Abstract
Background:
The quality of peer relations is linked to mental health in childhood and adolescence, but few studies have investigated its clinical relevance. In particular, the potential mediating role of peer functioning in the associations between different dimensions of symptoms and quality of life (QoL) has not been sufficiently examined.
Objective:
In a clinical sample of adolescents, we examined peer relations in light of psychiatric diagnoses, as well as QoL and symptoms of mental health problems, with particular focus on symptoms of anxiety, depression, and ADHD. We also examined the potential mediating role of peer problems in the relationship between such symptoms and QoL.
Methods:
The sample consisted of 603 adolescents (ages 13-18) referred to clinical assessment. Psychiatric diagnoses according to the criteria of the International Statistical Classification of Diseases and Related Health Problems, 10th revision, were collected from participants’ clinical charts. Symptoms of disorders, QoL, and quality of peer relations were measured by self-report questionnaires.
Results:
Adolescents diagnosed with anxiety/depressive disorder reported more peer problems and lower QoL than adolescents with attention deficit/hyperactivity disorder. These findings were supported with symptom ratings. A path model with bootstrapping was used to assess the potential mediating role of peer problems in the association between symptoms and QoL, showing that peer problems partly mediated the relationship between emotional symptoms and QoL, but not the relationship between ADHD-symptoms and QoL.
Conclusion:
Improvement of peer relations may be a fruitful path for enhancing QoL among adolescents with symptoms of anxiety and depression.
Keywords: Life satisfaction, adolescence, symptoms, peer problems, mediation
Introduction
Recent research has illuminated that psychiatric problems may not only be understood in terms of symptoms and/or diagnoses, but also as self-evaluated quality of life (QoL). Whereas clinical symptoms and impairments are more or less objective outcome measures, QoL is on the other hand regarded as a more subjective measure. As such, the diagnostic approach and the QoL approach may distinguish between how an individual is and feels (1). Studies have shown that an improvement in QoL (feels) is attainable without reducing his/her psychiatric symptoms (is) and vice versa (2). Hence, improving QoL may be a crucial treatment aim, particularly with regard to persisting psychiatric problems. Moreover, among children and adolescents, problematic friendships and relationships with peers have repeatedly been shown to undermine well-being, and to exacerbate mental health adversities, both in proximal terms (3, 4) and as long-term effects spanning into adulthood (5, 6). It is thus conceivable that peer relations may be of importance for QoL among adolescents with mental health challenges. Hence, the main focus of the present study was the role of peer problems in the relationships between anxiety/depression and QoL, as well as hyperactivity/inattention and QoL, among adolescents referred to specialist mental health services.
The quality of life and psychiatric problems
Although there are many definitions of QoL, the construct is commonly accepted as multi-dimensional, including physical, psychological, and social dimensions (1). QoL is defined as “the subjective reported well-being in regard to an adolescent’s physical and mental health, self-esteem, perception of his/her own activities (playing/having hobbies), perceived relationship with his/her friends, family and school, and his/her global evaluation of life” (7, 8). Previous studies have indicated that children and adolescents with psychiatric problems have a lower QoL than children and adolescents who are healthy and those who have chronic somatic illnesses (8-12). However, findings are inconsistent with regard to whether various psychiatric disorders are related to QoL outcomes in different ways. Some studies show few or no differences in overall QoL between the various diagnostic categories (11, 13, 14), whereas other studies find internalizing problems to be associated with a lower QoL than externalizing problems (15-17). These inconsistencies may be due to actual differences or to methodological weaknesses, such as the assessment of psychiatric diagnoses vs symptoms, a lack of control for item overlap, a lack of control for medication, and the use of different respondents (usually children vs parents) (12, 14). Nevertheless, the few studies that control for item overlap or medication use, indicate lower levels of QoL among children with mental health problems than among those with somatic problems (12) and lower QoL in children with internalizing problems compared to children with externalizing problems (15, 17). In fact, these previous studies reporting a difference between internalizing and externalizing problems have been based on symptom scores and not psychiatric diagnoses. In contrast, all studies reporting no differences have been based on clinical diagnoses. To the best of our knowledge, no previous studies have compared how internalizing and externalizing problems measured by diagnoses and those measured by symptom severity are related to QoL.
The potential mediating role of peer problems
It is well established that psychiatric problems among adolescents are related to a reduced QoL (3-6). However, few studies have examined social factors that may influence this association and thus may be considered alternative, or indirect, paths toward better psychological health. One study, evaluating 252 Dutch children (ages 8-18 years) referred to outpatient child psychiatric clinics, found that better social support and family functioning were associated with higher QoL (18). However, this study did not differentiate between internalizing and externalizing problems. A more recent study of 120 German children and youths (aged 6-18 years) commencing outpatient psychotherapy treatment found that family functioning was related to QoL both among children with internalizing and externalizing problems (17). This study focused on family factors and did not assess whether social relationships outside the family, such as peer relations, affected the association between QoL and psychiatric problems. A 3-year longitudinal study of 1,554 German children and adolescents from a community sample, aged 11 to 17 at baseline, showed social support to be associated with better QoL, but social support did not moderate a negative association between mental health problems and QoL (19). These studies did not examine whether any of these factors mediated the association between mental health and QoL. However, another German community study of 2,517 adolescents and adults (ages 14-91) did find that the association between self-reported ADHD-symptoms and life satisfaction was partly mediated by social support (20). Examining these relationships in clinical samples are needed as symptoms may be more severe in such samples.
Problematic peer relationships in childhood and adolescence are associated with more internalizing and externalizing problems (21-25). Several longitudinal studies have detected reciprocal relationships in which problems related to peer functioning and problems related to anxiety/depression and hyperactivity/inattention reinforce each other through “vicious cycles” (23, 24, 26-29). For example, early signs of psychopathology may cause children to behave in ways that result in peer rejection (30). Children with ADHD are more often rejected by their peer group due to negative interactions with others or negative attributions by others (31, 32). Their social challenges may be caused by deficits in social skills or social problem-solving, which lead to inappropriate or intrusive behaviors in social situations (33). Conversely, poor peer functioning may predict an increase in ADHD-symptoms (34). Furthermore, peer problems among children with externalizing problems may lead to internalizing problems over time (23). These findings demonstrate that peer problems may be likely to influence the QoL of adolescents with symptoms of anxiety/depression and hyperactivity/inattention.
The present study
Recent research has pinpointed peer relations as a crucial factor for the development of mental health in childhood and adolescence. However, few studies have studied the role of peer functioning in QoL among adolescents with mental health problems. Furthermore, no known studies have examined the role of peer relations in the association between QoL and internalizing or externalizing problems among adolescents in a clinical setting. Hence, whether peer relations can exacerbate poor QoL in adolescents with such problems remains unclear. First, we compared whether diagnoses of depression/anxiety and ADHD and self-reported symptoms were associated with QoL differently. Second, we observed the correlations between self-reported symptoms, QoL, and peer problems. Third, we tested a path model consisting of symptoms of disorders, peer problems, and QoL, where symptoms were defined as predictors, QoL as the outcome variable, and peer problems as the intermediate variable.
Methods
Study design
The study is part of The Health Survey of the Department of Child and Adolescent Psychiatry (CAP), St. Olav’s University Hospital, Trondheim, Norway. This clinic provides diagnostic assessment and treatment for all psychiatric conditions in referred children and adolescents (ages 0-18 years). This was a cross-sectional study of a defined clinical population. The inclusion criteria were being a referred adolescent (ages 13-18 years) who had attended the clinic at least once between February 2009 and February 2011. Exclusion criteria were presenting major difficulties in answering the questionnaire due to psychiatric state, cognitive function, visual impairments, or a lack of sufficient language skills. Emergency patients were invited to participate once they entered a stable phase.
Study procedure
Newly referred patients and patients already enrolled at the CAP clinic received verbal and written invitations during their first visit after the project started. Written informed consent was obtained from adolescents and their parents prior to inclusion, in accordance with the CAP survey procedures. The participating adolescents responded to an electronic questionnaire about their mental and physical health in conjunction with a clinic appointment, without the presence of their parents. Participants accessed the questionnaire via a password-protected website. A project coordinator provided assistance if needed. In addition, psychiatric diagnoses were collected from patients’ clinical charts. These diagnoses were issued by a clinical psychologist or child/adolescent psychiatrist, after a consensus discussion, in accordance with the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10), multi-axial diagnostics (axes I-VI) (35). The clinic follows standardized procedures for the assessment and diagnosis of adolescent psychiatric disorders.
Study population
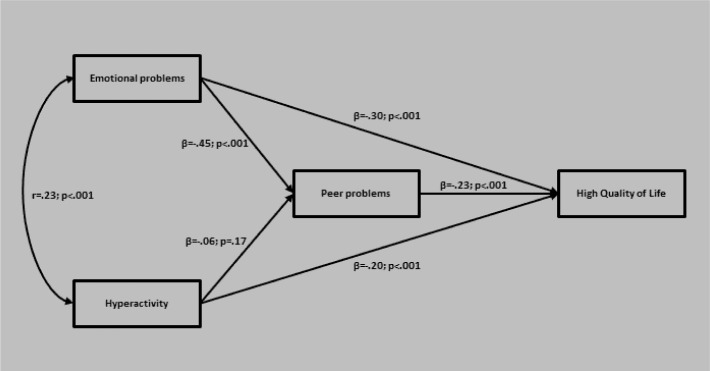
In the study period, 2,032 adolescent patients attended the CAP clinic at least once. Of these patients, 289 were excluded on the basis of the exclusion criteria, and 95 were lost to registration. Hence, 1,648 (81.1%) were eligible and were invited to participate. Of these patients, a total of 717 (43.5%) participated in the CAP survey, 393 (54.8%) girls and 324 (45.2%) boys.
To explore the representativeness of the participants, anonymous information about all adolescent patients at the clinic in the study period (n = 2,032) minus those excluded (n = 289) was collected from annual reports of St. Olav’s University Hospital, 2009–2011. In accordance with the permission given by The Data Protection Official for Research of the Norwegian Social Science Data Services, we compared the age, sex and main reason for referral between the participants (n = 717) and non-participants (n = 1,026). Participants were 0.27 (95% CI: 0.10-0.45) years older than non-participants (mean (SD): 15.66 (1.65) vs 15.39 (1.95), p = 0.0015). There were more girls in the study group than in the non-participating group (393 (54.8%) vs 509 (49.6%), p = 0.032). The main reason for referral did not differ between participants and non-participants (data not shown; Pearson’s exact χ2 test: p = 0.11).
Measures
Quality of life
QoL was measured using the Norwegian self-report version (36) of the Inventory of Life Quality in Children and Adolescents (ILC) (37). This instrument consists of seven items: six items address the adolescent’s functioning in school, relationships with his/her parents, siblings, and friends, activities when alone, physical health, and mental health, and one item addresses the adolescent’s global evaluation of his/her QoL. Each item is rated on an ordinal scale (1=very poor; 5=very good), and the values are summed to yield a score between 0 and 28 (0=very low QoL, 28=very high QoL). In the present study, all seven items were used. The ILC has been shown to have satisfactory reliability and validity in samples of Norwegian adolescents (36),with a Cronbach’s alpha of 0.84 in the present study, indicating good internal consistency.
Psychiatric problems
Emotional problems, hyperactivity/inattention problems, and peer problems were measured using the Norwegian self-report version (38) of the Strengths and Difficulties Questionnaire (SDQ) (39). This instrument consists of 25 items assessing emotional problems, conduct problems, hyper-activity/inattention problems, peer problems, and a prosocial scale. In the present study, the subscales measuring emotional problems, hyperactivity/ inattention problems, and peer problems were used. These three subscales of the SD have been shown to have adequate reliability and validity for use with samples of Norwegian adolescents, with Cronbach’s alphas ranging between 0.60 and 0.70 (40, 41).
Psychiatric diagnoses
Clinical diagnoses were based on ICD-10. Diagnoses of primary anxiety/depressive disorder (F40-41, F32-34, F38-39, F93.0, F93.1, F93.2) and hyperkinetic disorder (F90) hereafter called ADHD) were collected from clinical charts.
Statistics
Individuals above the age of 18 years were excluded from further analyses due to the small proportion of patients this age in the sample (n = 16; 2.2%), which reduced the sample to 701 participants. Furthermore, following the ILC manual (37), respondents with incomplete responses on more than four of the seven items were excluded from further analyses (n = 11; 2.0%). After their exclusion, missing values ranged from 0.6 to 1.9% across the seven items. A total of 87 adolescents (12.6%) did not complete the Strengths and Difficulties Questionnaire (SDQ), resulting in a total sample size of 603 (see Figure 1). One item on the ILC assesses participants’ relationships with their friends (“How do you get along with other adolescents in your leisure time?”). To control for item overlap between this item of the ILC and the scale measuring peer problems, analyses were run both with and without that ILC item, but this did not affect the findings. Thus, the results from the analyses using the complete ILC scale are presented. Also, we estimated multigroup models separating girls and boys. However, no gender differences were found, and we therefore present results on the complete sample without stratification but with adjustment for gender as more girls than boys had anxiety/depressive disorder.
FIGURE 1.
Flowchart of participants in the present study
Descriptive analyses and t-tests were performed in IBM SPSS Statistics 22, whereas regression analyses and the proposed path model were tested in Mplus version 7 (42). Differences in QoL and peer problems among adolescents diagnosed with depression/anxiety and those diagnosed with ADHD were examined by t-tests because QoL and peer problems were approximately normally distributed. Cohen’s d was used as a measure of effect size. Differences in QoL and peer problems related to emotional symptoms vs hyperactivity/inattention symptoms were examined by one regression analysis with QoL and peer problems as dependent variables.
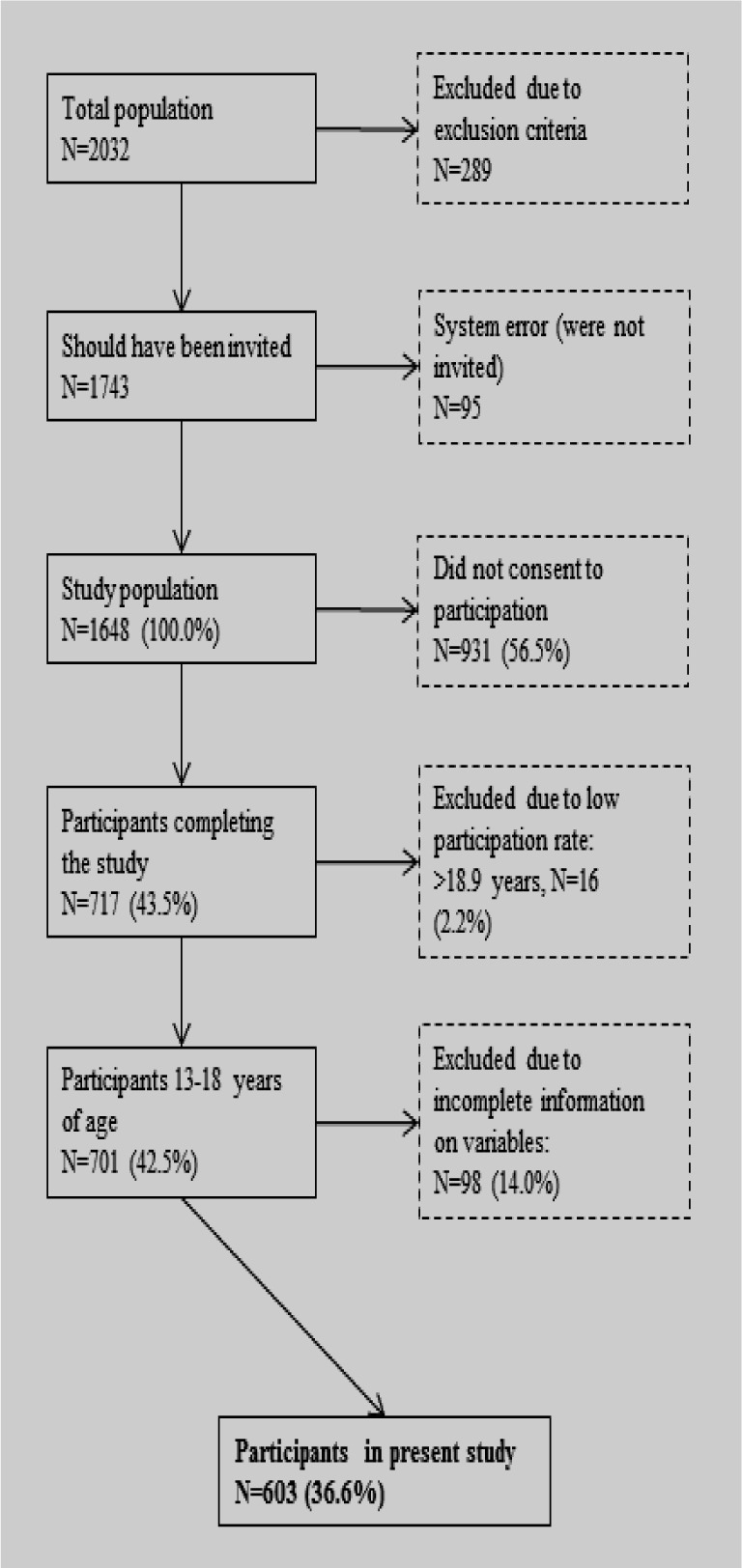
Differences between coefficients were tested with Wald tests. The mediating role of peer problems in the associations between emotional symptoms and QoL and between hyperactivity/inattention symptoms and QoL was assessed by a path model. In this model, emotional problems and hyperactivity/inattention symptoms were the independent predictor variables, and QoL was the dependent variable. Peer problems, which we hypothesized would function as a mediator of the relationship between psychiatric problems and QoL was an intermediate variable (see Figure 2). Additionally, the covariance between emotional symptoms and hyperactivity/inattention was freed because they overlapped in the preliminary analyses. Hence, all paths in the model were adjusted, e.g., that the effect of emotional problems on peer problems was controlled by the effect of hyperactivity/ attention problems on the same outcome, and vice versa. Furthermore, we added “sacks” for error variance in the model (e1 and e2). When estimating the indirect paths in the mediation model, we followed recommended procedures with 1,000 bootstrap samples with bias-correction (43). We noted that we tested a mediation model on cross-sectional data. The rationale for this was based on findings from previous empirical studies, which according to Hayes and Scharkow (44) is feasible. However, we emphasized that the method does not give grounds for causal interpretation.
FIGURE 2.
Path model with standardized coefficients and p-values
Results
In the sample of 603 adolescents, 108 (17.9%; 77.8% females; mean age (SE) = 16.2 [1.46]) fulfilled the criteria for a primary depressive or anxiety disorder (defined as ICD-10 codes F32, F33, F34, F38, F39, F40, F41, F93.0, F93.1 and F93.2), whereas 177 (29.4%; 42.9% females; mean age (SE) = 15.4 [1.59]) fulfilled the criteria for a primary diagnosis of ADHD (defined as ICD-10 code F90). Approximately 80% of the remaining participants received other diagnoses, most notably stress and adjustment disorders, obsessive-compulsive disorder, autism spectrum disorders, and eating disorders (45) On average, adolescents with anxiety/depressive disorders scored lower on QoL (M = 14.7, SE = 5.10) than adolescents with ADHD (M = 19.0, SE = 4.98). This difference was statistically significant with a large effect size (t(331) = −7.50, p < 0.001; d = 0.85). Furthermore, adolescents with anxiety/ depressive disorders reported more peer problems (M = 3.22, SE = 2.07) than adolescents with ADHD (M = 2.60, SE = 2.08). This difference was also statistically significant with a small to medium effect size (t(283) = 2.46, p < 0.001, d = 0.30).
Table 1 displays descriptive information and the correlations between variables. No correlations were high enough to indicate multicollinearity. Age and sex were significantly correlated with several of the problem variables and were thus adjusted for in the analyses.
TABLE 1.
Means, standard deviations, and correlations between study variables
| Range | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. QoL | 0-28 | 17.7 | 5.24 | - | |||||
| 2. Emotional symptoms | 0-10 | 4.66 | 2.65 | -0.511** | - | ||||
| 3. Hyperactivity symptoms | 0-10 | 5.47 | 2.36 | -0.291** | 0.231** | - | |||
| 4. Peer problems | 0-10 | 2.71 | 2.06 | -0.330** | 0.326** | 0.028 | - | ||
| 5. Age | 13.0-18.9 | 15.6 | 1.54 | -0.241** | 0.198** | 0.046 | -0.046 | - | |
| 6. Sex | 0=girl, 1=boy | 0.45 | 0.50 | 0.300** | -0.515** | -0.084* | -0.040 | -0.163** | - |
p < 0.05;
p < 0.01
Table 2 displays the results from the regression analyses that examined the relationships between QoL and symptom levels of emotional problems, hyperactivity/inattention, and peer problems. Wald tests of path differences revealed that adolescents scoring high on emotional problems had a significantly lower QoL than adolescents scoring high on hyperactivity/inattention symptoms (Wald test of parameter constraints (1) = 9.978, p = 0.002). Furthermore, adolescents scoring high on emotional symptoms also reported significantly more peer problems than adolescents scoring high on hyperactivity/inattention symptoms (Wald test of parameter constraints (1) = 54.023, p < 0.001). These findings on symptom scores therefore support the results of the examination of psychiatric diagnoses.
TABLE 2.
Results of regression analyses determining the relationships between disorder symptoms and quality of life and peer problems
| B | SE | β | p | |
|---|---|---|---|---|
| QoL | ||||
| Emotional problems | -0.798 | 0.080 | -0.403 | <0.001 |
| Hyperactivity problems | -0.411 | 0.077 | -0.185 | <0.001 |
| Age | -0.513 | 0.116 | -0.152 | <0.001 |
| Sex | 0.737 | 0.414 | 0.070 | 0.075 |
| Peer problems | ||||
| Emotional problems | 0.348 | 0.035 | 0.447 | <0.001 |
| Hyperactivity problems | -0.049 | 0.034 | -0.057 | 0.144 |
| Age | -0.138 | 0.051 | -0.104 | 0.007 |
| Sex | 0.698 | 0.183 | 0.169 | <0.001 |
Note. Unstandardized b, standard errors, and beta coefficients of linear regression analysis with QoL and peer problems as dependent variables and emotional hyperactivity problems, age, and sex as independent variables
The analyses of the path model are shown in Figure 2. More emotional problems and more hyperactivity/inattention symptoms were related to a poorer QoL (respective beta effects: β = −0.30, p < 0.001 and β = −0.20, p < 0.001). Moreover, emotional problems were negatively associated with peer problems (β = −0.45, p < 0.001), whereas hyperactivity/inattention symptoms were unrelated to peer problems when the effect of emotional problems was controlled for (β = −0.06, p = 0.17). Furthermore, peer problems were negatively associated with QoL (β = −0.23, p < 0.001), and finally, emotional difficulties were positively correlated with hyperactivity/inattention symptoms (r = 0.23, p < 0.001).
The hypothesis that peer problems may mediate and thus increase the effects of emotional problems and hyperactivity symptoms on poor QoL was confirmed with regard to the effect of emotional problems (indirect effect: β (95% BCBootstrap CI) = −0.10, (−0.15, −0.07) but not hyperactivity/ inattention symptoms (indirect effect: β (95% BCBootstrap CI) = 0.01, (−0.01, 0.03).
Discussion
In a large sample of adolescent outpatients, we investigated QoL in relation to mental health problems and peer relations. Foremost, when analyzing adolescents with clinically assessed diagnoses, the results revealed that adolescents with a primary diagnosis of anxiety/depressive disorder reported lower QoL and more peer problems than adolescents with a primary diagnosis of ADHD. These findings were also replicated when symptom ratings were employed. Adolescents scoring high on emotional symptoms reported a significantly lower QoL and more peer problems than adolescents scoring high on hyperactivity/inattention symptoms. Peer problems were not significantly related to hyperactivity/inattention problems, whereas peer problems partly mediated the relationship between emotional symptoms and QoL.
First, the present study does not confirm previous findings indicating no differences in overall QoL between diagnostic categories (11, 13, 14). Rather, our study supports the studies based on symptom scores that have found internalizing problems to be more negatively associated with QoL than inattention/hyperactivity problems (15-17). Compared to previous studies reporting no differences in QoL between diagnostic categories, the present study did find such difference. However, the anxiety/depression and ADHD diagnostic groups were larger in this study than in previous studies (11, 13), which may have contributed to the differences observed. A larger sample size may thus be required to uncover such differences when research is based on clinically assessed diagnoses rather than symptom measures. Moreover, many of the adolescents with ADHD in this sample were medicated for their ADHD, which could have been relevant for the observation of a higher QoL among these adolescents, but a previous study based on the same sample found that medication did not significantly affect QoL or emotional symptoms (46).
Second, adolescents with emotional problems also reported more peer problems than adolescents with hyperactivity/inattention problems. Although previous studies have indicated that peer problems are related to depressive symptoms and ADHD-symptoms (29, 34, 47, 48), few studies have compared the subjective perception of peer problems in the two diagnostic categories. Adolescents with ADHD may overestimate their social competence (49) despite having fewer friends and experiencing more peer rejection than adolescents without ADHD (22). This overestimation might explain why hyper-activity/inattention problems were not related to peer problems in the present study. On the other hand, emotional problems were significantly related to peer problems; this finding supports studies showing that maladaptive evaluations of peer relationships and peer-related loneliness are associated with depressive symptoms (21, 47). Furthermore, reduced energy and activity are core symptoms of depressive diagnoses, whereas increased energy and activity are core symptoms of ADHD (50). These factors are important for social activity and may explain why adolescents with emotional problems report more peer problems than adolescents with hyperactivity/inattention problems. To avoid potentially biased self-reports due to emotional or hyperactivity/inattention problems in participants, our findings should therefore be confirmed in studies employing observational or multi-informant designs.
Third, the measurement of peer problems was found to partially mediate the association between emotional problems and QoL, but not the association between hyperactivity/inattention problems and QoL. This is an important contribution to previous research because few studies have considered factors that may affect the association between mental health problems and QoL, and to the best of our knowledge, only one community study has investigated and found that social support partially mediates the association between symptoms of ADHD and QoL (20). However, the present study did not confirm this finding in a clinical sample examining peer problems as a mediator. This may be explained by ADHD-symptoms being more severe in clinical samples or that this finding does not apply to adolescent samples, as the participants in the previous study were predominantly adults. The fact that peer problems partially mediated the relationship between emotional problems and QoL is also in accordance with findings showing that negative social interactions and friendship quality are strong predictors of QoL and well-being (51, 52). Furthermore, this result aligns with studies showing a reciprocal relationship between emotional problems and peer problems (24, 26, 28). Our finding indicates that peer relations influences the relationship between emotional problems and QoL, and thus seems to be of particular importance for adolescents with such problems. Thus, treatment efforts could be aimed at improving peer relations to enhance the QoL of adolescents struggling with anxiety/depression. Peer problems did not mediate the association between hyperactivity/inattention symptoms and QoL, suggesting that differentiating between types of psychiatric problems is important when assessing factors assumed to affect the relationship between QoL and mental health.
Limitations
The present study has some notable limitations. The cross-sectional design of the study constitutes a limitation because this design does not allow causal inferences based on these data. Hence, our model does not imply that emotional problems lead to peer problems and thus to a low QoL; rather, it indicates that these problems are associated. Longitudinal studies would to a larger degree allow examinations of the potential reciprocal relationships between the measures examined in the present study. Therefore, all our findings should be confirmed in future prospective studies examining the role of peer relations for mental health problems and QoL.
Also, the present study was based solely on adolescent self-reports of peer problems and symptoms. As hyperactivity/inattention problems may affect self-evaluations positively, whereas emotional problems may affect such evaluations negatively, this may constitute a threat to our findings. Although self-evaluations most likely affect an individual’s QoL, future studies should include observational and/or multi-informant designs.
A quite low response rate was obtained in the study, which may affect the representativeness of the findings. Comparisons of the participants and non-participants in the study period revealed that participants were somewhat older and more often girls. Emotional problems are usually more common among girls, whereas hyperactivity problems tend to be more common among boys (53). Although we adjusted for sex in the analyses, the higher rate of female participants may have affected our findings. However, the main reason for referral, which was a variable with 16 categories coded according to a national classification system of suspected mental health problems, did not differ between participants and non-participants. This finding suggests that the participants were fairly representative of the clinical population with regard to presenting problems. The diagnoses of anxiety/depression and ADHD were based on clinical ICD-10 diagnoses rather than standardized semi-structured psychiatric interviews. Thus, we were not able to examine interrater reliability. However, the diagnoses were issued by experienced child/adolescent psychiatrists or clinical psychologists and were based on standard national and international guidelines. Also, information on comorbid disorders was considered beyond the scope of this paper, and was unfortunately not included. Differences in QoL and peer problems may therefore result from comorbid diagnoses although the diagnoses included in the present study were considered by the clinicians to be the patients’ primary problem/diagnosis, and hence main diagnosis. Furthermore, a minority of the participants were well enough to not receive a diagnosis, which naturally affects their responses. Finally, QoL and peer problems were measured by short scales. Therefore, examining different areas of QoL and peer problems was difficult and should be a future priority.
Clinical implications and future research
Our findings indicate that peer relations are important for QoL in adolescents with emotional problems. Peer relations may thus be an important target in both specific and general treatment of emotional problems. This was found in the present study of clinically referred adolescents, and will probably also apply for non-referred individuals who may struggle with emotional problems. Emotional symptoms are highly prevalent and comes in various degrees, and the majority of those affected do not receive specialist mental health services. These findings are therefore relevant for professionals in all arenas for young people, including family doctors, nurses, counselors, and last but not the least teachers and coaches who may be in a special position to influence peer relations.
Future research should explore the role of peer relations in various mental health problems further, preferably in prospective studies employing observational or multi-informant designs. Examining both mediating and moderating variables would be valuable, and one priority should be to examine the inconsistent findings on the relationships between peer problems, ADHD-symptoms, and QoL. Another important point for future studies will be to account for comorbid problems or disorders, and to examine different dimensions of QoL and peer problems. Finally, to study the effect of intermediate factors in the development of mental health problems could bring important knowledge and new target points for intervention, as indicated by our findings of the relationships between emotional symptoms, peer problems, and QoL.
Conclusions
Although successful social functioning has been shown to affect the development of mental health among children and adolescents, few studies have investigated this in a clinical setting. In the present study, carried out among clinical outpatients in Norway, we found that peer problems were associated with poorer QoL, and this was in particular observed among adolescents with emotional problems. Both the categorical assessment of psychiatric diagnoses and the continuous assessment of symptoms produced this finding. Thus, improving the QoL of adolescents with emotional problems is particularly important. Also, peer problems partly mediated the relationship between emotional problems and QoL. As such, the present findings have clinical significance, in that improving peer relations may be an important target in enhancing the QoL of adolescents struggling with emotional problems.
Acknowledgement
The authors thank the participants of the CAP survey.
Footnotes
Ethical approval and consent to participate and publication
Written informed consent was obtained from adolescents and parents prior to inclusion, in accordance with the study procedures in the CAP survey. Study approval was issued by the Regional Committees for Medical and Health Research Ethics (reference number CAP survey: 4.2008.1393, present study: 2014/1467) and by the Norwegian Social Science Data Services (reference number CAP survey: 19976).
All participants consented to the publication of anonymous results from the CAP survey.
Availability of data and material
The data sets generated and/or analyzed during the current study are not publicly available, in accordance with the permission given by the Regional Committees for Medical and Health Research Ethics (reference number CAP survey: 4.2008.1393, present study: 2014/1467).
Competing interests
The authors declare that they have no competing interests.
Funding
This study was financed by the Regional Centre for Child and Youth Mental Health and Child Welfare (RKBU), Faculty of Medicine, Norwegian University of Science and Technology, NTNU. The CAP survey is a product of the collaboration between St. Olav’s University Hospital and the Regional Centre for Child and Youth Mental Health and Child Welfare (RKBU). It is also funded by Unimed Innovation at St. Olav’s University Hospital and the Liaison Committee between the Central Norway Regional Health Authority and the NTNU.
Authors’ contributions
All authors contributed to the design of the study. IR, EG, and FS were responsible for the analyses and drafting of the manuscript. MSI was responsible for the data collection. All authors critically reviewed and approved the final manuscript.
References
- 1.Coghill D, Danckaerts M, Sonuga-Barke E, Sergeant J.. Practitioner review: quality of life in child mental health – conceptual challenges and practical choices. J Child Psychol Psychiatry 2009;50:544-61. [DOI] [PubMed] [Google Scholar]
- 2.Bastiaansen D, Koot HM, Ferdinand RF.. Psychopathology in children: improvement of quality of life without psychiatric symptom reduction? Eur Child Adolesc Psychiatry 2005;14:364-70. [DOI] [PubMed] [Google Scholar]
- 3.Zwierzynska K, Wolke D, Lereya TS.. Peer victimization in childhood and internalizing problems in adolescence: a prospective longitudinal study. J Abnorm Child Psychol 2013;41:309-23. [DOI] [PubMed] [Google Scholar]
- 4.Troop-Gordon W, Ladd GW.. Trajectories of peer victimization and perceptions of the self and schoolmates: precursors to internalizing and externalizing problems. Child Dev 2005;76:1072-91. [DOI] [PubMed] [Google Scholar]
- 5.Sakyi KS, Surkan PJ, Fombonne E, Chollet A, Melchior M.. Childhood friendships and psychological difficulties in young adulthood: an 18-year follow-up study. Eur Child Adolesc Psychiatry 2015;24:815-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modin B, Östberg V, Almquist Y.. Childhood peer status and adult susceptibility to anxiety and depression: a 30-year hospital follow-up. J Abnorm Child Psychol 2011;39:187-99. [DOI] [PubMed] [Google Scholar]
- 7.Jozefiak T, Larsson B, Wichstrøm L.. Quality of life as reported by school children and their parents: a cross-sectional survey. Health Qual Life Outcomes 2008;6:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jozefiak T, Larsson B, Wichstrøm L, Wallander J, Mattejat F.. Quality of Life as reported by children and parents: a comparison between students and child psychiatric outpatients. Health Qual Life Outcomes 2010;8:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P.. Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry 2002;41:530-7. [DOI] [PubMed] [Google Scholar]
- 10.Escobar R, Soutullo CA, Hervas A, Gastaminza X, Polavieja P, Gilaberte I.. Worse quality of life for children with newly diagnosed attention-deficit/hyperactivity disorder, compared with asthmatic and healthy children. Pediatrics 2005;116:e364-e9. [DOI] [PubMed] [Google Scholar]
- 11.Bastiaansen D, Koot HM, Ferdinand RF, Verhulst FC.. Quality of life in children with psychiatric disorders: self-, parent, and clinician report. J Am Acad Child Adolesc Psychiatry 2004;43:221-30. [DOI] [PubMed] [Google Scholar]
- 12.Dey M, Mohler-Kuo M, Landolt MA.. Health-related quality of life among children with mental health problems: a population-based approach. Health Qual Life Outcomes 2012;10:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schubert M, Herle M, Wurst E.. ICD-10 Diagnostik und Lebensqualität: Pilotstudie zur Lebensqualität psychisch auffälliger Kinder und Jugendlicher. Z Kinder Jugendpsychiatr Psychother 2003;31:285-91. [DOI] [PubMed] [Google Scholar]
- 14.Dey M, Landolt MA, Mohler-Kuo M.. Health-related quality of life among children with mental disorders: a systematic review. Qual Life Res 2012;21:1797-814. [DOI] [PubMed] [Google Scholar]
- 15.Sharpe H, Patalay P, Fink E, Vostanis P, Deighton J, Wolpert M.. Exploring the relationship between quality of life and mental health problems in children: implications for measurement and practice. Eur Child Adolesc Psychiatry 2016;25:659-67. [DOI] [PubMed] [Google Scholar]
- 16.Thaulow CM, Jozefiak T.. A comparison between child psychiatric outpatients with AD/HD and anxiety/depression. Nord J Psychiatry 2012;66:396-402. [DOI] [PubMed] [Google Scholar]
- 17.Weitkamp K, Daniels JK, Romer G, Wiegand-Grefe S.. Health-related quality of life of children and adolescents with mental disorders. Health Qual Life Outcomes 2013;11:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bastiaansen D, Koot HM, Ferdinand RF.. Determinants of quality of life in children with psychiatric disorders. Qual Life Res 2005;14:1599-612. [DOI] [PubMed] [Google Scholar]
- 19.Otto C, Haller AC, Klasen F, Holling H, Bullinger M, Ravens-Sieberer U,. et al. Risk and protective factors of health-related quality of life in children and adolescents: Results of the longitudinal BELLA study. PLoS One 2017;12:e0190363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hennig T, Koglin U, Schmidt S, Petermann F, Brahler E.. Attention-deficit/hyperactivity disorder symptoms and life satisfaction in a representative adolescent and adult Sample. J Nerv Ment Dis 2017;205:720-4. [DOI] [PubMed] [Google Scholar]
- 21.Rudolph KD. The interpersonal context of adolescent depression In: Nolen-Hoeksema S, Hilt LM, (Eds.). Handbook of depression in adolescents. New York, NY: Routledge; 2009, pp. 377-418. [Google Scholar]
- 22.Bagwell CL, Molina BS, Pelham WE, Hoza B.. Attention-deficit hyperactivity disorder and problems in peer relations: predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry 2001;40:1285-92. [DOI] [PubMed] [Google Scholar]
- 23.van Lier PA, Koot HM.. Developmental cascades of peer relations and symptoms of externalizing and internalizing problems from kindergarten to fourth-grade elementary school. Dev Psychopathol 2010;22:569-82. [DOI] [PubMed] [Google Scholar]
- 24.Deater-Deckard K. Annotation: Recent research examining the role of peer relationships in the development of psychopathology. J Child Psychol Psychiatry 2001;42:565-79. [PubMed] [Google Scholar]
- 25.Ladd GW. Peer rejection, aggressive or withdrawn behavior, and psychological maladjustment from ages 5 to 12: an examination of four predictive models. Child Dev 2006;77:822-46. [DOI] [PubMed] [Google Scholar]
- 26.Hodges EV, Perry DG.. Personal and interpersonal antecedents and consequences of victimization by peers. J Pers Soc Psychol 1999;76:677-85. [DOI] [PubMed] [Google Scholar]
- 27.Stice E, Ragan J, Randall P.. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol 2004;113:155-9. [DOI] [PubMed] [Google Scholar]
- 28.Vernberg EM. Psychological adjustment and experiences with peers during early adolescence: reciprocal, incidental, or unidirectional relationships? J Abnorm Child Psychol 1990;18:187-98. [DOI] [PubMed] [Google Scholar]
- 29.Tseng W-L, Kawabata Y, Gau SS-F, Crick NR.. Symptoms of attention-deficit/hyperactivity disorder and peer functioning: a transactional model of development. J Abnorm Child Psychol 2014;42:1353-65. [DOI] [PubMed] [Google Scholar]
- 30.Parker JG, Asher SR.. Peer relations and later personal adjustment: are low-accepted children at risk? Psychol Bull. 1987;102(3):357-89. [DOI] [PubMed] [Google Scholar]
- 31.Hodgens JB, Cole J, Boldizar J.. Peer-based differences among boys with ADHD. J Clin Child Psychol. 2000;29(3):443-52. [DOI] [PubMed] [Google Scholar]
- 32.Hoza B. Peer functioning in children with ADHD. J Pediatr Psychol. 2007;32(6):655-663. [DOI] [PubMed] [Google Scholar]
- 33.Gardner DM, Gerdes AC.. A review of peer relationships and friendships in youth with ADHD. J Atten Disord 2015;19:844-55. [DOI] [PubMed] [Google Scholar]
- 34.Stenseng F, Belsky J, Skalicka V, Wichstrøm L.. Peer rejection and attention deficit hyperactivity disorder symptoms: reciprocal relations through ages 4, 6, and 8. Child Dev 2016;87:365-73. [DOI] [PubMed] [Google Scholar]
- 35.The World Health Organization.. International statistical classification of diseases and related health problems, 10 th revision Geneva: World Health Organization; 1992. [Google Scholar]
- 36.Jozefiak T, Mattejat F, Remschmidt H.. Inventory of life quality in children and adolescents manual, Norwegian version Stockholm: Hogrefe; 2012. [Google Scholar]
- 37.Mattejat F, Remschmidt H.. Das Inventar zur Erfassung der Lebensqualität bei Kindern und Jugendlichen (ILK) [The inventory of quality of life in children and adolescents (ILC)] Bern: Hans Huber Verlag; 2006. [PubMed] [Google Scholar]
- 38.Van Roy B, Grøholt B, Heyerdahl S, Clench-Aas J.. Self-reported strengths and difficulties in a large Norwegian population 10–19 years. Eur Child Adolesc Psychiatry 2006;15:189-98. [DOI] [PubMed] [Google Scholar]
- 39.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. [DOI] [PubMed] [Google Scholar]
- 40.Van Roy B, Veenstra M, Clench-Aas J.. Construct validity of the five-factor Strengths and Difficulties Questionnaire (SDQ) in pre-, early, and late adolescence. J Child Psychol Psychiatry 2008;49:1304-12. [DOI] [PubMed] [Google Scholar]
- 41.Kornør H, Heyerdahl S.. Psychometric properties of the Norwegian version of Strengths and Difficulties Questionnaire, self-report (SDQ-S). PsykTestBarn 2013;2:6. [Google Scholar]
- 42.Muthén LK, Muthén BO.. Mplus user’s guide 7th ed. Los Angeles, CA: Muthén & Muthén; 1998-2015. [Google Scholar]
- 43.Lau RS, Cheung GW.. Estimating and comparing specific mediation effects in complex latent variable models. Organ Res Methods 2012;15:3-16. [Google Scholar]
- 44.Hayes AF, Scharkow M.. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: does method really matter? Psychol Sci 2013;24:1918-27. [DOI] [PubMed] [Google Scholar]
- 45.Mangerud WL, Bjerkeset O, Lydersen S, Indredavik MS.. Chronic pain and pain-related disability across psychiatric disorders in a clinical adolescent sample. BMC Psychiatry 2013;13:272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schei J, Nøvik TS, Thomsen PH, Indredavik MS, Jozefiak T.. Improved quality of life among adolescents with attention-deficit/hyperactivity disorder is mediated by protective factors: a cross sectional survey. BMC Psychiatry 2015;15:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qualter P, Brown SL, Munn P, Rotenberg KJ.. Childhood loneliness as a predictor of adolescent depressive symptoms: an 8-year longitudinal study. Eur Child Adolesc Psychiatry 2010;19:493-501. [DOI] [PubMed] [Google Scholar]
- 48.Witvliet M, Brendgen M, Van Lier PA, Koot HM, Vitaro F.. Early adolescent depressive symptoms: prediction from clique isolation, loneliness, and perceived social acceptance. J Abnorm Child Psychol 2010;38:1045-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM.. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clin Child Fam Psychol Rev 2007;10:335-51. [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization (WHO).. The ICD-10 classification of mental and behavioural disorders Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (WHO); 1992. [Google Scholar]
- 51.Helgeson VS. Social support and quality of life. Qual Life Res 2003;12:25-31. [DOI] [PubMed] [Google Scholar]
- 52.Hartup WW, Stevens N.. Friendships and adaptation in the life course. Psychol Bull 1997;121:355-70. [Google Scholar]
- 53.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A.. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003;60:837-44. [DOI] [PubMed] [Google Scholar]