Abstract
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine. Brace treatment is effective for eligible patients with AIS and the effectiveness is significantly correlated with the average brace-wear time per day. Three-dimensional (3D) printing technology is a recent advancement that offers unique opportunities for biomedical applications, and customisation of scoliosis braces might lead to greater patient satisfaction and improved compliance. We present here the design of a randomised controlled trial on the clinical effectiveness of 3D-printed braces versus thoracolumbosacral orthoses (TLSO) for patients with AIS.
Methods and analysis
Patients with AIS (age 10–16 years) with Risser sign 0-II, Cobb angle of main curve of 20°−40°, premenarchal or no more than 1-year postmenarchal (for women), and no history of treatment are eligible, unless they are unable to tolerate the treatment or refuse participation. A total of 88 patients will be randomised into either the 3D group or TLSO group on a 1:1 basis. Participants in the 3D group will choose between a 3D-printed brace and TLSO, according to the Zelen’s design of the trial. Primary outcome measures will include the average brace-wear time per day, health-related quality of life and Cobb angle progression of the primary curve. Secondary outcome measures will include immediate in-brace correction of Cobb angle of the primary curve, rate of conversion to surgery and incidence of any adverse events. This study is designed as a single-centre, two-arm, superiority and open-label randomised controlled trial. The sample size is calculated with reference to the preliminary study and based on the sample size calculation formula.
Ethics and dissemination
This study was approved by the Peking University Third Hospital Medicine Science Research Ethics Committee (No: 2019-017-02). Results of the trial will be submitted for publication in a peer-reviewed journal and as conference presentations.
Trial registration number
ChiCTR1900027379, pre-results.
Keywords: scoliosis, paediatric orthopaedics, clinical trials
Strengths and limitations of this study.
This trial is a comparative effectiveness trial in a setting similar to the real-life clinical situation.
This trial, following the Zelen’s design, includes no non-interventional group, to increase acceptability of randomisation among the study participants.
Participants and treating physicians are not blinded to the intervention under evaluation; however, orthotists, data managers and radiologists are blinded.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional (3D) deformity of the spine and discovered at the age of 10 or later. It manifests as lateral curvature of the spine, rotation of the vertebrae, and a flexible or rigid deformity on the frontal plane.1 2 The risk of progression in adulthood increases with a curve above 30°; moreover, the risk of health problems and reduction in the quality of life, which are almost certain to happen with a curve above 50° and surgery might be required.3 Conservative treatment to stop progression of the curve, resolve health issues and improve aesthetics via postural correction is important because of the high risk, trauma and large financial burden of the surgery.4
Brace is known to be an effective treatment for eligible patients with AIS, mainly by the application of external corrective forces to the trunk.1 5–8 Thoracolumbosacral orthoses (TLSO) is a classical and effective brace for patients with AIS; however, there is an apparent time–dose effect.7–9 Katz et al7 found that the success rate in patients who wore the brace for more than 12 hours per day was 82%; however, it was 61% and 31% in those who wore it for 7–12 hours and fewer than 7 hours, respectively. Weinstein et al8 reported that the average number of hours of brace wear per day was strongly associated with the outcome. An average more than 12.9 hours per day was associated with success rates of 90%–93%, but the rate was 42% if worn for fewer than 6 hours per day. A recent study by Dolan et al also demonstrated a lower rate of failure of treatment at Italian Scientific Spine Institute than Bracing in Adolescent Idiopathic Scoliosis Trial, primarily explained by longer average hours of brace wear.9 The reported failure rate (progression of AIS warranting surgery) varied widely, ranging from 0% to 79% after bracing.6 8–11 Many factors might have an impact on patient compliance with brace treatment, including a negative cosmetic appearance, physical and functional discomfort resulting from pressure points, humidity and restriction of movement. It is important to develop an ideal brace with biomechanical effectiveness, which will encourage better compliance for patients with AIS.
In recent years, many studies have focused on the computer-aided design and manufacturing system (CAD/CAM) for the design and manufacture of braces for scoliosis. It can achieve clinical outcomes similar to those with conventional methods.12–17 CAD/CAM system was introduced for better customisation of braces in 2004.18 Trunk surface acquisition can be performed using a surface topography system, which provides basic information for the brace design and production.19 However, incomplete consideration of all AIS curve types, and the increased cost and time required might still be the limitations in the clinical setting.15 3D printing is a recent advancement that offers unique opportunities for biomedical applications, with the advantages of customisable results, speedy design and low cost.20 Its use in customisation of scoliosis braces might lead to greater patient satisfaction and improved compliance. In this randomised clinical trial, we aim to compare the 3D-printed brace with TLSO with respect to the compliance, health-related quality of life (HRQoL), Cobb angle progression of the primary curve, immediate in-brace correction of Cobb angle of primary curve, rate of conversion to surgery and incidence of any adverse events. Topography and CAD/CAM system will be used with 3D printing technology to design and produce a customised brace, which can be lighter, more aesthetic and comfortable.
Aims and objectives
The objective of this trial is to compare the clinical effectiveness between 3D-printed brace and conventional TLSO, and we aim to provide clinical evidence about the application of 3D printing technology in brace design and manufacture.
Methods and analysis
Study design
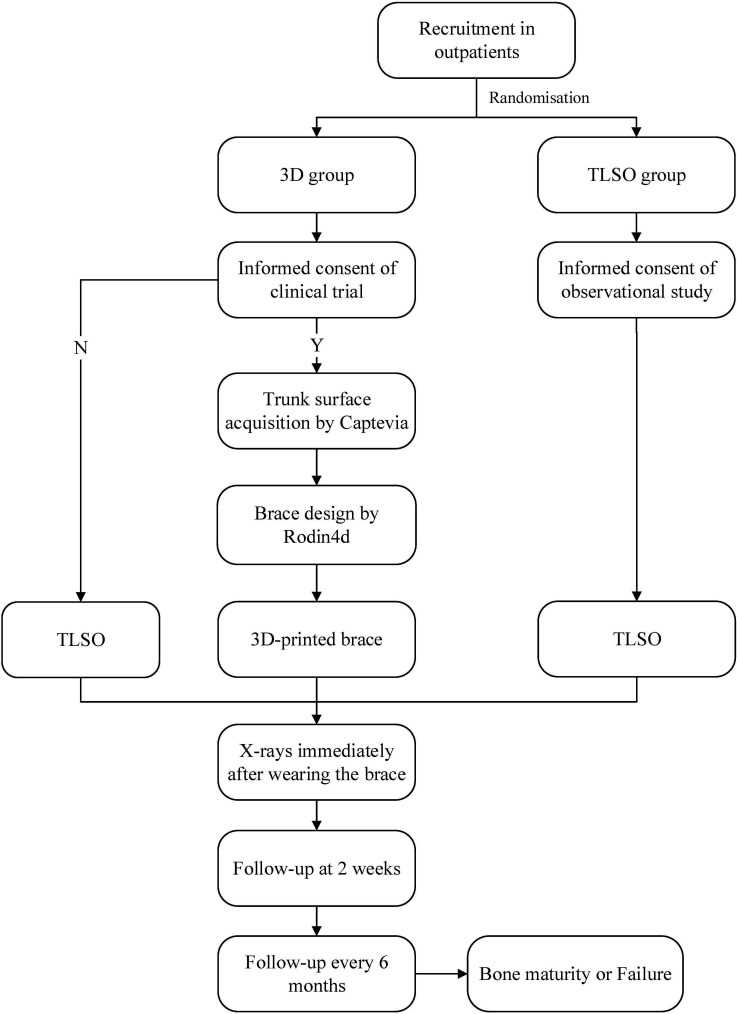
This study is planned to be a prospective, two arm, superiority and open-label randomised controlled trial (RCT) (figure 1).
Figure 1.
Study design. 3D, three-dimensional; TLSO, thoracolumbosacral orthoses.
Zelen’s design21 will be used for allocation and randomisation. There will be two groups, TLSO group (control group) and 3D group (experimental group). The participants enrolled in the TLSO group will be prescribed a conventional TLSO after obtaining informed consent for the observational study. Participants in the 3D group will be allowed to choose between a TLSO and a 3D-printed brace, after obtaining informed consent for the clinical trial according to the Zelen’s design. Patients will be assessed at admission, immediately after wearing the brace, 2 weeks later, and every 6 months until bone maturity or failure of brace treatment. Statistical analysis will be performed between the outcomes of 3D and TLSO groups. Risser sign of 4 (Risser 5 for boys) will be regarded as endpoint for bone maturity. Main curve >45° or need for surgery will be defined as endpoint of failure.
Recruitment and informed consent
This single-centre study will be conducted in Peking University Third Hospital (PUTH). Eligible patients with AIS will be recruited from the outpatient unit of PUTH. The researchers will obtain informed consent for the clinical trial from the 3D group and for an observational study from the TLSO group after randomisation. According to Zelen’s design, participants in the 3D group can choose between a 3D-printed brace and a TLSO. After enrolment, participants will be coded as a unique number and general information will be collected.
Eligibility
Inclusion criteria:
Diagnosis of AIS.
Age between 10 and 16 years.
Risser sign 0-II.
Cobb angle of main curve between 20° and 40°.
No prior treatment.
Premenarchal or no more than 1-year postmenarchal for female patients.
Exclusion criteria:
Secondary scoliosis.
Unable to tolerate the brace.
Patients or guardians refuse to participate in the study for any reason.
Randomisation
Participants recruited from the outpatient clinic in PUTH will be randomised to either the 3D group or the TLSO group via a random number system. All patients in the 3D group will be considered as participants in the experimental group even if they opt for TLSO, according to the Zelen’s design. Randomisation to the experimental group (3D) and control group (TLSO) will be on a 1:1 basis.
Blinding
Participants and treating physicians will not be blinded to the interventions. According to Zelen’s design of the trial, patients randomised to the 3D group will choose between a 3D-printed brace and TLSO. Therefore, a patient receiving TLSO might either be from the 3D group who has opted for a TLSO or from the TLSO group. Thus, the orthotist will be blinded to the result of randomisation even when he or she is customising the TLSO for the patient. The data manager and radiologists will be blinded to the trial.
Interventions
Braces
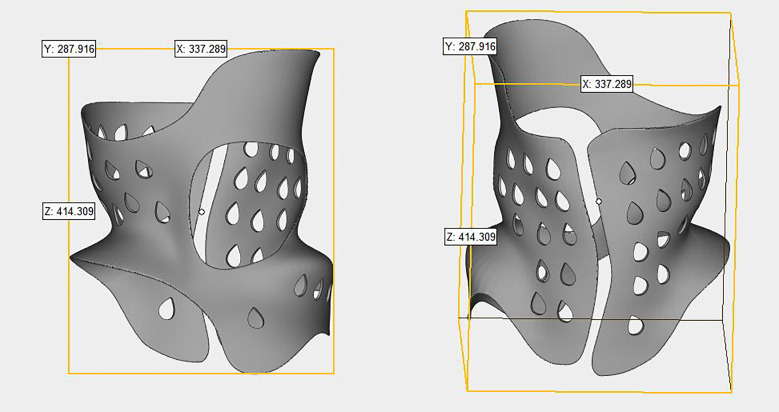
This trial will involve two braces: TLSO and 3D-printed brace. These two types of brace will be made by the same brace room in PUTH. Trunk surface acquisition (Captevia) and CAD/CAM system (Rodin4d) will be used for the 3D-printed brace (figure 2). Parameters and radiograph for the 3D-printed brace will be obtained at admission. Participants will be asked to come back for the fitting of 3D-printed brace 1 week later, after completion of the design and manufacturing. CAD/CAM technology will be applied with the preparation of a positive and then thermoforming for TLSO manufacture. Temperature data logger (HOBO 64K Pendant-UA-001-64, Onset Computer) will be implanted in both, 3D-printed brace and TLSO to log the date, time and temperature every 15 min. The raw data will be downloaded at follow-up and the battery will be replaced every 6 months. It will then be maintained for continuing the data collection. Participants will be informed about the logger for monitoring the temperature of the skin so that we can evaluate the fitness of brace; however, they will not be informed about the time logger. To reduce the chances of patient’s awareness about the presence of time logger, self-reported compliance will also be required from the patients or guardians via a time record software (Brace Former) on the mobile phone, which can record the exact brace-wearing time every day and create a time curve automatically. Compliance outcome from the data logger will be statistically analysed. This approach was approved by our ethics committee. Moreover, the temperature data logger (2.3 in (5.8 cm)×1.3 in (3.3 cm)×0.9 in (2.3 cm)) is small and would not be obstructive to the patient.
Figure 2.
Three-dimensional-printed brace design.
Assessment and management
All participants will be assessed at admission, including physical examination and general condition. X-rays will be taken for all participants at admission, immediately after in-brace, and every 6 months until bone maturity or failure. We set a 6-month interval to minimise radiation exposure. Compliance and HRQoL data will be maintained at 2 weeks after in-brace and every 6 months until bone maturity or failure (table 1). We will check any potential issues with the brace and make necessary adjustments at 2 weeks after in-brace.
Table 1.
Time schedule
| Interventions | Admission | In-brace | 2 weeks | half-yearly |
| Clinical evaluation | ╳ | ╳ | ╳ | ╳ |
| Brace prescription | ╳ | |||
| Compliance and HRQoL | ╳ | ╳ | ╳ | |
| Radiographs | ╳ | ╳ | ╳ |
HRQoL, health-related quality of life.
A form for clinical evaluation including height, and chest, shoulder and back asymmetry will be completed by the clinicians at admission and follow-up. Full-time rigid bracing (20–24 hours per day) will be applied and prescribed for the participants. Physiotherapeutic scoliosis-specific exercise will be taught to all the patients. X-rays including lateral and posteroanterior radiographs of the spine (including both full iliac crests) will be taken at the first in-brace and out of the brace at admission and follow-up. Generally, participants would not take off the brace until radiographic examination and will wear it immediately after.
Outcome measurements
Primary outcomes
Compliance
Except for the data logger monitoring, self-reported compliance will be required from the patients or guardians using a time record software (Brace Former) on the mobile phone. Compliance from the data logger will be statistically compared between the 3D and TLSO groups as primary outcome.
Health-related quality of life
Scoliosis Research Society (SRS) HRQoL outcome assessment tool (SRS-22 Questionnaire) will be used. SRS-22 Questionnaire includes not only the physical health, but also the emotional and psychosocial factors.22–24 Chinese version of the SRS-22 has been verified for clinical use.25 Moreover, Brace Questionnaire (BrQ) has demonstrated good clinical validity for patients with AIS.26 In this study, the Chinese version of BrQ will also be used for additional comparison with SRS-22. HRQoL including SRS-22 and BrQ will be compared between the groups as the primary outcome.
Cobb angle progression
Curve progression above 5° will be measured as the binary outcome. Cobb angle progression of the primary curve will be statistically analysed as the primary outcome.
Secondary outcomes
Immediate correction
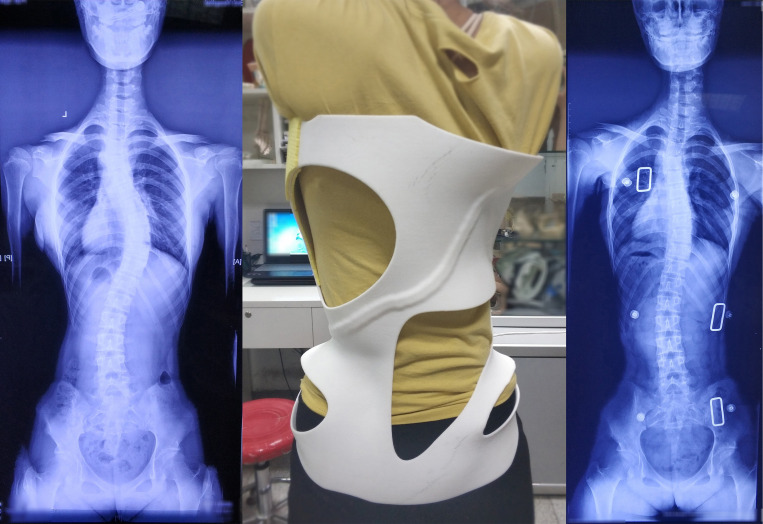
All participants will undergo radiographic examination immediately after in-brace (figure 3). Immediate in-brace correction has been reported to be correlated with long-term effectiveness of brace treatment.27 28 The immediate in-brace correction of Cobb angle of the primary curve will be measured as the secondary outcome.
Figure 3.
Immediate correction of three-dimensional-printed brace.
Rate of conversion to surgery
Main curve over 45° will be recommended for surgery in our study. Rate of conversion to surgery in two groups will be analysed as a secondary outcome.
Incidence of adverse events
All adverse events resulting from use of the brace will be monitored, including any skin problem, intolerable pain, pressure ulcer, dyspnoea, drop-out from our study and so on. Necessary adjustments for the brace will be made by the orthotists immediately. Incidence of any adverse events will be compared between the two groups as a secondary outcome.
Data management
Each participant will receive a unique number and all data will be associated with this number. Data entry, transfer and subsequent maintenance will be performed by a data manager, who is blinded to the allocation. All data including baseline information, type of brace, radiographic outcome and follow-up will be secured in PUTH and the access to the research team will be restricted.
Patient and public involvement
Patients or public were not involved in the design, conduct, reporting, or dissemination plans of our research.
Safety monitoring and adverse events
Participants in this study will receive either a TLSO or 3D-printed brace. Professional physicians will assist in the design, production and wear process. All participants receiving the 3D-printed brace will be evaluated 40 min after in-brace for the skin condition, to check for a likely pressure ulcer. Moreover, all expected or unexpected adverse events from this study will be recorded and monitored. Patients suffered from any adverse events related to brace will also receive free treatment. Regular telephone contact with all participants will be maintained by the assistants once a month. There will be a fast channel in PUTH for the emergency or abnormal sensations requiring the clinician’s intervention.
Sample size calculation
The sample size is calculated with reference to the preliminary study and based on the sample size calculation formula. According to the semistructured interviews of eight patients in the preliminary study, the compliance associated with 3D-printed brace was 50% higher than that with conventional TLSO. The success rate of brace treatment can reach 90% in patients who strictly follow recommendation and less than 70% in patients who do not.8 We will recruit a total of 88 patients for two groups. The sample size is based on a two-sided t-test, a type I error at 0.05 and type II error at 0.2 considering a 1:1 allocation rate and a drop-out rate of 20%.
Statistical analysis
The baseline characteristics of all participants will be summarised by groups, and presented as means (SD) for continuous variables, and count (%) for categorical variables. Statistical analyses in this study will be performed following the intention-to-treat (ITT) analysis. ITT analysis is usually required for Zelen’s design. We will also perform a per-protocol analysis including all the patients and consider the worst-case scenario by including drop-out as failures. Patients in the 3D group will be considered as participants in experimental group even when they choose TLSO. Curve progression, rate of conversion to surgery and any adverse events will be measured as binary outcomes. Compliance and immediate correction of Cobb angle of the primary curve will be measured as continuous outcomes in our design. Non-parametric test will be used for analysing the HRQoL outcomes including SRS-22 and BrQ. Non-parametric test or t-test will be performed for continuous outcomes according to the distribution. Χ2 test and logistical regression model will be used for analysing the binary outcomes. A value of p<0.05 will be considered as statistically significant. All analyses will be performed using the SPSS V.20.0 software, by a researcher blinded to the recruitment and data collection.
Ethics and dissemination
This trial has been approved by PUTH Medical Science Research Ethics Committee (No: 2019-017-02) and registered on Chictr.org. Informed consent will be obtained differently between two groups in this study, observational study for TLSO group and clinical trial for 3D group according to Zelen’s design. Results of the trial will be submitted for publication in a peer-reviewed journal and as conference presentations.
Discussion
We have presented the rationale and design of a prospective RCT to compare the outcomes of 3D-printed brace with conventional TLSO in patients with AIS. The planned RCT will focus on the impact on patients and radiographic outcomes of two braces to explore the clinical effectiveness of using the 3D printing technology in brace treatment for patients with AIS.
In most previous studies of brace for AIS, the outcome was evaluated on radiography, which cannot provide adequate information about the impact of brace on patients. Adolescence is a transitional period involving both physical growth and psychological instability. An externally visible brace might further challenge the compliance of patients with AIS. A literature review by Negrini et al1 mentioned that classical RCTs for brace treatment are limited currently due to the difficulty in randomisation and the lack of attention towards the problems associated with wearing the brace including QoL, disability, back pain and others. In this trial, we will measure compliance (average time of brace wear per day), HRQoL (SRS-22 and BrQ) and Cobb angle progression of primary curve as the primary outcomes. This trial, following the Zelen’s design, will include no non-interventional group, to increase the acceptability of randomisation among the participants. SRS criteria for AIS brace studies recommended that the assessment of effectiveness of brace should include the percentage of curve progression, the percentage of curves exceeding 45° and patients who have been recommended or have undergone surgery.29 We will measure curve progression above 5° as the primary outcome and the rate of conversion to surgery (usually recommended for main curve above 45°) as the secondary outcome in this study. Additionally, it is worth mentioning that the team approach, doctors, physios and certified prosthetist/orthotist can also play an important role in patient compliance, which has been already reported.30 31 Patients in our study will be treated and guided by one single team including medical and physiotherapeutic guidance.
Supplementary Material
Footnotes
YZ and JL contributed equally.
Contributors: YZh contributed to designing the trial and drafted the manuscript. JL helped design the trial. NX contributed to designing the trial, and oversaw the manuscript writing and submission. LZ contributed to the statistical analysis. YZh, JL, NX, LZ, CD, YD, YZe, MY and ZL contributed to the trial design, and have read and approved this manuscript.
Funding: This trial is funded by Young Scientists Fund of the National Natural Science Foundation of China (CN) (2019NSFC81901822), Peking University Fund of Fostering Young Scholars’ Scientific & Technological Innovation (BMU2018PYB016) and Capital’s Funds for Health Improvement and Research (2018-4-4097).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Spine 2016;41:1813–25. 10.1097/BRS.0000000000001887 [DOI] [PubMed] [Google Scholar]
- 2.Kalichman L, Kendelker L, Bezalel T. Bracing and exercise-based treatment for idiopathic scoliosis. J Bodyw Mov Ther 2016;20:56–64. 10.1016/j.jbmt.2015.04.007 [DOI] [PubMed] [Google Scholar]
- 3.Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 2018;13:3. 10.1186/s13013-017-0145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vigneswaran HT, Grabel ZJ, Eberson CP, et al. Surgical treatment of adolescent idiopathic scoliosis in the United States from 1997 to 2012: an analysis of 20,346 patients. J Neurosurg Pediatr 2015;16:322–8. 10.3171/2015.3.PEDS14649 [DOI] [PubMed] [Google Scholar]
- 5.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the brace study of the scoliosis research Society. J Bone Joint Surg Am 1995;77:815–22. 10.2106/00004623-199506000-00001 [DOI] [PubMed] [Google Scholar]
- 6.Danielsson AJ, Hasserius R, Ohlin A, et al. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine 2007;32:2198–207. 10.1097/BRS.0b013e31814b851f [DOI] [PubMed] [Google Scholar]
- 7.Katz DE, Herring JA, Browne RH, et al. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010;92:1343–52. 10.2106/JBJS.I.01142 [DOI] [PubMed] [Google Scholar]
- 8.Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21. 10.1056/NEJMoa1307337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolan LA, Donzelli S, Zaina F, et al. Adolescent idiopathic scoliosis bracing success is influenced by time in brace: comparative effectiveness analysis of BrAIST and ISICO cohorts. Spine 2020;45:1193–9. 10.1097/BRS.0000000000003506 [DOI] [PubMed] [Google Scholar]
- 10.Fernandez-Feliberti R, Flynn J, Ramirez N, et al. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop 1995;15:176–81. 10.1097/01241398-199503000-00009 [DOI] [PubMed] [Google Scholar]
- 11.Goldberg CJ, Moore DP, Fogarty EE, et al. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine 2001;26:42–7. 10.1097/00007632-200101010-00009 [DOI] [PubMed] [Google Scholar]
- 12.Cobetto N, Aubin C-E, Clin J, et al. Braces optimized with computer-assisted design and simulations are Lighter, more comfortable, and more efficient than Plaster-Cast braces for the treatment of adolescent idiopathic scoliosis. Spine Deform 2014;2:276–84. 10.1016/j.jspd.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 13.Wong MS, Cheng JCY, Wong MW, et al. A work study of the CAD/CAM method and conventional manual method in the fabrication of spinal orthoses for patients with adolescent idiopathic scoliosis. Prosthet Orthot Int 2005;29:93–104. 10.1080/17461550500066782 [DOI] [PubMed] [Google Scholar]
- 14.Cobetto N, Aubin CE, Parent S, et al. Effectiveness of braces designed using computer-aided design and manufacturing (CAD/CAM) and finite element simulation compared to CAD/CAM only for the conservative treatment of adolescent idiopathic scoliosis: a prospective randomized controlled trial. Eur Spine J 2016;25:3056–64. 10.1007/s00586-016-4434-3 [DOI] [PubMed] [Google Scholar]
- 15.Phan P, Mezghani N, Aubin Carl-Éric, et al. Computer algorithms and applications used to assist the evaluation and treatment of adolescent idiopathic scoliosis: a review of published articles 2000-2009. Eur Spine J 2011;20:1058–68. 10.1007/s00586-011-1699-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cottalorda J, Kohler R, Garin C, et al. Orthoses for mild scoliosis: a prospective study comparing traditional plaster mold manufacturing with fast, noncontact, 3-dimensional acquisition. Spine 2005;30:399–405. 10.1097/01.brs.0000153346.40391.3b [DOI] [PubMed] [Google Scholar]
- 17.Clin J, Aubin C-E, Labelle H. Virtual prototyping of a brace design for the correction of scoliotic deformities. Med Biol Eng Comput 2007;45:467–73. 10.1007/s11517-007-0171-4 [DOI] [PubMed] [Google Scholar]
- 18.Périé D, Aubin CE, Petit Y, et al. Personalized biomechanical simulations of orthotic treatment in idiopathic scoliosis. Clin Biomech 2004;19:190–5. 10.1016/j.clinbiomech.2003.11.003 [DOI] [PubMed] [Google Scholar]
- 19.Labelle H, Bellefleur C, Joncas J, et al. Preliminary evaluation of a computer-assisted tool for the design and adjustment of braces in idiopathic scoliosis: a prospective and randomized study. Spine 2007;32:835–43. 10.1097/01.brs.0000259811.58372.87 [DOI] [PubMed] [Google Scholar]
- 20.Anderson PA. Clinical applications of 3D printing. Spine 2017;42:S30–1. 10.1097/BRS.0000000000002039 [DOI] [PubMed] [Google Scholar]
- 21.Zelen M. A new design for randomized clinical trials. N Engl J Med 1979;300:1242–5. 10.1056/NEJM197905313002203 [DOI] [PubMed] [Google Scholar]
- 22.Haher TR, Gorup JM, Shin TM, et al. Results of the scoliosis research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine 1999;24:1435–40. 10.1097/00007632-199907150-00008 [DOI] [PubMed] [Google Scholar]
- 23.Asher MA, Min Lai S, Burton DC. Further development and validation of the scoliosis research Society (SRS) outcomes instrument. Spine 2000;25:2381–6. 10.1097/00007632-200009150-00018 [DOI] [PubMed] [Google Scholar]
- 24.Cheung KMC, Cheng EYL, Chan SCW, et al. Outcome assessment of bracing in adolescent idiopathic scoliosis by the use of the SRS-22 questionnaire. Int Orthop 2007;31:507–11. 10.1007/s00264-006-0209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheung KMC, Senkoylu A, Alanay A, et al. Reliability and concurrent validity of the adapted Chinese version of scoliosis research Society-22 (SRS-22) questionnaire. Spine 2007;32:1141–5. 10.1097/01.brs.0000261562.48888.e3 [DOI] [PubMed] [Google Scholar]
- 26.Vasiliadis E, Grivas TB, Gkoltsiou K. Development and preliminary validation of brace questionnaire (BrQ): a new instrument for measuring quality of life of brace treated scoliotics. Scoliosis 2006;1:7. 10.1186/1748-7161-1-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landauer F, Wimmer C, Behensky H. Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil 2003;6:201–7. 10.1080/13638490310001636817 [DOI] [PubMed] [Google Scholar]
- 28.Clin J, Aubin C-É, Sangole A, et al. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine 2010;35:1706–13. 10.1097/BRS.0b013e3181cb46f6 [DOI] [PubMed] [Google Scholar]
- 29.Richards BS, Bernstein RM, D'Amato CR, et al. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on bracing and Nonoperative management. Spine 2005;30:2068–77. 10.1097/01.brs.0000178819.90239.d0 [DOI] [PubMed] [Google Scholar]
- 30.Donzelli S, Zaina F, Negrini S. In defense of adolescents: they really do use braces for the hours prescribed, if good help is provided. results from a prospective everyday clinic cohort using thermobrace. Scoliosis 2012;7:12. 10.1186/1748-7161-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tavernaro M, Pellegrini A, Tessadri F, et al. Team care to cure adolescents with braces (avoiding low quality of life, pain and bad compliance): a case-control retrospective study. 2011 SOSORT Award winner. Scoliosis 2012;7:17. 10.1186/1748-7161-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.