ABSTRACT
Objectives
The majority of cases of placenta previa or a low‐lying placenta in the second trimester will have a normal placental position in the third trimester. The aim of this study was to assess the accuracy of the distance between the placenta and the internal os of the cervix (IOD) in the second trimester for the prediction of third‐trimester low‐positioned placenta, and to define a cut‐off value at which all cases of third‐trimester low‐positioned placenta are identified.
Methods
This was a prospective cohort study including women undergoing a transvaginal ultrasound examination between 18 and 24 weeks' gestation who had a low‐positioned placenta, defined as an IOD of < 20 mm. Low‐positioned placenta included placenta previa, defined as a placenta covering the internal os of the cervix, and a low‐lying placenta, defined as a placenta lying near to (within 20 mm) but not overlying the internal os. All women were re‐evaluated in the third trimester. Relative risks for a low‐positioned placenta in the third trimester were calculated for women with placenta previa vs a low‐lying placenta, posterior vs anterior placenta and positive vs negative history of Cesarean section. Multilevel likelihood ratios for ranges of IOD in the prediction of a low‐positioned placenta in the third trimester were calculated separately for anteriorly and posteriorly located placentae. Corresponding receiver‐operating‐characteristics curves were constructed.
Results
In total, 958 women were included in the study. In the second trimester, placentae were more frequently located on the posterior side (62.0%) than on the anterior side (38.0%). In the third trimester, 48/958 (5.0%) placentae persisted as a low‐positioned placenta. Women with placenta previa in the second trimester had a higher risk of a low‐positioned placenta in the third trimester than did those with a low‐lying placenta in the second trimester (37/181 (20.4%) vs 11/777 (1.4%); relative risk (RR), 17.9 (95% CI, 8.9–36.0)). Women with a posterior placenta had a higher risk of a low‐positioned placenta in the third trimester than did those with an anterior placenta (38/594 (6.4%) vs 10/364 (2.7%); RR, 2.4 (95% CI, 1.2–4.9)), as did women with a history of Cesarean section compared with those without such a history (14/105 (13.3%) vs 34/853 (4.0%); RR, 3.7 (95% CI, 1.9–7.2)). The cut‐off value of IOD in the second trimester to identify all cases of an abnormally located placenta in the third trimester was 15.5 mm for posteriorly located placentae, while for anteriorly located placentae the IOD cut‐off was lower, namely –4.5 mm, representing a 4.5‐mm overlap of the placental edge over the internal os of the cervix.
Conclusions
With incorporation of a safety margin of 5 mm and ensuring that all women with placenta previa undergo a follow‐up scan, we recommend lowering the IOD cut‐off value for follow‐up in cases of an anterior low‐positioned placenta from 20 to 5 mm, which would decrease the number of unnecessary follow‐up ultrasound examinations without missing any high‐risk women. © 2019 The Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of International Society of Ultrasound in Obstetrics and Gynecology.
Keywords: low‐lying placenta, migration, placenta previa, second trimester, ultrasonography
Short abstract
A video abstract of this article is available online here.
What are the novel findings of this work?
A low‐lying placenta or placenta previa in the second trimester persists more often in the third trimester when the placenta is posteriorly located compared with when the placenta is located on the anterior side.
What are the clinical implications of this work?
In cases of an anterior low‐positioned placenta in the second trimester, we recommend lowering the cut‐off value of the distance between the placental edge and the internal os of the cervix from 20 mm to 5 mm for re‐evaluation of placental position in the third trimester.
INTRODUCTION
Placenta previa and low‐lying placenta are potentially fatal conditions for both mother and child. They are major causes of maternal hemorrhage and fetal complications such as prematurity and vasa previa 1 , 2 , 3 , 4 . To improve both maternal and fetal outcomes, it is important to diagnose low‐positioned placentae during pregnancy. However, owing to ‘placental migration’, over 90% of women with placenta previa or a low‐lying placenta in the second trimester will no longer have this condition in the third trimester 5 . Numerous guidelines advise re‐evaluation in the third trimester, but all agree that the number of ‘migrating’ low‐positioned placentae during pregnancy is high, and follow‐up in the third trimester will confirm normal placental position in most cases 6 . Thus, the necessity of follow‐up ultrasound examination in the third trimester for all women with a low‐positioned placenta in the second trimester is questionable 7 . In addition to the additional costs of follow‐up ultrasound, diagnosis of a low‐positioned placenta in the second trimester may also have a psychological impact on patients and carers 8 , as it could create needless fear of bleeding or other pregnancy complications, potentially contributing to more elective and emergency Cesarean sections.
If we could predict which women will have a low‐positioned placenta in the third trimester, we would be able to assign the necessary resources to those women at high risk for maternal and fetal complications. Recently, we performed a systematic review and meta‐analysis to evaluate the proportion of second‐trimester low‐positioned placentae that have a position towards the fundus in the third trimester. Unfortunately, we could not determine an optimal cut‐off value for anteriorly and posteriorly located placentae that included all women in whom the placenta would remain low in the third trimester 9 .
The aim of this study was to assess the accuracy of the distance between the placenta and the internal os of the cervix, in this study called the internal os distance (IOD), in the second trimester in the prediction of third‐trimester low‐positioned placenta and, more specifically, to define the cut‐off value at which all anteriorly and posteriorly located third‐trimester low‐positioned placentae would be identified in the second trimester with the smallest number of unnecessary follow‐up ultrasound examinations.
PATIENTS AND METHODS
Patients, setting and procedures
This was a prospective cohort study conducted at the Amsterdam UMC location Academic Medical Center in Amsterdam, a large tertiary hospital in The Netherlands. The study protocol was approved by the medical ethics committee of the hospital (W14‐294). Between 1 January 2014 and 1 October 2018, we included all pregnant women undergoing a routine second‐trimester scan in our center between 18 and 24 weeks' gestation who had a low‐positioned placenta, defined as an IOD of < 20 mm. Low‐positioned placenta included placenta previa, defined as a placenta covering the internal os of the cervix, and low‐lying placenta, defined as a placenta lying near to (within 20 mm) but not overlying the internal os 10 . Our hospital is a tertiary referral center for pregnant women, but it also serves as a regional ultrasound center for uncomplicated pregnancies. Therefore, ultrasound scans were performed in women receiving primary, secondary and tertiary care. We included only asymptomatic women with a scheduled appointment for ultrasound, which was mostly the 20‐week routine anomaly scan and occasionally a scan to assess fetal biometry. Women who consented to the measurement of IOD were included.
During the ultrasound examination, transabdominal sonography (TAS) was performed with the woman's bladder normally filled, using a Voluson E8 or E10 ultrasound machine (GE Healthcare, Zipf, Austria) with either a two‐dimensional (2D) convex transducer (C4‐8‐D; 2–8 MHz) or a RealTime 2D/ three‐dimensional (3D)/four‐dimensional (4D) convex transducer (RAB6‐D Ultra‐light; 2–8 MHz). Additional transvaginal sonography (TVS) was performed with the woman's bladder empty to measure the IOD in mm. TVS was performed using a micro‐convex 2D/3D/4D intracavitary transducer (RIC5‐9‐D; 4–6MHz). Placental location was documented as anterior or posterior, depending on the location of the largest area of the placenta. All ultrasound evaluations were performed by experienced sonographers trained in performing IOD measurements.
Women with an IOD of < 20 mm in the second trimester were scheduled for an ultrasound evaluation in the third trimester after 28 weeks' gestation. In the third trimester, all placentae were re‐evaluated primarily by TAS and, when a low‐positioned placenta could not be ruled out, an additional TVS scan was performed with Doppler ultrasound to exclude vasa previa. If the placental edge was within 20 mm of the internal os of the cervix, additional ultrasound evaluations were performed over the subsequent weeks, until the placenta had an IOD of ≥ 20 mm or until delivery. In such cases, the final classification of placental location (normal or abnormal) was based on the last ultrasound examination performed, i.e. the one closest to delivery.
Data collection
All ultrasound evaluations and measurements were documented and stored in the database Astraia version 3.4 (Astraia GmbH, Munich, Germany). Patient characteristics, including maternal age, mode of conception (spontaneous or by assisted reproductive technology), parity, previous Cesarean delivery and gestational age at ultrasound evaluation, were collected. In addition, delivery information was collected and categorized as vaginal delivery, Cesarean section due to hemorrhage as a result of a low‐positioned placenta or Cesarean section for other reasons (for example, fetal distress or breech presentation). As delivery in a hospital is medically indicated in women with an IOD of < 20 mm in The Netherlands, an uncomplicated delivery led by a primary‐care midwife would indicate normal placental location. Thus, when the follow‐up ultrasound measurements could not be retrieved, for example when they were performed elsewhere, but the baby was delivered by a normal vaginal delivery in primary care, we considered the final placental position to be normal.
Statistical analysis
The main outcome of our study was abnormal location of the placenta in the third trimester. Details of placental location included type (placenta previa or low‐lying placenta) and side (anterior or posterior) in the second and third trimesters. Baseline patient characteristics are reported with summary statistics. Continuous variables are presented as mean (SD) or median (interquartile range (IQR)), as appropriate, and categorical or dichotomous variables are presented as n (%).
Associations between baseline and ultrasound characteristics and abnormal placental location in the third trimester are expressed as relative risks with 95% CIs. After all significantly associated variables had been identified, the possible interactions between them were assessed by an interaction term using logistic regression analysis.
The association between IOD and placental location in the third trimester was evaluated and the accuracy of IOD in the prediction of abnormal placental location in the third trimester was assessed using receiver‐operating‐characteristics (ROC) curve analysis. If placental side was associated significantly with abnormal location in the third trimester, the analysis was performed separately for anteriorly and posteriorly located placentae. For different ranges of second‐trimester IOD, the corresponding (multilevel) likelihood ratios were calculated, i.e. the likelihood that an IOD within that range would be observed in the second trimester in a woman with an abnormally located placenta in the third trimester as opposed to one with normal third‐trimester placental location 11 . We aimed to define a cut‐off at which all abnormally located placentae in the third trimester would be identified with the smallest number of unnecessary follow‐up ultrasound examinations (i.e. an examination confirming a normally located placenta in the third trimester). At the ideal cut‐off, the likelihood ratio would be 0, meaning this (range of) IOD would be observed only in women with a normal placental position in the third trimester. This implies that an IOD below this cut‐off would identify all women with abnormal placental position in the third trimester. The number of women with an IOD within this range who had normal placental position in the third trimester corresponds to the number of unnecessary follow‐up ultrasound examinations. The optimal cut‐off values for abnormal placental location were also evaluated using available data at 32, 34 and 36 weeks' gestation.
Data analysis was performed using IBM SPSS statistics 25 (IBM Corp., Armonk, NY, USA); P < 0.05 was considered to indicate statistical significance.
RESULTS
A total of 1071 women with a low‐positioned placenta at the second‐trimester ultrasound examination were eligible for inclusion. Nineteen women (1.8%) were excluded owing to delivery or follow‐up evaluation before 28 weeks' gestation and 94 women (8.8%) were lost to follow‐up, leaving 958 women included in the study. The cohort baseline characteristics are shown in Table 1. In the second trimester, 777 (81.1%) women had a low‐lying placenta and 181 (18.9%) women had placenta previa. Placentae were more frequently located on the posterior side (594 women (62.0%)) than on the anterior side (364 women (38.0%)). Median gestational age at the second‐trimester scan was 19 (IQR, 19–20) weeks.
Table 1.
Baseline characteristics of 958 pregnant women with low‐positioned placenta in second trimester
| Characteristic | Value |
|---|---|
| Age (years) | 31 ± 5.5 |
| Parous | 527 (55.0) |
| Assisted reproductive technology | 129 (13.5) |
| Intrauterine insemination | 15 (1.6) |
| In‐vitro fertilization | 17 (1.8) |
| Intracytoplasmic sperm injection | 97 (10.1) |
| Smoker | 56 (5.8) |
| History of Cesarean delivery | 105 (11.0) |
| One | 99 (10.3) |
| Multiple | 6 (0.6) |
Data are given as mean ± SD or n (%).
Placental location in third trimester
The main outcome could be assessed in all women. Of the 958 included women, 755 had one or more follow‐up scans in the third trimester while the remaining 203 women had an uncomplicated vaginal delivery in primary care and thus were considered to have a normal final location of the placenta. In 738 women, the exact gestational age at follow‐up ultrasound was known. All follow‐up scans were performed between 28 and 38 weeks. Median gestational age at the first follow‐up scan was 31 (IQR, 31–32) weeks. The follow‐up ultrasound scan of these 738 women was performed by 32, 34 and 36 weeks' gestation in 648 (87.8%), 713 (96.6%) and 735 (99.6%) women, respectively.
In the third trimester, 48/958 (5.0%) placentae were abnormally located. All 297 second‐trimester anterior low‐lying placentae had a normal location in the third trimester. Of the 67 cases of second‐trimester placenta previa that were anteriorly located, 10 were abnormally located in the third trimester, of which five were still overlying the internal os and five were lying within 20 mm of the internal os. Of the second‐trimester posterior placentae, 480 were low lying and, of those, 469 had a normal location in the third trimester. Of the 114 cases of second‐trimester placenta previa that were posteriorly located, 27 were abnormally located in the third trimester, of which 18 were still overlying the internal os of the cervix and nine were lying within 20 mm of the internal os.
Table 2 shows the associations between abnormal third‐trimester placental location and a previous Cesarean delivery, the side of the placenta (anterior vs posterior) and the type of placental position in the second trimester (placenta previa or low‐lying placenta). Women with placenta previa, a posteriorly located placenta or a previous Cesarean section were at higher risk of having an abnormally located placenta in the third trimester. There were no significant interactions between the three variables.
Table 2.
Association between abnormal third‐trimester placental location and previous Cesarean delivery, side of placenta and type of placental location in 958 women with second‐trimester low‐positioned placenta
| Third‐trimester placental location (n (%)) | ||||
|---|---|---|---|---|
| Variable | Abnormal | Normal | Relative risk (95% CI) | P |
| Previous Cesarean delivery | ||||
| Yes (n = 105) | 14 (13.3) | 91 (86.7) | 3.7 (1.9–7.2) | < 0.001 |
| No (n = 853) | 34 (4.0) | 819 (96.0) | Reference | |
| Second‐trimester placental side | ||||
| Posterior (n = 594) | 38 (6.4) | 556 (93.6) | 2.4 (1.2–4.9) | 0.01 |
| Anterior (n = 364) | 10 (2.7) | 354 (97.3) | Reference | |
| Second‐trimester placental location | ||||
| Placenta previa (n = 181) | 37 (20.4) | 144 (79.6) | 17.9 (8.9–36.0) | < 0.01 |
| Low‐lying placenta (n = 777) | 11 (1.4) | 766 (98.6) | Reference | |
In our cohort, there were five women with vasa previa in the third trimester. One woman with placenta previa in the second trimester had a normal placental location in the third trimester, but during the last scan vasa previa was detected. In the other four women, vasa previa had already been detected in the second trimester. One of these women had a low‐lying placenta on the posterior side with an IOD of 17 mm and three had a bilobed placenta in the second trimester. There were no women with an abnormally invasive placenta.
IOD cut‐off values for third‐trimester abnormal placental position
Second‐trimester IOD was associated significantly with placental position in the third trimester in the whole cohort as well as when considering those with an anteriorly located placenta and those with a posteriorly located placenta separately, with a higher proportion of women with normal placental position in the third trimester for greater IOD values (P < 0.01 for all) (Figure 1). Table 3 shows that in women with a posteriorly located placenta, IOD values of at least 15.5 mm had a likelihood ratio of 0 in the prediction of an abnormally positioned placenta in the third trimester. In women with an anteriorly located placenta (Table 3), a likelihood ratio of 0 was reached for IOD values of at least –4.5 mm, representing a 4.5‐mm overlap of the placental edge over the internal os of the cervix. All women with an IOD at or above these cut‐off values can be reassured without follow‐up that their final placental position will be normal. This could have reduced the number of follow‐up ultrasound examinations from 364 to 54 in women with an anteriorly located placenta and the number of unnecessary follow‐up ultrasound examinations from 354 to 44. In women with a posterior placenta, the number of follow‐up ultrasound examinations would reduce from 594 to 500 and the number of unnecessary follow‐up ultrasound scans would reduce from 556 to 462. The corresponding ROC curves are shown for anterior and posterior placentae in Figure 2. Using only the ultrasound findings that were available at 32, 34 and 36 weeks' gestation, we found the same cut‐off values for anteriorly and posteriorly located placentae.
Figure 1.
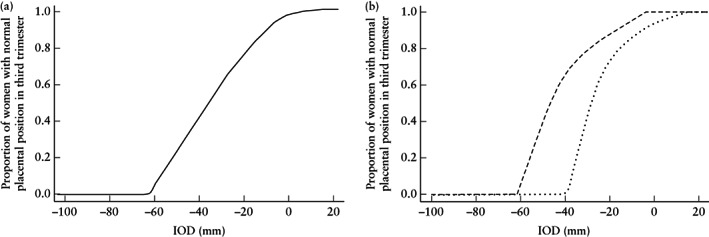
Association between distance from placental edge to internal os (IOD) in second trimester, in women with low‐positioned placenta, and proportion of women with normal placental position in third trimester, in whole cohort (a) and in those with anterior ( ) or posterior (
) or posterior ( ) placenta (b).
) placenta (b).
Table 3.
Multilevel likelihood ratios (LR) for abnormal third‐trimester placental position for different ranges of distance between internal os and placental edge (IOD) in second trimester
| Third‐trimester placental position | |||
|---|---|---|---|
| IOD range | Abnormal (n) | Normal (n) | LR |
| Anterior placenta | |||
| –100 to < –40 mm | 3 | 3 | 35 |
| –40 to < –25 mm | 3 | 5 | 21 |
| –25 to < –4.5 mm | 4 | 36 | 3.9 |
| –4.5 to < 0 mm | 0 | 14 | 0 |
| 0 to < 5 mm | 0 | 84 | 0 |
| 5 to < 10 mm | 0 | 74 | 0 |
| 10 to < 15.5 mm | 0 | 88 | 0 |
| 15.5 to < 20 mm | 0 | 50 | 0 |
| Total | 10 | 354 | — |
| Posterior placenta | |||
| –100 to < –40 mm | 7 | 0 | ∞ |
| –40 to < –25 mm | 3 | 6 | 7.3 |
| –25 to < –15 mm | 9 | 24 | 5.4 |
| –15 to < –4.5 mm | 5 | 41 | 1.8 |
| –4.5 to < 5 mm | 6 | 142 | 0.6 |
| 5 to < 10 mm | 4 | 121 | 0.5 |
| 10 to < 15.5 mm | 4 | 128 | 0.4 |
| 15.5 to < 20 mm | 0 | 94 | 0 |
| Total | 38 | 556 | — |
Figure 2.
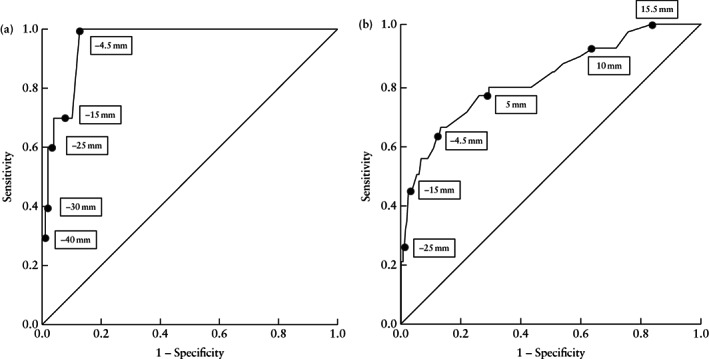
Receiver‐operating‐characteristics curves for distance from placental edge to internal os (IOD) in second trimester in prediction of abnormal third‐trimester placental position, in women with anterior (a) or posterior (b) low‐positioned placenta. Slope of tangent at cut‐off points (boxes) gives likelihood ratio for that value of IOD.
Delivery
Data on delivery were available for 820 women. Attempted vaginal delivery was successful in 677 women, 20 women had a scheduled Cesarean delivery owing to placenta previa and five women had a scheduled Cesarean delivery owing to vasa previa. Cesarean delivery was performed in 118 women for obstetric reasons other than a low‐lying placenta, such as a previous Cesarean section, breech presentation, non‐progressive labor or fetal distress. One woman had unexplained extensive blood loss during induction of labor with a Foley catheter for which a Cesarean delivery was indicated, but during Cesarean section no sign of a low‐positioned placenta was seen.
DISCUSSION
In our cohort, a low‐positioned placenta in the second trimester was located more frequently on the posterior side than on the anterior side. There was a higher incidence of low‐lying placenta than of placenta previa in the second trimester. Only 5% of women with a low‐positioned placenta in the second trimester had an abnormally located placenta in the third trimester. Women with placenta previa, a posteriorly located placenta or a previous Cesarean section were at higher risk of having an abnormally located placenta in the third trimester.
To our knowledge, this is one of the largest prospective cohort studies assessing re‐evaluation of a low‐positioned placenta. Our hospital is a tertiary referral center for pregnant women, but also serves as a regional ultrasound center for uncomplicated pregnancies. Therefore, women in primary, secondary and tertiary care were included. In addition, by collecting data prospectively, we reduced the chance of selection bias. Therefore, our cohort is likely to be representative of the general population without overestimation of the incidence of a low‐positioned placenta. Nevertheless, some limitations should be discussed. As in every cohort, there was loss to follow‐up, which was mostly due to follow‐up of the patients outside our hospital. Since this was less than 10% of the cohort, we consider it to be acceptable given the size of our cohort. However, these women might have had a persisting low‐positioned placenta in the third trimester, which could have resulted in over‐ or underestimation in our results.
Our findings are consistent with those of a recent study that examined resolution of a low‐positioned placenta in 1289 women and showed that the probability of resolution is inversely proportional to IOD. Resolution was noted in 99.5% of women with an IOD of 10–20 mm, in 95.4% with an IOD of 0.1–10 mm and in 72.3% with placenta previa 7 . The higher percentage of normal third‐trimester placental location in cases of a second‐trimester low‐lying placenta compared with that of placenta previa might be due to trophotropism. This is a process of atrophy of the thin placental margins due to a poor vascular supply in the lower uterine segment, while other placental regions continue to grow and migrate towards sites with a higher vascular density in the fundal region of the uterus. In contrast to the lower uterine segment, which has a thinner muscular wall and lower vascular supply, the cervix establishes an improved blood supply, which makes atrophy of the placental margin less likely to occur in placenta previa than in a low‐lying placenta 12 . The higher rate of persistence of placentae on the posterior side than on the anterior side found in our cohort has also been described by others 7 , 12 , 13 . This might be associated with dynamic placentation, in which the anterior uterine wall expands more than the posterior wall. Since the uterus grows gradually by elongation and hypertrophy during pregnancy, the lower uterine segment will lengthen 14 . Consequently, the placenta moves away from the internal cervical os, with migration of the lowest margin of the placenta towards the fundus. In addition to a higher incidence of migration, anteriorly located placentae may have a better prognosis, with lower incidences of Cesarean section, premature delivery and vaginal spotting during pregnancy 12 . In contrast, another study found a higher rate of normal placental location in the third trimester for posteriorly located placentae, although the obstetric and neonatal outcomes in this cohort were similar for the two placental sides 15 .
Most guidelines recommend re‐evaluation of the placental location in the third trimester. Within the current recommendations, anteriorly and posteriorly low‐positioned placentae are considered as one group, despite placental side having a significant effect on migration. We thus suggest using different cut‐off values for anteriorly and posteriorly located placentae, as this can better identify women with a persisting low‐positioned placenta. Our results show that, in posteriorly located placentae, an IOD of 15.5 mm in the second trimester is associated with a negligible risk for placenta previa or low‐lying placenta in the third trimester. In contrast, for anteriorly located placentae, even one covering the internal os of the cervix by up to 4.5 mm in the second trimester is likely to resolve by the third trimester. Using these cut‐off values, the number of unnecessary follow‐up ultrasound examinations could be substantially decreased, notwithstanding the current advice to rescan all women with a low‐positioned placenta.
However, these cut‐offs were data‐driven and thus optimal for our cohort, but they may not apply perfectly to other populations. In addition, owing to trophotropism of placental tissue, placenta previa is a known risk factor for vasa previa 4 . While atrophy causes low‐lying placental tissue to vanish, the vessels may persist and vasa previa could occur. Therefore, we recommend that all women with placenta previa in the second trimester be re‐evaluated by TVS in the third trimester.
In conclusion, based on our findings, we advise that IOD cut‐off values should be adjusted for re‐evaluation of an anterior low‐lying placenta, but all women with placenta previa should be followed up and, as our cut‐off values were data driven, a safety margin of 5 mm should be applied. We suggest that the cut‐off for posteriorly located placentae remains as it is, namely 20 mm. For anteriorly located placentae, we suggest that the cut‐off value be lowered to 5 mm. Placenta previa or a low‐lying placenta on the anterior side of the uterus increases the risk of placenta accreta in women with a previous Cesarean section 16 . Therefore, we advise that all such women with a placenta reaching or overlapping the Cesarean scar area should be followed up in order not to miss any cases of abnormally invasive placenta. Our suggested approach may reduce unnecessary follow‐up visits, the psychological burden for the women involved and the financial burden for the healthcare system.
Disclosure
B.W. Mol is supported by a NHMRC Practitioner Fellowship (GNT1082548); B.W. Mol reports consultancy for ObsEva, Merck, Merck KGaA and Guerbet; the remaining authors report no conflict of interest.
A video abstract of this article is available online here.
REFERENCES
- 1. Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R. Maternal complications with placenta previa. Am J Perinatol 2000; 17: 101–105. [DOI] [PubMed] [Google Scholar]
- 2. Iyasu S, Saftlas AK, Rowley DL, Koonin LM, Lawson HW, Atrash HK. The epidemiology of placenta previa in the United States, 1979 through 1987. Am J Obstet Gynecol 1993; 168: 1424–1429. [DOI] [PubMed] [Google Scholar]
- 3. Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol 2003; 188: 275–281. [DOI] [PubMed] [Google Scholar]
- 4. Ruiter L, Kok N, Limpens J, Derks JB, de Graaf IM, Mol B, Pajkrt E. Incidence of and risk indicators for vasa praevia: a systematic review. BJOG 2016; 123: 1278–1287. [DOI] [PubMed] [Google Scholar]
- 5. Reddy UM, Abuhamad AZ, Levine D, Saade GR; Fetal Imaging Workshop Invited Participants. Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal–Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound Fetal Imaging workshop. Obstet Gynecol 2014; 123: 1070–1082. [DOI] [PubMed] [Google Scholar]
- 6. Oppenheimer L, Maternal Fetal Medicine Committee. Diagnosis and management of placenta previa. J Obstet Gynaecol Can 2007; 29: 261–266. [DOI] [PubMed] [Google Scholar]
- 7. Durst JK, Tuuli MG, Temming LA, Hamilton O, Dicke JM. Resolution of a Low‐Lying Placenta and Placenta Previa Diagnosed at the Midtrimester Anatomy Scan. J Ultrasound Med 2018; 37: 2011–2019. [DOI] [PubMed] [Google Scholar]
- 8. McClure N, Dornal JC. Early identification of placenta praevia. Br J Obstet Gynaecol 1990; 97: 959–961. [DOI] [PubMed] [Google Scholar]
- 9. Jansen CHJR, Kleinrouweler CE, van Leeuwen L, Ruiter L, Limpens J, van Wely M, Mol BW, Pajkrt E. Final outcome of a second trimester low‐positioned placenta: a systematic review and meta‐analysis. Eur J Obstet Gynecol Reprod Biol 2019; 240: 197–204. [DOI] [PubMed] [Google Scholar]
- 10. Silver R, Depp R, Sabbagha RE, Dooley SL, Socol ML, Tamura RK. Placenta previa: aggressive expectant management. Am J Obstet Gynecol 1984; 150: 15–22. [DOI] [PubMed] [Google Scholar]
- 11. Haynes BR, Sackett DL, Guyatt GH, Tugwell P. Clinical Epidemiology: How to do clinical practice research (3rd edn). Lippincott Williams & Wilkins: Philadelphia, PA, 2006. [Google Scholar]
- 12. Cho JY, Lee YH, Moon MH, Lee JH. Difference in migration of placenta according to the location and type of placenta previa. J Clin Ultrasound 2008; 36: 79–84. [DOI] [PubMed] [Google Scholar]
- 13. Pradhan S, Tuladhar A, Shrestha A, Amatya NB, Pradhan P. Sonographic assessment of placental migration in second trimester low lying placenta. Nepal Med Coll J 2012; 14: 331–333. [PubMed] [Google Scholar]
- 14. Sand H. Ultrasonic diagnosis of placenta praevia. Acta Obstet Gynecol Scand 1977; 56: 109–113. [DOI] [PubMed] [Google Scholar]
- 15. Feng Y, Li X‐Y, Xiao J, Li W, Liu J, Zeng X, Chen X, Chen K‐Y, Fan L, Chen S‐H. Relationship between placenta location and resolution of second trimester placenta previa. J Huazhong Univ Sci Technolog Med Sci 2017; 37: 390–394. [DOI] [PubMed] [Google Scholar]
- 16. Hull AD, Moore TR. Multiple repeat cesareans and the threat of placenta accreta: incidence, diagnosis, management. Clin Perinatol 2011; 38: 285–296. [DOI] [PubMed] [Google Scholar]


