Abstract
Objectives
To quantify the contribution variation in socioeconomic status in predicting the distribution of COVID-19 cases and deaths.
Methods
Analyses used incidence data on daily COVID + case counts from all counties from the initial wave of infections, merged with data from the U.S. census data to measure county-level SES and confounders. Multivariable analyses relied on survival analyses and Poisson regression to examine timing of county-level index cases and of COVID-19 incidence and mortality in infected counties to examine the spread and severity of COVID-19 while adjusting for adjusted for Black race, Hispanic ethnicity, age, gender, and urbanicity. Effect moderation by social distancing parameters was examined.
Results
Results indicate that higher SES was associated with earlier incidence of index cases, but that as social distancing took place inequalities in SES inverted so that growth in incidence was slower in higher SES counties, where case-fatality rates were lower.
Conclusions
This study is the first to date to show what happens when an opportunistic disease that could affect anyone meets the American system of inequality and is powerfully shaped by it.
Keywords: COVID-19, Fundamental cause theory, Socioeconomic inequalities and health
1. Introduction
The global COVID-19 pandemic has caused the World Health Organization to declare a global emergency (Sohrabi et al., 2020). COVID-19 is a highly infectious disease (Wu et al., 2020) that can cause multi-organ failure (Zaim et al., 2020) and carries a high case-fatality rate among older adults (Onder et al., 2020). The spatial dynamics of the COVID-19 pandemic and its transmission through global social networks have been well discussed as the epidemic has unfolded (Guo et al., 2020). However, incident cases and deaths per day, to date, have not consistently evaluated how US county-level socioeconomic status (SES) inequalities have shaped COVID-19 outcomes (Sohrabi et al., 2020).
Social epidemiology and medical sociology assert that when social scientists study socioeconomic inequality, racism, gender inequality, social relationships, or a host of other circumstances they simultaneously study factors that have cascading influences on the biology of disease and death. A general principle from this line of work is that social inequalities reliably beget health inequalities (Link and Phelan, 1995). From this tradition, we turn attention to the Coronavirus disease-2019 (COVID-19) pandemic noting that at the biological level, the virus can infect anyone, regardless of wealth or occupation. Despite this appearance of equality of risk, epidemic characteristics of COVID-19 are likely to be shaped in part by our systems of inequality to fulfill the adage that social inequality reliably begets health inequality.
Fundamental cause theory (FCT) (Link and Phelan, 1995; Phelan et al., 2010) proposes that socioeconomic inequalities should play a multifaceted role as the virus spreads (He et al., 2020; Nicola et al., 2020). The theory was initially developed to explain why associations between socioeconomic status (SES) and mortality have emerged across places and times and persist in the face of radical changes in the diseases and risk factors afflicting humans at any particular time (Link and Phelan, 2010). The theory proposes that this occurs because SES-related resources of knowledge, money, power, prestige, and beneficial social connections are flexible resources that are consistently deployed across vastly different health circumstances to ensure better health outcomes for individuals and groups with advantageous circumstances. In essence, the theory proposes that mechanisms linking SES to disease and death change over time as individuals, households, and social groups deploy unequally distributed SES-related resources to gain privileged access to protective factors and to help avoid risk factors.
Clouston et al. (2016) proposed extending FCT to examine changes in social inequalities in health follow four unique stages of disease (SOD) that arise when social forces infiltrate the biological processes that produce disease etiology. Specifically, they suggest that when disease processes are viewed temporally, they present as multiple stages. In the early phases, heterogeneous associations between disease incidence and indicators of socioeconomic status are commonly observed and may favor higher or lower SES individuals. At this stage, the authors suggest that there is insufficient knowledge about the disease to mount an effective defense against it. In this regard, COVID-19 would have most likely been transported to the U.S. from infected countries via prosperous and/or socially interconnected elites with the means to travel globally for business or leisure. However, as knowledge of a new threat grows, the theory suggests that inequalities will also grow as it becomes possible to implement strong public health measures to combat the disease such as sheltering in place, adhering to social distancing guidelines (Sen-Crowe et al., 2020) or advocating reductions in social contacts as an effective way to control epidemics with low reproductive rates (Reluga, 2010). For example, starting on March 16th numerous states throughout the U.S. began issuing initial guidelines advocating for the use of lockdowns, quarantining, and social distancing in hopes of reducing transmission and preserving public health. SES inequalities are expected to grow rapidly because communities and individuals use community agency to control risk and improve survival for their community members, sometimes by disadvantaging others. For example, though being an effective way to avoid infectious disease, social distancing is difficult for those who live in dense or shared housing, with large multi-generational families, who live in short-term housing, who lack access to extra-urban housing, who are/live with “essential workers”, or who lack resources needed to reduce in-person interactions including the ability to negotiate working from home or shop at a distance.
While the forgoing is likely to influence the incidence of COVID-19, factors that occur after the illness is acquired are also likely to be influenced by SES. Firstly, a lifetime of adversity experienced by people from lower SES circumstances increases the risk that individuals may have one or multiple mild to severe health conditions (Langenberg et al., 2006), including notably increased cardiovascular disease burden (Mackenbach et al., 2000), which may be poorly controlled due to lack of access to healthcare and poorer knowledge about managing cardiovascular conditions (Chang and Lauderdale, 2009), and therefore put individuals at risk for unfavorable outcomes from COVID-19 (Zhou et al., 2020). Upon identification of a new COVID-19 case, knowledgeable medical staff must utilize a proactive monitoring protocol for hospital patients that may depend on the timing and availability of resources to improve health (Arabi et al., 2020). Thus, while no known prevention or cure exists for COVID-19, effective disease management includes encouraging patients to receive treatment promptly, avoiding spreading the disease, and assessing symptom dynamics to appropriately characterize this novel disease (Meng et al., 2020; Singer et al., 2020).
Interestingly, the principles from fundamental cause (FCT) and stage of disease (SOD) theories were developed before COVID-19 existed. They are abstract principles about the social shaping of disease before and after encountering social inequality. Whether this novel disease and its consequences spread as predicted bears considerable importance for the value of these theories. Based on these theories we propose that the epidemic occurs as a two-stage process, at first catching elites and higher socioeconomic status (SES) communities unready, leading initial cases to occur in higher SES locales. Then in a second stage, we anticipate that inequalities will arise and grow as communities begin to mobilize by implementing social distancing strategies to rapidly, but unequally, control risk (Clouston et al., 2016). Irrespective of the disease timing, however, we would anticipate that lower SES communities will face the biggest burden of disease and experience more COVID-19 cases than higher SES communities who can mobilize resources to stymie the spread of the virus, reduce overall prevalence, and diminish the risk of death due to the disease.
1.1. Objectives
The goal of this study was to examine the role of SES in the distribution of COVID-19 cases throughout the U.S. We have formed the following questions: 1) Did initial cases between January 22nd, 2020 through May 28th, 2020arise in counties with higher SES? 2) Did social inequalities shift to favor reduced incidence in higher SES counties? 3) Were mortality statistics lower in counties with higher SES?
1.2. Methods
The U.S. is separated into fifty states that enact state-wide policies, interpret federal guidelines, and provide inter-county organizational support. States are formed of counties, our unit of analysis, that implement local public health efforts such as contact tracing, testing, and quarantine requirements. COVID-19 data comes from USAFacts which is a not-for-profit, nonpartisan initiative that provides government data from over 70 sources about numerous topics including daily incidence data concerning COVID-19 by US county (www.usafacts.org). Data on county-level populations are derived from the U.S. Census Bureau which collects demographic and economic survey data of all U.S. residents (https://www.census.gov/). Each year, the Census Bureau publishes population estimates for populations by age, sex, and race/ethnicity, as well as by national, state, and county locations. Additional data on potential confounders was ascertained via the US Census Bureau's American Community Survey that publishes yearly estimates of social and economic indicators at the county level.
The first main outcome of our analysis is defined by the date of the first case in a county – the index case. The selection of this outcome variable allows us to test our prediction that the time a first case will be shorter in relatively high SES counties. The two other outcomes of interest are daily COVID-19 incidence and mortality rates following the index case. These outcomes allow us to test our hypothesis that the SES association with incidence and mortality shifts from a positive (higher SES higher rates) to a negative (higher SES lower rates) over time. Incidence of COVID-19, defined as the rate of newly reported cases of COVID-19, and the rate of COVID-19. Data on mortality within 3141 counties in the U.S. Date of case identification and death were retrieved from USAFacts data.
County-level data from the U.S. census detailing populations were merged with daily confirmed cases and daily COVID-related mortality over January 22nd, 2020 through May 28th, 2020to examine associations between COVID-19 outcomes and a validated SES index. Specifically, to estimate county-level SES we relied on data from the American Community Survey (5-year estimates) for age (% aged 65 and older), race/ethnicity (% Black, % Hispanic), and sex (% male) were merged on at the county level. Socioeconomic status (SES) was measured using a validated method that integrated information on income, education, and wealth into a county-level index (Singh et al., 2002).
We used the date that stay-at-home orders were initially implemented in a state to roughly operationalize the staging concept. We conceptualized the first “natural mortality” stage as the period before the lockdown was implemented and the second “growing inequalities” stage as the period after the lockdown. While social distancing behaviors may have changed before the lockdowns, these requirements signal the beginning of the primary COVID-19 social distancing interventions. In line with this reasoning, we created a dichotomous variable identifying pre (0) versus post (1) the implementation of initial state-wide lockdowns.
1.3. Statistical analyses
For descriptive purposes, we reported associations between the number of COVID-19 cases and variables capturing the demographic composition of counties. To test our first hypothesis that early infections would emerge in counties with higher socioeconomic status, we began by showing Kaplan-Meier onset curves examining the initial presentation of a COVID-19 case in a county by SES tertiles. We conducted multivariable analyses modeling time until the index case was observed using Cox proportional hazards regression. Cox models were used because they allowed us to reliably predict the time until the index case, a central hypothesis in these analyses. To investigate the association between SES and incidence, models were separated into an initial period before a widespread social distancing response and a second period after such a response had occurred. Schoenfeld residuals were used to examine the proportional hazards assumption, and multivariable-adjusted hazard ratios were reported with 95% confidence intervals and p-values.
To examine the hypothesis that incidence rates changed differently in high as opposed to low SES areas in the second stage, we began by showing incidence rates over time starting at the date at which the initial case presented. The multivariable analysis further probed this process using a Zero-inflated Poisson model to model predictors of incidence while jointly estimating the risk of having an index case (Lambert, 1992). Zero-inflated Poisson is unique in allowing researchers to model incidence rates while jointly modeling (and adjusting for) the process examined in our first hypothesis, that is by capturing the initial emergence of community transmission. Since case numbers can increase more rapidly in counties with larger populations, county-level population size was used to capture the number of people who are believed to be susceptible to the disease. Incidence rate ratios and 95% confidence intervals were reported.
To test the hypothesis that higher SES was associated with a reduced risk of COVID-related mortality, we began by showing mortality incidence by SES tertile. Next, multivariable regression analyses relied on Poisson regression to estimate mortality rates among COVID + populations. Poisson regression is a multivariable regression model that allows researchers to examine predictors of count data when the mean is normally dispersed (Gardner et al., 1995). Additionally, since the outcome of interest here was COVID-related mortality, the population at risk of mortality was determined to be all those diagnosed, or posthumously categorized, as having COVID-19. Mortality rate ratios were reported with 95% confidence intervals and p-values. Stata 15.1/IC [StataCorp] was used in statistical analyses.
1.4. Results
Across U.S. counties, 10% of residents were Non-Hispanic Black, 9% Hispanic, and half were female. There were, on average, 4.27 incident cases and eight deaths per day in the U.S (Table 1 ) in the period of observation. The number of counties experiencing their index case on any given day was higher in high-SES counties and lower in low-SES counties over the entire period of observation. The highest SES counties recorded 8.9 incident cases/day and 16 deaths per 1000 cases per day as compared to the lowest SES counties with 1.5 incident cases per day and 3.4 deaths per 1000 cases per day.
Table 1.
Descriptive characteristics across all U.S. counties and separated by socioeconomic status tertile.
| Characteristics | All U.S. Counties | Highest SES tertile | Medium SES tertile | Lowest SES tertile |
|---|---|---|---|---|
| % Black | 9.89 | 5.76 | 6.57 | 17.33 |
| % Hispanic | 8.87 | 9.57 | 8.32 | 8.73 |
| % Female | 49.95 | 50.02 | 50.01 | 49.83 |
| % Aged 65 and older | 8.61 | 7.93 | 9.06 | 8.85 |
| Urbanicity | 4.87 (27.68) | 8.86 (38.56) | 3.34 (20.24) | 2.41 (19.44) |
| Socioeconomic Status | 0.00 (0.75) | 0.79 (0.46) | 0.03 (0.18) | −0.81 (0.42) |
| Incident cases/day | 4.27 (38.98) | 8.90 (57.86) | 2.38 (26.84) | 1.54 (21.49) |
| Number of deaths/day | 8.09 (111.63) | 16.06 (142.44) | 4.8 (104.91) | 3.41 (77.50) |
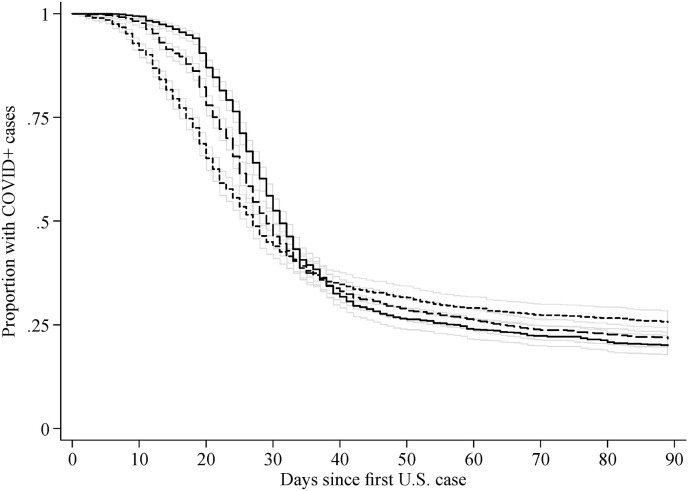
Examining the hypothesis that higher SES was associated with changes in the spread of COVID-19 throughout the population, Kaplan-Meier hazards curve showed that SES was associated with earlier identification of initial COVID + cases (Fig. 1 ). Accounting for the variable impact of social distancing policies highlighted the dual impact of SES, showing that onset of the first COVID + case was earlier (aHR = 2.21; 95%CI 1.95–2.51]) in higher SES counties before social distancing policies were implemented but inverted thereafter (aHR = 0.42; 95%CI[0.36–0.48]) (Supplemental Table 1). This result was not explained away when confounders were included. Concerning covariates other than SES we found that counties with higher average age were at lower risk of experiencing their first case (aHR = 0.88; 95%C.I. = [0.83–0.94]). Higher urbanicity was associated with a greater likelihood of experiencing their first case before social distancing but had larger reductions in risk following social distancing procedures. Blacks and Hispanics faced equal risk for initial cases and less risk after social distancing.
Fig. 1.
Identification of the first reported COVID + case among U.S. counties by high (short dashes) versus (medium dashes) and low (solid) socioeconomic status. 95% Confidence Intervals are provided using thin gray enclosing envelopes.
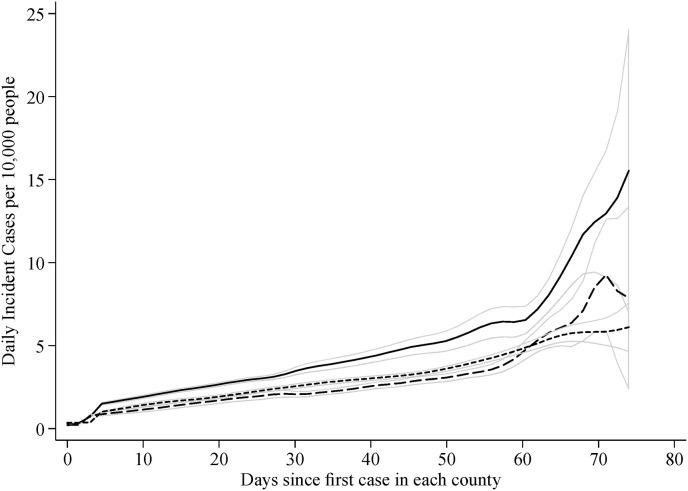
Next, we examined associations between growth in incident cases and growth in incident cases by SES (Fig. 2 ). These results showed that while higher SES counties had higher initial incidence rates, the rate of growth inverted over time resulting in lower growth over time in higher SES counties at the end of the observation period. Results from Fig. 2 were supported by multivariable analyses (Supplemental Table 2) suggesting that growth rates as a whole were more rapid in areas with higher SES before social distancing (aIRR = 1.138; 95% C.I. = [1.37–1.39]) but also suggested that this pattern inverted as social distancing emerged, resulting in smaller increases in COVID cases thereafter.
Fig. 2.
Analyses of population data comparing growth in COVID-19 cases in U.S. counties by high (short dashes) versus medium (dashes) and low (solid) socioeconomic status. 95% Confidence Intervals are provided using thin gray enclosing envelopes.
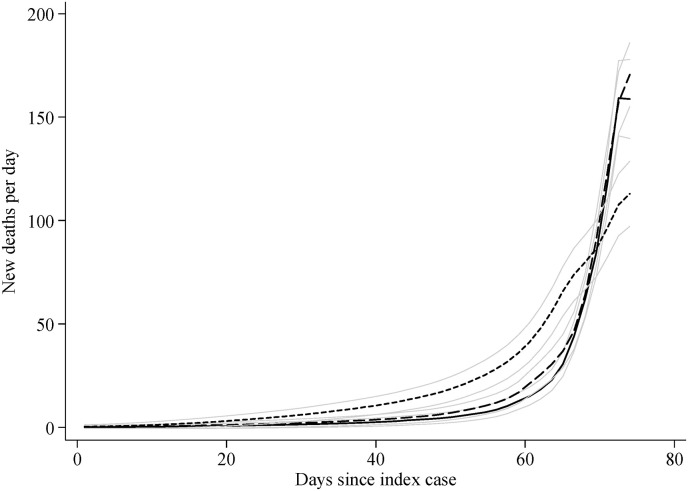
Examining the hypothesis that mortality would be reduced in areas with higher SES (Fig. 3 ), results from unadjusted and multivariable-adjusted models revealed that higher SES was associated with reduced risk of mortality. Counties with higher percentages of minority residents, older people, males, and people living in higher-density communities had higher mortality rates. Results from the figure were supported by multivariable analyses (Supplemental Table 3) revealing that residents of higher SES counties were at much lower risk of COVID-19 mortality as compared to those living in lower SES counties (aMRR = 0.884 [0.876–0.891]).
Fig. 3.
Analyses of population data comparing COVID-19 mortality rates in U.S. counties by high (short dashes) versus medium (dashes) and low (solid) socioeconomic status. 95% Confidence Intervals are provided using thin gray enclosing envelopes.
2. Discussion
Engaging in a long tradition of research on the social shaping of disease and death we set out to determine whether principles derived from two theoretical/conceptual approaches within that tradition could speak to the social distribution and consequences of the novel COVID-19 virus. We used principles from fundamental cause theory and stages of disease theory to derive hypotheses of what we might expect when COVID-19 met social inequality in the US context. We found that during the early period of the COVID-19 epidemic, as the virus was actively diffusing through the American population, that SES was a strong determinant shaping that diffusion. In an initial period, SES was positively associated with the emergence of COVID-19, but then subsequently as a public health response emerged that higher SES individuals were more able to engage in, the SES association with incidence and mortality became inverse. SES inequalities often arise when a new disease is affected either by the structure of a society or as a result of concentrated efforts to reduce disease exposure and severity in a way that advantages some community members.
The present study supports previous work contextualizing the rise and fall of social inequalities, whereby diseases “transition through four stages at a given time: (1) natural mortality, characterized by no knowledge about risk factors, preventions, or treatments for a disease in a population; (2) producing inequalities, characterized by unequal diffusion of innovations; (3) reducing inequalities, characterized by increased access to health knowledge; and (4) reduced mortality/disease elimination, characterized by widely available prevention and effective treatment” (Clouston et al., 2016). Regarding the current pandemic, we posited that structural factors are still producing inequalities, as higher SES counties experience less spread and fewer deaths as new information is diffused and resources are mobilized. Indeed other studies on COVID-19 show that neighborhoods in Chicago, IL, with a higher percentage of Blacks were associated with increased levels of social vulnerability and risk factors (Kim and Bostwick, 2020) and confirm our results that emergency conditions present with COVID-19 highlights existing SES and racial inequities in the U.S.
FCT and SOD theories offer frameworks with which to understand socioeconomic inequalities in health and disease. In essence, these theories drive researchers to ask the question: why is mortality avoidable for some and not others? For our finding of growing SES inequalities in incidence, these theories point to the fact that as knowledge of the threat of COVID-19 grew people of higher SES were more able to shelter in place and enact social distancing. People of lower SES, on the other hand, were much more likely to be classified as essential workers and therefore to live and work in crowded spaces, and to have less adequate worker protections. Our finding that inequalities in mortality when demand for testing kits and personal protective equipment emerged may additionally indicate that communal competition at multiple levels including counties and the hospital systems within them. Areas with more resources were likely better able to access these badly needed resources to accommodate more patients while experiencing a sizable “surge” of new patients with a cluster of new symptoms they had not seen before (Meng et al., 2020; Singer et al., 2020). Together, our results on the influence of SES on COVID incidence and mortality imply that in areas with more resources, individual and collective actions allowed people to deploy the resources available to them to protect themselves. Because of these processes, SES inequalities emerged.
The entire world is waiting on a COVID-19 vaccine. However, the development of a COVID-19 vaccine could exacerbate the patterns described here resulting in a further favoring of high SES areas. As with Salk's discovery of poliomyelitis (polio) vaccine, high SES individuals with greater access to resources were initially first able to access the vaccine (Tan and Ponstein, 2019), Such inequalities are often compounded when vaccinations need to be taken regularly over time to reduce disease risk, as has been shown in human papillomavirus in U.S. adolescents (Polonijo and Carpiano, 2013), and for influenza vaccination (Endrich et al., 2009). To the extent that vaccination is made accessible, FCT suggests that efforts to improve access in low-risk populations might improve distribution and also reduce overall risk since those populations are at higher overall risk (Tan and Ponstein, 2019). Like the polio vaccine, the COVID-19 vaccine must be rapidly extended to the U.S. population irrespective of SES to both reduce health inequalities and more efficiently eliminate COVID-19.
While not the focus of the present study, COVID-19 may increase social inequalities in the long-term. Notably, there is a growing literature that discusses the role of cumulative disadvantage in causing the build-up of stress-related and health-related disadvantage. COVID-19 is known to affect individuals who have multiple comorbidities at greater rates (Atkins et al., 2020). However, there is growing concern about the potential for post-COVID-19 syndrome (Davido et al., 2020). This syndrome is likely to impact those who were already most disadvantaged, thereby amplifying the impacts of a lifetime of exposures (Holuka et al., 2020). Future work is needed to follow individuals with the post-COVID-19 syndrome and determine the longer-term consequences of the infection.
2.1. Limitations
Though being the first of its kind, the current study has several limitations that should be considered when interpreting the results. First, because analyses relied on county-level information to elucidate processes affecting dynamics in the risk of infection at the population level, we could not examine whether individual-level factors might help to explain which individuals were exposed to the disease. Nationwide individual data do not exist at this juncture. Additionally, despite their limitations, county-level data are what policymakers use to determine how the disease is spreading, where hot spots are emerging, and what sorts of interventions should be deployed. County-level data are sufficient to test the theoretically derived hypotheses we proposed, and we contend that the results supporting those predictions are valuable evidence bearing on the validity of the theories (FCT and SOD) that were used to derive those predictions. . Since measures are unavailable across the U.S. to dynamically and accurately determine rates of testing, we could not determine the role of testing as a mediator of the link between SES and COVID-related mortality. The lack of information on testing limits the resolution of the index case, potentially resulting in delayed reporting of index cases in higher SES regions that were affected earlier in the pandemic; if so, then results showing early distribution in high-SES areas would be conservative. Some estimates have suggested that each death due to COVID-19 is accompanied by a second death that went undetected and ignored (Ciminelli and Garcia-Mandicó, 2020). If true, these effects would likely exacerbate the inequalities shown here as counties and states with resources to actively test and monitor the epidemic would have more accurate death identification protocols, and thus higher reported death rates, while places with less testing would have more unobserved or misclassified deaths.
Discussions about the role of racism during this pandemic have highlighted ways in which such racism has disadvantaged the people it has targeted. It is hard to study topics at the nexus of poverty and public health in the U.S. and not see the influence of institutional racism and racist beliefs. Adjustment for percent-Black or Hispanic did not change the results; however, this adjustment may not capture the full potential for racism in minority outcomes since as noted in the descriptive analyses here, minorities are concentrated in the most impoverished counties. Ongoing research in this field needs to continue to examine how COVID-19 affects Black and Latino communities that have had their healthcare resources dismantled (Chung et al., 2020) with an inevitable result being more severe outcomes (Kim and Bostwick, 2020; Nicola et al., 2020).
3. Conclusion
The COVID-19 pandemic has placed into stark relief the incredibly different circumstances that separate our most disadvantaged populations from those who have the privilege of avoiding disease. Vulnerability is a central component of risk exposure and outcomes associated with disasters and hazards, including COVID-19. However, vulnerability is shaped by social, economic, and political contexts (Thomas et al., 2013; Thorpe et al., 2016). Consequently, vulnerability to global pandemics such as COVID-19 depends on structural factors including county-level SES (Kim and Bostwick, 2020; Williams and Collins, 2016). Exposures to diseases and the ability to avoid them are increasingly embedded within social structures that reflect pre-existing patterns of social stratification (Bourgois et al., 2017). This pandemic highlights an urgent need to strengthen social protection systems to make them more responsive to crises and embed them within human rights-based approaches to better support vulnerable populations and enact health and social security benefits. In the absence of adequate social protection, areas of low SES need to be aware of the potential for infections and adopt policies and legislation to both protect public health but ensure no aggravation of existing inequalities.
Funding
We would like to acknolwedge support for studying issues relating to disparities in aging-related conditions (RF1 AG058595).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113554.
Credit author statement
Sean A. P. Clouston conceptualized the study and conducted all analyses, created the visualizations, and edited the draft. Ginny Natale drafted the original manuscript and edited follow-up drafts. Bruce G. Link.provided scientific oversight, helped to conceptualize the study, edited the original manuscript and helped with interpretation
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Arabi Y.M., Murthy S., Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020:1–4. doi: 10.1007/s00134-020-05955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins J.L., Masoli J.A., Delgado J., Pilling L.C., Kuo C.-L., Kuchel G.A., Melzer D. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J. Gerontol.: Series A. 2020;75(11):2224–2230. doi: 10.1093/gerona/glaa183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P., Holmes S.M., Sue K., Quesada J. Structural vulnerability: operationalizing the concept to address health disparities in clinical care. Acad. Med. 2017;92(3):299–307. doi: 10.1097/acm.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang V.W., Lauderdale D.S. Fundamental cause theory, technological innovation, and health disparities: the case of cholesterol in the era of statins. J. Health Soc. Behav. 2009;50(3):245–260. doi: 10.1177/002214650905000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung R.Y., Dong D., Li M.M. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020;369:m1329. doi: 10.1136/bmj.m1329. [DOI] [PubMed] [Google Scholar]
- Ciminelli G., Garcia-Mandicó S. vol. 22. VOXEU, Centre for Economic Policy Research; London: 2020. (Covid-19 in italy: an Analysis of Death Registry Data). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston S.A.P., Rubin M.S., Phelan J.C., Link B.G. A social history of disease: contextualizing the rise and fall of social inequalities in cause-specific mortality. Demography. 2016;53(5):1631–1656. doi: 10.1007/s13524-016-0495-5. [DOI] [PubMed] [Google Scholar]
- Davido B., Seang S., Tubiana R., de Truchis P. Post–COVID-19 chronic symptoms: a postinfectious entity? Clin. Microbiol. Infect. 2020;26(11):1448–1449. doi: 10.1016/j.cmi.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endrich M.M., Blank P.R., Szucs T.D. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27(30):4018–4024. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- Gardner W., Mulvey E.P., Shaw E.C. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol. Bull. 1995;118(3):392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Guo Y.R., Cao Q.D., Hong Z.S., Tan Y.Y., Chen S.D., Jin H.J.…Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J., He L., Zhou W., Nie X., He M. Discrimination and social exclusion in the outbreak of COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(8) doi: 10.3390/ijerph17082933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holuka C., Merz M.P., Fernandes S.B., Charalambous E.G., Seal S.V., Grova N., Turner J.D. The COVID-19 pandemic: does our early life environment, life trajectory and socioeconomic status determine disease susceptibility and severity? Int. J. Mol. Sci. 2020;21(14) doi: 10.3390/ijms21145094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.J., Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ. Behav. 2020 doi: 10.1177/1090198120929677. 1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert D. Zero-inflated Poisson regression, with an application to defects in manufacturing. Technometrics. 1992;34(1):1–14. [Google Scholar]
- Langenberg C., Kuh D., Wadsworth M.E., Brunner E., Hardy R. Social circumstances and education: life course origins of social inequalities in metabolic risk in a prospective national birth cohort. Am. J. Publ. Health. 2006;96(12):2216–2221. doi: 10.2105/AJPH.2004.049429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav, Spec No. 1995:80–94. https://www.ncbi.nlm.nih.gov/pubmed/7560851 [PubMed] [Google Scholar]
- Link B.G., Phelan J. In: Handbook of Medical Sociology. sixth ed. Bird C.E., Conrad P., Fremont A.M., Timmermans S., editors. Vanderbilt University Press; Nashville, TN: 2010. Social conditions as fundamental causes of health inequalities; pp. 3–17. [Google Scholar]
- Mackenbach J.P., Cavelaars A., Kunst A.E., Groenhof F. Socioeconomic inequalities in cardiovascular disease mortality. An international study. Eur. Heart J. 2000;21(14):1141–1151. doi: 10.1053/euhj.1999.1990. [DOI] [PubMed] [Google Scholar]
- Meng L., Qiu H., Wan L., Ai Y., Xue Z., Guo Q.…Xiong L. Intubation and ventilation amid the COVID-19 outbreak: wuhan's experience. Anesthesiology. 2020;132(6):1317–1332. doi: 10.1097/aln.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C.…Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J. Am. Med. Assoc. 2020;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J. Health Soc. Behav. 2010;51(1 Suppl. l):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Polonijo A.N., Carpiano R.M. Social inequalities in adolescent human papillomavirus (HPV) vaccination: a test of fundamental cause theory. Soc. Sci. Med. 2013;82:115–125. doi: 10.1016/j.socscimed.2012.12.020. [DOI] [PubMed] [Google Scholar]
- Reluga T.C. Game theory of social distancing in response to an epidemic. PLoS Comput. Biol. 2010;6(5) doi: 10.1371/journal.pcbi.1000793. e1000793-e1000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen-Crowe B., McKenney M., Elkbuli A. Social distancing during the COVID-19 pandemic: staying home save lives. Am. J. Emerg. Med. 2020;38(7):1519–1520. doi: 10.1016/j.ajem.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer A., Morley E.J., Meyers K., Fernandes R., Rowe A.L., Viccellio P.…Henry M.C. Cohort of 4404 persons under investigation for COVID-19 in a NY hospital and predictors of ICU care and ventilation. Ann. Emerg. Med. 2020 doi: 10.1016/j.annemergmed.2020.05.011. (Forthcoming) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G., Miller B., Hankey B. Changing area socioeconomic patterns in US cancer mortality, 1950-1998: Part II--Lung and colorectal cancers. J. Natl. Cancer Inst. 2002;94(12):916–925. doi: 10.1093/jnci/94.12.916. [DOI] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A.…Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan S.Y., Ponstein N. Jonas Salk (1914-1995): a vaccine against polio. Singap. Med. J. 2019;60(1):9–10. doi: 10.11622/smedj.2019002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D.S., Phillips B.D., Lovekamp W.E., Fothergill A. CRC Press; 2013. Social Vulnerability to Disasters. [Google Scholar]
- Thorpe R.J., Fesahazion R.G., Parker L., Wilder T., Rooks R.N., Bowie J.V.…LaVeist T.A. Accelerated health declines among african Americans in the USA.(Report) J. Urban Health. 2016;93(5):808. doi: 10.1007/s11524-016-0075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Collins C.J., h r P. 2016. Racial Residential Segregation: a Fundamental Cause of Racial Disparities in Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.T., Leung K., Bushman M., Kishore N., Niehus R., de Salazar P.M.…Leung G.M. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat. Med. 2020;26(4):506–510. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020;45(8) doi: 10.1016/j.cpcardiol.2020.100618. 100618-100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z.…Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.