mental health support (Guan et al., 2020).
9. Body composition
Individual, family and environmental factors have been traditionally linked to pediatric obesity (Sánchez-Cruz et al., 2014). A study by Nevill et al. (2016) found strong associations between weight status (i.e. waist circumference and body mass index) and social deprivation in children. Further, less perception of social isolation was associated to less overweight in children (de Assis et al., 2018). The possible decrease of physical activity levels, as well as an increase of sedentary behavior could contribute to increase children's fat percentage during COVID-19 lockdown (Collings et al., 2016; Meredith-Jones et al., 2018). Such adiposity increments are usually related to decrements in cardiorespiratory fitness levels and increments in blood pressure and C-reactive protein in children among both normal-weight and obese (Hayes et al., 2013; Tsiros et al., 2016).
10. Environmental issues
Housing and household occupancy conditions also deserve a closer look since they are related to health basic elements such as accessibility to community facilities and elementary needs, and could influence health risk behaviors (Lawrence, 2006). Neighborhood conditions affect children's development and independently account for a substantial part in the explanation of both emotional and behavioral problems (Caspi et al., 2000). Because important declines in vitamin D have been observed during months with less natural light and less nature light exposure in children from Northern latitudes, similar vitamin D declines might also occur among countries with stronger enacted measures concerning COVID-19 lockdown, although it could be mitigated through frequent intake of vitamin D supplements (Petersen et al., 2016). Outdoor play has been also underscored as a critical point in relation to increase physical activity, decrease sedentary behavior and improve weight status (i.e. lower weight), reinforced by the fact that rainy days associate with less overall physical activity in children (Larouche et al., 2016; Rahman et al., 2019; Stone and Faulkner, 2014). Further, environmental features of parks and presence of active peers have been associated with higher levels of physical activity in children (Floyd et al., 2011). Since children have been partially or completely deprived of those outdoor stimuli in many countries affected by the COVID-19 pandemic, homes can play an important role to provide the adequate environment to circumvent this situation. However, interaction with other children in institutionalized environments has been observed to provide higher levels of physical activity than nature-based orienteering activities; thus it might be possible that initial de-escalating COVID-19 lockdown measures based on going outside with proximity-to-others restrictions do not provide substantial increases regarding physical activity.(Barton et al., 2015) A case in point is the study review by Maitland et al. (2013), in which TV watching limitations and the existence of physical activity equipment were observed to mainly associate with less sedentary behavior and more physical activity among children. Household initiatives can also promote a healthy diet (i.e. vegetables consumption), making availability and accessibility to this food easier to children (Kristiansen et al., 2017). Besides, promoting motor skill development through home-based activities can lead to higher motor competence and support higher engagement in physical activity in pre-school aged children (Adamo et al., 2016).
11. Injuries
Although pediatric fractures are a common phenomenon, social deprivation in children has been observed to increase the odds of suffering a fracture as a result of a fall, blunt trauma, or a road traffic accident (Ramaesh et al., 2015). Due to a probably drop of physical activity levels in countries with more restrictive lockdown measures regarding COVID-19, risk of fractures might increase among children populations (Alshamrani et al., 2019). Particularly, accidents such as burns and scalds or high falls have been pointed out to be the most prevalent among social deprived British children (Silversides et al., 2005). Long-term physical consequences might not be expected since adverse childhood experiences have not been associated with musculoskeletal injuries years later (Ottenhoff et al., 2019). Similarly, social deprivation has been also observed to associate with self-harm in both children and adolescents (Ayton et al., 2003).
12. Perspectives
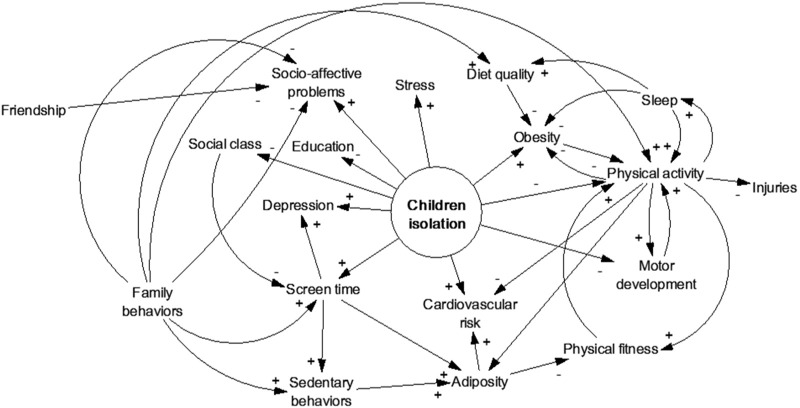
Because this is an unprecedented situation, there is no prior study regarding how a strict lockdown might affect health risk behaviors in healthy children. We assumed that similar situations of isolation in healthy children can provide valuable information about this topic. After reviewing more than 70 studies, we hypothesize both future socio-affective complications (i.e. hampered social interaction and lower social skills) and physical difficulties derived from insufficient physical activity (i.e. lower motor competence and injuries) regardless gender, although it could widely vary depending on each specific individual situation and the country enacted measures in relation to COVID-19. For instance, those countries with longer lockdowns and stricter restrictions could present children with higher health risk behaviors and subsequent derived sequels (Wang et al., 2020a); thus those countries might need to promote specific health strategies aimed at this population so that the mentioned deficits could be compensated and the regular timetables recovered; this would include a closer look on how educational institutions are dealing with these situations and make the learning process more efficient without promoting too much exposure to screen (e.g. massive online classes and mobile applications), which has been associated to less physical activity, higher adiposity and worse global cognition (Berentzen et al., 2014; Venetsanou et al., 2019; Walsh et al., 2018). Fig. 1 summarises potential health-related consequences of COVID-19 lockdown in children, which could be exacerbated with the course of time, whereas Fig. 2 illustrates a loop diagram highlighting the main associations among the identified health-related components according to the literature search. Only with the end of this pandemic, we will be able to estimate the real impact of this novel situation among children and to prevent potential health damage in similar situations to come. For that to happen, longitudinal research in collaboration with both families and schools should be further required and both community and family-friendly policies revised. As observed in prior research, both family support and adequate access to community facilities are warranted since it could contribute to mitigate the potential worsen of health-related behaviors (Lawrence, 2006; Xu et al., 2015).
Fig. 1.
Potential health-related consequences of COVID-19 lockdown in children.
Fig. 2.
Associations found in the study search regarding health-related components in isolated children.
13. Strengths and limitations
The main strength of our study is the search process carried out through four large databases. However, interpretations of the findings of this study should be made in the light of several limitations. First, the settings where most of the revised studies took place are substantially different among them as well as from the unprecedented Covid-19 pandemic we are living. This fact hampers generalizations or comparisons of the current situation with that from the examined research. Second, the review of the research was conducted using the available evidence to date thus it is quite likely that further studies will be published showing a better picture of the current situation; a case in point of a preliminary attempt is a recent study involving Spanish children whose health-related habits (i.e. physical activity, eating habits, and screen exposure) worsened during the Spanish Covid-19 strict confinement phase (López-Bueno et al., 2020).
14. Conclusions
This study provides an insight into the potential health-related behaviors regarding children locked down due to COVID-19 pandemic. As a consequence of isolation, lack of both socio-affective and physical activity stimuli emerge as two of the main concerns, particularly in socio-economic deprived children, although both issues could be mitigated with either adequate parental or community guidance or support. The maintenance of a regular timetable and the referral parents following healthy habits have been remarked as effective strategies to minimize potential health damage in isolated children.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contribution
RL-B and LS were responsible for the conception and design. All authors analyzed and interpreted the included articles and revised the present article for important intellectual content. RL-B drafted the article and is guarantor.
This manuscript has not been published and is not under consideration for publication elsewhere.
Declaration of Competing Interest
The authors declare that there are no conflict of interest.
References
- Adamo K.B., Wilson S., Harvey A.L.J., Grattan K.P., Naylor P.J., Temple V.A., Goldfield G.S. Does intervening in childcare settings impact fundamental movement skill development? Med. Sci. Sports Exerc. 2016;48:926–932. doi: 10.1249/MSS.0000000000000838. [DOI] [PubMed] [Google Scholar]
- Adank A.M., Van Kann D.H.H., Hoeboer J.J.A.A., de Vries S.I., Kremers S.P.J., Vos S.B. Investigating motor competence in association with sedentary behavior and physical activity in 7-to 11-year-old children. Int. J. Environ. Res. Public Health. 2018;15 doi: 10.3390/ijerph15112470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aires L., Pratt M., Lobelo F., Santos R.M., Santos M.P., Mota J. Associations of cardiorespiratory fitness in children and adolescents with physical activity, active commuting to school, and screen time. J. Phys. Act. Health. 2011;8(Suppl. 2):198–205. doi: 10.1123/jpah.8.s2.s198. [DOI] [PubMed] [Google Scholar]
- Alshamrani H.A., Alloub H., Burke D., Offiah A.C. Vitamin D intake, calcium intake and physical activity among children with wrist and ankle injuries and the association with fracture risk. Nutr. Health. 2019;25:113–118. doi: 10.1177/0260106019826422. [DOI] [PubMed] [Google Scholar]
- Andersen K.L., Seliger V., Rutenfranz J., Nesset T. Physical performance capacity of children in Norway. Eur. J. Appl. Physiol. Occup. Physiol. 1980;45:155–166. doi: 10.1007/bf00421323. [DOI] [PubMed] [Google Scholar]
- Aparicio-Ugarriza R., Mielgo-Ayuso J., Ruiz E., Ávila J.M., Aranceta-Bartrina J., Gil Á., Ortega R.M., Serra-Majem L., Varela-Moreiras G., González-Gross M. Active commuting, physical activity, and sedentary behaviors in children and adolescents from spain: findings from the ANIBES study. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17020668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ávila-garcía M., Femia-marzo P., Huertas-delgado F.J., Tercedor P. Bidirectional associations between objective physical activity and sleep patterns in spanish school children. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17030710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayton A., Rasool H., Cottrell D. Deliberate self-harm in children and adolescents: association with social deprivation. Eur. Child Adolesc. Psychiatry. 2003;12:303–307. doi: 10.1007/s00787-003-0344-0. [DOI] [PubMed] [Google Scholar]
- Barton J., Sandercock G., Pretty J., Wood C. The effect of playground-and nature-based playtime interventions on physical activity and self-esteem in UK school children. Int. J. Environ. Health Res. 2015;25:196–206. doi: 10.1080/09603123.2014.915020. [DOI] [PubMed] [Google Scholar]
- Belmon L.S., van Stralen M.M., Busch V., Hamsen I.A., Chinapaw M.J.M. What are the determinants of children's sleep behavior? A systematic review of longitudinal studies. Sleep Med. Rev. 2019;43:60–70. doi: 10.1016/j.smrv.2018.09.007. [DOI] [PubMed] [Google Scholar]
- Berentzen N.E., Smit H.A., Van Rossem L., Gehring U., Kerkhof M., Postma D.S., Boshuizen H.C., Wijga A.H. Screen time, adiposity and cardiometabolic markers: mediation by physical activity, not snacking, among 11-year-old children. Int. J. Obes. 2014;38:1317–1323. doi: 10.1038/ijo.2014.110. [DOI] [PubMed] [Google Scholar]
- Bick J., Luyster R., Fox N.A., Zeanah C.H., Nelson C.A. Effects of early institutionalization on emotion processing in 12-year-old youth. Dev. Psychopathol. 2017;29:1749–1761. doi: 10.1017/S0954579417001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer S.I., Küpers L.K., Kors L., Sijtsma A., Sauer P.J.J., Renders C.M., Corpeleijn E. Parental physical activity is associated with objectively measured physical activity in young children in a sex-specific manner: The GECKO Drenthe cohort. BMC Public Health. 2018;18:1–10. doi: 10.1186/s12889-018-5883-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardadeiro G., Baptista F., Rosati N., Zymbal V., Janz K.F., Sardinha L.B. Influence of physical activity and skeleton geometry on bone mass at the proximal femur in 10- to 12-year-old children - a longitudinal study. Osteoporos. Int. 2014;25:2035–2045. doi: 10.1007/s00198-014-2729-y. [DOI] [PubMed] [Google Scholar]
- Caspi A., Taylor A., Moffitt T.E., Plomin R. Neighborhood deprivation affects children's mental health: environmental risks identified in a genetic design. Psychol. Sci. 2000;11:338–342. doi: 10.1111/1467-9280.00267. [DOI] [PubMed] [Google Scholar]
- Caspi A., Harrington H.L., Moffitt T.E., Milne B.J., Poulton R. Socially isolated children 20 years later: risk of cardiovascular disease. Arch. Pediatr. Adolesc. Med. 2006;160:805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Collings P.J., Wijndaele K., Corder K., Westgate K., Ridgway C.L., Sharp S.J., Atkin A.J., Stephen A.M., Bamber D., Goodyer I., Brage S., Ekelund U. Objectively measured physical activity and longitudinal changes in adolescent body fatness: an observational cohort study. Pediatr. Obes. 2016;11:107–114. doi: 10.1111/ijpo.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan P.A. Social isolation and cognitive development: logical operations and role-taking abilities in three norwegian social settings. Child Dev. 2016;44:630–641. [Google Scholar]
- de Assis M.M., Leite M.A., Côrtes A.J., do Carmo A.S., Matozinhos F.P., Cândido A.P.C., Mendes L.L. Excesso De Peso, Ambiente Percebido E Privação Social: Um Estudo Da Percepção De Pais Ou Responsáveis. Rev. Paul. Pediatr. 2018;36:466–473. doi: 10.1590/1984-0462/;2018;36;4;00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Decker E., De Craemer M., De Bourdeaudhuij I., Wijndaele K., Duvinage K., Koletzko B., Grammatikaki E., Iotova V., Usheva N., Fernández-Alvira J.M., Zych K., Manios Y., Cardon G. Influencing factors of screen time in preschool children: an exploration of parents' perceptions through focus groups in six European countries. Obes. Rev. 2012;13:75–84. doi: 10.1111/j.1467-789X.2011.00961.x. [DOI] [PubMed] [Google Scholar]
- De Meester F., Van Dyck D., De Bourdeaudhuij I., Deforche B., Cardon G. Changes in physical activity during the transition from primary to secondary school in Belgian children: what is the role of the school environment? BMC Public Health. 2014;14:1–15. doi: 10.1186/1471-2458-14-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Gennaro F., Pizzol D., Marotta C., Antunes M., Racalbuto V., Veronese N., Smith L. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17082690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Lorenzo G., Di Trolio R. Vol. 7. 2020. Coronavirus Disease ( COVID-19 ) in Italy : Analysis of Risk Factors and Proposed Remedial Measures; pp. 23–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donin A.S., Nightingale C.M., Owen C.G., Rudnicka A.R., Cook D.G., Whincup P.H. Takeaway meal consumption and risk markers for coronary heart disease, type 2 diabetes and obesity in children aged 9-10 years: a cross-sectional study. Arch. Dis. Child. 2018;103:431–436. doi: 10.1136/archdischild-2017-312981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drury S.S., Theall K., Gleason M.M., Smyke A.T., De Vivo I., Wong J.Y.Y., Fox N.A., Zeanah C.H., Nelson C.A. Telomere length and early severe social deprivation: linking early adversity and cellular aging. Mol. Psychiatry. 2012;17:719–727. doi: 10.1038/mp.2011.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eather N., Morgan, Lubans D.R. Social support from teachers mediates physical activity behavior change in children participating in the Fit-4-Fun intervention. Int. J. Behav. Nutr. Phys. Act. 2013;10:1–15. doi: 10.1186/1479-5868-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner G., Bassett-Gunter R., White L., Berry T.R., Tremblay M.S. Can the Moblees™ move Canadian children? Investigating the impact of a television program on children's physical activity. Front. Public Heal. 2018;6:1–8. doi: 10.3389/fpubh.2018.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd M.F., Bocarro J.N., Smith W.R., Baran P.K., Moore R.C., Cosco N.G., Edwards M.B., Suau L.J., Fang K. Park-based physical activity among children and adolescents. Am. J. Prev. Med. 2011;41:258–265. doi: 10.1016/j.amepre.2011.04.013. [DOI] [PubMed] [Google Scholar]
- Ford T., Parker C., Salim J., Goodman R., Logan S., Henley W. The relationship between exclusion from school and mental health: a secondary analysis of the British Child and Adolescent Mental Health Surveys 2004 and 2007. Psychol. Med. 2018;48:629–641. doi: 10.1017/S003329171700215X. [DOI] [PubMed] [Google Scholar]
- Foweather L., Knowles Z., Ridgers N.D., O'Dwyer M.V., Foulkes J.D., Stratton G. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. J. Sci. Med. Sport. 2015;18:691–696. doi: 10.1016/j.jsams.2014.09.014. [DOI] [PubMed] [Google Scholar]
- Gaya A.R., Silva P., Martins C., Gaya A., Ribeiro J.C., Mota J. Association of leisure time physical activity and sports competition activities with high blood pressure levels: study carried out in a sample of portuguese children and adolescents. Child Care Health Dev. 2011;37:329–334. doi: 10.1111/j.1365-2214.2010.01179.x. [DOI] [PubMed] [Google Scholar]
- Grao-Cruces A., Segura-Jiménez V., Conde-Caveda J., García-Cervantes L., Martínez-Gómez D., Keating X.D., Castro-Piñero J. The role of school in helping children and adolescents reach the physical activity recommendations: the UP&DOWN Study. J. School Health. 2019;89:612–618. doi: 10.1111/josh.12785. [DOI] [PubMed] [Google Scholar]
- Gu X., Keller M.J., Weiller-Abels K.H., Zhang T. The roles of physical activity and sedentary behavior on Hispanic children's mental health: a motor skill perspective. Qual. Life Res. 2018;27:185–193. doi: 10.1007/s11136-017-1687-1. [DOI] [PubMed] [Google Scholar]
- Guan H., Okely A.D., Aguilar-Farias N., del Pozo Cruz B., Draper C.E., El Hamdouchi A., Florindo A.A., Jáuregui A., Katzmarzyk P.T., Kontsevaya A., Löf M., Park W., Reilly J.J., Sharma D., Tremblay M.S., Veldman S.L.C. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc. Health. 2020;4642:19–20. doi: 10.1016/S2352-4642(20)30131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes H.M., Eisenmann J.C., Pfeiffer K., Carlson J.J. Weight status, physical activity, and vascular health in 9- to 12-year-old children. J. Phys. Act. Health. 2013;10:205–210. doi: 10.1123/jpah.10.2.205. [DOI] [PubMed] [Google Scholar]
- Hesketh K.R., Griffin S.J., Van Sluijs E.M.F. UK preschool-aged children's physical activity levels in childcare and at home: a cross-sectional exploration. Int. J. Behav. Nutr. Phys. Act. 2015;12:1–9. doi: 10.1186/s12966-015-0286-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen X., Martin A., Hughes A.R., Hill C.M., Kotronoulas G., Hesketh K.R. Associations of screen time, sedentary time and physical activity with sleep in under 5s: a systematic review and meta-analysis. Sleep Med. Rev. 2020;49:101226. doi: 10.1016/j.smrv.2019.101226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M.K.A., Chu Y.L., Kirk S.F.L., Veugelers P.J. Are sleep duration and sleep quality associated with diet quality, physical activity, and body weight status? A population-based study of Canadian children. Can. J. Public Health. 2015;106:e277–e282. doi: 10.17269/CJPH.106.4892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D.L., Delfabbro P.H., Billieux J., Potenza M.N. Problematic online gaming and the COVID-19 pandemic. J. Behav. Addict. 2020;2020 doi: 10.1556/2006.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer P., Elshaug C., Leslie E., Toumbourou J.W., Patton G.C., Williams J. Physical activity, leisure-time screen use and depression among children and young adolescents. J. Sci. Med. Sport. 2014;17:183–187. doi: 10.1016/j.jsams.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Kristiansen A.L., Bjelland M., Himberg-Sundet A., Lien N., Andersen L.F. Associations between physical home environmental factors and vegetable consumption among Norwegian 3-5-year-olds: the BRA-study. Public Health Nutr. 2017;20:1173–1183. doi: 10.1017/S1368980016003396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacey R.E., Kumari M., Bartley M. Social isolation in childhood and adult inflammation: evidence from the National Child Development Study. Psychoneuroendocrinology. 2014;50:85–94. doi: 10.1016/j.psyneuen.2014.08.007. [DOI] [PubMed] [Google Scholar]
- Lanca C., Saw S.M. The association between digital screen time and myopia: A systematic review. Ophthal. Physiol. Opt. 2020;40:216–229. doi: 10.1111/opo.12657. [DOI] [PubMed] [Google Scholar]
- Larouche R., Garriguet D., Tremblay M.S. Outdoor time, physical activity and sedentary time among young children: the 2012–2013 Canadian Health Measures Survey. Can. J. Public Health. 2016;107:e500–e506. doi: 10.17269/CJPH.107.5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B., Bukowski W.M., Aunola K., Nurmi J.E. Friendship moderates prospective associations between social isolation and adjustment problems in young children. Child Dev. 2007;78:1395–1404. doi: 10.1111/j.1467-8624.2007.01072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence R.J. Housing and health: Beyond disciplinary confinement. J. Urban Health. 2006;83:540–549. doi: 10.1007/s11524-006-9055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin A.R., Zeanah C.H., Fox N.A., Nelson C.A. Motor outcomes in children exposed to early psychosocial deprivation. J. Pediatr. 2014;164:123–129. doi: 10.1016/j.jpeds.2013.09.026. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., López-Sánchez G.F., Casajús J.A., Calatayud J., Gil-Salmerón A., Grabovac I., Tully M.A., Smith L. Health-related behaviors among school-aged children and adolescents during the Spanish covid-19 confinement. Front. Pediatr. 2020;8:1–11. doi: 10.3389/fped.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maitland C., Stratton G., Foster S., Braham R., Rosenberg M. A place for play? The influence of the home physical environment on children's physical activity and sedentary behaviour. Int. J. Behav. Nutr. Phys. Act. 2013;10 doi: 10.1186/1479-5868-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews T., Danese A., Wertz J., Ambler A., Kelly M., Diver A., Caspi A., Moffitt T.E., Arseneault L. Social isolation and mental health at primary and secondary school entry: a longitudinal cohort study. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:225–232. doi: 10.1016/j.jaac.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattioli A.V., Ballerini Puviani M., Nasi M., Farinetti A. COVID-19 pandemic: the effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr. 2020;74:852–855. doi: 10.1038/s41430-020-0646-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott B., Berry H., Cobham V. Social connectedness: a potential aetiological factor in the development of child post-traumatic stress disorder. Aust. N. Z. J. Psychiatry. 2012;46:109–117. doi: 10.1177/0004867411433950. [DOI] [PubMed] [Google Scholar]
- McDermott J.M., Troller-Renfree S., Vanderwert R., Nelson C.A., Zeanah C.H., Fox N.A. Psychosocial deprivation, executive functions and the emergence of socio-emotional behavior problems. Front. Hum. Neurosci. 2013;7:1–11. doi: 10.3389/fnhum.2013.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith-Jones K., Haszard J., Moir C., Heath A.L., Lawrence J., Galland B., Taylor B., Gray A., Sayers R., Taylor R. Physical activity and inactivity trajectories associated with body composition in pre-schoolers. Int. J. Obes. 2018;42:1621–1630. doi: 10.1038/s41366-018-0058-5. [DOI] [PubMed] [Google Scholar]
- Nevill A.M., Duncan M.J., Lahart I., Sandercock G. Modelling the association between weight status and social deprivation in English school children: can physical activity and fitness affect the relationship? Ann. Hum. Biol. 2016;43:497–504. doi: 10.3109/03014460.2015.1115126. [DOI] [PubMed] [Google Scholar]
- Niermann C.Y.N., Spengler S., Gubbels J.S. Physical activity, screen time, and dietary intake in families: a cluster-analysis with mother-father-child triads. Front. Public Heal. 2018;6:1–12. doi: 10.3389/fpubh.2018.00276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.S.M., Tosoni A., Kim Y.J., Kissoon N., Murthy S. Coronavirus disease 2019 in critically ill children: a narrative review of the literature. Pediatr. Crit. Care Med. 2020:1–5. doi: 10.1097/PCC.0000000000002376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenhoff J.S.E., Kortlever J.T.P., Boersma E.Z., Laverty D.C., Ring D., Driscoll M.D. Adverse childhood experiences are not associated with patient-reported outcome measures in patients with musculoskeletal illness. Clin. Orthop. Relat. Res. 2019;477:219–228. doi: 10.1097/CORR.0000000000000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira B., Rosário P., Silva C., Figueiredo G., Núñez J.C., Magalhães P. The mediator and/or moderator role of complexity of knowledge about healthy eating and self-regulated behavior on the relation between family's income and children's obesity. Int. J. Environ. Res. Public Health. 2019:16. doi: 10.3390/ijerph16214207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen R.A., Damsgaard C.T., Dalskov S.M., Sorensen L.B., Hjorth M.F., Ritz C., Kjolbæk L., Andersen R., Tetens I., Krarup H., Astrup A., Michaelsen K.F., Molgaard C. Vitamin D status and its determinants during autumn in children at northern latitudes: a cross-sectional analysis from the optimal well-being, development and health for Danish children through a healthy New Nordic Diet (OPUS) School Meal Study. Br. J. Nutr. 2016;115:239–250. doi: 10.1017/S000711451500433X. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., Antoniazzi F., Piacentini G., Fearnbach S.N., Heymsfield S.B. Effects of covid-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S., Maximova K., Carson V., Jhangri G.S., Veugelers P.J. Stay in or play out? The influence of weather conditions on physical activity of grade 5 children in Canada. Can. J. Public Health. 2019;110:169–177. doi: 10.17269/s41997-019-00176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaesh R., Clement N.D., Rennie L., Gaston M.S., Court-Brown C. Social deprivation as a risk factor for fractures in childhood. Bone Jt. J. 2015;97-B:240–245. doi: 10.1302/0301-620X.97B2.34057. [DOI] [PubMed] [Google Scholar]
- Ridgers N.D., Timperio A., Cerin E., Salmon J. Compensation of physical activity and sedentary time in primary school children. Med. Sci. Sports Exerc. 2014;46:1564–1569. doi: 10.1249/MSS.0000000000000275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgers N.D., Lamb K.E., Timperio A., Brown H., Salmon J. Investigating children's short-term responses to imposed or restricted physical activity. J. Phys. Act. Health. 2018;15:239–246. doi: 10.1123/jpah.2017-0297. [DOI] [PubMed] [Google Scholar]
- Robinson S., Daly R.M., Ridgers N.D., Salmon J. Screen-based behaviors of children and cardiovascular risk factors. J. Pediatr. 2015;167:1239–1245. doi: 10.1016/j.jpeds.2015.08.067. [DOI] [PubMed] [Google Scholar]
- Sánchez-Cruz J.J., de Ruiter I., Jiménez-Moleón J.J. Individual, family and environmental factors associated with pediatric excess weight in Spain: a cross-sectional study. BMC Pediatr. 2014;14:3. doi: 10.1186/1471-2431-14-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silversides J.A., Gibson A., Glasgow J.F.T., Mercer R., Cran G.W. Social deprivation and childhood injuries in North and West Belfast. Ulster Med. J. 2005;74:22–28. [PMC free article] [PubMed] [Google Scholar]
- Simons M., Brug J., Chinapaw M.J.M., De Boer M., Seidell J., De Vet E. Replacing non-active video gaming by active video gaming to prevent excessive weight gain in adolescents. PLoS One. 2015;10:1–21. doi: 10.1371/journal.pone.0126023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorić M., Starc G., Borer K.T., Jurak G., Kovač M., Strel J., Mišigoj-Duraković M. Associations of objectively assessed sleep and physical activity in 11-year old children. Ann. Hum. Biol. 2015;42:31–37. doi: 10.3109/03014460.2014.928367. [DOI] [PubMed] [Google Scholar]
- Spanish Government Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. 2020. https://www.boe.es/buscar/doc.php?id=BOE-A-2020-3692 2020.
- Stone M.R., Faulkner G.E.J. Outdoor play in children: associations with objectively-measured physical activity, sedentary behavior and weight status. Prev. Med. (Baltim.) 2014;65:122–127. doi: 10.1016/j.ypmed.2014.05.008. [DOI] [PubMed] [Google Scholar]
- Tandon P., Grow H.M., Couch S., Glanz K., Sallis J.F., Frank L.D., Saelens B.E. Physical and social home environment in relation to children's overall and home-based physical activity and sedentary time. Prev. Med. (Baltim.) 2014;66:39–44. doi: 10.1016/j.ypmed.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor R.W., Williams S.M., Farmer V.L., Taylor B.J. The stability of sleep patterns in children 3 to 7 years of age. J. Pediatr. 2015;166:697–702. doi: 10.1016/j.jpeds.2014.11.014. e1. [DOI] [PubMed] [Google Scholar]
- Timmons B.W. Exercise and immune function in children. Am. J. Lifestyle Med. 2007;1:59–66. doi: 10.1177/1559827606294851. [DOI] [Google Scholar]
- Tsiros M.D., Coates A.M., Howe P.R.C., Walkley J., Hills A.P., Wood R.E., Buckley J.D. Adiposity is related to decrements in cardiorespiratory fitness in obese and normal-weight children. Pediatr. Obes. 2016;11:144–150. doi: 10.1111/ijpo.12037. [DOI] [PubMed] [Google Scholar]
- Tsujiguchi H., Hori D., Kambayashi Y., Hamagishi T., Asakura H., Mitoma J., Kitaoka M., Anyenda E.O., Nguyen T.T.T., Yamada Y., Hayashi K., Konoshita T., Sagara T., Shibata A., Sasaki S., Nakamura H. Relationship between screen time and nutrient intake in Japanese children and adolescents: a cross-sectional observational study. Environ. Health Prev. Med. 2018;23:1–12. doi: 10.1186/s12199-018-0725-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venetsanou F., Kambas A., Gourgoulis V., Yannakoulia M. Physical activity in pre-school children: trends over time and associations with body mass index and screen time. Ann. Hum. Biol. 2019;46:393–399. doi: 10.1080/03014460.2019.1659414. [DOI] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including COVID-19 : a rapid systematic review. Lancet Child Adolesc. Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vissers P.A.J., Jones A.P., van Sluijs E.M.F., Jennings A., Welch A., Cassidy A., Griffin S.J. Association between diet and physical activity and sedentary behaviours in 9-10-year-old British White children. Public Health. 2012;127:231–240. doi: 10.1016/j.puhe.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner M.O., Bös K., Jekauc D., Karger C., Mewes N., Oberger J., Reimers A.K., Schlenker L., Worth A., Woll A. Cohort profile: the Motorik-Modul Longitudinal Study: physical fitness and physical activity as determinants of health development in German children and adolescents. Int. J. Epidemiol. 2014;43:1410–1416. doi: 10.1093/ije/dyt098. [DOI] [PubMed] [Google Scholar]
- Walsh J.J., Barnes J.D., Cameron J.D., Goldfield G.S., Chaput J.P., Gunnell K.E., Ledoux A.A., Zemek R.L., Tremblay M.S. Associations between 24 hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc. Health. 2018;2:783–791. doi: 10.1016/S2352-4642(18)30278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Schwartz M.B., Shebl F.M., Read M., Henderson K.E., Ickovics J.R. School breakfast and body mass index: a longitudinal observational study of middle school students. Pediatr. Obes. 2017;12:213–220. doi: 10.1111/ijpo.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Zhang Z., Yu M., Tao Y., Xie M. 15-Day mortality and associated risk factors for hospitalized patients with COVID - 19 in Wuhan , China : an ambispective observational cohort study. Intensive Care Med. 2020:2–4. doi: 10.1007/s00134-020-06047-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkie H.J., Standage M., Gillison F.B., Cumming S.P., Katzmarzyk P.T. Correlates of intensity-specific physical activity in children aged 9-11 years: a multilevel analysis of UK data from the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open. 2018;8:1–11. doi: 10.1136/bmjopen-2017-018373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K.D., Cheung C.K.T., Choi W. Cyberostracism: effects of being ignored over the internet. J. Pers. Soc. Psychol. 2000;79:748–762. doi: 10.1037/0022-3514.79.5.748. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Vol. 74. 2020. Coronavirus disease 2019 (COVID-19): Situation Report.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Google Scholar]
- Xu H., Wen L.M., Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J. Obes. 2015;2015:1–23. doi: 10.1155/2015/546925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A., Luyster R.J., Fox N.A., Zeanah C.H., Nelson C.A. The effects of early institutionalization on emotional face processing: evidence for sparing via an experience-dependent mechanism. Br. J. Dev. Psychol. 2017;35:439–453. doi: 10.1111/bjdp.12185. [DOI] [PMC free article] [PubMed] [Google Scholar]