Abstract
Acute gastroenteritis is one of the major health problems in children aged <5 years around the world. Rotavirus A (RVA) is an important pathogen of acute gastroenteritis. The burden of rotavirus disease in the pediatric population is still high in Bangladesh. This study investigated the prevalence of group A, B, and C rotavirus (RAV, RBV, RCV), norovirus, adenovirus (AdV) and human bocavirus (HBoV) infections in children with acute gastroenteritis in Bangladesh from February 2014 to January 2019. A total of 574 fecal specimens collected from children with diarrhea in Bangladesh during the period of February 2014-January 2019 were examined for RAV, RBV and RCV by reverse transcriptase- multiplex polymerase chain reaction (RT- multiplex PCR). RAV was further characterized to G-typing and P-typing by RT-multiplex PCR and sequencing method. It was found that 24.4% (140 of 574) fecal specimens were positive for RVA followed by AdV of 4.5%. RBV and RCV could not be detected in this study. Genotype G1P[8] was the most prevalent (43%), followed by G2P[4] (18%), and G9P[8] (3%). Among other genotypes, G9P[4] was most frequent (12%), followed by G1P[6] (11%), G9P[6] (3%), and G11P[25] (3%). We found that 7% RVA were nontypeable. Mutations at antigenic regions of the VP7 gene were detected in G1P[8] and G2P[4] strains. Incidence of rotavirus infection had the highest peak (58.6%) during November to February with diarrhea (90.7%) as the most common symptom. Children aged 4–11 months had the highest rotavirus infection percentage (37.9%). By providing baseline data, this study helps to assess efficacy of currently available RVA vaccine. This study revealed a high RVA detection rate, supporting health authorities in planning strategies such as introduction of RVA vaccine in national immunization program to reduce the disease burden.
Introduction
Acute gastroenteritis (AGE) is one of the major burden of diseases in children in the developing and developed countries [1, 2]. Viruses are the main pathogen of AGE in children worldwide [1, 3–5]. The incidence of pediatric AGE has been reduced in the developed countries in recent years [1]. However, virus associated pediatric AGE is still a major health burden in developing countries [1, 2, 8]. Among enteropathogenic viruses, rotavirus A (RVA) (the family Reoviridae) is the main causative agent of pediatric AGE [1–3]. It is estimated that about 3–5 billion cases of pediatric AGE occur every year around the world. Every year about 3 million children die of AGE worldwide [4–8]. Rotavirus A has been reported as the main pathogen from about one million deaths associated with pediatric AGE [4–8]. The incidence of rotavirus is estimated to be 10,000 cases per 100,000 children in children below five years in Bangladesh. About 27% of rotavirus infected children develop severe health conditions. Rotavirus associated mortality is estimated to be 2000 to 3000 per year in Bangladesh [9].
Rotavirus is a nonenveloped virus having a genome of segmented double stranded RNA (dsRNA) of about 18.55 kilo base pairs [10]. The genome encodes for six structural proteins called VP1 to VP6 and six nonstructural proteins called NSP1 to NSP6 [10]. There are ten species of the genus Rotavirus, referred to as A, B, C, D, E, F, G, H, I and J [11]. Among them, RVA is the main human pathogen and causes 90% of the diseases, while RVB and RVC are also found to be involved in human diseases [12]. RVA is further classified in two genotypes called as G genotype from VP7 or glycoprotein of the virus and P genotype from VP4 or protease [11, 13]. About 36 rotavirus G types and 51 rotavirus P types have been reported [14, 15]. The most common G types are G1-G4, G9 and G12, whereas P[4], P[6] and P[8] are the most common P genotypes worldwide [14–17]. The most commonly found genotype combination of RVA in human are G1P[8], G2P[4], G3P[8], G4P[8] and G9P[8] [16–18]. In Bangladesh, the genotypic distribution of rotavirus has changed over the years. Rotavirus genotype G1P[8], G2P[4], G3P[8], G4P[8] and G9P[8] have been reported from children with acute gastroenteritis in Bangladesh [16–21].
Four rotavirus A vaccines (RotaTeq-Merck, Rotarix- GSK, ROTAVAC, and ROTASIIL) have been prequalified by WHO. India, Vietnam and China have developed rotavirus A vaccine for their own market [19, 22]. Global rotavirus vaccines are available in Bangladesh market but the vaccination program has not been included in the national immunization program yet [9, 19]. Rotavirus vaccine coverage in children under five is high in Bangladesh. For rotavirus vaccine, DTP1 is 97%, DPT2 is 95.5% and DTP3 is 94% in Bangladesh. A recent Rotarix trial in Bangladesh has revealed that vaccine efficacy is decreasing due to the mutational and reassortment events of rotaviruses [9]. Molecular analysis and genetic characterization of rotavirus A will specify diversity that will be an important tool to evaluate vaccine efficacy [23, 24].
The main aim of this study is to characterize the genotypes of rotavirus A in Bangladesh. First objective of this study is to describe the age distribution, gender distribution, seasonal pattern and genotypic distribution of rotavirus A among children in Bangladesh. Second objective of this study is to describe intragenotypic heterogeneity of rotavirus G1 circulating in Bangladesh.
Materials and methods
Study population and fecal specimens
Between February 2014 and January 2019, 574 fecal specimens were collected from children with acute gastroenteritis from four clinics in three different regions (Chattogram, Savar and Sirajganj) in Bangladesh. Each clinic located in each region, except for Savar with two clinics. All children aged <15 years with viral gastroenteritis (clinically suspected) were enrolled in the study. Samples were collected from pediatric patients with three or more watery non-bloody stools/24 hours. Non-infectious bloody diarrheal cases were excluded following WHO case standard guideline. The ages ranged from 55 days to 15 years with a mean age of 24 months. One fecal specimen was collected from each patient. Informed consent of the parents was taken before sample collection. Ten percent suspension of the fecal specimens were made and centrifuged at 10000x g for 10 min. All the specimens were stored at -20°C until further analysis.
Ethical approval
This study was ethically approved by the Biosafety, Biosecurity & Ethical Committee (BBEC) of Jahangirnagar University. Ethics committee approval number for this study is BBEC, JU/M 2020/(10)3.
Viral RNA and DNA extraction
Fecal suspensions were thawed and centrifuged at 10000x g for 10 min. Viral RNA was extracted using 140 μL of the supernatant by SV Total RNA Isolation System (Promega kit) according to the manufacturer’s protocols (Promega, Madison, USA). Viral DNA for adenoviruses and human bocaviruses was extracted following the established protocols in Sharif et al. (2020).
Complementary DNA (cDNA) synthesis by reverse transcription
For rotavirus and norovirus, cDNA was synthesized using Promega cDNA synthesis kit (Promega, Madison, USA). For reverse transcription (RT), 3 μL of extracted RNA (100 ng) was mixed with a reaction mixture, consisting of 1 μL of oligo dT primer (25 μg/ml) and 1 μL of nuclease free water in nanocentrifuge tube, kept at 70°C for 5 min and chilled for 5 min in ice. After that 4 μL of 5X reaction buffer, 2 μL of 5 mM MgCl2, 1 μL of 10 mM PCR Nucleotide Mix, 0.5 μL of ribonuclease inhibitor (1 u/ μL), 1 μL of reverse transcriptase, and 6.5 μL of nuclease free water were mixed for each sample in the same nanocentrifuge tube, containing 5 μL of previously chilled genomic RNA. Total volume of the mixture was 20 μL. The mixture was heated at 25°C for 5 min, 42°C for 60 min and 70°C for 15 min. The cDNA was prepared and stored at -20°C.
Polymerase chain reaction (PCR)
For rotavirus A, two specific primers F-1GGCTTTAAAAGAGAGAATTTC28 and R-373ACTGATCCTGTTGGCCATCCTTT395 were used to amplify VP7 gene. For norovirus, two specific primers F-5342CGCCGTGGCTCCTGCTCT5361 and R-5671GTTCGCCATCACAAAAGATGTG5653 were used to amplify VP1 gene. For adenovirus, two specific primers AD1-F 1834TTCCCCATGGCICAYAACAC1853 and AD2-R 2315CCCTGGTAKCCRATRTTGTA2296 were used to amplify hexon gene. For human bocavirus, two specific primers AK-VP-F1 3274CGCCGTGGCTCCTGCTCT3291 and AK-VP-R1 3860TGTTCGCCATCACAAAAGATGTG3876 were used to amplify VP1 gene [25]. The PCR reaction was performed at 94°C for 3 min, followed by 35 cycles of denaturation at 94°C for 1 min, annealing at 55°C for 1 min and extension at 72°C for 1 min. Final extension was done at 72°C for 7 min and then held at 4°C. PCR reaction mixture contained 12.5 μL of the 2X master mix (GoTaq®Green Master Mix, Promega, USA), 1 μL of 1 μM forward (F) primer, 1 μL of 1 μM reverse (R) primer, 6.5 μL of nuclease free water, and 4 μL of template (200 ng). For rotavirus and norovirus, 4 μL cDNA (200 ng) was used as template. Total volume of the PCR reaction mixture was 25 μL. Previously sequenced samples were used as positive controls. The PCR was performed in 2720 Thermal Cycler (Applied Biosystems, USA) [25].
Group A rotavirus G typing
Group A rotavirus G typing was conducted using the protocol from the previously described method [23]. Reverse transcription (RT) was performed for the full-length VP7 gene, and the first amplification was completed by using Beg9 and End9 primers. The second amplification was performed using the first PCR product as the template with G type-specific mixed primers 9T1-1, 9T1-2, 9T-3P, 9T-4, and 9T-B and forward primer 9con1 (9con1 is specific primer that is used to characterize G genotype). Amplicons of 158 bp, 224 bp, 466 bp, 403 bp, and 110 bp were specifically generated for G1, G2, G3, G4, and G9, respectively.
Group A rotavirus P typing
Group A rotavirus P typing was conducted using the protocol from the previously described method [23]. The first amplification of VP4 gene was completed by using Con2 and Con3 primers by RT-PCR. The second amplification was performed by using a mixture of primers 1T-1, 2T-1, 3T-1, 4T-1, 5T-1, and Con3 for the identification of P[8], P[4], P[6], P[9], and P[10], with amplicons of 346 bp, 484 bp, 268 bp, 392 bp, and 584 bp, respectively.
Agarose gel electrophoresis
The amplicons were electrophoresed using 1.5% agarose gel. The gel run was continued for 25 min horizontally. Separated amplicons were visualized using UV spectrophotometer (SPECORD-205, Analytik-Jena, Germany) and photographed in the Gel doc system (BioRad, USA).
Nucleotide sequence analysis
The nucleotide sequences of PCR amplicons positive for rotavirus A, norovirus, human bocavirus and adenovirus were determined with the Big-Dye terminator cycle sequencing kit and an ABI Prism 310 Genetic Analyzer (Applied Biosystems Inc. Foster City, CA) [25]. The sequences were analyzed using Chromas 2.6.5 (Technelysium, Helensvale, Australia). The sequence data were converted into FASTA format. Sequence homology was confirmed using the BLASTn (https://blast.ncbi.nlm.nih.gov/Blast.cgi) program. Multiple sequence alignment was performed in the BioEdit 7.2.6 software using the ClustalW Multiple Alignment algorithm [26]. The similarity matrix was computed using the Maximum Composite Likelihood model. The nucleotide sequence data of all Bangladeshi RVA had been submitted to the GenBank database.
Phylogenetic analysis
Phylogenetic and evolutionary relationship analysis of RVA was conducted using VP7 gene and the reference sequences by the MEGA X software [27]. Phylogenetic trees with 1000 bootstrap replicates of the nucleotide alignment datasets were generated. For calculating the genetic distance, Kaimura-2 parameter model was used. Maximum Composite Likelihood (MCL) method was used for phylogenetic relationship analysis [28]. The reference strains used for RAV phylogenetic analysis are provided in the S1 Chart.
Nucleotide sequence submission
The nucleotide sequence data used in this study had been submitted to the GenBank database and had been assigned accession number MN202241 and MT310555-MT310574.
Statistical analysis
Statistical analysis was conducted using IBM® SPSS® Statistics for windows, version 23.0 (IBM Corp. Armonk, New York, USA) software package. Prevalence of diarrheal pathogens were detected by dividing number of cases by total number of study children during the study period. Statistical analysis for phylogenetic data was calculated by kimura-2-parameter model in the MEGA X software [27, 28].
Results
Demographic characteristics of children with acute gastroenteritis
Demographic characteristics of 574 pediatric patients with acute gastroenteritis were analyzed. Among the pediatric patients, 55.6% (319 of 574) were male and 44.4% (255 of 574) were female. The study population was distributed into six age groups from 1 month to 60 months (1–3, 4–11, 12–23, 24–35, 36–47 and 48–60). Most of the patients (22.8%) belonged to 4–11 months group followed by other five age groups (Table 1). Among the pediatric patients, 69.2% (397 of 574) received primary treatment and fluid replacement, and 30.8% (177 of 574) didn’t receive any treatment at home.
Table 1. Demographic characteristics of patients who were enrolled in this study during 2014–2019 in Bangladesh.
| Factors | Group | Percentage |
|---|---|---|
| Gender | Male | 55.6% (319 of 574) |
| Female | 44.4% (255 of 574) | |
| Age group (months) | 1–3 | 14.9% (86 of 574) |
| 4–11 | 22.8% (131 of 574) | |
| 12–23 | 21.6% (124 of 574) | |
| 24–35 | 15.3% (88 of 574) | |
| 36–47 | 12.5% (72 of 574) | |
| 48–60 | 12.7% (73 of 574) | |
| Treatment conditions | Received at home | 69.2% (397 of 574) |
| At hospital | 30.8% (177 of 574) |
Detection of viruses associated with acute gastroenteritis in children
Among 574 fecal specimens, 36.8% (211 of 574) were positive for viral infection. RV was the most prevalent (24.4%, 140 of 574) followed by NoV (4.9%, 28 of 574), AdV (4.2%, 24 of 574) and HBoV (3.3%, 19 of 574), respectively [25]. About 63.2% (363 of 574) of the samples were tested negative for diarrheal viruses.
Coinfection of children with acute gastroenteritis
Frequencies of both monoinfection and coinfection of pediatric patients were determined. Infection of viruses was found in 75.4% (159 of 211) of the cases. Coinfection between viruses was found in 24.6% (52 of 211) of cases. Dual infection between RV and NoV accounted for most of the cases (10) of coinfection, followed by RV-AdV (6), RV-HBoV (4), NoV-AdV (3), NoV-HBoV (2) and AdV-HBoV (1).
Age and gender distribution of rotavirus among children with acute gastroenteritis
Viruses associated with acute gastroenteritis were detected in every group aged <60 months. Rotavirus was most prevalent (37.9%, 53 of 140) among children aged 4–11 months, followed by 12–23 months (22.1%, 31 of 140), 1–3 months (15.7%, 22 of 140), 24–35 months (15%, 21 of 140), 48–60 months (5%, 7 of 140), and 36–47 months (4.3% 6 of 140). The distribution of gender in rotavirus positive cases were 62.1% (87 of 140) in male, and 37.9% (53 of 140) in female. The ratio between rotavirus infected male and female was 1.6:1, but it was not significantly different.
Clinical features of acute gastroenteritis associated with rotavirus infection
Viruses associated with acute gastroenteritis were found to be involved with various clinical complications of the pediatric population. Among rotavirus infected patients, diarrhea (90.7%) was the most common, followed by dehydration (88.7%), vomiting (84.3%), fever (77.8%) and abdominal pain (67.1%) (Fig 1). Whereas diarrhea (85.7%) was the most frequent in the norovirus infected children, vomiting (87.5%) was the most common in the adenovirus infected children, and dehydration (94.7%) was the most common in the human bocavirus infected children.
Fig 1. Comparison of clinical features between rotavirus positive children and rotavirus negative children during 2014–2019 in Bangladesh.
Seasonal pattern of rotavirus infection
Rotavirus infection was detected all year round. But majority of rotavirus infection cases (58.6%) were found during the winter season (Nov-Jan), followed by 30.7% in the rainy season (May-Jul), 7.1% in the spring season (Feb-Apr), and 3.6% in the autumn season (Aug-Oct), respectively. During the winter season the average temperature was around 17°C. The incidence of rotavirus had a peak at a lower temperature in Bangladesh (Fig 2).
Fig 2. Seasonal pattern of rotavirus infection in infants and children with acute gastroenteritis along with correlation of rotavirus incidence with average temperature in Bangladesh during 2014–2019.
Distribution of G and P genotypes of group A rotavirus
Among the G genotypes, G1 was the most predominant (57%), followed by G2 (20%), G9 (20%) and G11 (3%). Four P genotypes were detected during 2014 to 2019 in Bangladesh. Rotavirus genotype P[8] was the most frequent (46%), followed by P[4] (30%), P[6] (14%) and P[25] (3%). In combination of rotavirus G and P genotype, great diversity was detected. Rotavirus genotype combination G1P[8] was the most prevalent (43%), followed by G2P[4] (18%), G9P[4] (12%), G1P[6] (11%), G9P[8] (3%), G9P[6] (3%) and G11P[25] (3%), respectively. 7% rotavirus was nontypeable (Table 2).
Table 2. Distribution of group A rotavirus G and P genotypes among children with acute gastroenteritis in Bangladesh during 2014–2019.
| G genotype | P genotype | Nontypable | Total of G and P combination (%) | |||
|---|---|---|---|---|---|---|
| P[8] | P[4] | P[6] | P[25] | |||
| G1 | 60 (43%) | - | 16 (11%)a | - | 4 (3%) a | 80 (57) |
| G2 | - | 25 (18%) | - | - | 3 (2%) a | 28 (20) |
| G9 | 4 (3%) | 17 (12%) | 4 (3%) a | - | 3 (2%) a | 28 (20) |
| G11 | - | - | - | 4 (3%) a | - | 4 (3) |
| Total | 64 (46%) | 42 (30%) | 20 (14%) a | 4 (3%) | 10 (7%) a | 140 (100) |
aUnusual G/P combinations are indicated in bold.
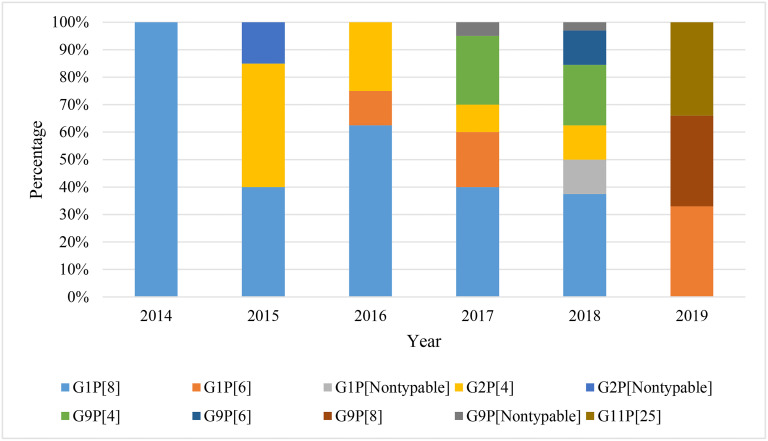
During the study period, rotavirus incidence was the highest in 2017 (28.6%), followed by 22.9% in 2018, 22.9% in 2016, 14.3% in 2015, 8.6% in 2019 and 2.9% in 2014. Genotype G1P[8] was detected in every year, but the highest incidence (33.3%) was found in 2016, followed by 26.7% in 2017, 20% in 2018, 13.3% in 2015 and 6.7% in 2014, respectively. Genotype G2P[4] was detected in the highest percentage (36%) in 2015, followed by 32% in 2016, 16% in 2017 and 16% in 2018, respectively. However, genotype G9P[4] was detected in the highest percentage (59%) in 2017. Genotype G1P[6] was detected in highest percentage (50%) in 2017, followed by 25% in 2016 and 25% in 2019, respectively. Genotype G1P[8] and G2P[4] were detected during 2014–2018, but none were detected in 2019. About 40% of nontypeable rotavirus was detected in 2018 (Fig 3). Of note, 51.4% rotavirus were detected from Savar region followed by 37.4% from Chattogram and 11.2% from Sirajganj.
Fig 3. Yearly distribution of rotavirus genotype in children with acute gastroenteritis in Bangladesh during 2014–2019.
Nucleotide sequence and phylogenetic analysis of group a rotavirus
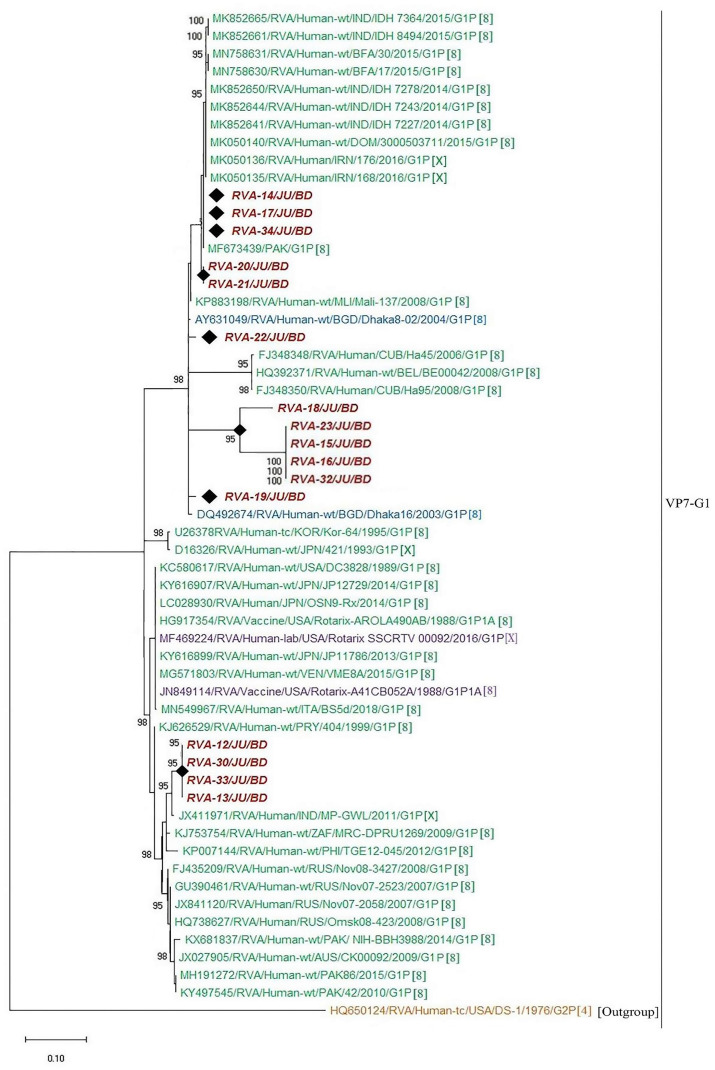
In order to understand the molecular epidemiology of rotavirus A in Bangladesh, sequence analysis of VP7 gene were conducted. A total of thirty-five representative sequences of rotavirus A were used for the phylogenetic analysis. Genotype G1P[8] was the most prevalent (45.7%), followed by G2P[4] (20%), G9P[4] (14.3%), G1P[6] (11.4%), G9P[8] (2.9%), G9P[6] (2.9%) and G11P[25] (2.9%), respectively. RVA genotype G1P[8] in Bangladesh during 2014–2019 were closely related with G1P[8] of India, Mali, Russia, Pakistan, Cuba, Iran and previous strains of Bangladeshi rotavirus G1P[8] (Fig 4). Further, genotype G2P[4] detected during 2014–2019 in Bangladesh clustered with each other and previously reported G2P[4] of Bangladesh, Mauritius and Australia (Fig 5). We also confirmed the genotypic relationship of G9 and G11 detected in Bangladesh with other circulating rotaviruses worldwide. Study genotype G9P[4] clustered with G9P[4] strain of India and study genotype G9P[8] was closely related with previously reported G9P[8] of Bangladesh, Mozambique and Thailand (Fig 6). Study genotype G11P[25] clustered with the G11P[25] of Korea, G11P[4] of Korea and G11P[6] of Bangladesh (Fig 7).
Fig 4. Maximum likelihood phylogenetic tree constructed from the nucleotide sequences of G1-VP7 strains and representative RVA strains with kimura-2-parameter model in MEGA X.
Bootstrap values <60 are not shown. RVA strains sequenced in this study are represented by the red color in italic bold letter. Bangladeshi strains reported in the previous studies are shown in blue. The vaccine strains are represented by purple color, while green shading represent strains isolated all over the world. The RVA strains sequenced in this study are represented by their ID and reference strains obtained from GenBank database are represented by Accession number, Strain Name, Country and year of Isolation. Scale bar: 0.10 substitutions per nucleotide.
Fig 5. Maximum likelihood phylogenetic tree constructed from the nucleotide sequences of G2-VP7 strains and representative RVA strains with kimura-2-parameter model in mega program 10.0.
Bootstrap values <60 are not shown. RVA strains sequenced in this study are represented by the red color in italic bold letter. Bangladeshi strains reported in the previous studies are shown in blue. The vaccine strains are represented by purple color, while green shading represent strains isolated all over the world. The RVA strains sequenced in this study are represented by their ID and reference strains obtained from GenBank database are represented by Accession number, Strain Name, Country and year of Isolation. Scale bar: 0.10 substitutions per nucleotide.
Fig 6. Maximum likelihood phylogenetic tree constructed from the nucleotide sequences of G9-VP7 strains and representative RVA strains with kimura-2-parameter model in MEGA X.
Bootstrap values <60 are not shown. RVA strains sequenced in this study are represented by the red color in italic bold letter. Bangladeshi strains reported in the previous studies are shown in blue, whereas green shading represent strains isolated all over the world. The RVA strains sequenced in this study are represented by their ID and reference strains obtained from GenBank database are represented by Accession number, Strain Name, Country and year of Isolation. Scale bar: 0.10 substitutions per nucleotide.
Fig 7. Maximum likelihood phylogenetic tree constructed from the nucleotide sequences of G11-VP7 strains and representative RVA strains with kimura-2-parameter model in MEGA X.
Bootstrap values <60 are not shown. RVA strains sequenced in this study are represented by the red color in italic bold letter. Bangladeshi strains reported in the previous studies are shown in blue, while green shading represent strains isolated all over the world and black color represented nonhuman primate RVA strains. The RVA strains sequenced in this study are represented by their ID and reference strains obtained from GenBank database are represented by Accession number, Strain Name, Country and year of Isolation. Scale bar: 0.10 substitutions per nucleotide.
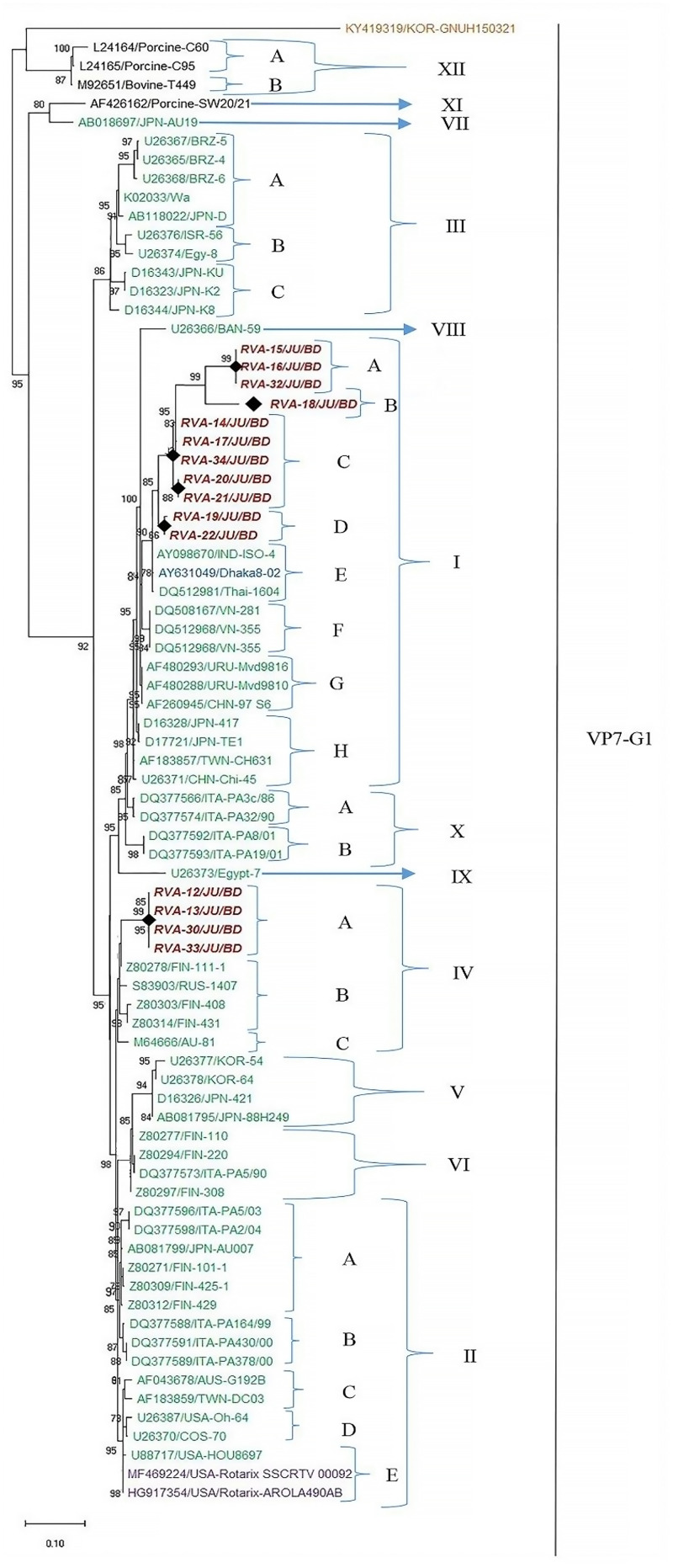
Distribution of G1 genotypes into unique sublineages
The sequences of VP7 genes of G1 isolates detected in this study and worldwide rotavirus reference G1 strains were used to investigate the heterogeneity of rotaviruses within G1 genotype. Twelve distinct lineages and 23 sublineages were identified (Fig 8). Among these, lineage XI and lineage XII consisted of nonhuman primate rotaviruses, while the lineage I to X were found only in humans. Fifteen sequences of G1 genotype from Bangladesh during 2014–2019 were classified into two distinct lineages, lineage I with 73.3% (11 of 15) isolates and the lineage IV with 30.77% (4 of 15) isolates. Within the lineage I, three isolates clustered in sublineage IA, one isolate in sublineage IB, five isolates in sublineage IC and two isolates in ID. G1 isolates of lineage I were closely related with each other and previously isolated G1 of Bangladesh and India. Within the lineage IV, four G1 isolates of this study made a unique sublineage (IVA) (Fig 8). G1 isolates of lineage IV were closely related with G1 rotavirus of Finland and Russia. Within each sublineage, the nucleotide identities of rotavirus strains ranged from 97% to 100%, indicating less than 3% genetic difference among them. On the contrary, the nucleotide sequence variation of rotavirus G1 strains between lineages was higher, ranging from 6% to 12%.
Fig 8. Maximum likelihood phylogenetic tree constructed from the nucleotide sequences of G1-VP7 strains and representative RVA strains with kimura-2-parameter model in MEGA X.
Lineages analysis was conducted using reference trees. Bootstrap values <60 are not shown. RVA strains sequenced in this study are represented by the red color in italic bold letter. Bangladeshi strains reported in the previous studies are shown in blue. The vaccine strains are represented by purple color, while green shading represent strains isolated all over the world and black color represented nonhuman primate RVA strains. The RVA strains sequenced in this study are represented by their ID and reference strains obtained from GenBank database are represented by accession number and Strain Name. Scale bar: 0.10 substitutions per nucleotide.
Mutation analysis of VP7 gene of group A rotavirus
Rotavirus VP7 protein has three important antigenic regions (region A—amino acid position 87 to 100, region B—amino acid position 141–150, and region C—amino acid position 208–224), which can be variable within genotype. About 90%-99% sequence similarities were found in the genotype G1P[8] of this study with vaccine strain MF469224 and JN849114. In five G1P[8] strains, substitution point mutations were detected in the region A. However, all G2P[4] strains had the same mutation G216R at the region C comparing with vaccine strain GU565068. About 95%-99% sequence similarity was detected among G2P[4] strains. No significant mutation was found for G9P[4] strains in the regions A, B or C. Two G1P[6] strains had a deletion mutation at the position 220. G9P[8] strains had several mutations at regions A and C, sharing 95% sequence similarity. G9P[6] strains had substitution mutation at the regions B and C, sharing 96% sequence similarity. Isolate of G11P[25] RVA had only one mutation at the position T97I, sharing 100% sequence similarity with the reference (Table 3).
Table 3. Amino acid substitution mutations in the antigenic regions of VP7 in Bangladeshi rotavirus strains detected during 2014–2019.
| Genotype (Strain) | Antigenic regions of VP7 [Position (Initial a.a.→ Mutated a.a.) | ||
|---|---|---|---|
| A (87–100) | B (141–150) | C (208–224) | |
| G1P[8] (RVA-15) | H88Q | - | - |
| G1P[8] (RVA-16) | C92G | - | - |
| G1P[8] (RVA-18) | I87F, I94R, Q95P, V99E | - | - |
| G1P[8] (RVA-23) | Y87A, R89V, N91S | - | - |
| G1P[8] (RVA-32) | Q95H, L96S, L100F | - | - |
| G2P[4] (RVA-1) | - | - | T218N |
| G2P[4] (RVA-2) | - | - | T218N |
| G2P[4] (RVA-9) | - | - | T218N |
| G9P[8] (RVA-28) | Q96H, T97S, G100V | - | N210Y |
| K224N | |||
| G9P[6] (RVA-29) | - | A147P | N215H, C224R |
| N149H | |||
| I150K | |||
| G11P[25] (RVA-31) | T97I | - | - |
a.a. amino acid.
- no mutation.
Discussion
Still in this 21st century rotavirus infection is a burden for children in developing countries like Bangladesh. Virus infection in the gastrointestinal tract is one of the major causes of children morbidity and mortality in developing countries [1, 2, 4]. In agreement with previous studies, this study detected 36.8% (211 of 574) prevalence of virus infection in children with acute gastroenteritis in Bangladesh [19]. It was also found that rotavirus (RV) had the highest prevalence (24.4%), followed by norovirus (4.9%), adenovirus (4.2%) and human bocavirus (3.3%) [25]. Prevalence of viral infection in diarrheal children with AGE reported in this study were similar with the previous studies in developing countries like Nepal, India, Sri Lanka, Pakistan, South America, Africa and Europe [19–21, 29–33]. In this study, rotavirus A was detected in 24.4% fecal specimens. No RVB or RVC was detected in this study from Bangladeshi children. This high prevalence of RVA in children with AGE in Bangladesh is an indication of lower vaccine efficacy or poor vaccine coverage. This finding of high RVA prevalence in children was consistent with the previous studies during pre-vaccinated era of rotavirus in Bangladesh and other developing countries [19–21, 29–33]. Other possible causes of high prevalence of RVA might be poor hygienic conditions of most of the residents, presence of great genotypic diversity and not including vaccine in the national immunization program in Bangladesh [19]. In this study, the coinfection of other viruses with rotavirus was also determined. Coinfection between diarrheal viruses was detected in 24.6% of the positive cases. Coinfection between rotavirus and norovirus accounted for most of the cases (10 of 52) of coinfection. These findings are in good agreement with the previous studies of rotavirus coinfection in many developing countries worldwide [33–35].
Children aged <60 months were divided into six age groups according to previous study [25, 33]. In this study, rotavirus was detected to be most prevalent (37.9%) among children aged 4–11 months, followed by 12–23 months (22.1%). Most of the rotavirus positive cases (62.1%) were detected in male children. Both the age and gender distribution of rotavirus in diarrheal children in Bangladesh were similar with the previous epidemiological studies in Bangladesh, Japan, Asia, Europe and South America [20, 29–35]. Rotavirus infection has been reported to cause various clinical symptoms in diarrheal children worldwide. In this study, diarrhea (90.7%) dehydration (88.7%) and vomiting was found in higher percentage in rotavirus positive cases than negative cases. However, abdominal pain was reported in higher percentage from rotavirus negative cases. Clinical symptoms associated with rotavirus infection reported in this study also agreed with the previous studies in Bangladesh, Asia, Africa and Europe [20, 21, 29–33].
While analyzing RVA infection seasonality, we found high incidence of rotavirus during the winter (Nov-Jan) season with low temperature in Bangladesh. About 58.6% of rotavirus infection in children were detected during the winter during 2014 to 2019. Another peak of rotavirus infection (30.7%) was found during the rainy season (May-Jul). During this study, the incidence of rotavirus increased with declining temperature and we found highest peak (21% infection) at 15°C average temperature in Bangladesh. High prevalence and peak of RVA infection had been reported in Dey et al. (2009) and Phan et al. (2007). The seasonality of RVA in this study is with good agreement with studies in Bangladesh, South East Asia and Japan [20, 36, 37].
One of the major objectives of this study was to characterize the genotype of circulating rotavirus in Bangladesh. Changing pattern of both G and P genotypes along with their combinations were characterized. Worldwide epidemiological research on rotavirus specified that G1 is the predominant genotype. However, incidence of genotype G2-G4, G9 and G12 has also been detected over time [14, 28]. During 1992 to 1997, rotavirus G4 genotype was the most common in Dhaka but became less common over time. During 2002–2005, genotype G1 was the most prevalent, while in 2005–2006, G2 was prevalent over G1 in Bangladesh [18–20]. Genotype G9 became predominant during 2006 to 2012 along with G1 in Bangladesh [19]. We found increased frequency of G1 genotype (57%) followed by G2 (20%), G9 (20%) and G11 (2.9%), respectively in children with acute gastroenteritis in Bangladesh. However, the frequency of G1 was found reducing in Giri et al. (2018) in developing countries of Asia. Interestingly, this study reported decreased frequency of G9 and increased frequency of G2 from previous studies, Mahmud-Al-Rafat et al. (2018) in Bangladesh [19]. Of note, G11 was also specified in this study. RVA studies, Giri et al. (2018) and Sadiq et al. (2019) have reported that prevalence of G3 has increased than before in developing countries in Asia and Europe in recent time [33]. However, genotype G3, G4 along with G12 was not detected in this study. Increased prevalence of G1 is in good agreement with previous reports but absence of G3, G4 and decreased prevalence of G9 along with increased incidence of G2 and G11 are new in Bangladesh [18–21]. This altered trends of RVA genotype distribution may also reflect regional variation in recent times. In this study, four P genotypes- P[8], P[4], P[6] and P[25] were detected. Genotype P[8] was the most frequent (45.7%) followed by P[4] (30%), P[6] (14.3%) and P[25] (2.9%) and 7.1% was nontypeable. Among P genotype, P[8] (80%) has remained the most prevalent genotype followed by P[4] and other non-P[8] genotype (20%) in previous studies in Bangladesh, India, Nepal and Pakistan [20, 28]. Of note, a decrease of P[8] frequency was replaced by an increase frequency of non-P[8] genotypes in Bangladesh during 2014–2019. To the best of our knowledge, this will be the first report of genotype P[6] in Bangladesh. There are no recent reports of P[6] from Bangladesh, but it has been reported from Nepal and Myanmar in Giri et al. (2018).
In the G and P genotype combination, G1P[8] was predominant (22.4%), followed by G9P[8] 20.8%, G2P[4] 16.9%, and G12P[8] 10.4% during 2006 to 2012 in Bangladesh. Further, genotype G3P[8] and G4P[8] had been also reported in Bangladesh [19, 35]. Another unusual genotype G9P[4] has emerged in Bangladesh in recent time and this genotype has also been reported in Asia, Europe, Africa and Americas [19, 29–33]. However, we also detected a great genotypic diversity of RVA during 2014–2019 in Bangladesh. Seven genotype combinations were revealed in this study. The most prevalent genotype was G1P[8] with the highest frequency of 43%, followed by G2P[4] (18%). This genotypic distribution of RVA in Bangladesh was in good agreement with the previous reports in India, Nepal, Pakistan, Japan, Brazil, Europe, Africa and Bangladesh [18–20, 23, 28–33]. Interestingly, we found that the frequency of previously predominant G9P[8] infection has reduced to 3%. We also detected high prevalence (12%) of genotype G9P[4], followed by genotype G1P[6] (11.4%), G9P[6] (3%), and G11P[25] (3%). To the best of our knowledge, it is the first report of G1P[6] and G9P[6] in Bangladesh. There are limited studies that had reported G1P[6] and G9P[6] in Nepal and Myanmar during 2009–2015 and Sadiq et al. (2019) has reported G1P[6] and G9P[6] in Pakistan [28]. True genotypic diversity of RVA in developing countries like Bangladesh may be greater than we can detect. In future, more studies should be conducted to measure the actual burden of RVA in Bangladesh.
Based on the divergence of VP7 genes of G1 rotaviruses a classification scheme has been developed that specifies G1 rotavirus into various lineages and sublineages. Numerous studies had been undertaken to specify the heterogeneity and dynamics of the evolution of G1 rotaviruses in USA, Italy and Japan [23, 38, 39]. In this study, we followed the classification scheme that was used in Phan et al. (2007) and Dey et al. (2009) to characterize the G1 rotavirus in Bangladesh. The sequences of VP7 gene of G1 genotype were analyzed to investigate the heterogeneity of G1 rotavirus in Bangladesh during 2014–2019. Among twelve lineages, Bangladeshi G1 RVA were distributed in two lineages. Within lineage I, VP7 of G1 from Bangladesh had 99% sequence similarity with IND-ISO-4 and Dhaka8-02 strains. Further, four G1 within lineage IV had 99.98% sequence similarity with FIN-408, FIN-431, AU-81 and FIN-111-1. We detected close relationship between G2P[4] and previously reported M315, M334 and M313 in Bangladesh. Both G1P[8] and G2P[4] genotypes in Bangladesh showed close relationship with previously isolated strains in Bangladesh. Our study is an important tool to understand the genetic diversity of circulating rotavirus in children with AGE in Bangladesh. The presence of diverse genotypes with mutation in antigenic regions can cause reinfection in vaccinated population and reduction of vaccine efficiency in Bangladesh. Further, circulation of diverse genotypes is the major reason of high prevalence of rotavirus in Bangladesh [17, 40].
Rotavirus VP7 protein has three important antigenic regions- amino acid position 87 to 100 (A), 141–150 (B) and 208–224 (C) which are involved in interaction with antibodies and neutralization of epitopes [41, 42]. We detected mutations at antigenic determination regions in G1P[8] and G2P[4] in Bangladesh during 2014–2019. Mutations at antigenic regions may alter rotavirus antigenic properties [41, 42]. Prevalence of unusual genotypes, intragenotypic diversity and frequent mutations at antigenic regions of rotavirus A are major explanations of the constant predominance of rotavirus in Bangladesh.
Bangladesh is one of the countries with the highest disease burden of RVA infections in children <5 years of age. The introduction of RVA vaccines has reduced the global disease burden of RVA in many countries [29]. According to recent survey by Mahmud-Al-Rafat et al. (2018), RVA vaccine coverage in capital Dhaka is good but in small town and suburban areas the RVA vaccine coverage are poor. Overall, RVA vaccine introduction in EPI program in Bangladesh could prevent over 10,000 deaths per year [19]. Besides, RVA studies including large number of samples for sustained time periods and diverse sentinel sites throughout the country will be required for assessing the true RVA disease burden. Moreover, whole genome analysis of human RVA strains and inclusion of animal and environmental samples in future studies is recommended to elucidate the current interspecies transmission and genomic reassortment and recombination events.
Conclusions
This study concludes the high prevalence of G1P[8] and G2P[4] RVA strains along with reduced prevalence of G3 RVA in Bangladesh during 2014–2019. This study will provide comprehensive insights to the researchers and public health authorities to measure the RVA disease burden in the country. The observed large diversity of RVA genotypes along with their yearly and seasonal fluctuations require an in-depth, broad surveillance system in the country. The findings of this study can provide guideline data before introduction of rotavirus vaccine in the national immunization program in Bangladesh. The data in this study can be used to assess the impact of rotavirus vaccine in the future.
Supporting information
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
This research was supported by Grants-in-Aid from the Ministry of Education, the People’s Republic of Bangladesh. The fund was granted to Dr. Shuvra Kanti Dey. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kotloff KL, Platts-Mills JA, Nasrin D, Roose A, Blackwelder WC, Levine MM. Global burden of diarrheal diseases among children in developing countries: Incidence, etiology, and insights from new molecular diagnostic techniques. Vaccine 2017;35: 6783–6789. 10.1016/j.vaccine.2017.07.036 [DOI] [PubMed] [Google Scholar]
- 2.Aliabadi N, Antoni S, Mwenda JM, Weldegebriel G, Biey JN, Cheikh D, et al. Global impact of rotavirus vaccine introduction on rotavirus hospitalisations among children under 5 years of age, 2008–16: findings from the Global Rotavirus Surveillance Network. The Lancet Global Health. 2019;7:e893–e903. 10.1016/S2214-109X(19)30207-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coşkun USŞ, Kasap T. Frequency of rotavirus and adenovirus in pediatric patients with acute gastroenteritis. Journal of Contemporary Medicine. 2019;9:85–88. [Google Scholar]
- 4.Milivojevic V, Milosavljevic T. Burden of Gastroduodenal Diseases from the Global Perspective. Current Treatment Options in Gastroenterology. 2020;18:148–157. 10.1007/s11938-020-00277-z [DOI] [PubMed] [Google Scholar]
- 5.Kotloff KL. The burden and etiology of diarrheal illness in developing countries. Pediatric Clinics. 2017;64:799–814. 10.1016/j.pcl.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 6.Hartman S, Brown E, Loomis E, Russell HA. Gastroenteritis in children. American family physician. 2019;99:159–165. [PubMed] [Google Scholar]
- 7.Tilmanne A, Lepage P, Vandenberg O, Martiny D, Hallin M, Quach C. Rotavirus: the guard dies, but it does not surrender. Infectious Diseases. 2019;51:67–70. 10.1080/23744235.2018.1508885 [DOI] [PubMed] [Google Scholar]
- 8.Dennehy PH. Rotavirus infection: a disease of the past? Infectious Disease Clinics. 2015;29:617–635. 10.1016/j.idc.2015.07.002 [DOI] [PubMed] [Google Scholar]
- 9.Pecenka C, Parashar U, Tate JE, Khan JA, Groman D, Chacko S, et al. Impact and cost-effectiveness of rotavirus vaccination in Bangladesh. Vaccine. 2017;35(32):3982–7. 10.1016/j.vaccine.2017.05.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadiq A, Bostan N, Yinda KC, Naseem S, Sattar S. Rotavirus: Genetics, pathogenesis and vaccine advances. Reviews in medical virology. 2018;28(6):e2003 10.1002/rmv.2003 [DOI] [PubMed] [Google Scholar]
- 11.Lefkowitz EJ, Dempsey DM, Hendrickson RC, Orton RJ, Siddell SG, Smith DB. Virus taxonomy: the database of the International Committee on Taxonomy of Viruses (ICTV). Nucleic Acids Research. 2018;46:D708–D717. 10.1093/nar/gkx932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Troeger C, Khalil IA, Rao PC, Cao S, Blacker BF, Ahmed T, et al. Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA pediatrics. 2018;172(10):958–65. 10.1001/jamapediatrics.2018.1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patton JT. Rotavirus diversity and evolution in the post-vaccine world. Discovery medicine. 2012;13:85 [PMC free article] [PubMed] [Google Scholar]
- 14.Zeng Y, Li T, Zhao B, Lai F, Tang X, Qiao Y, et al. Molecular epidemiology of group A rotavirus in outpatient diarrhea infants and children in Chongqing, China, 2011–2015. Journal of medical virology. 2019;91:1788–1796. 10.1002/jmv.25530 [DOI] [PubMed] [Google Scholar]
- 15.Liu N, Xu Z, Li D, Zhang Q, Wang H, Duan ZJ. Update on the disease burden and circulating strains of rotavirus in China: a systematic review and meta-analysis. Vaccine. 2014; 32:4369–4375. 10.1016/j.vaccine.2014.06.018 [DOI] [PubMed] [Google Scholar]
- 16.Kawai K, O’Brien MA, Goveia MG, Mast TC, El Khoury AC. Burden of rotavirus gastroenteritis and distribution of rotavirus strains in Asia: a systematic review. Vaccine. 2012;30:1244–1254. 10.1016/j.vaccine.2011.12.092 [DOI] [PubMed] [Google Scholar]
- 17.Miles MG, Lewis KD, Kang G, Parashar UD, Steele AD. A systematic review of rotavirus strain diversity in India, Bangladesh, and Pakistan. Vaccine. 2012;30:A131–A139. 10.1016/j.vaccine.2011.10.002 [DOI] [PubMed] [Google Scholar]
- 18.Paul SK, Kobayashi N, Nagashima S, Ishino M, Watanabe S, Alam MM, et al. Phylogenetic analysis of rotaviruses with genotypes G1, G2, G9 and G12 in Bangladesh: evidence for a close relationship between rotaviruses from children and adults. Archives of virology. 2008;153:1999 10.1007/s00705-008-0212-9 [DOI] [PubMed] [Google Scholar]
- 19.Mahmud-Al-Rafat A, Muktadir A, Muktadir H, Karim M, Maheshwari A, Ahasan MM. Rotavirus epidemiology and vaccine demand: considering Bangladesh chapter through the book of global disease burden. Infection. 2018;46:15–24. 10.1007/s15010-017-1082-4 [DOI] [PubMed] [Google Scholar]
- 20.Dey SK, Hayakawa Y, Rahman M, Islam R, Mizuguchi M, Okitsu S, et al. G2 strain of rotavirus among infants and children, Bangladesh. Emerging infectious diseases. 2009; 15:91 10.3201/eid1501.080883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Afrad MH, Hassan Z, Farjana S, Moni S, Barua S, Das SK, et al. Changing profile of rotavirus genotypes in Bangladesh, 2006–2012. BMC infectious diseases. 2013;13:320 10.1186/1471-2334-13-320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kirkwood CD, Ma LF, Carey ME, Steele AD. The rotavirus vaccine development pipeline. Vaccine. 2019;37:7328–7335. 10.1016/j.vaccine.2017.03.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phan TG, Khamrin P, Quang TD, Dey SK, Takanashi S, Okitsu S, et al. Detection and genetic characterization of group A rotavirus strains circulating among children with acute gastroenteritis in Japan. Journal of virology. 2007;81:4645–4653. 10.1128/JVI.02342-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez-Lacort M, Collado S, Díez-Gandía A, Díez-Domingo J. Rotavirus, vaccine failure or diagnostic error?. Vaccine. 2016;34:5912–5915. 10.1016/j.vaccine.2016.10.032 [DOI] [PubMed] [Google Scholar]
- 25.Sharif N, Parvez AK, Haque A, Talukder AA, Ushijima H, Dey SK. Molecular and epidemiological trends of human bocavirus and adenovirus in children with acute gastroenteritis in Bangladesh during 2015 to 2019. Journal of Medical Virology. In press. (2020). 10.1002/jmv.25812. [DOI] [PubMed] [Google Scholar]
- 26.Hall TA, editor. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic acids symposium series; [London]: Information Retrieval Ltd., 1999;c1979–c2000. [Google Scholar]
- 27.Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X. molecular evolutionary genetics analysis across computing platforms. Molecular biology and evolution. 2018;35:1547–9. 10.1093/molbev/msy096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tamura K, Nei M, Kumar S. Prospects for inferring very large phylogenies by using the neighbor-joining method. Proceedings of the National Academy of Sciences. 2004;101:11030–5. 10.1073/pnas.0404206101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giri S, Hemavathy RP, Arumugam R, Sherchand JB, Thu HM, Galagoda G, et al. Molecular epidemiology of rotaviruses in the south-east Asian region from 2009 to 2015. Vaccine. 2018;36:7851–7855. 10.1016/j.vaccine.2018.02.092 [DOI] [PubMed] [Google Scholar]
- 30.Sadiq A, Bostan N, Bokhari H, Matthijnssens J, Yinda KC, Raza S, et al. Molecular characterization of human group A rotavirus genotypes circulating in Rawalpindi, Islamabad, Pakistan during 2015–2016. PloS one. 2019;14(7):e0220387 10.1371/journal.pone.0220387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Primo D, Pacheco GT, Timenetsky MDCST, Luchs A. Surveillance and molecular characterization of human adenovirus in patients with acute gastroenteritis in the era of rotavirus vaccine, Brazil, 2012–2017. Journal of Clinical Virology. 2018;109:35–40. 10.1016/j.jcv.2018.10.010 [DOI] [PubMed] [Google Scholar]
- 32.Ouermi D, Soubeiga D, Nadembega WMC, Sawadogo PM, Zohoncon TM, Obiri-Yeboah D, et al. Molecular Epidemiology of Rotavirus in Children under Five in Africa (2006–2016): A Systematic Review. Pak J Biol Sci. 2017;20(2):59–69. 10.3923/pjbs.2017.59.69 [DOI] [PubMed] [Google Scholar]
- 33.Tcheremenskaia O, Marucci G, De Petris S, Ruggeri FM, Dovecar D, Sternak SL, et al. Molecular epidemiology of rotavirus in Central and Southeastern Europe. Journal of clinical microbiology. 2007;45(7):2197–204. 10.1128/JCM.00484-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharif N, Nobel NU, Sakib N, Liza SM, Khan ST, Billah B, et al. Molecular and Epidemiologic Analysis of Diarrheal Pathogens in Children With Acute Gastroenteritis in Bangladesh During 2014–2019. The Pediatric Infectious Disease Journal. 2020;39(7):580–5. 10.1097/INF.0000000000002637 [DOI] [PubMed] [Google Scholar]
- 35.Grimprel E, Rodrigo C, Desselberger U. Rotavirus disease: impact of coinfections. The Pediatric infectious disease journal. 2008;27:S3–S10. [DOI] [PubMed] [Google Scholar]
- 36.Jagai JS, Sarkar R, Castronovo D, Kattula D, McEntee J, Ward H, et al. Seasonality of rotavirus in South Asia: a meta-analysis approach assessing associations with temperature, precipitation, and vegetation index. PloS one. 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ameta P, Nayak VH, Goyal SC. Prevalence and Seasonal distribution of Rotavirus Diarrhea in hospitalized children less than 5 years old in South Rajasthan. International Journal on Biomedical Research. 2015;6:214–218. [Google Scholar]
- 38.Arista S, Giammanco GM, De Grazia S, Ramirez S, Biundo CL, Colomba C, et al. Heterogeneity and temporal dynamics of evolution of G1 human rotaviruses in a settled population. Journal of virology. 2006;80:10724–10733. 10.1128/JVI.00340-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin Q, Ward RL, Knowlton DR, Gabbay YB, Linhares AC, Rappaport R, P A, et al. Divergence of VP7 genes of G1 rotaviruses isolated from infants vaccinated with reassortant rhesus rotaviruses. Archives of Virology. 1996;141:2057–2076. 10.1007/BF01718215 [DOI] [PubMed] [Google Scholar]
- 40.Mazid R, Aung MS, Paul SK, Ahmad FU, Alam M, Ali MA, et al. Resurgence and predominance of G3P [8] human rotaviruses in north-central Bangladesh, 2018–2019. New Microbes and New Infections. 2020;33:100621 10.1016/j.nmni.2019.100621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diwakarla CS, Palombo EA. Genetic and antigenic variation of capsid protein VP7 of serotype G1 human rotavirus isolates. Journal of general virology. 1999;80:341–344. 10.1099/0022-1317-80-2-341 [DOI] [PubMed] [Google Scholar]
- 42.Zade JK, Chhabra P, Chitambar SD. Characterization of VP7 and VP4 genes of rotavirus strains: 1990–1994 and 2000–2002. Epidemiology & Infection. 2009;137:936–942. 10.1017/S0950268808001532 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.