Abstract
Purpose:
To review enrollment strategies, participation barriers, and program reach of a large, 2-year workplace intervention targeting sedentary behavior.
Approach:
Cross-sectional, retrospective review.
Setting:
Twenty-four worksites balanced across academic, industry, and government sectors in Minneapolis/Saint Paul (Minnesota) and Phoenix (Arizona) regions.
Participants:
Full-time (≥30+ h/wk), sedentary office workers.
Methods:
Reach was calculated as the proportion of eligible employees who enrolled in the intervention ([N enrolled/(proportion of eligible employees × N total employees)] × 100). Mean (1 standard deviation) and median worksite sizes were calculated at each enrollment step. Participation barriers and modifications were recorded by the research team. A survey was sent to a subset of nonparticipants (N = 57), and thematic analyses were conducted to examine reasons for nonparticipation, positive impacts, and negative experiences.
Results:
Employer reach was 65% (56 worksites invited to participate; 66% eligible of 56 responses; 24 enrolled). Employee reach was 58% (1317 invited to participate, 83% eligible of 906 responses; 632 enrolled). Postrandomization, on average, 59% (15%) of the worksites participated. Eighteen modifications were developed to overcome participant-, context-, and research-related participation barriers.
Conclusion:
A high proportion of worksites and employees approached to participate in a sedentary behavior reduction intervention engaged in the study. Interventions that provide flexible enrollment, graded participant engagement options, and adopt a participant-centered approach may facilitate workplace intervention success.
Keywords: sedentary behavior, workplace, reach, participation barriers, employee engagement
Purpose
Sedentary behavior (ie, any waking behavior in a seated or reclining posture at <1.5 metabolic equivalents)1 is now recognized as a unique health risk factor for cardiometabolic diseases and early mortality.2-6 Desk-based workers are at particular risk as they spend 70% to 80% of their workday sitting at a desk.7 Designing efficacious and feasible sedentary behavior reduction strategies targeting the workplace is of public health interest and several large-scale cluster randomized controlled trials (RCTs) are being conducted within workplace settings specifically targeting sedentary behavior reduction.8-10 However, many workplace health promotion studies report low participation rates11 and problems with dissemination and sustainability associated with the workplace environment.12 While it is understood that scientific rigor is necessary for researchers to design efficacious interventions, this does not necessarily equate to worksite adoption of effective interventions and high levels of employee participation.
Cluster RCTs are considered the gold standard research design for multigroup trials, in which an intervention is likely to be implemented at the group level (e.g., workplaces).13 These trials are often complex to implement and unanticipated difficulties are likely, particularly during the enrollment phase, which could provide useful insights for future dissemination efforts.14,15 Therefore, researchers are now encouraged to include evaluations of their enrollment strategies to inform future work in similar trials and increase the likelihood of dissemination.14 Further, when focusing on the reach of a given intervention (i.e., the proportion of eligible employees who engage in the intervention), others have suggested the need to report information on the target population, intervention focus, research design, and enrollment strategies to assess potential public health impact.16 To best understand the public health impact of these approaches, it is necessary to understand the reach, in addition to effectiveness, of different strategies.17 Particularly in workplace settings, practitioners may benefit from efficacy and effectiveness measures of reach to serve as a minimum participation benchmark for the dissemination of evidence-based health initiatives. Detailed documentation of enrollment processes and their reach may therefore provide a resource for establishing more realistic participation metrics to better manage employer expectations regarding perceived intervention success. Despite this, limited evidence exists regarding the enrollment processes and participation barriers experienced within ongoing workplace efficacy trials targeting sedentary behavior reduction.
There is an opportunity and need to evaluate the enrollment process, participation barriers experienced, and associated reach of a large workplace intervention during the efficacy stage to inform future dissemination efforts. In response to this need, we describe the planned 2-level (worksite; employee) enrollment process utilized in a large cluster RCT—Stand & Move@Work (NCT02566317). This multicomponent intervention to reduce sedentary behavior in the workplace had 2 participation goals: one at the worksite (cluster) and one at the employee (individual) level. We further describe the target population of worksites and employees that could benefit from, and engaged in, Stand & Move@Work (worksite and employee reach) while concurrently identifying barriers to participation and resultant modifications to overcome these barriers.15,18 Finally, we examine survey feedback from individuals who chose not to participate and posit recommendations to maximize translation from efficacy to effectiveness and dissemination of workplace health interventions.
Methods
The intervention design was a 2-year, 2-arm group randomized trial, with a recruitment goal of 24 worksites of small to moderate size (20-50 employees enrolled) and 720 participants balanced across 2 regions, Phoenix (Arizona) and Minneapolis (Minnesota), and 3 sectors, academic, industry, and government. Worksite size and resultant enrollment targets were informed by statistical power analyses to maintain scientific rigor of the cluster RCT. All worksites were randomized to 1 of 2 interventions: (1) MOVE+, a multilevel behavioral intervention targeting increases in light-intensity physical activity (LPA) at the worksite or (2) STAND+, the multilevel MOVE+ intervention along with the installation of sit–stand workstations to allow workers to stand at their desks while working. In cluster trials, selection bias can be introduced if participants are recruited after the clusters have been randomly allocated.13,19 To negate this bias, it was imperative that all worksites were randomized after the baseline assessment data were collected.
Worksite Enrollment
A staggered enrollment approach was chosen to account for potential confounders such as seasonal effects and to alleviate staffing and resource burden. This was also chosen to maximize the time between the first initiation of contact with a worksite and consent. It was anticipated that we would complete the first baseline assessments for 4 worksites in January 2016, pairing worksites by sector in each region. As such, we planned to start initial recruitment activity in August 2015. All worksites were to be recruited in pairs, per region, every other month (March, May, July, September, and November) until all 24 worksites were enrolled.
Another complexity included the decision to enroll 8 worksites across 3 sectors: academia, industry, and government. Across all 3 sectors, worksite eligibility criteria included the following: (1) worksites of small to moderate size (ie, 20-50 employees), (2) >80% of employees working full time in the office (30+ h/wk), (3) predominant worksite occupation being seated office work with little movement or walking (ie, computer or telephone-based work), (4) not currently undergoing a wellness program aimed at reducing sitting or increasing LPA at work, (5) <10% of employees currently using a sit–stand workstation at work, (6) willing to have sit–stand workstations installed at the workplace, and (7) worksite leadership willing to be randomized to either intervention arm. To minimize the potential for contamination across worksites, we planned to recruit relatively isolated units, with minimal physical interaction with other worksites. The aim was to begin the enrollment process as early as possible and to communicate the anticipated start date early on (based on desired timeline). Worksite enrollment was categorized into 3 main steps which utilized a combination of both active (in-person, over the phone) and passive (flyers, e-mail, surveys) techniques identified in the process flow diagram (Figure 1).
Figure 1.
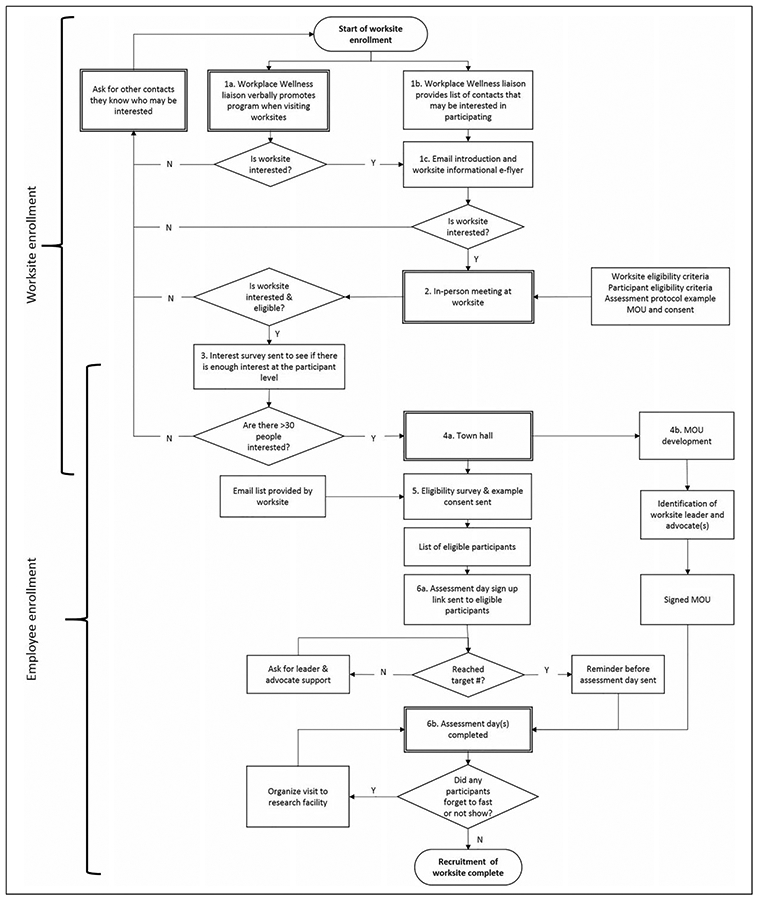
Intended 2-phase enrollment process flow diagram with active (double line rectangles) and passive (single line rectangles) strategies.
Step 1: Initial contact.
The first step was to establish contact with worksites that were potentially eligible to participate. The preferred method of initial contact was led by a workplace wellness liaison established in each region, who already had contact with workplace leaders. These liaisons either delivered intervention information in person when visiting the worksite or through conversational e-mail correspondence (Figure 1A). For organizational contacts with whom liaisons had no personal relationship, a list of potential contacts was forwarded to the researchers to contact directly (Figure 1B). Regardless of the initial contact method, if there was interest from the worksite, an e-mail introduction was sent to formally connect the worksite and researchers (Figure 1C).
Step 2: In-person meeting.
The next step was an in-person meeting with representatives of the worksites who expressed interest in the intervention, including the main intervention contact (ie, leader) and higher level management (if necessary). Documents to explain the timeline, worksite and employee eligibility, an example Memorandum of Understanding (MOU), the planned recruitment and consent process, and the assessment protocol were reviewed. The development of an informal MOU was undertaken in order to clearly state the roles of both the research staff and the participating worksite.20 For larger organizations (with several departments or locations), leaders were invited to identify individual workgroup(s) that may be most suited to the intervention. The meeting also facilitated a brief examination of the current worksite environment and whether it was conducive to sit–stand workstation installation.
Step 3: Establish worksite interest and eligibility.
Step 3 included the distribution of an interest survey designed and administered via Qualtrics (Salt Lake City, Utah) to determine the overall worksite interest. The 7-item questionnaire provided a link to additional intervention information and focused on pragmatic issues that may affect the overall worksite eligibility (eg, number of monitors at the desk, number of hours worked per week, having a sedentary job). Although similar to the participant eligibility survey, the intention was to identify early on whether the worksite had enough interested and eligible participants. As an anonymous survey, this was sent by the leader (alongside a supportive e-mail template provided by the research team) to the area(s) of interest. If the results indicated high interest (≥25 interested employees) in several areas, either 1 or 2 distinct areas were chosen to participate and an MOU drafted. If no areas showed high levels of interest, enrollment was terminated.
Employee Enrollment
The remaining 3 steps (4-6) focused on the transition from worksite to employee enrollment. Participant eligibility criteria included the following: (1)18 years or older, (2) generally good health and able to safely reduce sitting and increase LPA, (3) working full time on-site (ie, 30+ hours and at least 4 days in the office per week), (4) not currently pregnant, (5) predominant worksite occupation being seated office work, (6) not currently using a sit–stand workstation at their work desk location, (7) willing to have a sit–stand workstation installed at their desk, and (8) willing to be randomized to either intervention arm. Similar to the worksite (cluster) phase, both active and passive strategies were employed; however, additional support from designated worksite advocates (both in person and via e-mail) was encouraged. Prior to commencing step 4, research staff confirmed both the official number and e-mail addresses of each worksite’s eligible employees, which served as the number of employees screened at each worksite. This final employee list was occasionally identical to the list provided in step 3.
Step 4: Town hall.
The purpose of the town hall was to provide an open forum for all employees to attend. This was an opportunity to communicate the research background, research objectives, and specific participation requirements and to answer any additional employer and employee questions. The town hall(s) took place at the worksite, at a time and date selected by the leaders(s) to maximize employee attendance. Generally, either 1 or 2 individual town hall sessions were scheduled at each worksite. The 15- to 20-minute presentation was designed by all members of the research team, which included worksite health and wellness experts to ensure content was suited to the audience. The principal investigator delivered the presentation and allowed 10 to 15 minutes for questions.
Step 5: Determine employee eligibility.
Immediately after the town hall(s), employees were sent the Participant Eligibility Survey via Qualtrics to complete via self-report; up to 2 completion reminders were sent to nonrespondents. As a passive strategy, regular data reviews and examination/follow-up of incomplete responses were required. Participants were notified if they were deemed eligible or ineligible.
Step 6: Sign up distribution and completion.
The dates, times, and locations of all baseline assessment visits were approved and confirmed by necessary worksite leaders. Participants deemed eligible were invited to a 30-minute baseline assessment at their worksite and nonresponders were sent 2 reminders by e-mail and/or phone. An attempt was made to schedule all assessments at each worksite over 1 or 2 days for research convenience. Alternative assessment times were available as required (eg, coming to the research laboratory, attending a visit at a different worksite).
Feedback From Individuals Who Declined to Participate in the Trial
Using the e-mail lists provided prior to step 4, those who chose not to participate were invited to complete an evaluation survey at the 12-month time point (via Qualtrics). Three open-ended questions related to participation were asked: (1) What were your main reasons for not participating in the program?, (2) In what ways, if any, did the program positively impact you?, and (3) In what ways, if any, did the program negatively impact you? Only responses collected to date (12/24 worksites; n responses = 57) were included in this analysis.
Data Analyses
Reach was calculated as the proportion of eligible employees who enrolled in the intervention ([N enrolled/(proportion of eligible employees × N total employees)] × 100).21 Mean (1 standard deviation) and median worksite sizes were calculated at each recruitment step. Using the total number of employees per worksite as the denominator, percentages of participants who fell into each of the following categories were calculated: those who (1) did not complete the eligibility survey, (2) were found to be ineligible, (3) were eligible but did not enroll, and (4) who successfully completed baseline assessments and were randomized. Weekly recruitment meetings were attended by all members of the research team for 1 year (November 2015 to November 2016) to monitor ongoing enrollment progress and facilitate troubleshooting where necessary. Meeting notes and enrollment decisions were documented throughout. A retrospective review of the meeting notes and enrollment decisions per worksite was conducted by 2 members of the research team (Arizona—S.L.M. and Minnesota—S.A.R.) who coordinated recruitment across both regions and had an advanced understanding and recollection of the experiences per worksite. This review included (1) identification of participation barriers and (2) identification of the modifications made to overcome these barriers and maximize participation.
Thematic Analyses of Data from Individuals Who Declined to Participation in the Intervention
Thematic analysis was conducted using NVivo qualitative data analysis software (version 11; QSR International Pty Ltd, Burlington, MA, USA). An inductive (bottom-up) thematic analysis approach was used to code all responses and derive themes from nonparticipant experiences. Therefore, a review of all responses was conducted before nodes were created. All responses were coded and classified within 1 or more node(s). Deductive techniques were used iteratively to reduce all constructs into main themes and subthemes, while ensuring that all nodes were categorized.22
Results
An overview of the participant-, context-, and research-related participation barriers and the resultant modifications per enrollment step is presented in Table 1. A chronological overview of the enrolled worksites per sector is provided in Figure 2. A total of 56 worksites (Arizona = 26, Minnesota = 30) were asked to participate in the Stand & Move@Work intervention. Worksite reach was 65% (56 worksites invited to participate; 66% eligible of 56 responses; 24 enrolled). The worksite participation goal was reached within the proposed deadline, with 4 worksites enrolled every other month (January to November 2016), and balanced across each sector (8 per sector).
Table 1.
The Participant-Related (P), Context-Related (C), and Research-Related (R) Barriers Experienced and Modifications Required During Each Step of the 2-Phase Enrollment Strategy.
| Barriers | Modifications | |
|---|---|---|
| Process flow step 1 | ||
| Initial contact with worksite | List of worksite contacts provided by the wellness liaison were exhausted, still needed to enroll 4 remaining worksites. (R) (C) | 1. A review of local businesses was conducted to identify any potential worksites in the required sector. Researcher-led phone calls and e-mails were implemented: “cold-calling.” Informational flyers were delivered in-person to local worksites. Enrolled worksites were also asked to share any contacts they thought may be interested. |
| Process flow step 2 | ||
| Follow-up with worksite | Those who were originally contacted were not always the follow-up person, this led to inaccurate information being passed along; that is, everyone receives a sit–stand desk immediately. (C) | 2. Phone call with researcher prior to meeting in person to ensure the fundamental aspects of the study were understood. |
| Communicating the complexity of the study and program, several items or details discussed in person would not be fully understood or remembered. Similarly, expecting the leaders to know what questions to ask and that all information discussed in the meeting would be retained. (R) | 3. Following up in-person meetings with e-mail communication documenting all the major points of discussion. This ensured all correct processes were followed and communication was consistent. We developed e-mail templates that consistently outlined major study aspects. | |
| Process flow step 3 | ||
| Establish number of worksites and worksite eligibility | This interest survey was only useful when there were several worksites available. Tended to confuse participants—made them feel as though they had already signed up for the study. (C) (R) | 4. Selective use of the interest survey—more useful for large organizations with several potential worksites and clarifying language to differentiate between the interest and eligibility survey. Leaders were asked to send the survey link in cases where e-mail addresses could not be released. |
| Process flow step 4 | ||
| Begin individual-level enrollment | Unable to organize time for all employees to be available for a own hall. Particularly challenging in call center environment. Concern that people who missed it would be prematurely excluded. (C) (P) | 5. Creation of an “E-town hall”—a presentation sent via e-mail with audio to explain the study. People could listen to the town hall at their own pace at a convenient time. |
| Communicating the complexity of the study at the individual level, ensuring that the correct information was being communicated by leaders. (P) (R) | 6. E-mail templates that consistently outlined major study aspects and assessment requirements were developed. | |
| Some worksites required additional approval from their own IRB or legal departments—this inhibited the individual recruitment processes and reduced either town hall or e-town hall/drop-in session lead time significantly. (R) (C) | 7. Maintained regular contact with the leader(s) to ensure all information could be distributed once approved. Processes 4 to 6 were collapsed to occur in a short time frame. Communication included the E-town hall, eligibility survey, and sign-up link. People were further encouraged to sign up on the day – more time was allocated to the consent process. | |
| Slow MOU development and approval—often a repercussion of IRB or additional approval delays. (R) (C) | 8. A larger emphasis was placed on establishing the types of approvals required and by whom during the initial contact phase. Reiteration that the MOU was an informal agreement. Processes 4 to 6 were collapsed to occur in a short time frame where necessary. | |
| Process flow step 5 | ||
| Determine participant eligibility | Some worksites were unable to share e-mail list until people had officially enrolled and consented. (C) | 9. Survey was sent by the leader and the eligibility survey was adjusted to collect required information. |
| Not everyone wanted to watch the E-town hall, easy to overlook. Cannot ask questions in person to clarify eligibility. (P) | 10. Drop-in sessions were arranged at the worksite. Two research team members had a designated area for approximately 1 hour. People were invited to visit during that time to discuss the study, their eligibility, and ask any questions. | |
| White-listing issues. (C) | 11. All survey links were sent to the worksite following step 2, to ensure that step 3 and remaining surveys would be accessible. | |
| Participants misread eligibility statements. (P) | 12. Reduction of e-mail communication and thorough checking of responses. Follow up with ineligible participants to ensure they were ineligible. | |
| Process flow step 6 | ||
| Encourage people to sign up and complete the assessment day | Late identification of leader and advocate, delayed encouragement from leadership. (C) | 13. Prepared to have people sign up on the day of assessment day—spare participant pack and activPALs prepared. Researchers spent longer with these participants to explain the study. |
| Building access/logistics. (C) | 14. Facilities contact provided during initial contact phase. | |
| People forgetting fast. (P) | 15. Assessment mornings were moved from Mondays and Tuesday mornings, to Tuesday and Wednesday mornings as reminder sent on Friday or Sunday evening were ineffective and people were more likely to forget. | |
| 16. Addition of an e-mail reminder (sent between 5 and 5:30 am) the morning of the assessment to remind people to fast. | ||
| 17. Addition of a backup blood draw day(s) at the worksite if necessary. | ||
| People not wanting to do the blood draw but wanting to take part in the study. (P) | 18. Explanation of the study goals and cardiometabolic markers as a secondary outcome. If the blood draw was the only element deterring a person from participating, we did not collect their blood. |
Abbreviations: IRB, institutional review board; MOU, Memorandum of Understanding.
Figure 2.
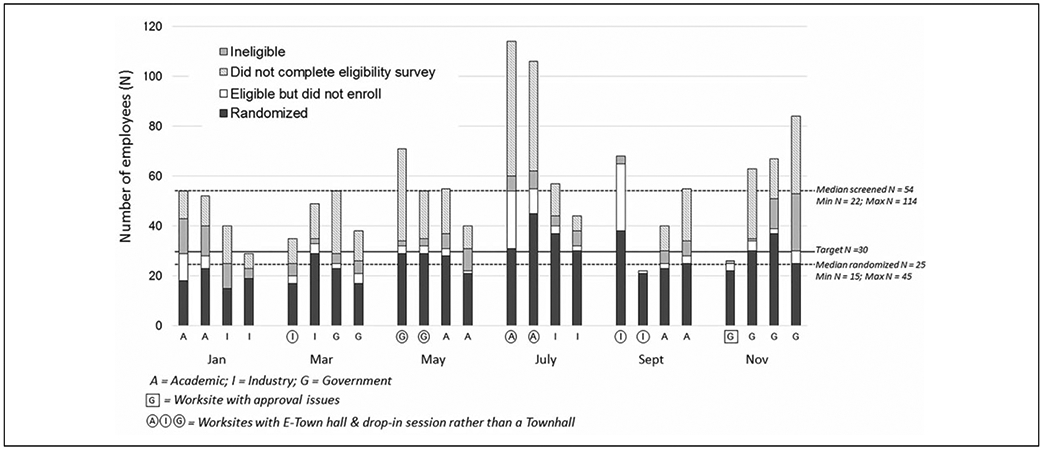
Stacked bar graphs indicating the total number of employees per worksite and the corresponding proportion of employees who did not respond to the eligibility survey, were ineligible, were eligible but did not enroll, and were randomized per worksite.
Step 1 results: Overall, 63% of worksites were initially contacted by a wellness liaison. Contrary to the original enrollment plan, the remaining 37% of worksites were initially contacted by members of the research team without wellness liaison support (Table 1, modification 1). Research staff reached out to these potential sites via personal networks or through cold calling. Following initial contact, 7% of worksites were not interested due to the anticipated time commitment and 34% were ineligible and therefore did not progress to the second recruitment step.
Step 2 results: Following the in-person meeting, 27% no longer wished to participate. Two modifications were developed to improve the researcher–leader communication early in the recruitment process (Table 1, modifications 2 and 3).
Step 3 results: Of those that progressed, 72% distributed an interest survey, while 28% continued straight to step 4. Of note, only 1 worksite was deemed ineligible following the interest survey. The main modification at this stage pertained to the use of the interest survey (Table 1, modification 4).
Step 4 results: All worksites that reached step 4 were officially enrolled in the intervention. The mean size of the worksites screened and enrolled during cluster recruitment was 55 (22). Of the 24 enrolled worksites, 67% were initially contacted by a wellness liaison and 33% were initially contacted by a research team member. Four modifications were developed to increase the flexibility of the employee enrollment process and to improve researcher–participant communication (Table 1, modifications 5-8).
Step 5 results: Ultimately, a total of 1317 employees were screened for eligibility, of which 756 were deemed eligible (see Figure 2). Of the total screened, the mean percentage of employees who did not complete the eligibility survey was 28% (14%), while of those who did complete the survey, 12% (8%) were ineligible. Of those who were eligible, on average, 8% (8%) chose not to proceed to step 6 (ie, sign up for the baseline assessment). Another 4 modifications were developed to reduce participant burden (Table 1, modifications 9-12).
Step 6 results: Employee reach was 58% (1317 invited to participate, 83% eligible of 906 responses; 632 enrolled) to achieve 88% of the participation goal. Mean worksite size was 26 (8), which represented 52% (16%) of the total worksite. The largest number of modifications was required at this stage (Table 1, modifications 13-18). Five worksites yielded <70% of the employee participation target, 6 worksites yielded 70% to 80%, 6 yielded >80% to 97%, and 7 yielded ≥100% (see Figure 2).
Feedback From Individuals Who Declined to Participate in the Intervention
Out of the 293 individuals invited to complete this survey, 57 responses were received. The primary themes cited for nonparticipation included the fact they were ineligible, foreseen conflicts with the intervention design or measures, or missed the sign-up opportunity (see Table 2). The positive impact themes that were reported included individual behavior change, culture change within the organization, and benefits from the e-newsletters that were sent to the entire worksite. While a number of nonparticipants reported no negative impact, those who did reported 2 primary themes including that the intervention may be distracting and exclusive.
Table 2.
Thematic Coding of Nonparticipant Survey Responses Using NVivo (N = 57).
| Why Did They Not Participate? | Positive Impacts | Negative Impacts | |
|---|---|---|---|
| Theme 1 | Ineligibility | Behavior change | Exclusivity |
| “I actually wanted to participate but I was not able to because I had already been using a standing desk.” | “It gave me a good reason to take long walks when time permits.” | “Didn’t get a standing desk, yet was the one who wanted it to begin with.” | |
| “Medical issues related to standing.” | “I now set a reminder—once in the morning and once in the afternoon to stretch” | “We were upset that we never got one.” | |
| “My job has me constantly moving, climbing, packing, and lifting.” | “Learning about small ways to improve fitness that I implemented.” | ||
| “My department was not allowed to participate. I wanted to.” | |||
| “Not interested in a standing desk.” | |||
| Theme 2 | Study design and measures | Culture change | Distraction |
| “The length of the study was daunting—1+ years is a long time.” | “I appreciate how the program has changed the culture around here about standing during meetings and has encouraged people to take stand and move break.” | “Our seating is not private enough and I think it would be too much of a distraction.” | |
| “The requirements of the blood draw and monitoring device.” “I don’t like needles.” | “It was nice to see the inspirational signs and reminders, suggestions to get up and move, permissions to stand in meetings, and just generally feeling like it was ok to be away from your desk for 10-15 minutes walking and moving.” | “Sometimes the signs and reminders were a bit excessive but only when I was already feeling super busy or behind on work load. It was hard to see those signs and realize that your day wasn’t going to allow for any free time. Added to the stress.” | |
| “Too time consuming.” | “It engaged my coworkers and encouraged more active meetings.” | ||
| Theme 3 | Missed opportunity | E-newsletters | No negative impact |
| “I missed the several initial meetings organized by ASU due to time conflict. I am interested in taking part in another cohort if you are planning to take second cohort.” | “I liked receiving the informational emails about chair and computer positioning as well as tips to stand and move more.” | “The program did not negatively impact me.” None.” “N/A” | |
| “Forgot to sign up for it, wanted to, just spaced it.” | “The e-mails sent to me have provided knowledge and useful tips.” |
Discussion
This retrospective review elicited insights regarding reach, and participation barriers faced, at both the worksite and employee levels (Table 1 and Figure 2). Additionally, we gained useful insights from the nonparticipant survey data (Table 2). We discuss our results in the context of recommendations for future workplace intervention recruitment strategies to maximize dissemination and participation.
Increasing Worksite Size
Results indicated that worksite enrollment was highly successful (100%) meeting both timeline and participation targets. Employee participation was high (88%), with all participants enrolled within the original timeline. However, the worksite (65%) and employee reach (58%) and percentage of employees successfully randomized per worksite (59% [15%]) suggest that researchers should plan to screen approximately 40% more than the intended number of worksites and enroll worksites approximately double the size of the target worksite size. Interestingly, screening larger worksites (N ≥ 80) did not necessarily equate to a relative increase in the number of participants enrolled (see Figure 2). Overall, the results suggested that our worksite eligibility criteria (20-50 employees) may have been too low and that a worksite size of ~60 to 70 employees may be more likely to have yielded the desired individual participation target (N = 30 per site).
The Importance of Timing Within Sectors
Our research team intentionally set a lower worksite target size for January to refine all processes, which elicited the lowest mean worksite size (19 [3]). The aim was to increase the worksite size each recruitment month; however, recruitment peaked in July (36 [7]). Although no obvious recruitment patterns were observed by sector, we posit that fluctuations in employee receptivity may be attributed to timing and known busy periods within each sector. For example, during September, recruitment in the academic sector coincided with the start of the academic calendar term and heavy enrollment periods, further contributing to the decrease in mean worksite size (27 [8]). Temporal influences may be further amplified by departmental duties and job type (eg, a human resources advisor at the end of the tax year). Our experiences are aligned with previous research highlighting the need to design strategies that maximize participant convenience.23,24 We posit that the impact of deadlines and “busyness” within the worksite environment may have significant implications on employee receptivity and perceived convenience. We suggest that researchers should address the issue of “timing” early in the enrollment process to avoid known busy periods that may occur monthly, quarterly, biannually, or annually and may vary greatly by sector, department, and job type.
Flexible Participant-Centered Approach
Worksites cannot be considered homogenous environments, as each likely has different organizational structures and cultures.25 Consequently, tailoring strategies to the worksite and employee needs became a priority. As illustrated in Table 1, we modified the recruitment strategy to adopt a more participant-centric approach which aimed to address employee needs while balancing scientific rigor.23 For example, a town hall was not always conducive to the workplace culture. The main barrier was identifying a time and date suitable for all employees to attend simultaneously. Providing the option of an E-town hall with narration and a link to the eligibility survey overcame schedule conflicts and communicated researcher respect for their schedule.24 This was particularly useful in call center–based worksites. Further, as building rapport has been identified as an effective way to improve both recruitment and retention,24 the option of a “drop-in” session (1-hour researcher visit) was given to build rapport with employees.
Improving Researcher–Worksite Communication
Consistency of communication is critical throughout the enrollment process.15 Despite in-depth informational flyers and briefing by the wellness liaison, misconceptions regarding intervention commitments were still evident during the first in-person meeting. As 27% decided not to participate following the meeting, we posit that a phone call to reinforce the intervention-related aspects may have negated an in-person meeting (saving both time and resources) and should be considered for future workplace interventions. Leader feedback also indicated that receiving both an interest survey and eligibility survey confused some employees. Given the abundance of e-mail communication in the workplace,26 there is a risk of overwhelming employees which may impact participation interest. Therefore, in a workplace environment, individual e-mail communication during worksite enrollment should be minimized. Further, an interest survey may better serve as a tool to facilitate leader decision making when several divisions/departments may be eligible.
Communication issues also arose on the assessment day. The most common issues included (1) forgetting the appointment over the weekend and not seeing the reminder e-mail sent on the Friday or Sunday evening, (2) remembering the appointment but forgetting to fast overnight and in the morning in preparation for blood draw, and (3) remembering the appointment and to fast but misunderstanding how strict the term “fasting” was. Although we offered an alternative (visiting the research laboratory), this was often perceived as a barrier given the extra effort required. We suggest that avoiding Monday morning assessments, providing a more detailed description of the term “fasting” across all participant communication, and sending an additional fasting reminder early on the morning of the assessment day may reduce the incidence of these issues.
Reaching worksite and employee participation goals was highly reliant on advocate and leader communication with employees. All worksites meeting the ≥100% participant target had extensive leader and advocate support. However, in real-world workplace settings, a high level of leader or advocate engagement cannot be guaranteed. Research indicates that participants are motivated by altruism, as well as by the opportunity to obtain services designed to address their needs.24 Therefore, particularly during the efficacy stage of evidence based health promotion, we suggest that all means of communication should emphasize being “partners in science,” which further advocates for a participant-centered approach.23 We posit that this may evolve to the communication of more “home-grown” initiatives when reaching dissemination efforts.
Overcoming Unforeseen Events
As with any large trial, not all scenarios can be anticipated. During worksite enrollment, the preferred method of initial contact was exhausted sooner than expected. Although our results indicated that the presence of a wellness liaison to foster initial relationships was most effective, we suggest that leveraging referrals from enrolled worksites early in the enrollment process in addition to ongoing wellness liaison support would be more prudent.
Maintaining best practices and the integrity of the intervention also caused extended MOU development or additional approvals (ie, institutional review board oversight agreements or legal team reviews). In some cases, gaining the required approvals to progress to employee reenrollment hindered progress significantly. As highlighted in Figure 2, unforeseen approval issues prohibited individual contact and elicited a smaller worksite size for screening than originally intended. Approval issues also prevented leaders from promoting the intervention and delayed the identification of advocate(s) to champion the intervention, which impacted compliance to research-related assessments. Establishing lines of approval early in the enrollment process and identifying a second point of contact may prevent approval delays and reduce research-related barriers.15
Graded Participation
The survey results and thematic analyses presented in Table 2 provided several useful insights. First, the most common reason for nonparticipation was “ineligibility.” This indicates that there is continued interest in similar workplace interventions. Interestingly, those who were eligible were mostly deterred by the intervention longevity or blood collection (both research-related barriers). We recommend that researchers recruit based on the primary outcome to alleviate participant concerns where possible (.e, activPAL compliance was communicated as higher priority than blood draw compliance for those who expressed concerns). Another emerging theme for nonparticipation was “missed opportunity” where employees were interested but forgot to sign up, which may be related to the context and associated busyness. This was supported by the number of employees identified in Figure 2 who were eligible but failed to enroll (total N = 124). We posit that this population represents an area for participation improvement and may require (1) additional advocate support to serve as an in-person reminder, (2) more frequent e-mail reminders, or (3) calendar invites.
The survey responses also indicated that positive changes were experienced by nonparticipants. These included (1) individual behavior change (eg, setting personal reminders to stretch/take a walk), (2) workplace cultural change (eg, support for standing meetings, active breaks), and (3) e-newsletters (eg, content that was highly inclusive and applicable to all). These responses suggest that the benefits of similar workplace interventions extend beyond the installation of a sit–stand workstation alone and reinforce the need for multicomponent interventions.
The predominant responses regarding negative impact to nonparticipants pertained to the issue of “exclusivity” and may be attributed to the enrollment process in which worksites were screened but considered ineligible. These responses are again indicative of the high demand for similar workplace interventions. More notable responses included the perceived lack of privacy when colleagues were using their sit–stand workstation (in cubicle environments) and distraction caused by reminders and signage. Although the negative responses were less frequent and most reported “none,” we suggest that providing mechanisms for graded levels of participation (minimal to maximal) may appeal to a wider population and facilitate larger scale dissemination.
It is important to note that our results reflect health promotion efforts at the efficacy stage, within which maintaining scientific rigor was of high priority. Specifically, our results suggest that researchers should plan to screen 40% more than the intended number of worksites and target worksites that are approximately double the size of the intended worksite size. While this is not initially translatable to practitioner enrollment efforts, it is necessary to develop evidence-based interventions that are likely to be implemented by health practitioners. Practitioners may be able to better gauge the likely reach of their dissemination efforts using efficacy and effectiveness measures of reach as benchmarks to establish more realistic participation targets. Furthermore, both researchers and practitioners may benefit from accommodating the heterogeneous nature of workplace environments and acknowledging temporal fluctuations in “busyness,” by providing flexible options throughout the enrollment process (eg, E-Town halls and drop-in sessions). Similarly, when designing for dissemination, researchers and practitioners may wish to consider providing well-defined, graded levels of participation to maximize reach.
Limitations
We acknowledge that our recommendations are only generalizable to highly sedentary office workers within small- to medium-sized worksites at the efficacy stage of intervention design. However, recruiting across 3 sectors required application of the enrollment process across different organizational structures which varied substantially in terms of flexibility and leader support. Further, given the health risks associated with sedentary behavior and identification of the workplace as an opportune intervention setting, there is a distinct need to share our context-specific experiences to inform future workplace interventions. We further acknowledge that research timelines may vary greatly from workplace health promotion programs in practice. Adhering to the timeline was of high priority due to the staggered and paired, long-term enrollment required to maintain scientific rigor. While resource and timeline constraints may vary within research and practice, we feel that maintaining a consistent timeline is paramount within workplace environments, as delays could damage relationships with management and potentially cause worksite attrition. Ultimately, maintaining strong relationships at the worksite level is critical to reaching participation goals. Finally, we acknowledge that those who did not complete the nonparticipant survey may be more representative of true “nonparticipants.” However, we anticipate that those willing to respond to the nonparticipant survey present a more probable opportunity for participation improvement.
Future Directions
We suggest that future research continue to examine the utility of each intervention to reduce sedentary time, but to move toward a stronger determination of understanding the public health impact of the interventions by assessing both reach and effectiveness. We propose that a future effectiveness trial could use a cluster RCT to determine the reach of each intervention by completing randomization at the worksite level where participants within each worksite are only exposed to and consent to receive a single intervention. By doing so, additional information related to proportional reach of each intervention can be gleaned and can provide an understanding of the representativeness of those who engage compared to those who do not.21
It would also be of benefit to examine the factors related to enrollment outside the context of accrual for the research intervention. Specifically, future effectiveness research should examine the degree to which characteristics of each intervention influence organizational decision-making relative to focusing on sedentary behavior in contrast to, or in combination with, other health initiatives. Developing decision aids that examine information on cost and cost–benefit analysis and testing the degree to which different information can influence organizational uptake of the interventions would add substantially to the worksite health promotion literature.
Conclusions
Cluster RCTs are a gold standard approach to examine intervention effectiveness at the group level and are therefore needed to inform the design of effective workplace health interventions. To increase the translation from efficacy to effectiveness and dissemination of workplace health interventions, we encourage researchers and practitioners to monitor, document, and evaluate intervention reach and participation barriers at all stages. Increasing participation flexibility, building rapport and altruistic relationships, providing consistent communication, and managing expectations to promote a participant-centered approach in both research and practice may further facilitate the translation of evidence-based health initiatives to real-world settings.
SO WHAT?
What Is Already Known on This Topic?
The workplace has been identified as an opportune setting for sedentary behavior reduction and health promotion. Designing efficacious interventions that are adopted by worksites and employees remains to be a challenge.
What Does This Article Add?
This research provides insight regarding participation barriers experienced and associated reach of a large workplace intervention during the efficacy stage, to inform future dissemination efforts. We discuss our results in the context of recommendations to reach participation goals in future workplace interventions.
What Are the Implications for Health Promotion Practice or Research?
Our detailed description and evaluation of worksite and employee reach and identification of participation barriers during the efficacy stage can inform both the design and participation goals of future workplace interventions. This may facilitate their translation from efficacy to effectiveness and dissemination.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (R01CA198971).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN)—terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. [DOI] [PubMed] [Google Scholar]
- 3.Buckley JP, Mellor DD, Morris M, Joseph F. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup Environ Med. 2014;71(2):109–111. [DOI] [PubMed] [Google Scholar]
- 4.Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (Aus-Diab) study, 2004–2005. Diabetes Care. 2010;33(2):327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. 2016;48(2):175–181. [DOI] [PubMed] [Google Scholar]
- 6.Crespo NC, Mullane SL, Zeigler ZS, Buman MP, Gaesser GA. Effects of standing and light-intensity walking and cycling on 24-h glucose. Med Sci Sports Exerc. 2016;48(12):2503–2511. [DOI] [PubMed] [Google Scholar]
- 7.McCrady SK, Levine JA. Sedentariness at work: how much do we really sit?. Obesity. 2009;17(11):2103–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Healy GN, Eakin EG, Owen N, et al. A cluster RCT to reduce office workers’ sitting time: impact on activity outcomes. Med Sci Sports Exerc. 2016;49(10):2032–2039. [DOI] [PubMed] [Google Scholar]
- 9.Danquah IH, Kloster S, Holtermann A, et al. Take a Stand!—a multi-component intervention aimed at reducing sitting time among office workers—a cluster randomized trial. Int J Epidemiol. 2016;46(1):128–140. [DOI] [PubMed] [Google Scholar]
- 10.Buman MP, Mullane SL, Toledo MJ, et al. An intervention to reduce sitting and increase light-intensity physical activity at work: design and rationale of the ‘Stand & Move at Work’ group randomized trial. Contemp Clin Trials. 2016;53:11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robroek SJ, Van Lenthe FJ, Van Empelen P, Burdorf A. Determinants of participation in worksite health promotion programmes: a systematic review. Int J Behav Nutr Phy. 2009;6(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilpatrick M, Blizzard L, Sanderson K, Teale B, Venn A. Factors associated with availability of, and employee participation in, comprehensive workplace health promotion in a large and diverse Australian public sector setting: a cross-sectional survey. J Occup Environ Med. 2015;57(11):1197–1206. [DOI] [PubMed] [Google Scholar]
- 13.Torgerson DJ. Contamination in trials: is cluster randomisation the answer? BMJ. 2001;322(7282):355–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell MK, Snowdon C, Francis D, et al. Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study. Health Technol Assess. 2007;11(48):iii,ix–105. [DOI] [PubMed] [Google Scholar]
- 15.Gul RB, Ali PA. Clinical trials: the challenge of recruitment and retention of participants. J Clin Nurs. 2010;19(1-2):227–233. [DOI] [PubMed] [Google Scholar]
- 16.Mutrie N, Foster C, Estabrooks P, Burton NW, Baker G. Recruiting hard-to-reach populations to physical activity studies: evidence and experiences. J Phys Act Health. 2010;7(suppl):329–331. [Google Scholar]
- 17.Glasgow RE, Nelson CC, Strycker LA, King DK. Using RE-AIM metrics to evaluate diabetes self-management support interventions. Am J Prev Med. 2006;30(1):67–73. [DOI] [PubMed] [Google Scholar]
- 18.Treweek S, Mitchell E, Pitkethly M, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Library. 2010;20;(1):2–14. [DOI] [PubMed] [Google Scholar]
- 19.Hahn S, Puffer S, Torgerson DJ, Watson J. Methodological bias in cluster randomised trials. Bmc Med Res Methodol. 2005;5(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman JR. Critical issues in developing and following community based participatory research principles. Community Bas Participat Res Health. 2003;1:53–76. [Google Scholar]
- 21.You W, Almeida FA, Zoellner JM, et al. Who participates in internet-based worksite weight loss programs? BMC Public Health. 2011;11(1):709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Welsh E Dealing with data: using NVivo in the qualitative data analysis process. Forum Qualitative Sozialforschung/Forum. Qualitat Soc Res. 2002;3(2):1–9. [Google Scholar]
- 23.Gross D, Fogg L. Clinical trials in the 21st century: the case for participant-centered research. Res Nurs Health. 2001;24(6):530–539. [DOI] [PubMed] [Google Scholar]
- 24.Leonard NR, Lester P, Rotheram-Borus MJ, Mattes K, Gwadz M, Ferns B. Successful recruitment and retention of participants in longitudinal behavioral research. Aids Educ Prev. 2003;15(3):269–281. [DOI] [PubMed] [Google Scholar]
- 25.Mullane SL, Toledo MJ, Rydell SA, et al. Social ecological correlates of workplace sedentary behavior. Int J Behav Nutr Phys Act. 2017;14(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soucek R, Moser K. Coping with information overload in email communication: evaluation of a training intervention. Comput Hum Behav. 2010;26(6):1458–1466. [Google Scholar]


