Abstract
Objective
To identify and synthesise the experiences and expectations of women victim/survivors of intimate partner abuse (IPA) following disclosure to a healthcare provider (HCP).
Methods
The databases MEDLINE, Embase, CINAHL, PsychINFO, SocINDEX, ASSIA and the Cochrane Library were searched in February 2020. Included studies needed to focus on women’s experiences with and expectations of HCPs after disclosure of IPA. We considered primary studies using qualitative methods for both data collection and analysis published since 2004. Studies conducted in any country, in any type of healthcare setting, were included. The quality of individual studies was assessed using an adaptation of the Critical Appraisal Skills Programme checklist for qualitative studies. The confidence in the overall evidence base was determined using Grading of Recommendations, Assessment, Development and Evaluations (GRADE)-Confidence in the Evidence from Reviews of Qualitative Research methods. Thematic synthesis was used for analysis.
Results
Thirty-one papers describing 30 studies were included in the final review. These were conducted in a range of health settings, predominantly in the USA and other high-income countries. All studies were in English. Four main themes were developed through the analysis, describing women’s experiences and expectations of HCPs: (1) connection through kindness and care; (2) see the evil, hear the evil, speak the evil; (3) do more than just listen; and (4) plant the right seed. If these key expectations were absent from care, it resulted in a range of negative emotional impacts for women.
Conclusions
Our findings strongly align with the principles of woman-centred care, indicating that women value emotional connection, practical support through action and advocacy and an approach that recognises their autonomy and is tailored to their individual needs. Drawing on the evidence, we have developed a best practice model to guide practitioners in how to deliver woman-centred care. This review has critical implications for practice, highlighting the simplicity of what HCPs can do to support women experiencing IPA, although its applicability to low-income and-middle income settings remains to be explored.
Keywords: qualitative research, public health, quality in healthcare
Strengths and limitations of this study.
This review synthesises and reinterprets rich qualitative data from a range of health settings.
It used a comprehensive search strategy and robust methods for quality appraisal, analysis and interpretation.
A multidisciplinary group of reviewers were involved in the meta-analysis.
A limitation is that few studies were found from low-income or-middle income countries or representing the voices of marginalised communities.
The use of quality appraisal tools in the context of qualitative research is disputed.
Introduction
Intimate partner abuse (IPA) is a violation of human rights that damages health and demands a response from clinicians globally.1 2 Characterised as any behaviour by an intimate partner that causes physical, psychological or sexual harm,1 it is associated with a range of serious physical and mental health conditions1 that can last for many years after the relationship has ended. These include chronic pain, gynaecological problems, sexually transmitted infections and unwanted pregnancies, anxiety, depression, post-traumatic stress disorder and suicidal ideation.1 3 Although anyone in a relationship can experience IPA, it is a gendered phenomenon with more harmful and systematic abuse predominantly perpetrated by men against their female partners.4 IPA has been identified as one of the major causes of morbidity and mortality for women of childbearing age,5 with associated costs to healthcare systems worldwide.6–9
Healthcare providers (HCPs) play an important role in identifying, responding and supporting women experiencing IPA.2 Women experiencing IPA tend to seek healthcare more frequently than women who have not experienced abuse,10 11 providing opportunities for providers to inquire about and address abuse. For example, HCPs—particularly in community or general practice settings—may see women seeking treatment for associated conditions for themselves or their children such as infant sleep and settling issues and poor mental health.10 Similarly, HCPs working in emergency departments may be the first to treat injuries resulting from IPA.12 Although studies have acknowledged a range of barriers to disclosure,13–17 there is growing evidence that women are willing to discuss experiences of IPA with a HCP2 18 and that HCPs can be successfully trained to intervene and respond effectively.19 20 Yet, training and education of HCPs vary greatly,19 21 as does individual practitioner knowledge, understanding and readiness to respond.22 23
In 2006, a qualitative metasynthesis of 29 studies in high-income countries by Feder and colleagues24 looked at women’s experiences and expectations of HCPs when experiencing IPA, finding that women wanted HCPs to respond non-judgementally, be compassionate and sensitive. Women’s readiness to change their situation was found to have an impact on their perceptions of care, highlighting the need for tailored responses.24 Feder and colleagues also concluded that HCPs need to validate women’s experiences, provide them with confidence and respect the decisions they make.24 Feder’s review has made a critically important contribution towards understanding what women want from HCPs. However, since 2006, there has been a great deal more research conducted in the area of violence against women, including in low-income and-middle income countries such as Jordan,25 Nigeria,26 Peru27 and India.28 The problem of IPA has received increasing global attention, as has the potential role of HCPs in addressing it.2 It is an opportune time to re-examine HCP responses to see what (if anything) has changed and where further improvements still need to be made.
A further consideration is the recent development and implementation of various clinical guidelines to support HCPs in identifying and responding to IPA. In 2013, for instance, the WHO released evidence-based guidelines and, in 2014, a handbook with best practice recommendations for HCPs.3 29 These tools—based on extensive consultation with victim/survivors and other experts—recommend that after identifying abuse, HCPs should listen to women non-judgementally, inquire about their needs, validate their experiences of abuse, enhance safety, and provide Support and follow-up care (LIVES; see box 1).29 These strategies are underpinned by the principles of woman-centred care,30 which place the individual woman and her needs at the centre of the patient encounter.31
Box 1. Current recommendations for first-line response (LIVES).
Listen to the woman closely, with empathy, without judging.
Inquire about and respond to her various needs and concerns.
Validate experiences—show her that you understand and believe her. Assure her that she is not to blame.
Enhance safety—discuss a plan to protect herself and children from harm.
Support and follow-up—help her connect to information, services and social support.
LIVES provides suggestions for specific actions that HCPs can take to support women after identification or disclosure of IPA. What is less evident, however, is how HCPs can provide support in a woman-centred way, and the effect on women’s health and well-being if they do not provide care that matches women’s expectations. To fill this gap in the evidence, we have conducted a metasynthesis of qualitative studies focusing on women’s experiences after disclosure of IPA and how they would like HCPs to respond. Our review aims are twofold: (1) to explore women’s experiences and expectations after disclosing IPA to a HCP and (2) to determine the impacts on women if care does not meet their expectations.
Methods
Our metasynthesis methods were based on Cochrane guidance.32 The research question guiding our search was: “What are women’s experiences and expectations after disclosing IPA to a HCP?” The protocol for this review was registered with PROSPERO (CRD42018091523).
Search strategy
Seven databases were searched in February 2020: MEDLINE, Embase, CINAHL, PsychINFO, SocINDEX, ASSIA and the Cochrane Library. Initially, our MEDLINE/Ovid search was designed using subject headings, text words and keywords for women, IPA and qualitative research. This search strategy was then appropriately amended to suit other databases. Grey literature searching took place on both GreyLit and OpenGrey databases. See online supplemental appendix 1 for the Ovid search strategy.
bmjopen-2020-041339supp001.pdf (43.2KB, pdf)
Inclusion criteria
We included primary studies that used qualitative study designs (eg, ethnography or phenomenology) and used qualitative methods for data collection (eg, focus group discussions, individual interviews or observations) and for data analysis (eg, thematic analysis, grounded theory or framework analysis). These were studies that focused on women’s experiences with HCPs after disclosure of IPA, conducted in any country and in any type of clinical or healthcare setting (eg, general practice, emergency department or community health). We considered studies published in in any language since 2004 (picking up where Feder and colleagues24 finished). Studies were excluded if they (1) collected data using qualitative methods but did not use a qualitative method of analysis; (2) were not primary studies (eg, reviews or commentaries); (3) focused on women’s experiences of identification/screening or predisclosure in healthcare settings; (4) included participants who were not women experiencing IPA or (5) included women experiencing IPA who were unable to be distinguished from other participants in analysis.
Selection of studies
Two reviewers (LT and MB) used the software program Covidence33 to independently screen titles and abstracts. Disagreements over inclusion of studies were resolved through discussion with a third reviewer (KH). Following this, Covidence was used by the same two reviewers to screen the full-text articles for inclusion.
Data extraction involved one of five reviewers (LT, MB, LOD, RP or MW) extracting data from the original articles into a form developed for this synthesis. A second reviewer checked the data extraction forms for accuracy and relevance against the original articles and the aim of the research question. The data extraction form included information about the study setting, sample characteristics, objectives, guiding framework, study design, data collection/analysis methods, and qualitative themes, findings and supporting quotations.
All data were imported into NVivo V.12,34 a qualitative data analysis software program. The first author (LT) undertook a process of thematic synthesis, following the methodology proposed by Thomas and Harden.35 Their approach treats both participant quotes and author interpretations as a single body of text to be coded line-by-line. This sets it apart from other approaches to qualitative metasynthesis (such as the modified metaethnographical method used by Feder and colleagues in their original review24), where a distinction is made between first-order, second-order and third-order constructs.
The first step in the analysis was to read and reread the extracted data from the included studies, selecting portions of relevant text and coding them. From the coded text, descriptive themes were developed that outlined the concepts being discussed within the dataset. Finally, the descriptive codes were combined into analytical codes reflecting the ideas that were being formed through engagement with the dataset. The first author met several times with other members of the research team (KH, CG-M, JC and MB) to discuss the development of themes.
Assessing methodological limitations and confidence in review findings
Assessment of methodological limitations of the included articles was undertaken by two independent reviewers (combinations of LT, LOD, RP, RF and MW) using an adaptation of the Critical Appraisal Skills Programme (CASP) Qualitative Checklist.36 This checklist includes the following domains: aims, methodology, design, recruitment, data collection, data analysis, reflexivity and ethical considerations. For each study, reviewers decided whether or not each domain was addressed adequately, recording an answer of ‘yes’, ‘no’, ‘partial’ or ‘unclear’ in a spreadsheet. Reviewers then commented on any other methodological concerns in a free-text response. As the CASP is primarily a learning tool, it does not have a scoring system per se. Consequently, we used the Confidence in the Evidence from Reviews of Qualitative Research (CERQUAL) ratings of ‘no or minor concerns’, ‘minor concerns’, ‘moderate concerns’ or ‘serious concerns’ to categorise our appraisals of overall methodological quality. Authors JC and LT made an assessment of each study’s overall quality based on the CASP domain ratings and the free-text responses provided by each independent reviewer. Disagreements over methodological ratings were resolved through discussion with a third member of the review team to reach a final judgement.
Confidence in the review findings was assessed using the CERQual approach37 by two reviewers (JC and LT). This approach assesses the findings of the review against four key areas. The first area considers methodological limitations38 (which in this case were assessed using the CASP checklist36 as outlined earlier); the second considers the coherence of the data39; the third considers data ‘adequacy’, which refers to the richness of the data within each theme.40 The final area addresses the relevance of the data contributing to each theme.41 The overall level of confidence for each theme finding was rated as either high, moderate, low or very low. This assessment provides a CERQual evidence profile that summarises the overall confidence and rationale for each finding.
Review author reflexivity
The review authors’ views regarding the context and dynamics of IPA, the role of the healthcare system and other demographic factors may have affected the manner in which the data have been interpreted. The authors are a multidisciplinary team of social scientists working in healthcare and violence research, and medical and public health professionals. At the outset of this review, all authors believed that the healthcare system has an important part to play in identifying and responding to women experiencing IPA. Although specialist services are also critical, the healthcare system is often the first point of disclosure or support for many women,2 particularly if they are not ready to name the abuse. The authors were also informed by a feminist and ecological view of IPA as a phenomenon that is ‘wicked’, with many drivers at the societal, community and relationship levels.42 43
Patient and public involvement
Patients and community members were not involved in the review process; however, as this is a meta-synthesis of qualitative studies, patients and the public (in this case, women with lived experience of IPA) were involved as participants in each of the studies included in the review.
Results
We identified 30 studies in 31 articles published between 2004 and January 2020. Figure 1 depicts the flow of studies. Included studies were conducted in 11 countries (see table 1). Ten were conducted in the USA44–53; 4 were conducted in the UK54–57; and 3 were conducted in Canada58–60 and Australia,61–63 respectively. Two studies were conducted in Sweden,61–63 and one study was conducted in Mexico by Swedish researchers.64 The remaining studies were conducted in Japan, Scotland, Israel, Jordan, Germany and Bangladesh (one study per country).25 65–70 All studies were written in English.
Figure 1.
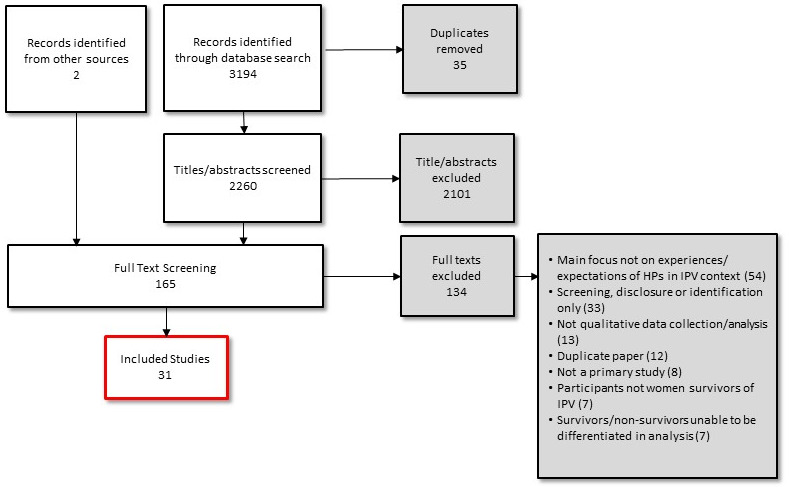
Flow of studies.
Table 1.
Sample characteristics
| Number | Authors | Year (country) | Objective | Qualitative method (analysis) | Sample (age range) |
| 1 | Ahmad et al 58 | 2009 (Canada) | To explore the views of Southeast Asian immigrant women with experiences of IPA and the meaning of help-seeking and reasons for/against help-seeking | Focus groups (thematic analysis) | n=22 (29–68) |
| 2 | Bacchus et al 44 | 2016 (USA) |
To explore women’s views and experiences of being screened for IPA during perinatal home visits in rural and urban contexts in the USA | Interviews (thematic analysis) | n=26 (16–35) |
| 3 | Bradbury-Jones et al 65 | 2011 (Scotland) | To explore the healthcare experiences of women living with IPA, specifically in relation to the primary care setting | Interviews (thematic analysis) | n=17 (age not specified) |
| 4 | Buchbinder and Barakat66 | 2014 (Israel) |
To understand the relationships between Arab–Israeli abused women with social workers in community health clinics | Interviews (content analysis) | n=12 (27–56) |
| 5 | Chang et al 45 | 2005 (USA) |
To describe what women want from IPA healthcare interventions and to understand why they found certain interventions useful or not useful | Interviews (grounded theory) | n=21 (22–62) |
| 6 | Damra et al 25 | 2015 (Jordan) | To explore the experiences of pregnant women disclosing IPA and seeking help from public hospitals in Jordan | Interviews (thematic analysis) | n=25 (20–42) |
| 7 | Dienemann et al 46 | 2005 (USA) |
To increase understanding of abused women’s preferences concerning HCP response when they disclose IPA | Focus groups (thematic analysis) | n=26 (21–65+) |
| 8 | Evans and Feder54 | 2014 (UK) |
To explore pathways to support for IPA victim/survivors and their experiences of barriers and facilitators to disclosure and help-seeking | Interviews (thematic analysis) | n=31 (20–65) |
| 9 | Jack et al 59 | 2012 (Canada) | To develop an IPA intervention to embed within a nurse family partnership | Interviews (content analysis) | n=20 (mean age 21) |
| 10 | Keeling and Fisher55 | 2015 (UK) |
To gain a deeper understanding of women’s experiences of disclosure of IPA to HCPs | Interviews (thematic analysis) | n=15 (21–54) |
| 11 | Kelly47 | 2004 (USA) |
To describe experiences Latina women receiving healthcare, and expectations of HCPs and healthcare systems when experiencing IPA | Interviews (interpretive phenomenological analysis) | n=17 (19–53) |
| 12 | Larsen et al 67 | 2014 (Germany) | To listen to the voices of female victim/survivors exposed to IPA in Germany | Interviews (transcendental phenomenology) |
n=6 (Age range 20–49) |
| 13 | Lundell et al 64 | 2017 (Mexico) | To describe how women in Mexico who have suffered from IPA experience their encounters with HCP | Interviews (thematic analysis) | n=7 (age not specified) |
| 14 | Lutz48 | 2006 (USA) |
To explore how IPA during pregnancy influences women’s decisions about seeking care and disclosing abuse and their preferences for HCP responses | Interviews (grounded theory) | n=12 (18–43) |
| 15 | Malpass et al 56 | 2014 (UK) |
To understand women’s experiences of disclosure of IPA in general practice settings and subsequent referral by their GP or practice nurse to a domestic violence advocate | Interviews (thematic analysis) | n=12 (27–81) |
| 16 | Narula et al 60 | 2012 (Canada) | To understand how women affected by IPA felt their family physicians cared for them and to identify where gaps in care exist | Interviews (content analysis) | n=10 (40–73) |
| 17 | Naved et al 68 | 2009 (Bangladesh) | To understand how women affected by IPA found an initiative to use paramedics as the first-level mental health counsellors of abused women in rural Bangladesh | Interviews (thematic analysis) | n=30 (not stated) |
| 18 | Nemoto et al 70 | 2006 (Japan) |
To explore Japanese women’s experiences of healthcare after disclosing IPA | Interviews and focus groups (content analysis) | n=6 (20–60) |
| 19 | Nemoto69 | 2006 (Japan) |
To explore Japanese women’s experiences of healthcare after disclosing IPA | Interviews (content analysis) | n=6 (20–60) |
| 20 | Nicolaidis et al 4 | 2008 (USA) |
To explore what IPA victim/survivors believe about the relationship between mental health and physical symptoms and to elicit their recommendations for addressing depression | Focus groups (thematic analysis) | n=23 (age not specified) |
| 21 | Olive57 | 2017 (UK) |
To explore women’s emotional responses following attendance to emergency department after an incident of IPA | Interviews (thematic analysis) | n=6 (age not specified) |
| 22 | Örmon et al 71 | 2014 (Sweden) | To elucidate how women subjected IPA experience care provided at a general psychiatric clinic after the disclosure of abuse | Interviews (content analysis) | n=9 (20–55) |
| 23 | Pratt-Eriksson et al 72 | 2014 (Sweden) | To gain a deeper understanding of women’s lived experience of IPA and their encounters with HCP, social workers and police following IPA | Interviews (thematic analysis) | n=12 23–56) |
| 24 | Ragavan et al 50 | 2017 (USA) |
To explore the opinions of women and adolescents residing at a transitional housing programme for adult female IPA victim/survivors and their children | Focus groups (thematic analysis) | n=25 (26–45+) |
| 25 | Reeves and Humphreys51 | 2018 (USA) |
To develop knowledge on women victim/survivors' HCP experiences | Interviews (thematic analysis) | n=14 (22–63) |
| 26 | Reisenhofer and Seibold61 | 2012 (Australia) | To explore healthcare experiences of Australian women living with IPA and consider how these influence their understanding of IPA and sense of self | Interviews (grounded theory) | n=7 (35–50) |
| 27 | Spangaro et al 62 | 2019 (Australia) | To explore Aboriginal women’s perceptions of the impact of IPA enquiry on themselves or their family, and the conditions associated with positive or nil positive impact | Interviews (grounded theory) | n=12 (20–36) |
| 28 | Spangaro et al 63 | 2020 (Australia) | To refine and extend a model and understand the pathways leading to perceptions of positive impact of screening | Interviews (thematic analysis) | n=32 (17–41) |
| 29 | Tower et al 73 | 2006 (Australia) | To explore the health and HCP of women affected by IPA in order to interrogate current health service responses. | Interviews (thematic analysis) | n=9 (Age range 29–45) |
| 30 | Watt et al 52 | 2008 (USA) |
To describe the potential for social support for IPA victim/survivors in healthcare settings, according to a woman’s stage of readiness to disclose and take action to address her safety | Interviews (thematic analysis) | n=16 (19–47) |
| 31 | Zink et al 53 | 2004 (USA) |
To better understand the experiences and needs of older victim/survivors of IPA in the healthcare setting | Interviews (thematic analysis) | n=38 (55–90) |
GP, general practitioner; HCP, healthcare provider; IPA, intimate partner abuse.
Women were recruited from a variety of settings including emergency departments, clinics, hospitals, family practices, women’s refuges and specialist IPA services. Where specified, the types of HCPs that women referred to included doctors, midwives, nurses and social workers.
The methods used for data collection mostly involved interviews (26 studies), with four of the studies using focus groups.
Quality of studies
Thirty of the included articles were published in peer-reviewed journals (one publication was a full doctoral dissertation69). Across all studies, there was a statement of aims and design to either partially or adequately address the objective. All studies included a brief description of the participants, sampling and recruitment strategy, data collection and data analysis. There was transparent reporting of ethical issues. Several studies were unclear or provided only partial information concerning the data analyses.48 50 52 56 60 61 68 70 Eight studies reported incomplete or ambiguous findings not supported by evidence.46 48 59 61 65 66 68 69 Overall, drawing on CASP and CERQual criteria for methodological quality, we assessed 1 study as having serious concerns,68 10 studies as having moderate concerns47–50 52 61 66 69 70 and the remaining 20 studies (which comprised the bulk of the studies) with no/very minor51 53–55 63 71 or minor concerns.25 44–46 51 56–58 60 62 64 65 67 72 73 Missing data may be attributed to word limits set by journals. Table 2 outlines the results of the CASP quality appraisal process and the corresponding rating used in the CERQual assessment.
Table 2.
Methodological assessment of contributing studies
| Author and year | Statement of aims? | Qualitative methodology appropriate? | Research design appropriate? | Recruitment strategy appropriate? | Relationship between researcher and participants adequately considered? | Ethical issues taken into consideration? | Data analysis sufficiently rigorous? | Findings supported by evidence? | Other limitations? | Overall assessment of methodological quality |
| Evans and Feder54 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | No or very minor concerns |
| Keeling and Fisher55 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | N/A | No or very minor concerns |
| Örmon et al 71 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | N/A | No or very minor concerns |
| Reeves and Humphreys51 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | No or very minor concerns |
| Spangaro et al 63 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | No or very minor concerns |
| Zink et al 53 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | N/A | No or very minor concerns |
| Ahmad et al 58 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Community workers recruited participants, potential conflict of interest | Minor concerns |
| Bacchus et al 44 | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Purposive sampling may create bias | Minor concerns |
| Bradbury-Jones et al 65 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Partial | N/A | Minor concerns |
| Chang et al 45 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No limitations acknowledged and quotes not given any identifier (strength of themes unclear) | Minor concerns |
| Damra et al 25 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | Minor concerns |
| Dienemann et al 46 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Partial | No limitations acknowledged and quotes not given any identifier (strength of themes unclear) | Minor concerns |
| Jack et al 59 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | No primary data reported on women’s expectations, only author interpretations | Minor concerns |
| Larsen et al 67 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Minor concerns | |
| Lundell et al 64 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Low response rate | Minor concerns |
| Malpass et al 56 | Yes | Yes | Yes | Yes | Yes | Yes | Partial | Yes | Low response rate | Minor concerns |
| Narula et al 60 | Yes | Yes | Yes | Yes | Yes | Partial | Partial | Yes | Questionable approach to recruitment could have created a selection bias | Minor concerns |
| Olive57 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | Minor concerns |
| Pratt-Eriksson et al 72 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Recruit methods not outlined | Minor concerns |
| Spangaro et al 62 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Minor concerns | |
| Tower et al 73 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Small sample size | Minor concerns |
| Buchbinder and Barakat66 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Partial | Although 12 women were interviewed twice, results (quotes) from only five women are reported. | Moderate concerns |
| Kelly47 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Not always clear what the overarching and subthemes were | Moderate concerns |
| Lutz48 | Yes | Yes | Partial | Partial | Yes | Yes | Partial | Unclear | N/A | Moderate concerns |
| Nemoto69 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Partial | Inconsistent/patchy reporting of data in findings | Moderate concerns |
| Nemoto et al 70 | Yes | Yes | Partial | Partial | Yes | Yes | Partial | Yes | N/A | Moderate concerns |
| Nicolaidis et al 49 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No limitations acknowledged and quotes not given identifiers (strength of themes unclear) | Moderate concerns |
| Ragavan et al 50 | Yes | Yes | Yes | Yes | Unclear | Yes | Unclear | Yes | Concerns about how the data analysis was performed, without statement of which theory was used | Moderate concerns |
| Reisenhofer and Seibold61 | Yes | Yes | Yes | Yes | Unclear | Yes | Unclear | Yes | Lack of detail around how rigor was ensured in analysis. | Minor concerns |
| Watt et al 52 | Yes | Yes | Yes | Yes | Unclear | Yes | Unclear | Yes | N/A | Moderate concerns |
| Naved et al 68 | Yes | Yes | Partial | Partial | Partial | Partial | No | Partial | Lack of detail on sampling and methods | Serious concerns |
N/A, not applicable.
Confidence in review findings
Using the CERQual approach, we assessed two review findings as high confidence and two review findings as moderate confidence (see table 3 for a summary of review findings and explanation for each CERQual assessment).
Table 3.
CERQual evidence profile table
| Summary of review finding | Studies contributing to the review finding | Assessment of methodological limitations by theme | Assessment of coherence | Assessment of adequacy | Assessment of relevance | Overall CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
| Connection through kindness and care | |||||||
| Kindness and empathy | Studies 2, 5, 7, 11, 12, 15, 17, 18, 19, 21, 22, 23, 25, 26, 29, 30 (16 studies) |
|
No or very minor concerns about coherence (26 studies). The data reflected that kindness and care were central to women’s expectations of HCPs after disclosure of IPA. |
No or very minor concerns about adequacy (26 studies) Sixteen studies contributed data and described a need for kindness, care, empathy and a feeling of being looked after. Fourteen studies contributed data and described the importance of respecting women, building trust between them and HCP. Nine studies contributed data on the importance of ongoing support and continuity of care. Based on an overall assessment of the richness and quantity of the data, we concluded that we had no or very minor concerns about data adequacy. |
No or very minor concerns about relevance (26 studies) | High confidence | This finding was graded as high confidence as it is likely that the finding is a reasonable representation of women’s experiences and expectations after disclosure of IPA to a HCP. 26 studies with minor-moderate methodological limitations. No or very minor concerns about coherence and adequacy. |
| Trust & respect | Study 1, 3, 11, 13, 16, 17, 18, 20, 21, 23, 24, 26, 29, 30 (14 studies) |
||||||
| Ongoing support/continuity of care | Studies 6, 7, 9, 10, 14, 15, 16, 24, 28 (nine studies) |
||||||
| See the evil, hear the evil, speak the evil | |||||||
| Being heard and understood | Studies 1, 2, 6, 9, 11, 12, 13, 16, 17, 19, 29, 30, 20, 22, 23, 24, 27, 28, 31 (19 studies) |
|
No or very minor concerns about coherence (28 studies). The finding highlights the critical importance of HCPs recognising and understanding abuse. Women across the studies emphasised the need for HCPs to make time to listen to them, even though they accepted that there were competing pressures and organisational barriers. |
No concerns about adequacy (28 studies). Twenty-two studies contributed data on the importance of validating women’s experiences. Nineteen studies described how the HCP needs to 'really hear' what women are saying. Eight studies described a need to take time to listen to women. Eight studies identified the need for HCP to be non-judgemental. Eight studies described the need for raising awareness. Based on an overall assessment of the richness of the data and the quantity of the data, we concluded that we had no concerns about data adequacy. |
No or very minor concerns about relevance (28 studies) | High confidence | This finding was graded as high confidence as it is likely that the finding is a reasonable representation of women’s experiences and expectations after disclosure of IPA to a healthcare provider. 26 studies with minor–moderate methodological limitations. No or very minor concerns about coherence and adequacy |
| Making time to listen | Studies 6, 7, 13, 18, 21, 23, 25, 26 (eight studies) | ||||||
| Being non-judgemental | Studies 1, 6, 7, 13, 17, 22, 26, 29 (eight studies) |
||||||
| Validating experiences | Studies 9, 10, 12, 14, 15, 16, 20, 22, 26, 29, 3, 4, 14, 16, 6, 11, 18, 19, 23, 25, 13, 31 (22 studies) |
||||||
| Raising awareness/naming | Studies 5, 7,14,15, 26, 31, 27, 28 (eight studies) |
||||||
| Do more than just listen | |||||||
| Action and advocacy | Studies 10, 11, 15, 18, 19, 25, 30, 7, 12, 14, 16, 5 (12 studies) |
|
No or very minor concerns about coherence (16 studies). The findings identified women greatly valued HCPs taking the time to listen and validate their experiences, a strong theme across included studies was the need for HCPs to provide practical support. |
No or very minor concerns about adequacy (16 studies). Fourteen studies described a need to connect to other services. Twelve studies the need for HCP to take practical action to help women. Ten studies described it is important that doctor be guided by what women want. Four studies described the need for safety planning. Based on an overall assessment of the richness of the data and the quantity of the data, we concluded that we had no or very minor concerns about data adequacy. |
No or very minor concerns about relevance (16 studies). | Moderate confidence | This finding was graded as moderate confidence as it is likely that the finding is a reasonable representation of women’s experiences and expectations after disclosure of IPA to a healthcare provider. 16 studies with minor-moderate methodological limitations. No or very minor concerns about coherence and adequacy. |
| Safety planning | Studies 2, 9, 10, 14 (four studies) | ||||||
| Response needs to match needs | Studies 6, 8, 10, 11, 12, 16, 18, 19, 26, 29 (10 studies) | ||||||
| Connect me to resources | Studies 2, 3, 8, 9, 11, 15, 7, 9, 10, 11, 12, 14, 15, 23, 30 (15 studies) | ||||||
| Planting the right seed | |||||||
| My life is my own. | Studies 4, 5, 7, 9, 11, 12, 13, 14, 30, 27 (10 studies) |
|
No or very minor concerns about coherence (16 studies). The findings emphasised the importance of the HCP facilitating choice and control for women, without feeling compelled to ‘fix’ their problems. Women felt strongly that they were the agents of their own lives, and that the HCP’s role was to provide options, encouragement and support rather than dictating what actions they should take. |
No or very minor concerns about adequacy (16 studies). Ten studies described a focus on empowerment, women’s choice and control. Ten studies described the importance for the response to be sensitive to woman’s stage of readiness. Five studies recognised potential for power imbalance. Four studies contributed to women don’t want HCP to 'fix' things. Based on an overall assessment of the richness of the data and the quantity of the data, we concluded that we had no or very minor concerns about data adequacy. |
No or very minor concerns about relevance (16 studies) | Moderate confidence | This finding was graded as moderate confidence as it is likely that the finding is a reasonable representation of women’s experiences and expectations after disclosure of IPA to an HCP. 16 studies with minor-moderate methodological limitations. No or very minor concerns about coherence and adequacy |
| Meet me where I'm at. | Studies 2, 4, 5, 7, 9, 11, 14, 15, 20, 30 (10 studies) |
||||||
| Power imbalance HCP/patient | Studies 10, 15, 20, 25, 17 (five studies) |
||||||
| You don't need to fix things. | Studies 5, 11, 14, 29 (four studies) | ||||||
CERQual, confidence in the evidence from reviews of qualitative research; HCP, healthcare provider; IPA, intimate partner abuse.
Key themes
Four analytical themes were developed that describe women’s experiences and expectations after disclosure of IPA to an HCP: (1) connection through kindness and care; (2) see the evil, hear the evil, speak the evil; (3) do more than just listen; and (4) plant the right seed. Each of these themes is described in detail as follows, with supporting quotations taken from the included articles. Table 4 provides a summary of analytical themes, HCP actions and emotional impacts on women if these key expectations are absent from care.
Table 4.
Summary of analytical themes, HCP actions and emotional impacts on women if absent from care
| Theme | HCP actions | Emotional impact on women if absent from care | Example quotation |
| Connection through kindness and care | Demonstrate kindness, caring, empathy and respect to build trust. | Retraumatised51 | I think had she (HCP) had a better bedside manner, that experience wouldn’t have been as traumatic…she just wasn’t very kind51 (p.1173) |
| Untouchable61 | It’s as if you’ve got some kind of disease, nobody wants to come close to you, nobody wants to catch it.61 (p.2258). | ||
| Ignored, abandoned and neglected47 72 | She (HCP) made it clear to me that she didn’t care about the situation that I was in.47 (p.99) | ||
| Intimidated62 | It was a bit intimidating because of the midwife, her attitude. I don’t think she was having a good day.62 (p.800) | ||
| Sustain personal engagement to maintain support. | Alone50 60 | How can they help when they do not know me?50 (p.1216) | |
| Feeling like time was wasted63 | …you get one lady that asks you about that type of stuff and then you talk to that person and you go to your next visit but THAT lady has no idea and then you go to your NEXT visit and then THAT person has no idea63 (p.346) | ||
| See the evil, hear the evil, speak the evil. | When listening to women, strive to understand the dynamics and context of their situation. | Dismissed53 67 | She asked my children, ‘Where is your father?’ … She just avoided my feelings and kept saying they have to see their father and I should not stop that opportunity.50 (p1216) |
| Silenced53 55 72 | Most of the time, they (physicians) think you are just getting a little carried away, you are a little high-strung, you are very nervous, you have always been this way, so calm down53 (p.902) | ||
| Name the abuse and validate experiences. | Feelings of self-blame and guilt61 64 | If you are not left black and blue or (do not) have physical injuries, (then) it feels that it does not count. As if you should be able to take a few bad words or insults because it is normal.64 (p952) | |
| Feeling ignored and disrespected51 53 69 70 72 78 | I told the physician that this (injury) was caused by my husband… But his response was like, ‘So what? What do you want me to examine? ’It was like he was asking me why I had gone there (the ER) with such a minor injury… He seemed to be annoyed that I had come to the ER due to marital quarrels69 (p.67) | ||
| Distress51 | That’s one of the most distressing things about going to see doctors… you know that something’s not right but… they tell you you’re fine… You just want to take them by their shoulders and be like ‘no, I promise you that I’m not!’51 (p.1175) | ||
| Do more than just listen. | Action and advocacy guided by women’s needs | Feeling like time was wasted54 55 67 73 | (the HCP) only offered pills, no conversation, no therapy or counselling… nothing, only pills.67 (p.369) |
| Let down47 63 64 | My solicitors were sending letters to my doctor. My doctor wasn’t doing nothing for me though, you know tests for the courts and stuff, he wouldn’t do nothing like that… He has not done nothing for me, you know what I mean, and that’s what caused me problems.55 (p.2369) | ||
| Betrayed47 69 | I trusted him (the physician) because he took care of my body when I was pregnant. However, I finally realised that I had made a mistake in choosing a person to talk to about (my problems with IPV). I never visited that clinic again69 (p.297) | ||
| Connect women with services in the community for health, safety and well-being. | Vulnerable, helpless46 67 | You are a bit helpless at the beginning. You don’t know which kind of help you can get at all, which (help) makes sense.67 (p.370) | |
| Planting the right seed | Tailor responses to women’s individual circumstances. | Disappointed56 63 64 67 69 | Most of them (HCPs) have been neutral when I′ve talked about it (IPV). Someone has said that I’ve been strong, you are smart and intelligent, and you’ll make it. I′m so tired of hearing that!71 (p.2307) |
| Facilitate women’s empowerment, choice and control. | Infantilised55 | I don’t do well with paternalistic doctors who just wanna tell you what to do and you’re supposed to just say ‘yes ma’am, yes sir’ and do it51 (p.1173) | |
| Oppressed64 | I came to talk to a male nurse for some time, but he would always reprimand me. It was like he got angry when I did not do the things he told me to do; it was like the situation felt oppressive.64 (p.) | ||
| Overwhelmed45 | I was traumatised all the time. Everybody’s opinion was better than my opinion and I never took time to think of what I wanted or what I needed. Nobody asked me what I wanted. Everybody told me, ‘You should, you should, you should.45 (p.26) |
HCP, healthcare provider.
Connection through kindness and care
A major finding of this meta-analysis was that kindness and care were central to women’s expectations of HCPs after disclosure of IPA.44–47 51 52 56 57 61 67–73 The emotional support that women wanted from HCPs was described as ‘feeling cared for’44 71 and being ‘taken care of, physically and emotionally’.52 Two quotes below illustrate the importance of emotional support:
I just cried. I was just so relieved that somebody, somebody just said something. And he gave me the box of tissues and I just sat and cried and cried and cried. And he said ‘tell me when you’re ready’. And he was just the nicest person to me ever.56 (pe153)
What I wanted was someone to sit on my bed and tell me that they understand, talk to me about some options that I may have had…and hold my hand.61 (p2258)
Alongside kindness and empathy, women highlighted the need for the HCP to foster a trusting relationship in order to facilitate open discussion.47 49 50 52 57 58 60 61 64 65 68 69 72 73
…When you feel comfortable then you can talk about anything.58 (p618)
Developing a trusting relationship with the HCP had the potential to ameliorate some of the effects of the perpetrator’s psychological abuse.
It’s hard to take help when you’ve been in a situation, because your man will say ‘You can’t cope; don’t do this, don’t do that, don’t speak to strangers, don’t discuss our business’. They (partners) drum into you not to talk about it… But if you get that wee (little) trust in someone and that someone takes a wee bit of time with you – that goes a long way.65 (p38)
HCPs could foster trust by treating women with respect at all times. As one participant put it:
I can understand what you tell me. Talk to me intelligently and don’t treat me like a mushroom and answer my questions.49 (p1161)
Just sit there and maybe just listen to a few words that they’ve got to say. Are they hungry? Do they want a cup of tea? And respect them for who they are … They (women) actually want respect, respect, respect.73 (p194)
The absence of empathy, kindness, trust and respect had a negative emotional impact on women. Some reported feeling dehumanised, traumatised, and untouchable.
When I was talking with the psychiatrist, being diagnosed and prescribed medicine, I felt that he saw only my symptoms. It didn’t seem like one human being talking to another. It was a tough experience for me.69 (p65)
I understood on one hand that the doctor was there to do her job…(but) I think had she had a better bedside manner, that experience wouldn’t have been as traumatic… she just wasn’t very kind51 (p1173)
Helen recalled her desire to be ‘touched’ with compassion saying: ‘There was no feeling, there was nothing there. There was no interaction…everything is cold’. She noted that this accentuated her sense of being untouchable.61 (p.257)
Lastly, women appreciated ongoing, sustained engagement from their HCP.25 46 48 50 55 56 59 60 63 This could be achieved by the HCP subtly letting the woman know that they were available to help if she needed it. Specifically, women spoke of the need for continuity of carer—the same individual with whom they had built up a trusting relationship—rather than simply being able to access a particular service consistently.
…if I go in he (Doctor) says ‘is everything okay?’ and he will say, because he has met my new husband, he will say ‘he’s alright this one he is not as ugly as the last one is’. You know it is just like a nice conversation I think, and I think he says that in a way to let me know that I (the Doctor) am here if you want to talk about things, or I (Doctor) have not forgotten about what’s happened.55 (p.2371)
My children’s paediatrician knows about the abuse and always makes sure I am ok. I drive 30 min to see him, but I don’t want to switch providers.50 (p1216)
Women expected the HCP to understand that making change may take time, and to have patience with them:
Support has to go on… it gives you a chance to make mistakes.46 (p227)
Being unable to see the same practitioner left women frustrated and questioning the value of disclosing IPA in the first place. As a participant in a study by Spangaro and colleagues63 pointed out:
You get one lady that asks you about that type of stuff (IPA) and then you talk to that person and you go to your next visit but THAT lady has no idea and then you go to your NEXT visit and then THAT person has no idea. Yeah. It kind of loses track of why the lady asked the first time. (p346)
See the evil, hear the evil, speak the evil
This theme highlights the critical importance of HCPs recognising, validating and understanding abuse. Women emphasised the need for HCPs to make time to listen to them, even though they accepted that there were competing pressures and organisational barriers.25 46 51 57 61 64 69 72
The nurse who sat with me that day, she was lovely. She was really, really nice. She just listened. Sometimes it’s just nice to have someone to listen. I know that A&E staff are busy. I understand that. But I suppose when it’s a crisis you just need that, even if it’s just five min, just to let it all out.57 (p2322)
Women valued having someone to talk to about their relationship who would understand and really hear what they were saying.25 44 47 49 50 52 53 58–60 62–64 67–69 71–73 For South Asian ethnic minority women in a study by Ahmad et al,58 this meant being able to access a HCP from their own culture. In a study by Spangaro and colleagues,62 Australian Aboriginal women valued the opportunity to ‘yarn about it’ with HCPs from an Aboriginal-specific service (yarning is a form of storytelling). For others, it simply meant having someone who could see their perspective and understand the complexity of their situation. A participant in a study by Larsen and colleagues67 explained that the HCP made her feel that, ‘I see that I am understood and that I(will) get help and that I won’t be alone’. (p369) Similarly, women who received a paramedic-led mental healthcare intervention in rural Bangladesh valued the opportunity just to talk to someone:
I felt good talking, and afa (sister) listened to me, which helped me overcome my pain. … I don’t quite have people who I could open my heart to. … I found such a person and I talked, which made me feel great. … My heart felt light, and I had this good feeling even after I returned home.68 (p486)
When HCPs failed to make time for the woman or made it obvious that they were impatient with her for holding them up, it led to feelings of being unimportant and dismissed.
You tell a story that is so hard to tell; it is so difficult and ugly, and they (the healthcare professionals) do not even respect you enough to give you their undivided attention. They answer the telephone or keep looking at their watch; you can see it in their eyes that they are thinking about something else.64 (p953)
Most studies mentioned the importance of the HCP not only listening but believing, acknowledging and validating the woman’s experiences.25 47–49 51 53 55 56 59–61 64–67 69–73 Failure to validate women, suggested Keeling and Fisher,55 ‘feeds into the discourse of perpetrators, who often also claim that a survivor who chooses to disclose will not be believed’ (p2372). Indeed, Malpass and colleagues in their study of women’s help-seeking56 argued that validation may, in fact, be the ‘most important ingredient’ in the HCP response. When the HCP believed and validated women’s experiences, it could lead to an amelioration of shame and self-blame, reassuring women that what they were going through was not acceptable.48 60 65 66 One participant in a study by Bradbury-Jones and colleagues65 reported that
It’s really nice to hear somebody say ‘It’s not you. You haven’t done anything. It’s him (the abusive partner) – his behaviour is unacceptable’. (p38)
For some women, the HCP could play a role in validating their experiences by naming them as abuse.45 46 48 53 56 61–63 The process could sometimes be confronting, particularly when they had previously been in denial about what was happening in their relationship. A participant in Malpass’ study,56 for instance, described her fear and discomfort at having the HCP name the abuse, yet ultimately, she experienced this response as supportive.
I didn’t think that the problems that I have at home are domestic violence. I really didn’t … it’s so difficult to see myself in that position … because I see people (at work in the refuge) with their faces hanging off and that’s never happened to me. He’s pushed me a couple of times but never really hit me … bullying and God, controlling. He (the GP) put the label on which gave me a bit of a shock. But it also made me feel supported. (pe153)
Unfortunately, many studies described experiences where women received judgemental or blaming responses from a HCP after a disclosure of IPA. For instance, Örmon and colleagues71 reported that participants in their Swedish study were questioned by psychiatric care staff as to why they had not defended themselves from the perpetrator. Similarly, Kelly47 described women being told to ‘just leave’. These responses were interpreted by many of the study authors as being due to a lack of understanding on the part of the HCP with regard to the dynamics and context of IPA. The experience of being judged was repeated across countries and settings, with Reisenhofer and Seibold61 describing instances of nurses in an Australian emergency department context behaving in equally judgemental ways:
Participants felt blamed for ongoing violence for ‘choosing’ not to leave their abuser… Anna recalled one experience: ‘I could hear some of the (nurse’s) comments like ‘why would she do that to herself’, meaning you know, obviously why won’t she get out?’61 (p2258)
Older women in a US study by Zink and colleagues53 and a participant in a Jordanian study by Damra et al 25 also related similar experiences:
I did talk to one doctor years ago, and he advised me to leave, and I said I can’t. He said, well then you’ll have to suffer it out.53 (p902)
After he severely abused me, I decided to ask help from A & E department. When the staff came and started asking me about what happened, I felt that they were slowly withdrawing from helping and started asking about what I had done to make my husband angry and were totally focused on my physical injuries.25 (p812)
Having the HCP respond in a judgemental or blaming manner exacerbated women’s existing feelings of guilt at being abused.
…it’s making me feel bad about myself, I wasn’t doing it to myself.61
Many times, they (the healthcare professionals) make you feel guilty saying things out loud or sometimes it is even the way they look at you. … Once they even told me it was my own fault (that) he beat me up; that in one way or another, I deserved it.64 (p953)
Women also felt invalidated and doubted themselves when the HCP misunderstood or minimised the violence, particularly when they were experiencing psychological or other non-physical forms of IPA.
I still feel (that) many do not take it seriously, not even the medical staff…If you are not left black and blue or (do not) have physical injuries, (then) it feels that it does not count. As if you should be able to take a few bad words or insults because it is normal.64 (p952)
Do more than just listen
Although women greatly valued HCPs taking the time to listen and validate their experiences, a strong theme across the included studies was the need for HCPs to provide practical support.45–48 51 52 55 56 60 67 69 70 One woman described this as receiving ‘real help, not the kind that just passes you from one to another’52 (p723). In Kelly’s study of pregnant Latina women,47 one participant, Sara, described how HCPs assisted her with a range of issues, despite being ‘undocumented, uninsured, and Spanish-speaking’ (p.101):
When she arrived at the ED, pregnant and haemorrhaging from an assault by the abuser, she received prompt medical care. Sara experienced the nurses and doctors as very caring and concerned about her. She was given free medical care and information about applying for Medicaid. She was referred to an advocate who assisted her in obtaining a restraining order. She was referred for prenatal care.47 (p101)
Specific ways that women wanted to be helped by HCPs included addressing co-occurring health issues,45 49 53 67 documenting and describing physical injuries to assist with court cases46 48 60 63 67 and providing legal testimony.48 In Dienemann et al’s 2005 study of victim/survivors in the USA,46 they found that women also wanted
…documentation of any threats made by the abuser to the healthcare providers ‘You want it for the court situation and also from my own personal standing that I know that if it’s documented someplace that I didn’t just stand by and do nothing.’46 (p224)
Another key way that HCPs could provide practical support was through referrals and connection to other organisations and services within the broader community.44 46–48 52 54–56 59 65 67 72 Referrals were not restricted to IPA specialist organisations or refuges but could cover a whole spectrum of services. For instance, Jack and colleagues,59 based on their qualitative data, suggested that HCPs can assist women to ‘learn about and navigate health, social, education, childcare, employment, justice, domestic violence and housing services’ (p7). Watt and colleagues made a similar recommendation.52 Only four studies44 48 55 59 mentioned safety planning or risk assessments as a way HCPs could assist women.
Importantly, women across several of the studies identified an opportunity for the HCP to perform an advocacy role. For instance, in Dienemann et al’s study,46 this entailed making contact on behalf of women when an agency or service would not respond directly to her: ‘They never called me back. My doctor called and they did call him back’. (p226) Based on interviews with women in Canada, Narula and colleagues60 concluded that
…Many women felt very appreciative of the effort their physicians made to advocate for them by means of supporting insurance and disability applications, finding alternative housing, providing medical leave and support in legal cases in the form of clear documentation in their patient chart. (p597)
When HCPs failed to advocate on women’s behalf, this led to feelings of abandonment. For instance, in Nemoto et al’s study,70 a woman described how a nurse—with whom she had a good relationship—could have supported her during a meeting with a psychiatrist and her abusive ex-husband, but instead chose to keep silent:
During the meeting, she felt ill-treated by the psychiatrist, who saw her as ‘a crazy person who needed medicine to shut up.’ The nurse, however, kept quiet the entire time, which she felt was not helpful. She said that she would have liked the nurse to advocate for her in front of the physician and her husband by explaining that she was not crazy but was just tired. (p298)
Similarly, mismatches between women’s needs and the responses they received from the HCP caused frustration and disillusionment.25 47 54 55 60 61 67 69 70 73 In these situations, women felt that they had taken a risk to disclose to the HCP only to be left with a feeling of ‘coming up empty’.47 Even if the HCP was empathetic and listened without judgement, providing an inappropriate response was still perceived as a disappointment.63 For example, women across several studies mentioned being prescribed medication to treat their mental health issues, without the HCP attempting to address the underlying IPA. The excerpt from a study of women’s help-seeking pathways by Evans and Feder54 highlights this:
All but four of the disclosing women (n=16) said their doctor listened and was empathetic, but in most cases prescribed antidepressants and took no further action. Women did not find this supportive and few of them took the medication. This experience set up a cycle of disillusion where further consultation was not considered helpful and disclosing abuse seen as a waste of time. (p69)
Planting the right seed
The importance of the HCP facilitating choice and control for women, without feeling compelled to ‘fix’ their problems was emphasised.45 47 48 73 Women felt strongly that they were the agents of their own lives, and that the HCP’s role was to provide options, encouragement and support rather than dictating what actions they should take.45–48 52 54 62 64 66 67 One participant in Kelly’s47 study described this as ‘planting the seed’—priming the woman to be able to make her own decisions and take control of her own life and not badgering her with questions.
I am responsible for my own life. I choose what is good for me. I have been through enough with my husband, who tried to erase me. Here (with the HCP), I can be genuine and honest. I am not afraid of anything and that strengthens me. Here, I feel as though my life is my own and that I am the one to decide what I will do.66 (p403)
…Even if the choices aren’t that good, I still want a choice.51 (p1176)
Several studies touched on the challenges for HCPs in navigating the boundaries between advocacy and action, and empowering women to make their own choices.49 51 55 56 68 The power dynamic inherent in the medical encounter, for instance, was raised by Malpass and colleagues:
Some women ‘need that push from their GP’ to make contact with a DVA (domestic violence and abuse) advocate. This finding raises questions about shared decision making in the context of DVA and particularly how male GPs should skillfully manage the accentuated power imbalance in a consultation with a female survivor of DVA.56 (pe156)
Related to the concept of empowering women through giving her options is the idea that the HCP needs to respond according to the woman’s level of readiness and her individual circumstances.44–49 52 56 59 66 In other words, to continue the metaphor of planting a seed, the HCP must plant the right seed. This was reflected in ten of the included studies and was a strong theme across the data. Watt et al, who conducted vignette-based interviews with victim/survivors, concluded that:
IPV victims desire appropriate responses by health professionals, suitable to the woman’s stages of readiness for disclosure and accepting assistance…For IPV victims who disclose and are not ready to take action, informational support is important specifically when it is coupled with emotional support. IPV victims who disclosed and are ready for help need action undertaken with respect.52 (p724)
A participant in Spangaro’s study63 further explained this in the context of her interactions with a social worker:
The social worker asked me why I was still in contact with him, or if I was waiting for something from him and I said ‘Yes, just because I’m not ready to do anything more than this.’ It’s like—your personal—your emotional strength, you got like a limit and you just take care of yourself and the pregnancy. (p349)
When HCPs failed to understand or accept a woman’s level of readiness or the complexities of her situation, this led to frustration and a sense that the visit to the HCP had been a waste of time.
My GP asked if I can leave my home and go to a safer place… it is impossible to do that25 (p811)
Discussion
Principal findings
This qualitative meta-synthesis updates and expands on the previous review by Feder and colleagues.24 However, where Feder’s review focused on predisclosure, intradisclosure and postdisclosure, we chose to focus specifically on the postdisclosure period, revisiting the question: ‘What are women’s experiences and expectations of HCPs after disclosure of IPA?’ The four key areas identified in our review that encompass women’s expectations of HCPs after disclosure of IPA are (1) emotional connection (‘connection through kindness and care’); (2) recognition and understanding (‘See the evil, hear the evil, speak the evil’); (3) action and advocacy (‘Do more than just listen’); and (4) choice and control (‘planting the right seed’). When these elements are absent from the care that HCPs provide to women, it can lead to a range of negative impacts on health and well-being.
What this study adds and implications
From Feder’s review,24 we know that women value a non-judgemental approach that validates their experiences, is non-directive and tailored to their individual needs. Our findings confirm that these factors are still central to women’s experiences and expectations of HCPs. Women across the included studies wanted HCPs not only to listen but also to really understand the context and dynamics of their situation to avoid giving inappropriate responses such as telling her to just leave. Furthermore, the HCP had a critical opportunity to validate women’s experiences, including naming the abuse, which could help alleviate some of women’s self-blame and feelings of guilt. Women confirmed that they wanted HCPs to inquire about their needs, and to play a role of encouragement and support that would empower them to make their own choices. Failure on the HCP’s part to offer these responses had potentially damaging impacts on women’s well-being, particularly their mental health.
One of the novel findings of this review is the emphasis women placed on having an emotional connection with the HCP. Although previous reviews and guidelines have acknowledged that practitioners need to be ‘supportive’,24 our review suggests that ‘being loving and kind’57 is a critical element of how HCPs need to respond to women’s disclosures. This could be as simple—as suggested by one participant—as offering a box of tissues and reassuring a woman that she could take her time. A recent review by Moudatsou and colleagues74 suggests further ways that empathy can be incorporated into routine care by HCPs. Their research also confirms that HCPs can be trained to improve their skills in providing empathy and kindness if they do not feel confident. Similarly, HCPs who showed women that they were respected as autonomous individuals were more successfully able to build a trusting relationship. Once this relationship was established, women valued the opportunity to continue to see the same practitioner, reflecting a need for continuity of carer, not just continuity of care. Although many guidelines for practitioners and service providers, particularly in high-income countries, tend to focus on conducting risk assessments and safety planning,75 we found that this was not a major focus for women in the included studies. We are certainly not recommending that HCPs ignore women’s safety concerns or fail to ask women if they are safe at home; however, our findings do suggest that what some women value more than safety discussions is the emotional interaction with the HCP.
Another area identified by our metasynthesis was the need for HCPs to do ‘more than listen’ and provide practical support and/or advocate on behalf of women. Women primarily wanted assistance with documentation of injuries, insurance issues and help with connecting to services within the community rather than referrals to IPA services or refuges. They also wanted the HCP to address their co-occurring health issues and advocate for them in situations where they were vulnerable. Again, this practical focus is somewhat contradictory to the current emphasis placed on issues of safety and risk; most recommendations for early intervention and response direct HCPs to refer to specialist services, yet this may not suit some women’s needs.
Lastly, our findings highlight the simplicity of what women actually want HCPs to do—facilitate emotional connection and provide practical support. They also foreground the negative implications for women’s health and well-being when these expectations are not met. Drawing on the literature from the field of midwifery, we suggest that the HCP can play the role of a ‘professional friend’76 who supports a woman through an emotionally challenging time in her life by providing an empathetic ear, guidance, encouragement and information.
From the findings of this review, we have developed the CARE model (see figure 2). We suggest that this model provides a guideline for HCPs around ensuring that the principles of woman-centred care underpin their practice. Whereas LIVES represents the best-practice model for what HCPs can do when a woman discloses IPA, CARE represents how they can insure that women’s individual needs are at the centre of the responses they provide.
Figure 2.
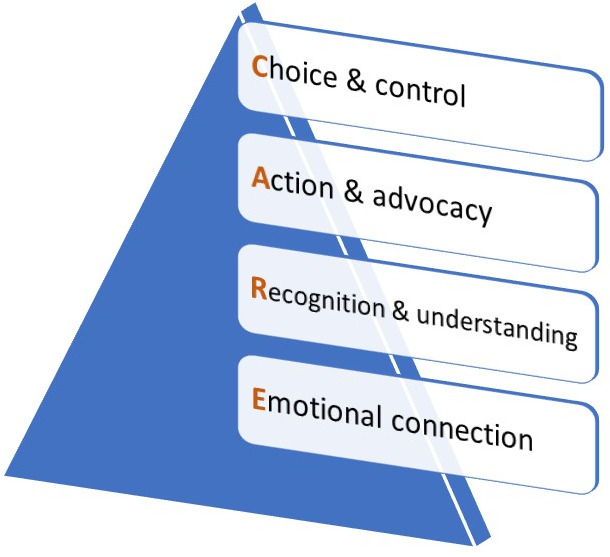
Care model.
It is important to acknowledge here that despite the potential role HCPs can play in supporting women experiencing IPA, ‘getting a disclosure’ should not be the ultimate goal. Although predisclosure and identification are outside the remit of this review, the same woman-centred principles also apply in this context. For example, respecting women’s choice and control over the timing of a disclosure (or whether to disclose at all) are critical. Similarly, demonstrating an emotional connection, advocating for women’s needs (even if unrelated to IPA) and displaying recognition and understanding of IPA as a social issue are all important, even if a disclosure never eventuates.2
Strengths and weaknesses of the study
A strength of this metasynthesis is its comprehensive search strategy (including a range of study designs) and a robust quality appraisal process drawing on Cochrane methods. The treatment of original participant quotations and author interpretations as one body of text to be coded line-by-line also acknowledges and embraces the subjective nature of qualitative work and that it is always open to levels of interpretation. At the same time, the involvement of a large and multidisciplinary review team increases the likelihood that our interpretation of the findings remains an authentic representation of the meanings in the data.
The major limitation of the study is the lack of data from low-income and-middle-income countries. This raises questions about the applicability of the findings and the CARE model for countries with different health system contexts and structural barriers affecting quality of care. The quality appraisal process was also a limitation of this study, although this problem is not unique to our review.77 Currently, there is no gold standard to appraise qualitative studies, and the benefit of appraising quality is contentious.77 Given that low quality was not one of our exclusion criteria, the methodological limitations of some of the included studies mean that the findings ought to be interpreted with caution.
Future research and recommendations
Our review highlights a number of gaps in the knowledge base that ought to be addressed by future research. First, there was a lack of data from low-income and-middle income countries, and most of the available evidence came from the USA. It is critical that the experiences and expectations of women who have experienced IPA in low-income and-middle income settings be explored in future qualitative research. Similarly, only one study in our review focused on an immigrant population, and one on an indigenous population, highlighting that many of the most marginalised voices are absent from the current evidence base. Second, as highlighted by Feder et al,24 there is a lack of longitudinal qualitative evidence on women’s experiences postdisclosure of IPA to a HCP; this remains the case to date. Third, the LIVES framework was only released in 2013 and there may not yet have been time for it to be widely taken up by HCPs. Consequently, it is possible that future qualitative studies exploring women’s perspectives may show different outcomes as LIVES becomes normalised into everyday practice.
From an implementation perspective, we suggest that the usefulness, feasibility and acceptability of the CARE model must now be tested in practice. Health settings are complex beasts; in order for HCPs to provide woman-centred care, there needs to be a whole-of-organisation approach that supports them in this work.23 How to do this effectively merits further investigation. Similarly, structural barriers that limit the accessibility of health systems to many women must also be acknowledged and addressed.17
Conclusions
This qualitative metasynthesis updates and expands the knowledge base around women’s experiences and expectations of HCPs postdisclosure of IPA. The findings have several implications for practice. First, they suggest that—for many women—a primary need is for the HCP is to provide emotional connection, continuity of carer and practical support that facilitate choice and empowerment. Although safety planning and referral to specialist services remain an important component of the healthcare response, HCPs should be mindful that this is not what every woman needs; for some, the desire for kindness and care will be greater. Second, the review suggests a new companion model (CARE) that could be used by practitioners alongside the existing LIVES model to facilitate a woman-centred approach. This may help to increase practitioner confidence in responding to this complex social and health issue.
Supplementary Material
Footnotes
Twitter: @DrLauraTarzia, @JacquiCameron18, @leesahoo
Contributors: LT led study design, data collection and data analysis, and wrote the first and subsequent drafts of the manuscript. MB participated in the study design and data collection and commented on all drafts. JC participated in the data collection, led the quality appraisal and Confidence in the Evidence from Reviews of Qualitative Research process, and contributed to drafting the manuscript. LH and RF made significant contributions to study design and data collection. LOD, RP and MW contributed significantly to the data collection and quality appraisal. CG-M contributed to the study conception, study design and data analysis. GF and JK-M contributed to the study conception and study design. KH led the study conception and contributed to the study design and data analysis and commented on all drafts. All authors read and commented on the final draft of the manuscript and approved it for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This review was supported by the National Health and Medical Research Council through the Centre for Research Excellence in Safer Families (APP1116690). The funding body played no role in the study design; the collection, analysis and interpretation of data; writing of the report; or the decision to submit the article for publication.
Competing interests: None declared.
Patient and public involvement statement: It was not appropriate or possible to involve patients or the public in the design or conduct of this research; however, we plan to involve them in the dissemination and implementation of the findings.
Patient consent for publication: Not required.
Ethics approval: As a review and metasynthesis of existing studies, ethics approval was not required for this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data sharing not applicable as no datasets generated and/or analysed for this study.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1. World Health Organization Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva, Switzerland: WHO, 2013. [Google Scholar]
- 2. García-Moreno C, Hegarty K, d'Oliveira AFL, et al. The health-systems response to violence against women. Lancet 2015;385:1567–79. 10.1016/S0140-6736(14)61837-7 [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva, Switzerland: WHO, 2013. [PubMed] [Google Scholar]
- 4. Johnson MP. Gender and types of intimate partner violence: a response to an anti-feminist literature review. Aggress Violent Behav 2011;16:289–96. 10.1016/j.avb.2011.04.006 [DOI] [Google Scholar]
- 5. Webster K. A preventable burden: measuring and addressing the prevalence and health impacts of intimate partner violence in Australian women: key findings and future directions, in ANROWS compass. Australia’s National Research Organisation for Women’s Safety (ANROWS): Sydney, 2016. [Google Scholar]
- 6. Oliver R, et al. The economic and social costs of domestic abuse: research report 107. United Kingdom: UK Government Home Office, 2019. [Google Scholar]
- 7. Australia P. A high price to pay: the economic case for preventing violence against women. Melbourne, Australia: Pricewater house Coopers, 2015. [Google Scholar]
- 8. Kahui S, Snively S. Measuring the economic costs of child abuse and Intimate partner violence to New Zealand: project commissioned by the glenn inquiry. Wellington, NZ: More Media Enterprises, 2014. [Google Scholar]
- 9. Max W, Rice DP, Finkelstein E, et al. The economic toll of intimate partner violence against women in the United States. Violence Vict 2004;19:259–72. 10.1891/vivi.19.3.259.65767 [DOI] [PubMed] [Google Scholar]
- 10. Hooker L, Versteegh L, Lindgren H, et al. Differences in help-seeking behaviours and perceived helpfulness of services between abused and non-abused women: a cross-sectional survey of Australian postpartum women. Health Soc Care Community 2020;28:958–68. 10.1111/hsc.12927 [DOI] [PubMed] [Google Scholar]
- 11. Kazmerski T, McCauley HL, Jones K, et al. Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Matern Child Health J 2015;19:1490–6. 10.1007/s10995-014-1653-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arora N, Hjalmarsson C, Lang E, et al. CJEM debate series: #domesticviolence - we should routinely screen for domestic violence (intimate partner violence) in the emergency department. CJEM 2019;21:701–5. 10.1017/cem.2019.358 [DOI] [PubMed] [Google Scholar]
- 13. Hegarty KL, Taft AJ. Overcoming the barriers to disclosure and inquiry of partner abuse for women attending general practice. Aust N Z J Public Health 2001;25:433–7. 10.1111/j.1467-842X.2001.tb00288.x [DOI] [PubMed] [Google Scholar]
- 14. Mertin P, Moyle S, Veremeenko K. Intimate partner violence and women’s presentations in general practice settings: Barriers to disclosure and implications for therapeutic interventions. Clinical Psychologist 2015;3:140. [Google Scholar]
- 15. Petersen R, Moracco KE, Goldstein KM, et al. Moving beyond disclosure: women's perspectives on barriers and motivators to seeking assistance for intimate partner violence. Women Health 2004;40:63–76. 10.1300/J013v40n03_05 [DOI] [PubMed] [Google Scholar]
- 16. Rose D, Trevillion K, Woodall A, et al. Barriers and facilitators of disclosures of domestic violence by mental health service users: qualitative study. Br J Psychiatry 2011;198:189–94. 10.1192/bjp.bp.109.072389 [DOI] [PubMed] [Google Scholar]
- 17. Sprague S, Madden K, Simunovic N, et al. Barriers to screening for intimate partner violence. Women Health 2012;52:587–605. 10.1080/03630242.2012.690840 [DOI] [PubMed] [Google Scholar]
- 18. Cox P. Violence against women: additional analysis of the Australian Bureau of statistics' personal safety survey, 2012, in ANROWS horizons. Australia’s National Research Organisation for Women’s Safety Limited: Sydney, 2016. [Google Scholar]
- 19. Zaher E, Keogh K, Ratnapalan S. Effect of domestic violence training: systematic review of randomized controlled trials. Can Fam Physician 2014;60:618–24. [PMC free article] [PubMed] [Google Scholar]
- 20. Sohal AH, Feder G, Boomla K, et al. Improving the healthcare response to domestic violence and abuse in UK primary care: interrupted time series evaluation of a system-level training and support programme. BMC Med 2020;18:48. 10.1186/s12916-020-1506-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Semin JN, Skrundevskiy-Coburn A, Smith LM, et al. Understanding the needs and preferences of domestic and sexual violence education for health profession students. Violence Against Women 2020;26:1876–96. 10.1177/1077801219890420 [DOI] [PubMed] [Google Scholar]
- 22. Kalra N, Di Tanna GL, García-Moreno C, et al. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev 2017;7:CD012423 10.1002/14651858.CD012423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hegarty K, et al. Health practitioners' readiness to address intimate partner violence: a qualitative meta-synthesis. PLOS One;15:e0234067 10.1371/journal.pone.0234067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Feder GS, Hutson M, Ramsay J, et al. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med 2006;166:22–37. 10.1001/archinte.166.1.22 [DOI] [PubMed] [Google Scholar]
- 25. Damra JK, Abujilban SK, Rock MP, et al. Pregnant women’s experiences of intimate partner violence and seeking help from health care professionals: a jordanian qualitative study. J Fam Violence 2015;30:807–16. 10.1007/s10896-015-9720-z [DOI] [Google Scholar]
- 26. Fawole O, et al. Training medical students: victims' perceptions of selectively screening women for intimate partner violence in health care settings. BMC Medical Education 2017;19:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cripe SM, Espinoza D, Rondon MB, et al. Preferences for intervention among Peruvian women in intimate partner violence relationships. Hisp Health Care Int 2015;13:27–37. 10.1891/1540-4153.13.1.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Decker MR, Nair S, Saggurti N, et al. Violence-related coping, help-seeking and health care-based intervention preferences among perinatal women in Mumbai, India. J Interpers Violence 2013;28:1924–47. 10.1177/0886260512469105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization, Health care for women subjected to intimate partner violence or sexual violence: A clinical handbook. Geneva, Switzerland: World Health Organization, 2014. [Google Scholar]
- 30. Brady S, Lee N, Gibbons K, et al. Woman-centred care: an integrative review of the empirical literature. Int J Nurs Stud 2019;94:107–19. 10.1016/j.ijnurstu.2019.01.001 [DOI] [PubMed] [Google Scholar]
- 31. Leap N. Woman-centred or women-centred care: does it matter? Br J Midwifery 2009;17:12–16. 10.12968/bjom.2009.17.1.37646 [DOI] [Google Scholar]
- 32. Noyes J. Qualitative evidence : Higgins J, Cochrane handbook for systematic reviews of interventions. Hoboken: Cochrane Library, 2019. [Google Scholar]
- 33. Veritas Health Innovation Covidence systematic review software. Melbourne, Australia. [Google Scholar]
- 34. QSR International NVivo 2018;12 (2020) NVivo (released in March 2020), https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home [Google Scholar]
- 35. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45. 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Critical Appraisal Skills Programme CASP qualitative checklist, 2018. Available: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf
- 37. Lewin S, Booth A, Glenton C, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13:2. 10.1186/s13012-017-0688-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Munthe-Kaas H, Bohren MA, Glenton C, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 3: how to assess methodological limitations. Implement Sci 2018;13:9. 10.1186/s13012-017-0690-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Colvin CJ, Garside R, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 4: how to assess coherence. Implement Sci 2018;13:13. 10.1186/s13012-017-0691-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Glenton C, Carlsen B, Lewin S, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 5: how to assess adequacy of data. Implement Sci 2018;13:14. 10.1186/s13012-017-0692-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Noyes J, Booth A, Lewin S, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 6: how to assess relevance of the data. Implement Sci 2018;13:4. 10.1186/s13012-017-0693-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Heise LL. Violence against women: an integrated, ecological framework. Violence Against Women 1998;4:262–90. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- 43. Fulu E, Miedema S. Violence against women: globalizing the integrated ecological model. Violence Against Women 2015;21:1431–55. 10.1177/1077801215596244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bacchus LJ, Bullock L, Sharps P, et al. ‘Opening the door’: A qualitative interpretive study of women’s experiences of being asked about intimate partner violence and receiving an intervention during perinatal home visits in rural and urban settings in the USA. J Res Nurs 2016;21:345–64. 10.1177/1744987116649634 [DOI] [Google Scholar]
- 45. Chang JC, Cluss PA, Ranieri L, et al. Health care interventions for intimate partner violence: what women want. Womens Health Issues 2005;15:21–30. 10.1016/j.whi.2004.08.007 [DOI] [PubMed] [Google Scholar]
- 46. Dienemann J, Glass N, Hyman R. Survivor preferences for response to IPV disclosure. Clin Nurs Res 2005;14:215–33. 10.1177/1054773805275287 [DOI] [PubMed] [Google Scholar]
- 47. Kelly UA. Si me preguntas, te lo contare todo: if you ask me, I'll tell you everything. Battered Latina women’s experiences of health care. Newton: Boston College, William F. Connell Graduate School of Nursing, 2004: 184. [Google Scholar]
- 48. Lutz KF. Abused pregnant women’s interactions with health care providers during the childbearing year. Journal of Obstetric, Gynecologic & Neonatal Nursing 2005;34:151–62. 10.1177/0884217505274580 [DOI] [PubMed] [Google Scholar]
- 49. Nicolaidis C, Gregg J, Galian H, et al. "You always end up feeling like you're some hypochondriac": intimate partner violence survivors' experiences addressing depression and pain. J Gen Intern Med 2008;23:1157–63. 10.1007/s11606-008-0606-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ragavan M, Bruce J, Lucha S, et al. The health of women and children after surviving intimate partner violence. Violence Against Women 2017;23:1205–27. 10.1177/1077801216656833 [DOI] [PubMed] [Google Scholar]
- 51. Reeves EA, Humphreys JC. Describing the healthcare experiences and strategies of women survivors of violence. J Clin Nurs 2018;27:1170–82. 10.1111/jocn.14152 [DOI] [PubMed] [Google Scholar]
- 52. Watt MH, Bobrow EA, Moracco KEB. Providing support to IPV victims in the emergency department: vignette-based interviews with IPV survivors and emergency department nurses. Violence Against Women 2008;14:715–26. 10.1177/1077801208317290 [DOI] [PubMed] [Google Scholar]
- 53. Zink T, Jacobson CJ, Regan S, et al. Hidden victims: the healthcare needs and experiences of older women in abusive relationships. J Womens Health 2004;13:898–908. 10.1089/jwh.2004.13.898 [DOI] [PubMed] [Google Scholar]
- 54. Evans MA, Feder GS. Help-Seeking amongst women survivors of domestic violence: a qualitative study of pathways towards formal and informal support. Health Expect 2016;19:62–73. 10.1111/hex.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Keeling J, Fisher C. Health professionals' responses to women's disclosure of domestic violence. J Interpers Violence 2015;30:2363–78. 10.1177/0886260514552449 [DOI] [PubMed] [Google Scholar]
- 56. Malpass A, Sales K, Johnson M, et al. Women's experiences of referral to a domestic violence advocate in UK primary care settings: a service-user collaborative study. Br J Gen Pract 2014;64:e151–8. 10.3399/bjgp14X677527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Olive P. First contact: acute stress reactions and experiences of emergency department consultations following an incident of intimate partner violence. J Clin Nurs 2017;26:2317–27. 10.1111/jocn.13311 [DOI] [PubMed] [Google Scholar]
- 58. Ahmad F, Driver N, McNally MJ, et al. "Why doesn't she seek help for partner abuse?" An exploratory study with South Asian immigrant women. Soc Sci Med 2009;69:613–22. 10.1016/j.socscimed.2009.06.011 [DOI] [PubMed] [Google Scholar]
- 59. Jack SM, Ford-Gilboe M, Wathen CN, et al. Development of a nurse home visitation intervention for intimate partner violence. BMC Health Serv Res 2012;12:50. 10.1186/1472-6963-12-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Narula A, Agarwal G, McCarthy L. Intimate partner violence: patients' experiences and perceptions in family practice. Fam Pract 2012;29:593–600. 10.1093/fampra/cms008 [DOI] [PubMed] [Google Scholar]
- 61. Reisenhofer S, Seibold C. Emergency healthcare experiences of women living with intimate partner violence. J Clin Nurs 2013;22:2253–63. 10.1111/j.1365-2702.2012.04311.x [DOI] [PubMed] [Google Scholar]
- 62. Spangaro J, Herring S, Koziol-McLain J, et al. 'Yarn about it': aboriginal Australian women's perceptions of the impact of routine enquiry for intimate partner violence. Cult Health Sex 2019;21:789–806. 10.1080/13691058.2018.1519117 [DOI] [PubMed] [Google Scholar]
- 63. Spangaro J, Koziol-McLain J, Rutherford A, et al. "Made Me Feel Connected": A Qualitative Comparative Analysis of Intimate Partner Violence Routine Screening Pathways to Impact. Violence Against Women 2020;26:334–58. 10.1177/1077801219830250 [DOI] [PubMed] [Google Scholar]
- 64. Lundell IW, Eulau L, Bjarneby F, et al. Women's experiences with healthcare professionals after suffering from gender-based violence: an interview study. J Clin Nurs 2018;27:949–57. 10.1111/jocn.14046 [DOI] [PubMed] [Google Scholar]
- 65. Bradbury-Jones C, Duncan F, Kroll T, et al. Improving the health care of women living with domestic abuse. Nurs Stand 2011;25:35–40. 10.7748/ns.25.43.35.s47 [DOI] [PubMed] [Google Scholar]
- 66. Buchbinder E, Barakat R. Between the empowered self and the social costs: Arab abused women's perceptions of their relationship with social workers in community health clinics in Israel. Soc Work Health Care 2014;53:398–413. 10.1080/00981389.2014.884039 [DOI] [PubMed] [Google Scholar]
- 67. Larsen MM, Krohn J, Püschel K, et al. Experiences of health and health care among women exposed to intimate partner violence: qualitative findings from Germany. Health Care Women Int 2014;35:359–79. 10.1080/07399332.2012.738264 [DOI] [PubMed] [Google Scholar]
- 68. Naved RT, Rimi NA, Jahan S, et al. Paramedic-conducted mental health counselling for abused women in rural Bangladesh: an evaluation from the perspective of participants. J Health Popul Nutr 2009;27:477–91. 10.3329/jhpn.v27i4.3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nemoto K. Battered Japanese women’s experiences in health care settings: what types of assistance they regarded as helpful or unhelpful, in nursing. USA: University of Wisconsin - Madison, 2006. [Google Scholar]
- 70. Nemoto K, Rodriguez R, Valhmu LM. Exploring the health care needs of women in abusive relationships in Japan. Health Care Women Int 2006;27:290–306. 10.1080/07399330500511774 [DOI] [PubMed] [Google Scholar]
- 71. Örmon K, Torstensson-Levander M, Sunnqvist C, et al. The duality of suffering and trust: abused women's experiences of general psychiatric care--an interview study. J Clin Nurs 2014;23:2303–12. 10.1111/jocn.12512 [DOI] [PubMed] [Google Scholar]
- 72. Pratt-Eriksson D, Bergbom I, Lyckhage ED. Don't ask don't tell: Battered Women living in Sweden encounter with healthcare personnel and their experience of the care given. Int J Qual Stud Health Well-being 2014;9:23166. 10.3402/qhw.v9.23166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Tower M, McMurray A, Rowe J, et al. Domestic violence, health & health care: women's accounts of their experiences. Contemp Nurse 2006;21:186–98. 10.5172/conu.2006.21.2.186 [DOI] [PubMed] [Google Scholar]
- 74. Moudatsou M, Stavropoulou A, Philalithis A, et al. The role of empathy in health and social care professionals. Healthcare 2020;8:26. 10.3390/healthcare8010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Family Violence Prevention Fund, National Consensus Guidelines . On identifying and responding to domestic violence victimization in health care settings. San Francisco USA: Family Violence Prevention Fund, 2004. [Google Scholar]
- 76. Walsh D. An ethnographic study of women's experience of partnership caseload midwifery practice: the professional as a friend. Midwifery 1999;15:165–76. 10.1016/S0266-6138(99)90061-X [DOI] [PubMed] [Google Scholar]
- 77. Mohammed MA, Moles RJ, Chen TF. Meta-synthesis of qualitative research: the challenges and opportunities. Int J Clin Pharm 2016;38:695–704. 10.1007/s11096-016-0289-2 [DOI] [PubMed] [Google Scholar]
- 78. Örmon K, Hörberg U. Abused women's vulnerability in daily life and in contact with psychiatric care: in the light of a caring science perspective. J Clin Nurs 2017;26:2384–91. 10.1111/jocn.13306 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-041339supp001.pdf (43.2KB, pdf)


