Abstract
Mucin-type O-glycans are involved in cancer initiation and progression, although details of their biological and clinicopathological roles remain unclear. The aim of this study was to investigate the clinicopathological significance of β1,3-N-acetylglucosaminyltransferase 6 (β3Gn-T6), an essential enzyme for the synthesis of core 3 O-glycan and several other O-glycans in pancreatic ductal adenocarcinoma (PDAC). We performed immunohistochemical and lectin-histochemical analyses to detect the expression of β3Gn-T6 and several O-glycans in 156 cases of PDAC with pancreatic intraepithelial neoplasias (PanINs) and corresponding normal tissue samples. The T antigen, Tn antigen, sialyl Lewis X (sLeX) antigen, and sLeX on core 2 O-glycan were more highly expressed in PDAC cells than in normal pancreatic duct epithelial cells (NPDEs). Conversely, the expression of 6-sulfo N-acetyllactosamine on extended core 1 O-glycan was found in NPDEs and was low in PDAC cells. These glycan expression levels were not associated with patient outcomes. β3Gn-T6 was expressed in ~20% of PDAC cases and 30–40% of PanINs but not in NPDEs. Higher expression of β3Gn-T6 was found in PDAC cells in more differentiated adenocarcinoma cases showing significantly longer disease-free survival in both univariate and multivariate analyses. In addition, the expression of β3Gn-T6 in PDAC cells and PanINs significantly correlated with the expression of MUC5AC in these cells, suggesting that β3Gn-T6 expression is related to cellular differentiation status of the gastric foveolar phenotype. Thus, it is likely that β3Gn-T6 expression in PDAC cells is a favorable prognostic factor in PDAC patients, and that the expression of β3Gn-T6 correlates with the gastric foveolar phenotype in pancreatic carcinogenesis.
Introduction
Mucin-type O-glycans play roles in various biological functions, including lymphocyte homing and gastric mucosal defense against Helicobacter pylori [1–3]. Cancer cells express unique and characteristic glycan structures [4], some of which are involved in cancer initiation, progression, and metastasis, mainly through cellular recognition and/or cell adhesion [5]. Although these unique characteristics have the potential to be used for diagnostic and therapeutic research and development, limited information is currently available regarding the biological roles and clinicopathological significance of O-glycans in cancer.
Glandular epithelial cells produce mucin consisting of core proteins and abundant O-linked glycans [6]. The synthesis of O-glycans is initiated by the addition of N-acetylgalactosamine to Ser/Thr to form the Tn antigen (Fig 1). Based on the Tn antigen, core 1 (T antigen) or core 3 structures are formed, which are then branched to give rise to core 2 or core 4 structures, sequentially. These core structures can be further extended thus resulting in complex glycans, such as several blood type antigens (Fig 1). It has been reported that both core and peripheral modified glycans are expressed specifically in some types of cancer and are related to biological characteristics of the cancer cells, thereby representing tumor markers and prognostic markers [7–10].
Fig 1. Biosynthetic pathways of mucin-type O-glycans.
β3Gn-T6 is the only core 3 synthetic enzyme. GalNAc: N-Acetylgalactosamine, GlcNAc: N-Acetylglucosamine, NeuAc: N-Acetylneuraminic acid.
Pancreatic ductal adenocarcinoma (PDAC) is a highly malignant disease [11]. Despite advances in diagnosis and treatments, the 5-year survival rate is less than 10% in PDAC [12]. To improve the patient outcomes, we have to understand PDAC more deeply. PDAC is known to express the Tn antigen and its sialylated derivative, the STn antigen [13]. These truncated O-glycans in PDAC cells are associated with aggressive characteristics [14, 15]. Sialyl Lewis A (sLeA), alternatively called CA19-9, and sialyl Lewis X (sLeX) are reported to be unfavorable prognostic factors in PDAC [15, 16]. Although this has been previously demonstrated by studies involving cell lines or animal models, only a few reports have addressed the clinicopathological and biological roles of glycans using human clinical samples. In addition, these two unique glycans, 6-sulfo N-acetyllactosamine on extended core 1 O-glycan detected by antibody MECA-79 [3, 17], and sLeX on core 2 O-glycan detected by antibody NCC-ST-439 (ST-439) [18, 19] have not yet been evaluated in PDAC. The presence of MECA-79 antigen is used as a marker of high endothelial venules of lymph nodes and the antigen is a part of the glycan structure of an L-selectin ligand [3], and is expressed in pancreatic ductal epithelial cells [20].
The presence of core 3 O-glycan that is induced in cancer cells by β1,3-N-acetylglucosaminyltransferase 6 (β3Gn-T6), which is an essential enzyme for the synthesis of core 3 O-glycan [8], has been reported to reduce malignant characteristics (proliferation, invasion, and metastasis) in colon, prostate, and pancreatic cancers according to in vitro assays with animal model experiments [8, 21, 22]. However, clinicopathological significance of core 3 O-glycan and β3Gn-T6 has not been evaluated yet.
The aim of this study was to investigate the clinicopathological impact of core 3 O-glycan on PDAC through immunohistochemical detection of β3Gn-T6, rather than measuring the structure of core 3 O-glycan, for which currently there is no specific antibody or lectin. We examined the expression of β3Gn-T6 in 156 consecutive cases of PDAC along with normal pancreatic tissue and the most popular premalignant lesion of pancreatic intraepithelial neoplasia (PanIN) [23], and compared the clinicopathological features. We also examined the clinicopathological impact of several O-glycans in PDAC.
Materials and methods
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the National Cancer Center, Japan (#2005–077). The written informed consent was obtained from all participants involved in the study, and all clinical investigations were conducted in line with the principles of the Declaration of Helsinki.
Study population
Clinical and pathological data and specimens used for this study were obtained through a detailed retrospective review of the medical records of 156 consecutive patients with PDAC who had undergone surgical resection between 2009 and 2011 at the National Cancer Center Hospital, Tokyo. None of the patients had received any therapy before surgery. All patients included in this study underwent macroscopic curative resection, and all cases involved conventional ductal carcinomas. The clinicopathological characteristics of the study participants are summarized in Table 1. The median follow-up period after surgical treatment was 29.1 (1.7–126.5) months. Recurrence was suspected when a new local or distant metastatic lesion was found on serial images, and an increase in tumor marker levels was observed. At the census date (September 2018), we checked whether the patients were dead or alive; 62 patients (39.7%) were alive, 82 (52.6%) had died of pancreatic cancer, and 12 (7.6%) had died of other causes. All M1 (TNM classification [24]) patients showed only nodal metastasis around the abdominal aorta.
Table 1. Correlations between Exp-scores of β3Gn-T6 and clinicopathological variables.
| Variable | Number (%) | Median Exp-score of β3Gn-T6 | P value | |
|---|---|---|---|---|
| Gender | Male | 90 (57.7%) | 30.0 | 0.32a |
| Female | 66 (42.3%) | 45.0 | ||
| Age (years, median 68.5) | 70–89 | 78 (50.0%) | 40.0 | 0.60a |
| 38–69 | 78 (50.0%) | 30.0 | ||
| Adjuvant chemotherapy | Presence | 111 (71.2%) | 30.0 | 0.42b |
| Absence | 44 (28.2%) | 47.5 | ||
| Unknown | 1 (0.6%) | 85 | ||
| Tumor size (mm, median 35) | 35–96 | 84 (53.8%) | 40.0 | 0.33a |
| 13–34 | 72 (46.2%) | 30.0 | ||
| Tumor grade | G1 | 44 (28.2%) | 55.0 | <0.0005b |
| G2 | 85 (54.5%) | 40.0 | ||
| G3 | 27 (17.3%) | 10.0 | ||
| Lymphatic invasion | ly2, ly3 | 131 (84.0%) | 37.5 | 0.58a |
| ly0, ly1 | 25 (16.0%) | 35.0 | ||
| Venous invasion | v2, v3 | 117 (75%) | 35.0 | 0.79a |
| v0, v1 | 39 (25%) | 35.0 | ||
| Intrapancreatic neural invasion | ne2, ne3 | 97 (62.2%) | 35.0 | 0.13a |
| ne0, ne1 | 59 (37.8%) | 32.5 | ||
| Nerve plexus invasion | Presence | 54 (34.6%) | 45.0 | 0.086a |
| Absence | 102 (65.4%) | 35.0 | ||
| Lymph node metastasis | N1, N2 | 116 (74.4%) | 35.0 | 0.92a |
| N0 | 40 (25.6%) | 47.5 | ||
| Disatant metastasis | M1 | 9 (5.8%) | 25.0 | 0.78a |
| M0 | 147 (94.2%) | 35.0 | ||
| Surgical margin | Positive | 45 (28.8%) | 40.0 | 0.55a |
| Negative | 111 (71.2%) | 35.0 |
aMann-Whitney-U test
bKruskal-Wallis test
Pathological evaluation
All carcinomas were examined pathologically and classified according to the World Health Organization (WHO) classification [11, 23], Union for International Cancer Control (UICC) TNM classification [24], and the Classification of Pancreatic Carcinoma of the Japan Pancreas Society [25]. Surgically resected specimens were fixed in 10% formalin and cut into serial 5-mm-thick slices and all sections were stained with hematoxylin and eosin (HE) for pathological examination. Representative tissue blocks were selected for subsequent analyses. We used PanINs and normal pancreatic tissue in this study as follows: the areas containing PanIN were apart from cancer cells during microscopic observation, and normal pancreatic tissues were more than 2 cm away from the tumor cells.
Immunohistochemistry and lectin-histochemistry
Immunohistochemistry was performed on 4-μm-thick formalin-fixed paraffin-embedded tissue sections using the avidin–biotin complex method as described previously [26]. Lectin-histochemical analysis was performed in the same way as the immunohistochemical analysis, except lectin was used instead of the primary antibody. The primary antibodies and lectins used in this study are listed in Table 2. Immunohistochemical analysis without the primary antibody was carried out as a negative control. Positive findings are shown in S1 Fig.
Table 2. Primary antibodies and lectins.
| antigen | antibody clone, lectin | type | dilution | internal positive control | source |
|---|---|---|---|---|---|
| β3Gn-T6 | G8-144 | Mouse IgG | 1:2000 | goblet cells of duodenal epithelium | in house (8)* |
| Tn antigen | NCC-LU-35-65 | Mouse IgM | 1:100 | surface epithelial cells of duodenal mucosa | in house (32)* |
| 6-sulfo N-acetyllactosamine on extended core 1 O-glycan | MECA-79 | Rat IgM | 1:100 | endothelial cells of high endothelial venule of lymph node | BD Biosciences |
| sLeX | CSLEX1 | Mouse IgM | 1:1000 | Brunner’s glands of duodenum | BD Biosciences |
| sLeX | HECA-452 | Rat IgM | 1:5 | Brunner’s glands of duodenum | ATCC |
| sLeX | NCC-ST-439 | Mouse IgM | 1:5 | Brunner’s glands of duodenum | in house (19)* |
| MUC5AC | CLH2 | Mouse IgG | 1:100 | Fovolar cells of gastric mucosa | Leica |
| T antigen | Peanut aggulutinin | lectin | 1:100 | Brunner’s glands of duodenum | VECTOR |
| non-reducing terminus of N-acetylglucosamine | Griffonia simplicifolia—II | lectin | VECTOR |
β3Gn-T6: β1,3-N-acetylglucosaminyltransferase 6, sLeX: sialyl Lewis X antigen
ATCC: American type culture collection, Leica: Leica Biosystems, VECTOR: Vector laboratories
*() reference number
Evaluation of immunohistochemistry and lectin-histochemistry
After the immunohistochemical and lectin-histochemical analyses, the antigen expression levels were assessed via a semiquantitative scoring system that incorporated percentages of stained cells with the categorized staining intensity. The staining intensity was recorded in comparison to internal positive controls as 0, negative; 1+, positive but weaker than an internal positive control; 2+, equal to the internal positive control; and 3+, stronger than the internal positive control. The percentage of stained cells was determined by the comparison of the number of cancer cells with each staining intensity to the total number of cancer cells. The sum of products obtained by multiplying the staining intensity and the percentage of corresponding intensity was defined as an expression score (Exp-score). Two observers, i.e., Japanese certified pathologists (ND and NH), who had no access to the patient data, independently evaluated the Exp-score. For statistical analyses, patients were subdivided into two groups by means of the medians as a cutoff.
Cell culture
Human pancreatic cancer cell lines, Capan-1, Capan-2, CFPAC-1, and AsPC-1, were obtained from the American Type Culture Collection (ATCC). Capan-1, Capan-2, and CFPAC-1 cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% of fetal calf serum at 37°C and 5% CO2 in a humidified atmosphere. AsPC-1 cells were cultured under the same conditions except the RPMI 1640 medium instead of DMEM medium.
Gene transduction
To generate lenti-viral expression vectors, a segment encoding 3'ΔLTR (between Kpn I and Stu I) of pCDH-MCS-T2A-copGFP-MSCV (SBI system biosciences, Palo Alto, CA) was exchanged by segment encoding 3'ΔLTR (Kpn I and Stu I fragment) of pLenti7.3 (Invitrogen); then, the Cla I and Nhe I segment encoding the CMV promoter, amplified by PCR using pLenti7.3 as a template, was inserted between the 5'LTR encoding and multi-cloning sites, resulting in pCDH-CMV-MCS-T2A-copGFP. The EcoR I and Nco I segment encoding the internal ribosome entry site (IRES) sequence from pIRES-hrGFP2a (Clontech) was subcloned into pcDNA3.1/Zeo(+) (Invitrogen), resulting in pcDNA3.1/IRES-Zeo. The EcoR I and Not I segment containing the IRES and Zeo resistance selection cassette from pcDNA3.1/IRES-Zeo was subcloned into pCDH-CMV-MCS-T2A-copGFP and resulted in pCDH-CMV-MCS-IRES-Zeo-T2A-copGFP. The Nhe I and Xho I fragment from pcDNA3.1-B3GnT6, B3GNT6 (encoding β3Gn-T6) expression vector [8], was subcloned into pCDH-CMV-MCS-IRES-Zeo-T2A-copGFP and resulted in pCDH-CMV-MCS-IRES-Zeo-T2A-copGFP/huB3GnT6. 293FT cells (Invitrogen) were co-transfected with psPAX2, pMD2.G, and pCDH-CMV-MCS-IRES-Zeo-T2A-copGFP/huB3GnT6 or pCDH-CMV-MCS-IRES-Zeo-T2A-copGFP using Lipofectamine LTX with Plus reagent (Invitrogen) according to the manufacturer’s instruction. Seventy-two hours after transfection, the culture supernatants were harvested and concentrated using Lenti-X Concentrator (Takara Bio, Kusatsu, Japan) as the virus solution. For viral infection and gene transduction, Capan-1 cells were seeded into 6-well culture plates at a density of 3.0 × 105 cells per well and cultured with the prepared viral solution (1:50) with polybrene (2 to 8 μg/mL) at 37°C for 24 hours. Viral-transduced cells were selected using Zeocin (Invitrogen) at 200 μg/mL for 10 days. Stably B3GNT6 and mock transduced Capan-1 cells were named as Capan1-B3GnT6 and Capan1-mock, respectively.
Immunofluorescence
Cells were seeded on a chamber slide. The staining procedure was previously described [27]. Immunofluorescence images were obtained using a BZ-X710 all-in-one fluorescence microscope (Keyence, Japan).
Extraction of RNA and quantitative RT-PCR (qRT-PCR)
Total RNA was extracted from pancreatic cancer cells, as described previously [28]. All samples were treated with rDNase during isolation, in accordance with the manufacturer’s instructions. qRT-PCR for target genes and non-target housekeeping control genes was performed with a Quantstudio 3 (Thermo scientific) using FastStart Universal Probe Master (ROX) and probes from the Universal Probe Library (Roche Diagnostics Corp., Indianapolis, IN), as described previously [26]. The sequences of the primers and the respective Universal Probe Library probes are given in S1 Table. The CT values were normalized to that of GAPDH, and the ΔΔCT method was utilized to compare the expression levels of the genes.
Immunoprecipitation and western blot analysis
Whole-cell lysates of Capan1-B3GnT6 and Capan1-mock cells were immunoprecipitated with an anti-MUC5AC antibody (45M1, Abcam, Cambridge, UK) according to the literature [29]. To analyze the structures of glycans attached to MUC5AC, immune complexes were subjected to western blot analysis. The immune complexes were separated by SDS-PAGE in a 4–12% gradient gel (Invitrogen) and were transferred to a Polyvinylidene fluoride (PVDF) membrane, which was then blocked by incubation with PBS-Tween containing 5% of bovine serum albumin as described elsewhere [30]. After that, the membrane was incubated with a primary antibody and biotin-conjugated secondary antibody or with biotin-conjugated lectins (Table 2) followed by ABC reagents (Vector laboratories).
Statistical analysis
Comparison analyses were performed using the nonparametric test. Post-operative overall survival (OS) and disease-free survival (DFS) rates were calculated using the Kaplan-Meier method and analyzed by the log-rank test. The factors found to be significant by univariate analysis were subjected to multivariate analysis using the Cox proportional hazards model (backward elimination method). Differences at P<0.05 were considered statistically significant. Statistical analyses were performed using SPSS software version 26 (IBM Corp., Armonk, USA).
Results
Expression of glycans and β3Gn-T6 in PDAC cells, premalignant cells, and normal tissues
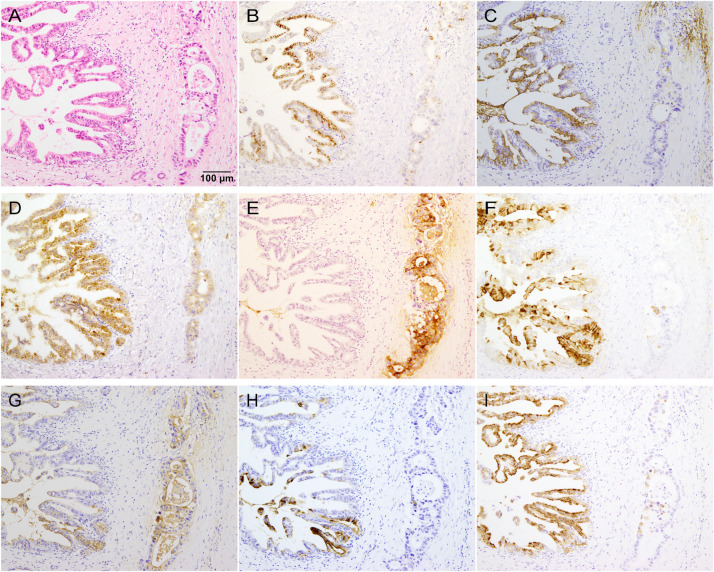
We evaluated the expression of the T antigen (staining with Peanut agglutinin, PNA) [31], Tn antigen [staining with antibody NCC-LU-35 (LU-35)] [32], 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (staining with antibody MECA-79) [3, 17], sLeX (staining with antibodies CSLEX1 and HECA-452) [33], sLeX on core 2 O-glycan (staining with antibody ST-439) [18, 19], and β3Gn-T6 (Fig 1) in PDAC cells, PanINs, and noncancerous tissues, normal pancreatic duct epithelial cells (NPDEs), and other normal tissues. Representative immunohistochemical and lectin-histochemical features are shown in Fig 2 and S1 Fig. PDAC is usually composed of variously differentiated cancer cells, with varied frequency and intensity of glycan expression in PDAC cells in the same case. We first analyzed glycan expression in each component of PDAC (Table 3). Next, to determine a representative value for overall expression of antigens in PDAC cells in each PDAC case, we calculated the Exp-score. All glycan antigens, except MECA-79 antigen, were expressed significantly more highly in PDAC cells than in NPDEs (Fig 3). In contrast, MECA-79 antigen expression in PDAC cells was significantly lower than that in NPDEs (Fig 3).
Fig 2. Representative microscopic images of immunohistochemistry and lectin-histochemistry in PDAC tissues.
Middle-power view of tissues stained with (A) HE, (B) β3Gn-T6, (C) T antigen (PNA), (D) Tn antigen (LU-35), (E) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (F) sLeX (CSLEX1), (G) sLeX (HECA-452), (H) sLeX on core 2 O-glycan (ST-439) and (I) MUC5AC. All these sections show the same region of PDAC tissue. In the left half of the panel, intraductal spreading of adenocarcinoma cells is seen, and invasive adenocarcinomas are present in the right half. All these antigens are expressed to various degrees of heterogeneity in the adenocarcinoma cells, even within the same case. Different staining patterns of sLeX are observed depending on the specificity of the antibodies used as described in the main text (F–H).
Table 3. Summary of glycan and its related antigen expression.
| antigens | β3Gn-T6 | T antigen | Tn antigen | MECA-79* | sLeX | MUC5AC | |||
|---|---|---|---|---|---|---|---|---|---|
| (CSLEX1) | (HECA-452) | (ST-439) | |||||||
| PDAC components | |||||||||
| Well differentiated adenocarcinoma | 10/38 (26.3%) | 3/38 (7.9%) | 29/38 (76.3%) | 1/38 (2.6%) | 25/38 (65.8%) | 32/38 (84.2%) | 14/38 (36.8%) | 17/38 (44.7%) | |
| Moderately differentiated adenocarcinoma | 7/38 (18.4%) | 4/38 (10.5%) | 35/38 (92.1%) | 3/38 (7.9%) | 35/38 (92.1%) | 37/38 (97.3%) | 30/38 (78.9%) | 6/38 (15.8%) | |
| Poorly differentiated adenocarcinoma | 0/26 (0%) | 6/26 (23.1%) | 17/26 (65.4%) | 2/26 (7.7%) | 20/26 (76.9%) | 21/26 (80.8%) | 17/26 (65.4%) | 1/26 (3.8%) | |
| Squamous cell carcinoma | 0/6 (0%) | 0/6 (0%) | 1/6 (16.7%) | 0/6 (0%) | 0/6 (0%) | 0/6 (0%) | 0/6 (0%) | 0/6 (0%) | |
| Premalignant lesion | |||||||||
| PanIN 1 | 7/21 (33.3%) | 10/21 (47.6%) | 17/21 (81.0%) | 0/21 (0%) | 8/21 (38.1%) | 5/21 (23.8%) | 0/21 (0%) | 7/21 (33.3%) | |
| PanIN 2 | 7/17 (41.2%) | 5/17 (29.4%) | 12/17 (70.6%) | 0/17 (0%) | 4/17 (23.5%) | 6/17 (35.3%) | 0/17 (0%) | 8/17 (47.1%) | |
| Normal tissue | |||||||||
| Pancreatic duct epithelial cell | 0/35 (0%) | 0/35 (0%) | 1/35 (2.9%) | 31/35 (88.6%) | 0/35 (0%) | 10/35 (28.6%) | 1/35 (2.9%) | 0/35 (0%) | |
| Acinar cell | 0/35 (0%) | 4/35 (11.4%) | 14/35 (40.0%) | 0/35 (0%) | 1/35 (2.9%) | 10/35 (28.6%) | 0/35 (0%) | 0/35 (0%) | |
| Islet cell | 0/36 (0%) | 9/36 (25.0%) | 1/36 (2.8%) | 0/36 (0%) | 2/36 (5.6%) | 0/36 (0%) | 1/36 (2.8%) | 0/36 (0%) | |
Cancer tissues of 40 cases selected randomly are subdivided into each component. Premalignant lesions were selected in non-cancerous area of the pancreas in PDAC cases. Normal pancreatic tissue at least 2 cm far from cancer cells are used in this assay. The number of tissues in which more than 50% of each component is positive for each antigen out of total tissues which contain each component is indicated.
*6-sulfo N-acetyllactosamine on extended core 1 O-glycan
Fig 3. Comparison of glycan antigens and β3Gn-T6 expression among PDACs (n = 156), PanINs (n = 26), and normal pancreatic tissues (n = 35).
((A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Boxes represent medians and interquartile ranges. Crosses represent mean values. Whiskers represent the minimum and maximum 1.5 interquartile ranges. Circles represent extremes. All glycan antigens, except MECA-79 antigen, are expressed significantly more highly in PDAC cells than in NPDEs. MECA-79 antigen expression in PDAC cells is significantly lower than that in NPDEs. Exp-scores were compared and analyzed using the Friedman’s test.
The T antigen: This antigen was found to be expressed in some of the well or moderately differentiated PDAC cells but not in NPDEs. Over 30% of low-grade PanINs expressed the T antigen (Table 3). T antigen expression was mildly higher in PDAC cells compared to NPDEs (Fig 3).
The Tn antigen: The majority of PDAC cells and PanINs expressed the Tn antigen, but most NPDEs did not (Table 3). Tn antigen expression in PDAC cells was markedly higher, and most of the cases were strongly positive, i.e., the Exp-score was >100 (Fig 3).
MECA-79 antigen: In contrast to NPDEs, which usually express MECA-79 antigen, PDAC cells were found to rarely express it, whereas PanINs did not express it at all (Table 3 and Fig 3).
SLeX: PDAC cells expressed sLeX strongly and at a high frequency, regardless of the antibodies applied. However, PanINs and NPDEs showed different profiles depending on the antibodies used (Table 3 and Fig 3). Antibody ST-439 identified the limited sLeX antigen, sLeX on core 2 O-glycan, so that ST-439+ PDAC cells also stained with antibodies CSLEX1 or HECA-452. Antibodies CSLEX1 and HECA-452 recognize both O-linked and N-linked sLeX. Antibodies HECA-452 and ST-439, but not CSLEX1, can recognize sulfated sLeX [2, 18], These features can be summarized: (1) both staining frequency and area were ranked as follows, in ascending order: HECA-452, CSLEX1, and ST-439; (2) potentially sulfated sLeX was found in MECA-79+ NPDEs, where HECA-452 staining was sometimes present while CSLEX1 staining was not; (3) low-grade PanINs were positive for HECA-452 staining and CSLEX1 staining, and normal epithelial cells were positive for HECA-452 staining but almost negative for ST-439 staining. These results suggest that PanINs and epithelial cells did not express core 2 O-glycan.
β3Gn-T6: β3Gn-T6 was expressed in ~20% of PDAC cells and 30–40% of low-grade PanINs but not in NPDEs (Table 3). Higher histological differentiation was associated with a higher level of β3Gn-T6+ in PDAC cells. NPDEs typically have a pancreatobiliary phenotype, whereas low-grade PanINs usually have a gastric phenotype [23, 34]. Furthermore, β3Gn-T6 is normally expressed in normal gastric foveolar cells as well as colonic goblet cells [8]. It is possible that β3Gn-T6 is expressed in cells with the gastric foveolar phenotype. When double immunohistochemical staining for β3Gn-T6 and MUC5AC was performed, both antigens were often found to be expressed in the same PDAC cells (Fig 4). In addition, there was a significant correlation between them, with a high correlation coefficient (ρ = 0.49; Table 4).
Fig 4. Double immunohistochemistry for β3Gn-T6 and MUC5AC.
Low-power view of histological staining (A) and double immunohistochemical staining (B) and high-power view of double immunohistochemical staining (C). Dotlike staining of β3Gn-T6 (green) and membranous staining of MUC5AC (brown) are often present in the same adenocarcinoma cells.
Table 4. Correlations among glycans and related proteins (Spearman's correlation coefficient value).
| β3Gn-T6 | T antigen | Tn antigen | MECA-79*** | sLeX | |||
|---|---|---|---|---|---|---|---|
| (CSLEX1) | (HECA-452) | (ST-439) | |||||
| T antigen | R = 0.16* | ||||||
| Tn antigen | R = 0.066 | R = 0.13 | |||||
| MECA-79*** | R = -0.17* | R = 0.13 | R = -0.032 | ||||
| sLeX (CSLEX1) | R = 0.064 | R = -0.047 | R = 0.081 | R = 0.11 | |||
| sLeX (HECA-452) | R = -0.11 | R = -0.075 | R = 0.034 | R = -0.080 | R = 0.38** | ||
| sLeX (ST-439) | R = 0.036 | R = -0.0010 | R = 0.13 | R = 0.13 | R = 0.69** | R = 0.32** | |
| MUC5AC | R = 0.49** | R = 0.19* | R = 0.19* | R = -0.20* | R = 0.12 | R = 0.016 | R = 0.15 |
*Correlation is significant at the 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed).
***6-sulfo N-acetyllactosamine on extended core 1 O-glycan
Relation between glycan expression and clinicopathological variables
The correlation between glycan expression in PDAC cells and various clinicopathological factors was examined next. Significant correlations were found only between higher β3Gn-T6 expression in PDAC cells and a lower histological grade, between higher MECA-79 antigen expression and a higher histological grade, and between higher sLeX expression (staining with antibody HECA-452) and a lower histological grade (Table 1 and S2 Fig).
Next, we evaluated correlations among expression levels of different glycans. We compared the Exp-scores of all glycans by Spearman’s test (Table 4). Scores on sLeX detected by different antibodies correlated positively. In addition, a few significant correlations were found between β3Gn-T6 and MUC5AC (ρ = 0.49) and between β3Gn-T6 and T antigen (ρ = 0.16), and a negative correlation was found between β3Gn-T6 and MECA-79 antigen (ρ = −0.17).
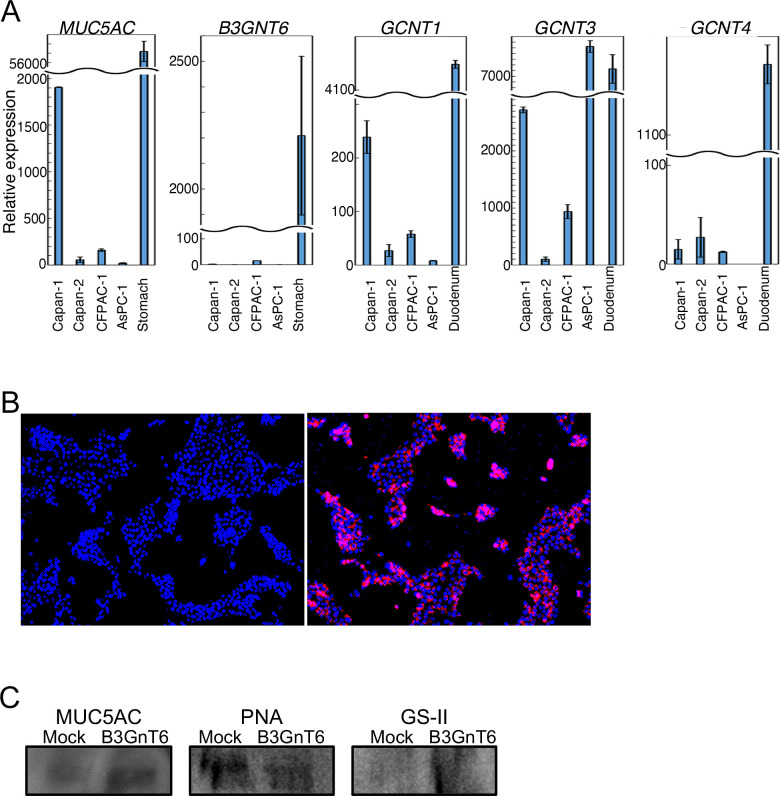
MUC5AC carries core 3 O-glycan generated by B3GNT6 gene expression in pancreatic cancer cells
To investigate whether MUC5AC contains core 3 O-glycan, we examined glycosylation status of MUC5AC. To select suitable pancreatic cancer cells for the assay, we analyzed the expression of genes B3GNT6 (encoding β3Gn-T6) and MUC5AC, together with genes encoding core 2 synthases (GCNT1, GCNT3, and GCNT4) by qRT-PCR. We chose Capan-1 cells because they show almost no expression of B3GNT6 and higher expression of MUC5AC compared to the other cell lines (Fig 5A). The immunofluorescence assay revealed that GFP-positive stably B3GNT6-transduced cells, Capan1-B3GnT6 expressed the β3Gn-T6 protein (Fig 5B). The N-acetylglucosaminyl terminus of core 3 O-glycan can be detected by a lectin called GS-II [21]. MUC5AC that was immunoprecipitated from the lysates of Capan1-B3GnT6 and Capan1-mock cells was subjected to SDS-PAGE followed by western blotting with GS-II (Fig 5C). An intense band was produced by MUC5AC isolated from Capan1-B3GnT6 cells. In contrast, no band was yielded by the MUC5AC isolated from Capan1-mock cells, even though anti-MUC5AC stained bands were comparable between them. These results indicated that MUC5AC from Capan1-B3GnT6 had core 3 O-glycan. In support of this finding, PNA binding to MUC5AC was lower in Capan1-B3GnT6 cells compared with Capan1-mock cells (Fig 5C). It was confirmed that core 3 O-glycan was present on MUC5AC isolated from Capan1-B3GnT6 cells, and that this glycan was synthesized by β3Gn-T6.
Fig 5. MUC5AC has core 3 O-glycan generated by B3GNT6 gene expression in pancreatic cancer cells.
(A) Comparison of expression of genes MUC5AC, B3GNT6, and core 2 O-glycan synthase among PDAC cells. Capan-1 cells express MUC5AC more highly than the other cell lines but do not express B3GNT6. (B) Capan1-B3GnT6 cells (right panel) but not Capan1-mock cells (left panel) express β3Gn-T6 as detected by the immunofluorescence assay (red). Nuclei are stained by 4’,6-diamindino-2-phenylindole (DAPI, blue). (C) MUC5AC immunoprecipitated with the anti-MUC5AC antibody was subjected to SDS-PAGE and transferred to a nitrocellulose membrane, then the membrane was blotted with GS-II, PNA, or the anti-MUC5AC antibody. The level of nonreducing terminal GlcNAc is higher in Capan1-B3GnT6 cells compared to Capan1-mock cells, even though the MUC5AC amount is comparable between these two cell lines. Conversely, the T antigen level is lower in Capan1-B3GnT6 cells compared to Capan1-mock cells.
Prognostic significance of glycan-related antigens in PDAC cells
Kaplan–Meier survival analyses revealed a statistically significant association between higher expression of β3Gn-T6 in PDAC cells and longer DFS (Fig 6). Patients with higher sLeX (staining with CSLEX1) expression tended to have shorter DFS. No significant association was found between any other glycan expression and patient outcomes (DFS or OS). No significant association was found between OS and β3Gn-T6 expression (S3 Fig).
Fig 6.
Kaplan-Meier survival curves for disease-free survival in patients with PDAC according to (A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Patients having PDAC with higher expression of β3Gn-T6 (red line) show a significantly longer survival compared to those with lower expression of β3Gn-T6 (blue line) in A. Patients having PDAC with higher expression of sLeX (CSLEX1) (red line) show a tendency to be shorter survival compared to those with lower expression of sLeX (CSLEX1) (blue line) in E. The other antigens are not significantly associated with patient outcome.
Cox proportional analysis of the groups categorized by each glycan expression and β3Gn-T6 expression in PDAC cells as well as conventional clinicopathological variables are shown in Table 5. Data on variables found to be significant by univariate analysis were subjected to multivariate analysis. In the latter, several variables (age, lymph node metastasis, nerve plexus invasion, tumor histological grade, and β3Gn-T6 expression) were found to be significantly associated with DFS.
Table 5. Univariate and multivariate analyses of prognostic factors associated with disease-free survival (A) and and overall survival (B) in patients with pancreatic ductal adenocarcinoma (n = 156).
| Cox univariate analysis | Cox multivariate analysis | ||||
|---|---|---|---|---|---|
| HR (95%CI) | P value | HR (95%CI) | P value | ||
| Gender: Male vs. Female | 0.9 (0.62–1.3) | 0.6 | |||
| Age (year): ≤69 vs. ≥70 | 0.56 (0.39–0.81) | 0.0024 | 0.66 (0.45–0.97) | 0.036 | |
| Adjuvant chemotherapy: No vs. Yes | 0.82 (0.54–1.2) | 0.34 | |||
| Tumor size (mm): <35 vs. ≥35 | 1.5 (1.0–2.1) | 0.042 | |||
| Tumor grade: 1 vs. 2 and 3 | 1.8 (1.2–2.9) | 0.0068 | 1.8 (1.2–2.9) | 0.0069 | |
| Lymphatic invasion: Low vs. High | 1.3 (0.74–2.2) | 0.4 | |||
| Venous invasion: Low vs. High | 1.7 (1.1–2.7) | 0.02 | |||
| Intrapancreatic neural invasion: Low vs. High | 1.6 (1.1–2.3) | 0.028 | |||
| Nerve plexus invasion: Low vs. High | 1.7 (1.1–2.4) | 0.0085 | 1.6 (1.1–2.4) | 0.022 | |
| Lymph node metastasis: No vs. Yes | 2.2 (1.4–3.6) | 0.0012 | 1.7 (1.0–2.9) | 0.035 | |
| Distant metastasis: No vs. Yes | 1.6 (0.74–3.4) | 0.24 | |||
| Surgical margin: Negative vs. Positive | 1.4 (0.97–2.2) | 0.07 | |||
| β3Gn-T6: Low vs. High | 0.63 (0.43–0.92) | 0.016 | 0.65 (0.44–0.95) | 0.024 | |
| T antigen: Low vs. High | 0.93 (0.64–1.3) | 0.69 | |||
| Tn antigen: Low vs. High | 1.1 (0.79–1.7) | 0.48 | |||
| MECA-79*: Low vs. High | 1.1 (0.76–1.6) | 0.61 | |||
| sLeX (CSLEX1): Low vs. High | 1.4 (0.97–2.0) | 0.068 | |||
| sLeX (HECA-452): Low vs. High | 0.9 (0.62–1.3) | 0.56 | |||
| sLeX (ST-439): Low vs. High | 1.1 (0.74–1.5) | 0.72 | |||
| (B) | |||||
| Cox univariate analysis | Cox multivariate analysis | ||||
| HR (95%CI) | P value | HR (95%CI) | P value | ||
| Gender: Male vs. Female | 0.84 (0.53–1.3) | 0.45 | |||
| Age (year): ≤69 vs. ≥70 | 0.61 (0.38–0.97) | 0.037 | 0.6 (0.37–0.96) | 0.035 | |
| Adjuvant chemotherapy: No vs. Yes | 0.76 (0.45–1.3) | 0.3 | |||
| Tumor size (mm): <35 vs. ≥35 | 2.2 (1.3–3.5) | 0.0016 | 2.0 (1.2–3.2) | 0.0067 | |
| Tumor grade: 1 vs. 2 and 3 | 2.2 (1.3–4.0) | 0.0053 | 2.3 (1.3–4.0) | 0.0054 | |
| Lymphatic invasion: Low vs. High | 1.1 (0.58–2.1) | 0.78 | |||
| Venous invasion: Low vs. High | 1.8 (1.0–3.2) | 0.037 | |||
| Intrapancreatic neural invasion: Low vs. High | 1.5 (0.96–2.5) | 0.075 | |||
| Nerve plexus invasion: Low vs. High | 1.9 (1.2–3.1) | 0.0054 | 1.7 (1.1–2.8) | 0.022 | |
| Lymph node metastasis: No vs. Yes | 1.9 (1.0–3.3) | 0.037 | |||
| Distant metastasis: No vs. Yes | 1.2 (0.48–3.0) | 0.69 | |||
| Surgical margin: Negative vs. Positive | 1.7 (1.1–2.8) | 0.027 | |||
| β3Gn-T6: Low vs. High | 0.82 (0.52–1.3) | 0.4 | |||
| T antigen: Low vs. High | 0.85 (0.54–1.3) | 0.48 | |||
| Tn antigen: Low vs. High | 1.4 (0.87–2.2) | 0.17 | |||
| MECA-79*: Low vs. High | 0.97 (0.61–1.5) | 0.89 | |||
| sLeX (CSLEX1): Low vs. High | 1.3 (0.8–2.0) | 0.32 | |||
| sLeX (HECA-452): Low vs. High | 0.74 (0.47–1.2) | 0.2 | |||
| sLeX (ST-439): Low vs. High | 1.1 (0.71–1.8) | 0.64 | |||
*6-sulfo N-acetyllactosamine on extended core 1 O-glycan
Discussion
Mucin-type O-glycan is known to be involved in tumor development and malignant characteristics. However, its clinicopathological significance has not yet been sufficiently elucidated. Here, we investigated the clinicopathological significance of both O-glycan cores and peripheral modified glycans in PDAC. Higher β3Gn-T6 expression was noted in more differentiated adenocarcinoma in PDAC patients. These PDAC cases showed significantly longer DFS. Together with previous reports indicating that forced expression of β3Gn-T6 reduces the aggressiveness of cancers in vitro and in vivo [8, 21, 22], our findings suggest that β3Gn-T6 expression in PDAC cells is a favorable prognostic indicator. In addition, the expression of β3Gn-T6 in PDAC cells and PanINs significantly correlated with the expression of MUC5AC in these cells, implying that β3Gn-T6 expression is related to cellular differentiation status of the gastric foveolar phenotype. The expression of the T antigen, Tn antigen, sLeX antigen, and sLeX on core 2 O-glycan was higher in PDAC cells. Unexpectedly, we did not find any significant association with patient outcome in our cohort. However, 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79 antigen) was underexpressed in PDAC cells compared to NPDEs and was not associated with patient outcome.
Core 3 O-glycan is widely distributed throughout the gastrointestinal tract [35] and is synthesized only by β3Gn-T6 expressed normally in gastric foveolar epithelial cells and colonic goblet cells [8]. β3Gn-T6 is not expressed in normal pancreatic tissue, and the induction of β3Gn-T6 has been previously found in some low-grade PanINs and differentiated PDAC cells (Table 3). Takano et al. have reported that MUC5AC+ PDAC tends to be a more differentiated adenocarcinoma [36]. In our study, these tumors were found to start expressing β3Gn-T6, which significantly correlated with MUC5AC expression (Fig 4 and Table 4). These results suggest that this induction of expression may be associated with gastric metaplasia.
Carcinoma cells, such as colonic, prostate, and pancreatic cancer cells [8, 21, 22], reduce their aggressiveness in vitro or in vivo when forced to express β3Gn-T6. Forced expression of the core 3 structure destabilizes oncoprotein MUC1 [22], affecting downstream signals and upregulating cell cycle inhibitor p21 [22]. The expression of β3Gn-T6 also leads to a reduction in the formation of the α2β1 integrin complex, subsequently reducing the level of phosphorylated FAK relative to total FAK, thereby leading to decreased tumor progression [21, 22]. β3Gn-T6 alters cancer cell invasion through impairment of actin stress fiber organization [21, 37]. Here, we demonstrated clinical significance of β3Gn-T6 expression, which turned out to be a favorable prognostic factor in PDAC, consistent with the known effects of β3Gn-T6 in cancer biology.
In the biosynthesis of O-glycans (Fig 1), the processes of formation of core 1 and core 3 structures compete with each other for the same substrate, although the expression levels of T antigen and β3Gn-T6 only weakly correlated in PDAC. This finding suggests that the core 1 structure (T antigen) is mostly modified, i.e., by extension, branching, or sialylation, which are not recognized by PNA. The extended core 1 structure detected by antibody MECA-79, which was only a limited 6-sulfated structure of extended core 1, weakly but statistically significantly negatively correlated with β3Gn-T6 levels (Table 4).
The Tn antigen is one of the representative truncated structures, whose expression is abundant in many types of carcinoma cells owing to the loss of Cosmc, a chaperone for core 1 synthase [9, 38]. Our study revealed that the positivity and Exp-score of the Tn antigen in PDAC cells were high (Table 3 and Fig 3), despite the high expression of sLeX in PDAC cells, suggesting that Cosmc inactivation does not entirely explain the presence of the Tn antigen in our cohort.
This study has several limitations. First, data collection and analyses were performed retrospectively. Second, it was difficult to investigate detailed glycan structural alterations and their changed biosynthesis in cancer cells in clinical samples, because of the lack of antibodies specific for various glycan structures. Therefore, our conclusions are drawn from speculation based on the limited findings. Further studies would be warranted to clarify the molecular mechanism of glycan alterations in PDAC.
In summary, this study is the first to report on the clinicopathological significance of β3Gn-T6 expression in PDAC. β3Gn-T6 was found to be expressed most highly in PDAC cells in differentiated adenocarcinoma and was significantly associated with longer DFS in PDAC patients. Our findings on the molecular mechanisms underlying the induction of core 3 O-glycan in PDAC provide a basis for its use as a therapeutic tool.
Supporting information
Positive staining in immunohistochemical or lectin-histochemical analyses for β3Gn-T6 (B,C), T antigen (staining with PNA) (E,F), Tn antigen (staining with LU-35) (H,I), 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (staining with MECA-79) (K,L), sLeX (staining with CSLEX1) (N,O), sLeX (staining with HECA-452) (Q,R), sLeX on core 2 O-glycan (staining with ST-439) (T,U), and MUC5AC (W,X) was investigated, and their corresponding histological features were revealed by hematoxylin and eosin staining (A, D, G, J, M, P, S, V). The left and the central panels of the photos are a middle-power view, and the right one is a high-power view. (A–C) Cytoplasmic dotlike staining in moderately differentiated adenocarcinoma cells was found by β3Gn-T6 immunohistochemical analysis, whose pattern was consistent with staining in the Golgi apparatus. (D–F) Cytoplasmic staining, especially in the apical portion of adenocarcinoma cells, was found in PNA lectin-histochemical analysis. (G–I) LU-35 staining yielded a cytoplasmic and sometimes membranous pattern, especially on the luminal surface of the carcinoma gland. (J–L) Mainly membranous staining of MECA-79, especially in the luminal surface of NPDEs, was observed in normal pancreatic tissue. (M–O) Cytoplasmic and membranous staining in adenocarcinoma cells was detected by CSLEX1 immunohistochemistry. (P–R) HECA-452 staining yielded both membranous and cytoplasmic patterns. (S–U) ST-439 staining showed positive cytoplasmic and membranous patterns in some cancer cells. (V–X) MUC5AC usually stained in adenocarcinoma cells with clear to light eosinophilic cytoplasm.
(TIF)
(A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Boxes represent medians and interquartile ranges. Crosses represent mean values. Whiskers represent the minimum and maximum 1.5 interquartile ranges. Circles represent extremes. Exp-scores were compared and analyzed using the Kruskal–Wallis test followed by Dunn–Bonferroni's post hoc analysis.
(TIF)
Kaplan-Meier survival curves for OS in patients with PDAC according to (A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Any antigens are not significantly associated with patient outcome.
(TIF)
(DOCX)
Acknowledgments
We thank Ms. Sachiko Miura and Toshiko Sakaguchi for excellent techniques. We are grateful to the National Cancer Center Biobank for the tissue samples used in this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by a Japan Society for the Promotion of Science (NH) and the Japan Agency for Medical Research and Development (NH).
References
- 1.Karasawa F, Shiota A, Goso Y, Kobayashi M, Sato Y, Masumoto J, et al. Essential role of gastric gland mucin in preventing gastric cancer in mice. J Clin Invest. 2012;122(3):923–34. Epub 2012/02/07. 10.1172/JCI59087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitoma J, Fukuda M. Core O-glycans required for lymphocyte homing gene knockout mice of core 1 beta1,3-N-acetylglucosaminyltransferase and core 2 N-acetylglucosaminyltransferase. Methods Enzymol. 2010;479:257–70. Epub 2010/09/08. 10.1016/S0076-6879(10)79015-7 . [DOI] [PubMed] [Google Scholar]
- 3.Yeh JC, Hiraoka N, Petryniak B, Nakayama J, Ellies LG, Rabuka D, et al. Novel sulfated lymphocyte homing receptors and their control by a Core1 extension beta 1,3-N-acetylglucosaminyltransferase. Cell. 2001;105(7):957–69. Epub 2001/07/06. 10.1016/s0092-8674(01)00394-4 . [DOI] [PubMed] [Google Scholar]
- 4.Varki A, Kannagi R, Toole B, Stanley P. Glycosylation Changes in Cancer In: rd, Varki A, Cummings RD, Esko JD, Stanley P, Hart GW, et al. , editors. Essentials of Glycobiology. Cold Spring Harbor (NY)2015. p. 597–609. [Google Scholar]
- 5.Pinho SS, Reis CA. Glycosylation in cancer: mechanisms and clinical implications. Nat Rev Cancer. 2015;15(9):540–55. Epub 2015/08/21. 10.1038/nrc3982 . [DOI] [PubMed] [Google Scholar]
- 6.Brockhausen I, Stanley P. O-GalNAc Glycans In: rd, Varki, Cummings RD, Esko JD, Stanley P, Hart GW, et al. , editors. Essentials of Glycobiology. Cold Spring Harbor; (NY: )2015. p. 113–23. [Google Scholar]
- 7.Cazet A, Julien S, Bobowski M, Burchell J, Delannoy P. Tumour-associated carbohydrate antigens in breast cancer. Breast Cancer Res. 2010;12(3):204 Epub 2010/06/17. 10.1186/bcr2577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwai T, Kudo T, Kawamoto R, Kubota T, Togayachi A, Hiruma T, et al. Core 3 synthase is down-regulated in colon carcinoma and profoundly suppresses the metastatic potential of carcinoma cells. Proc Natl Acad Sci U S A. 2005;102(12):4572–7. Epub 2005/03/10. 10.1073/pnas.0407983102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radhakrishnan P, Dabelsteen S, Madsen FB, Francavilla C, Kopp KL, Steentoft C, et al. Immature truncated O-glycophenotype of cancer directly induces oncogenic features. Proc Natl Acad Sci U S A. 2014;111(39):E4066–75. Epub 2014/08/15. 10.1073/pnas.1406619111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsuboi S, Sutoh M, Hatakeyama S, Hiraoka N, Habuchi T, Horikawa Y, et al. A novel strategy for evasion of NK cell immunity by tumours expressing core2 O-glycans. EMBO J. 2011;30(15):3173–85. Epub 2011/06/30. 10.1038/emboj.2011.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hruban RH, Adsay NV, Esposito I, Fukuchima N, Furukawa T, Kloeppel G, et al. Pancreatic ductal adenocarcinoma In: Board WCoTE, editor. World Health Organization Classification of Tumours 5th Edition Digestive System Tumours. World Health Organization Classification of Tumours. 5th ed Lyon: IARCPress; 2019. p. 322–32. [Google Scholar]
- 12.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. Epub 2018/01/10. 10.3322/caac.21442 . [DOI] [PubMed] [Google Scholar]
- 13.Itzkowitz S, Kjeldsen T, Friera A, Hakomori S, Yang US, Kim YS. Expression of Tn, sialosyl Tn, and T antigens in human pancreas. Gastroenterology. 1991;100(6):1691–700. Epub 1991/06/01. 10.1016/0016-5085(91)90671-7 . [DOI] [PubMed] [Google Scholar]
- 14.Mereiter S, Balmana M, Gomes J, Magalhaes A, Reis CA. Glycomic Approaches for the Discovery of Targets in Gastrointestinal Cancer. Front Oncol. 2016;6:55 Epub 2016/03/26. 10.3389/fonc.2016.00055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munkley J. The glycosylation landscape of pancreatic cancer. Oncol Lett. 2019;17(3):2569–75. Epub 2019/03/12. 10.3892/ol.2019.9885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takahashi S, Oda T, Hasebe T, Sasaki S, Kinoshita T, Konishi M, et al. Overexpression of sialyl Lewis x antigen is associated with formation of extratumoral venous invasion and predicts postoperative development of massive hepatic metastasis in cases with pancreatic ductal adenocarcinoma. Pathobiology. 2001;69(3):127–35. Epub 2002/03/02. 10.1159/000048767 . [DOI] [PubMed] [Google Scholar]
- 17.Streeter PR, Rouse BT, Butcher EC. Immunohistologic and functional characterization of a vascular addressin involved in lymphocyte homing into peripheral lymph nodes. J Cell Biol. 1988;107(5):1853–62. Epub 1988/11/01. 10.1083/jcb.107.5.1853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumamoto K, Mitsuoka C, Izawa M, Kimura N, Otsubo N, Ishida H, et al. Specific detection of sialyl Lewis X determinant carried on the mucin GlcNAcbeta1—>6GalNAcalpha core structure as a tumor-associated antigen. Biochem Biophys Res Commun. 1998;247(2):514–7. Epub 1998/06/27. 10.1006/bbrc.1998.8824 . [DOI] [PubMed] [Google Scholar]
- 19.Watanabe M, Ohishi T, Kuzuoka M, Nudelman ED, Stroud MR, Kubota T, et al. In vitro and in vivo antitumor effects of murine monoclonal antibody NCC-ST-421 reacting with dimeric Le(a) (Le(a)/Le(a)) epitope. Cancer Res. 1991;51(8):2199–204. Epub 1991/04/15. . [PubMed] [Google Scholar]
- 20.Maruyama M, Kobayashi M, Sakai Y, Hiraoka N, Ohya A, Kageyama S, et al. Periductal induction of high endothelial venule-like vessels in type 1 autoimmune pancreatitis. Pancreas. 2013;42(1):53–9. Epub 2012/07/04. 10.1097/MPA.0b013e318258ce4c . [DOI] [PubMed] [Google Scholar]
- 21.Lee SH, Hatakeyama S, Yu SY, Bao X, Ohyama C, Khoo KH, et al. Core3 O-glycan synthase suppresses tumor formation and metastasis of prostate carcinoma PC3 and LNCaP cells through down-regulation of alpha2beta1 integrin complex. J Biol Chem. 2009;284(25):17157–69. Epub 2009/04/28. 10.1074/jbc.M109.010934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radhakrishnan P, Grandgenett PM, Mohr AM, Bunt SK, Yu F, Chowdhury S, et al. Expression of core 3 synthase in human pancreatic cancer cells suppresses tumor growth and metastasis. Int J Cancer. 2013;133(12):2824–33. Epub 2013/06/12. 10.1002/ijc.28322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basturk O, Esposito I, Fukuchima N, Furukawa T, Hong SM, Kloeppel G, et al. Pancreatic intraepithelial neoplasia In: Board WCoTE, editor. World Health Organization Classification of Tumours 5th Edition Digestive System Tumours. World Health Organization Classification of Tumours. 5th ed Lyon: IARCPress; 2019. p. 307–9. [Google Scholar]
- 24.Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 8th ed Hoboken, NJ: Wiley-Blackwell; 2017. [Google Scholar]
- 25.Japan-Pancreas-Society. Classification of Pancreatic Cancer. 3rd English ed Tokyo, Japan: Kanehara; 2011. [Google Scholar]
- 26.Ino Y, Yamazaki-Itoh R, Oguro S, Shimada K, Kosuge T, Zavada J, et al. Arginase II expressed in cancer-associated fibroblasts indicates tissue hypoxia and predicts poor outcome in patients with pancreatic cancer. PLoS One. 2013;8(2):e55146 10.1371/journal.pone.0055146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oguro S, Ino Y, Shimada K, Hatanaka Y, Matsuno Y, Esaki M, et al. Clinical significance of tumor-infiltrating immune cells focusing on BTLA and Cbl-b in patients with gallbladder cancer. Cancer Sci. 2015;106(12):1750–60. Epub 2015/09/24. 10.1111/cas.12825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiraoka N, Yamazaki-Itoh R, Ino Y, Mizuguchi Y, Yamada T, Hirohashi S, et al. CXCL17 and ICAM2 Are Associated With a Potential Anti-Tumor Immune Response in Early Intraepithelial Stages of Human Pancreatic Carcinogenesis. Gastroenterology. 2011;140(1):310–+. 10.1053/j.gastro.2010.10.009 WOS:000285503200046. [DOI] [PubMed] [Google Scholar]
- 29.Magalhaes A, Rossez Y, Robbe-Masselot C, Maes E, Gomes J, Shevtsova A, et al. Muc5ac gastric mucin glycosylation is shaped by FUT2 activity and functionally impacts Helicobacter pylori binding. Sci Rep. 2016;6:25575 Epub 2016/05/11. 10.1038/srep25575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Magalhaes A, Gomes J, Ismail MN, Haslam SM, Mendes N, Osorio H, et al. Fut2-null mice display an altered glycosylation profile and impaired BabA-mediated Helicobacter pylori adhesion to gastric mucosa. Glycobiology. 2009;19(12):1525–36. Epub 2009/08/27. 10.1093/glycob/cwp131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharma V, Srinivas VR, Adhikari P, Vijayan M, Surolia A. Molecular basis of recognition by Gal/GalNAc specific legume lectins: influence of Glu 129 on the specificity of peanut agglutinin (PNA) towards C2-substituents of galactose. Glycobiology. 1998;8(10):1007–12. Epub 1998/08/28. 10.1093/glycob/8.10.1007 . [DOI] [PubMed] [Google Scholar]
- 32.Hirohashi S, Clausen H, Yamada T, Shimosato Y, Hakomori S. Blood group A cross-reacting epitope defined by monoclonal antibodies NCC-LU-35 and -81 expressed in cancer of blood group O or B individuals: its identification as Tn antigen. Proc Natl Acad Sci U S A. 1985;82(20):7039–43. 10.1073/pnas.82.20.7039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitoma J, Miyazaki T, Sutton-Smith M, Suzuki M, Saito H, Yeh JC, et al. The N-glycolyl form of mouse sialyl Lewis X is recognized by selectins but not by HECA-452 and FH6 antibodies that were raised against human cells. Glycoconj J. 2009;26(5):511–23. Epub 2008/12/18. 10.1007/s10719-008-9207-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yonezawa S, Higashi M, Yamada N, Yokoyama S, Goto M. Significance of mucin expression in pancreatobiliary neoplasms. J Hepatobiliary Pancreat Sci. 2010;17(2):108–24. Epub 2009/09/30. 10.1007/s00534-009-0174-7 . [DOI] [PubMed] [Google Scholar]
- 35.Robbe C, Capon C, Coddeville B, Michalski JC. Structural diversity and specific distribution of O-glycans in normal human mucins along the intestinal tract. Biochem J. 2004;384(Pt 2):307–16. Epub 2004/09/14. 10.1042/BJ20040605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takano Y, Ohike N, Tajiri T, Asonuma K, Harada K, Takahashi H, et al. Gastric- and intestinal-type marker expression in invasive ductal adenocarcinoma of the pancreas. Hepatobiliary Pancreat Dis Int. 2012;11(4):424–8. Epub 2012/08/16. 10.1016/s1499-3872(12)60202-1 . [DOI] [PubMed] [Google Scholar]
- 37.Clement M, Rocher J, Loirand G, Le Pendu J. Expression of sialyl-Tn epitopes on beta1 integrin alters epithelial cell phenotype, proliferation and haptotaxis. J Cell Sci. 2004;117(Pt 21):5059–69. Epub 2004/09/24. 10.1242/jcs.01350 . [DOI] [PubMed] [Google Scholar]
- 38.Ju T, Cummings RD. A unique molecular chaperone Cosmc required for activity of the mammalian core 1 beta 3-galactosyltransferase. Proc Natl Acad Sci U S A. 2002;99(26):16613–8. Epub 2002/12/05. 10.1073/pnas.262438199 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Positive staining in immunohistochemical or lectin-histochemical analyses for β3Gn-T6 (B,C), T antigen (staining with PNA) (E,F), Tn antigen (staining with LU-35) (H,I), 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (staining with MECA-79) (K,L), sLeX (staining with CSLEX1) (N,O), sLeX (staining with HECA-452) (Q,R), sLeX on core 2 O-glycan (staining with ST-439) (T,U), and MUC5AC (W,X) was investigated, and their corresponding histological features were revealed by hematoxylin and eosin staining (A, D, G, J, M, P, S, V). The left and the central panels of the photos are a middle-power view, and the right one is a high-power view. (A–C) Cytoplasmic dotlike staining in moderately differentiated adenocarcinoma cells was found by β3Gn-T6 immunohistochemical analysis, whose pattern was consistent with staining in the Golgi apparatus. (D–F) Cytoplasmic staining, especially in the apical portion of adenocarcinoma cells, was found in PNA lectin-histochemical analysis. (G–I) LU-35 staining yielded a cytoplasmic and sometimes membranous pattern, especially on the luminal surface of the carcinoma gland. (J–L) Mainly membranous staining of MECA-79, especially in the luminal surface of NPDEs, was observed in normal pancreatic tissue. (M–O) Cytoplasmic and membranous staining in adenocarcinoma cells was detected by CSLEX1 immunohistochemistry. (P–R) HECA-452 staining yielded both membranous and cytoplasmic patterns. (S–U) ST-439 staining showed positive cytoplasmic and membranous patterns in some cancer cells. (V–X) MUC5AC usually stained in adenocarcinoma cells with clear to light eosinophilic cytoplasm.
(TIF)
(A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Boxes represent medians and interquartile ranges. Crosses represent mean values. Whiskers represent the minimum and maximum 1.5 interquartile ranges. Circles represent extremes. Exp-scores were compared and analyzed using the Kruskal–Wallis test followed by Dunn–Bonferroni's post hoc analysis.
(TIF)
Kaplan-Meier survival curves for OS in patients with PDAC according to (A) β3Gn-T6, (B) T antigen (PNA), (C) Tn antigen (LU-35), (D) 6-sulfo N-acetyllactosamine on extended core 1 O-glycan (MECA-79), (E) sLeX (CSLEX1), (F) sLeX (HECA-452), and (G) sLeX on core 2 O-glycan (ST-439). Any antigens are not significantly associated with patient outcome.
(TIF)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.