Children of mothers with depression have elevated rates of healthcare utilization compared to children of non-depressed mothers.1 Mindfulness-based interventions are associated with lower use of healthcare services among adults2 and decreased maternal depression during the perinatal period.3 No research has explored the potential moderating role of mindfulness-based treatment on the positive relation between maternal depression and offspring healthcare utilization. We hypothesized that a prenatal mindfulness intervention would attenuate the relation between maternal depressive symptoms and infant healthcare utilization during the first year of life.
Data were drawn from a quasi-experimental study that enrolled overweight and obese pregnant women in a mindfulness-based intervention (Mindful Moms Training; MMT) or treatment as usual (TAU) during the second trimester of pregnancy.4 Women who begin pregnancy overweight or obese have a higher likelihood of developing perinatal depression,5 a risk factor that may be compounded by the sociodemographic characteristics of our sample. Women in the current study were ethnically diverse (40.2% = African American, 33.3% = Latina, 12.8% = White, 13.7% = Other/Multiracial) and predominantly low-income (median income of $19,000, Range $0 - $98,000). A subsequent study followed the infants of women who participated in the original project6 (49.6% female, M gestational age = 39.6 weeks, SD = 1.4). Healthcare utilization data was collected for 118 offspring (68 infants of women in MMT and 49 infants of women in TAU).
In previous analyses with this sample, latent profiles of perinatal maternal depressive symptoms were derived using continuous PHQ-9 scores collected during the third trimester of pregnancy, 6 months postpartum, and 18 months postpartum.7 Women in the present study were classified into one of three profiles of perinatal depression: none/minimal symptoms (24%), mild symptoms (53%), or moderate symptoms (24%). By uncovering heterogeneous subgroups of depressive symptom severity, latent profile analysis is more advantageous than creating a singular average depressive symptom score across the sample.8
Healthcare utilization data were abstracted from children’s medical records. Emergency room and primary care provider visits were averaged (M = 10.8, SD = 4.6, Range = 3–32) given research suggesting that lower income families disproportionately rely upon emergency room services for routine and preventive care healthcare. To contextualize healthcare utilization, we compared our rates to the American Academy of Pediatrics (AAP) recommendations for eight healthcare visits for children from birth through 12 months of age for growth monitoring, screenings, and immunizations.9
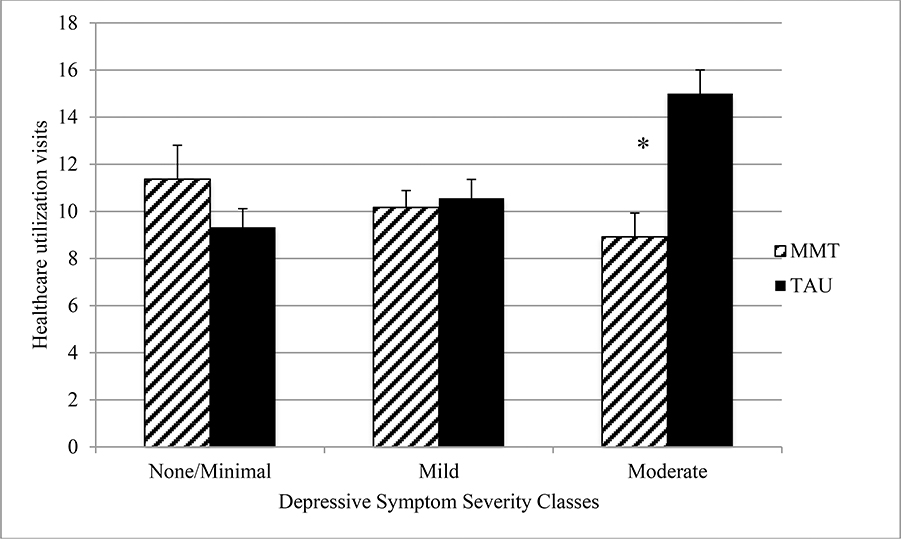
The interaction of maternal depressive symptom profile and intervention group on healthcare utilization was modeled using linear regression (rather than Poisson due to the high mean of our outcome) controlling for percent of poverty level, maternal education, race/ethnicity, infant gestational age at birth. There was no main effect of the intervention on healthcare utilization (p = .50), however depression profile interacted with intervention group to predict offspring utilization (interaction b = −7.16, SE = 2.54, p < .01; See Table 1 in Supplementary Materials). Participation in MMT during pregnancy attenuated the association between moderate maternal depressive symptom severity and utilization of healthcare services for infants. Among women in the moderate severity profile who received TAU, the mean number of healthcare visits was 15.0 (SD = 3.79). Among women in the moderate severity profile who received MMT, the mean number of infant healthcare visits was 8.93 (SD = 3.77), approximately 40% lower than TAU participants and a rate more consistent with the AAP-recommended eight visits (see Figure 1).
Figure 1. Average number of children’s healthcare visits and standard errors by depressive symptom severity profile and treatment group assignment.
Note. MMT = Mindful Moms Training, TAU = Treatment as usual. *p < .05
The influence of mothers’ enrollment in a mindfulness-based intervention on infant healthcare utilization adds to growing literature of the benefits of prenatal mindfulness training for health outcomes.3 Mindfulness may serve as a healthy cognitive and behavioral coping tool for new mothers, combating depression-related deficits in maternal self-efficacy that can lead to increased reliance on healthcare professionals for guidance when children are ill.10
Limitations include a focus on depressive symptoms and healthcare usage in terms of physician visits, precluding generalizability to women with clinical diagnoses of depression or to other types of healthcare services (e.g., inpatient hospitalizations, specialty care). The present research was also an early proof-of-concept pilot study of efficacy and did not utilize random assignment, which limits the causal inferences we may draw from our results.
In summary, the present study found an attenuation of the higher rates of infant healthcare utilization among a high-risk sample of women with moderate depression after participation in a prenatal mindfulness-based intervention. Incorporating screening and referral of maternal mental health problems into obstetric and pediatric healthcare settings may contribute to wide-ranging benefits for mothers, infants, and resource utilization.
Supplementary Material
Acknowledgments
Funding Sources: The work was supported by the National Heart, Lung, and Blood Institute (U01 HL097973; R01 HL116511-02); the Robert Wood Johnson Health and Society Scholars Program; the Lisa and John Pritzker Family Foundation; UCSF-CTSI UL1 TR000004; the UCSF Pathways to Discovery Summer Research Program; salary support to Dr. Felder from the California Preterm Birth Initiative post-doctoral fellowship, funded by Marc and Lynne Benioff, and a National Institute for Mental Health T32 grant (MH019391); salary support to Dr. Roubinov provided from the Canadian Institute for Advanced Research awarded to W.T. Boyce.
Abbreviations:
- AAP
American Academy of Pediatrics
- LPA
latent profile analysis
- MMT
Mindful Moms Training
- TAU
treatment as usual
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
References
- 1.Farr SL, Dietz PM, Rizzo JH, et al. Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatric and perinatal epidemiology. 2013;27(1):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth B, Stanley T-W. Mindfulness-based stress reduction and healthcare utilization in the inner city: preliminary findings. Alternative therapies in health and medicine. 2002;8(1):60. [PubMed] [Google Scholar]
- 3.Taylor BL, Cavanagh K, Strauss C. The Effectiveness of Mindfulness-Based Interventions in the Perinatal Period: A Systematic Review and Meta-Analysis. PloS one. 2016;11(5):e0155720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman-Phox K, Laraia BA, Adler N, Vieten C, Thomas M, Epel E. Peer reviewed: recruitment and retention of pregnant women for a behavioral intervention: lessons from the Maternal Adiposity, Metabolism, and Stress (MAMAS) study. Preventing chronic disease. 2013;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molyneaux E, Poston L, Ashurst-Williams S, Howard LM. Obesity and mental disorders during pregnancy and postpartum: a systematic review and meta-analysis. Obstetrics and gynecology. 2014;123(4):857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bush NR, Jones-Mason K, Coccia M, et al. Effects of Pre- and Post-natal Maternal Stress on Infant Temperament and Autonomic Nervous System Reactivity and Regulation In a Diverse, Low-Income Population. Development and Psychopathology. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felder J, Roubinov D, Bush NR, et al. Effect of prenatal mindfulness training on depressive symptom severity through 18-months postpartum: A latent class analysis. revise and resubmit. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung T, Wickrama K. An introduction to latent class growth analysis and growth mixture modeling. Social and personality psychology compass. 2008;2(1):302–317. [Google Scholar]
- 9.Workgroup BFPS, Practice Co, Medicine A. 2014 Recommendations for pediatric preventive health care. Pediatrics. 2014;133(3):568–570. [DOI] [PubMed] [Google Scholar]
- 10.Holland ML, Yoo B-K, Kitzman H, Chaudron L, Szilagyi PG, Temkin-Greener H. Self-efficacy as a mediator between maternal depression and child hospitalizations in low-income urban families. Maternal and child health journal. 2011;15(7):1011–1019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.