Abstract
Objective
This study aimed to provide an insight into the impact of the early outbreak of the novel Coronavirus Disease 2019 on the care management for patients with congenital heart disease.
Methods
This study respectively enrolled a cohort of surgical patients who underwent surgery in 2018 (group I), 2019 (group II), and 2020 (group III) and a cohort of follow-up patients who had follow-up in 2017 (group A), 2018 (group B), and 2019 (group C) in 13 children hospitals.
Results
During the Coronavirus Disease 2019 era, there was a significant decrease in total surgical volume and a change in case mix in terms of an increase in the proportion of emergency operations. Decrease in migration scale index was correlated to the decrease in both surgical volume (r = 0.64, P = .02) and outpatient visit volume (r = 0.61, P = .03). There was a significantly higher proportion of patients who had follow-up through the internet or phone in group C (26.4% vs 9.6% in group B and 8.9% in group A; P < .0001). There was no statistical difference in death or rehospitalization among the 3 follow-up groups (P = .49). There was higher parents' anxiety score (P < .0001) and more use of telemedicine (P = .004) in group C compared with groups A and B.
Conclusions
The Coronavirus Disease 2019 pandemic has resulted in a considerable decrease in total surgical volume and a change of case mix, which seems to be related to the strict traffic ban. Follow-up through the online medical service appears to be an effective alternative to the conventional method.
Key Words: congenital heart disease, COVID-19, follow-up, surgery
Graphical abstract
Congenital heart surgery program during early COVID-19 outbreak in China.

There was a substantial decrease in pediatric cardiac surgeries during the early outbreak of COVID-19 in children's hospitals in China.
Central Message.
The COVID-19 pandemic has resulted in significant changes in congenital heart services, such as decrease in total surgical volumes, redistribution of the case mix, and change in follow-up strategies.
Perspective.
The public health responses to the COVID-19 pandemic have resulted in the deferral of surgery and limited access to structured follow-up in patients with CHD, potentially posing a big threat to this subgroup patients. Our results provide a platform for further study of better serving patients with CHD in terms of patient triage, tiered precautions, and optimizing allocation of resources during the COVID-19 era.
See Commentaries on pages 1615 and 1516.
The outbreak of the novel Coronavirus Disease 2019 (COVID-19) has enormously strained healthcare systems across the globe.1 , 2 Many hospitals, particularly those in epicenter areas, have curtailed or postponed surgical procedures in an effort to mitigate the disease transmission and preserve the resources to care for patients with COVID-19. In addition, patients' access to routine face-to-face visits is heavily restricted because of the aggressive actions taken by the local governments.
Congenital heart disease (CHD) remains a global public health concern.3 The majority of patients with CHD require surgical repair, and a considerable proportion of critically ill neonates require emergency operations.4 The ongoing worldwide pandemic has greatly affected the optimal treatments delivery to patients with CHD,5 , 6 potentially placing this population at increased risk for adverse outcomes. Of note, postoperative cardiovascular and noncardiovascular morbidity are common among this subgroup patients, particularly in those with complex CHD (CCHD), emphasizing the need for structured follow-up surveillance.7 Guidelines8 , 9 have stressed the importance of maximizing optimization of care for surgical patients during the COVID-19 era, including appropriate triage of cases as well as resource allocation, tiered precautions, use of telemedicine, and a detailed follow-up program. Because management care for CHD requires significant resources and an organized regional system,10 , 11 understanding how the current pandemic affects the congenital heart surgical program is paramount.
Chinese health authorities have taken strict, far-reaching antiepidemic actions in Wuhan since January 22, 2020.12 , 13 With the suppression of the outbreak of the new coronavirus disease, there has been a gradual recovery in healthcare provision in most areas since Wuhan instituted outbound travel restrictions on April 8, 2020. In the present study, we recruited 13 participating pediatric cardiac surgery intuitions in China, representing the major children hospitals in the National Association of Pediatric Cardiology and Cardiac Surgery (the annualized case volume in each hospital in this association constitutes more than 60% of the CHD surgeries in the provinces/cities where these hospitals are located). Additionally, these 13 centers were located in the provinces where there was a reportedly considerable number of patients with a COVID-19 diagnosis. This study sought to evaluate the impact of early COVID-19 outbreak on the congenital heart surgery program and the outcomes of patients with repaired CCHD during this peak time when the COVID-19 forced significant changes in medical services in China.
Materials and Methods
Study Design, Participants, and Definitions
This multicenter observational cohort study included 13 pediatric tertiary cardiac centers (Figure E1) to survey the performance of CHD surgery and the follow-up program during the COVID-19 pandemic. The Ethics Committee approved this study, and informed consent was obtained. Data including the clinic and surgical information were retrospectively collected. Follow-up data including mortality and unplanned rehospitalization within 6 months after surgery were retrieved from the follow-up databases. Patients undergoing operations (surgical cohort) were classified into 3 groups. Groups I, II, and III refer to patients undergoing surgery between January 23 and April 8 in 2018, 2019, and 2020 (COVID-19 era), respectively. Patients who were discharged alive after surgical repair of CCHD and had follow-up (follow-up cohort) were also classified into 3 groups. Groups A and B refer to patients having follow-up between September 1 and December 31 in 2017 and 2018, respectively; group C refers to patients having follow-up between September 1, 2019, and January 23, 2020. Of note, there was a higher population in group C than groups A and B because additional data from January 1 to 23, 2020, were collected in group C, tending to better illustrate the impact of COVID-19. For patients discharged in 2017 and 2018, follow-up data including mortality and unplanned rehospitalization within 6 months after surgery were retrieved from the follow-up databases. Eleven patients (2.7%) were lost to follow-up in group A, and 13 patients (2.9%) were lost to follow-up in group B.
Figure E1.
The geographic location of the 13 participating centers in China.
Baidu migration14 is an open-source big data project characterizing population migration. Leveraging its location-based services system and Baidu Tianyan system, we obtained the daily migration scale index (MSI) from January 23 to April 8 in 2020 and 2019 of the cities where each recruited center is located. Haodaifu (Good-doctor) is one of the biggest online health services platform that provides online consultation services for patients.15 , 16 The number of network visits for each center from January 23 to April 8 in 2018, 2019, and 2020 was obtained from the customer service department as requested. Given the lack of nucleic acid testing outside the epicenter during this study period, each enrolled hospital followed a strict institutional protocol to control the spread of COVID-19, the principle of which included a 14-day quarantine duration before surgery (including patients and their parents) and negative pressure operation room plus personal protective equipment for emergency cases (Figure E2). During the 14-day quarantine duration, all patients and their parents were required to keep social distancing in a specific hotel near the hospitals and evaluation was done by specialized staff every day. During the hospital admission, clinical evaluation was made for patients and their parents. Examination including x-ray or computed tomography scan and serologic testing was also required. These principles were in line with the expert consensus guideline issued by the Chinese Medical Association for Pediatric Surgery17 , 18 and the policy of the local Health Bureau in 2020.
Figure E2.
The protocol of surgical program of surgical repair for CHDs during January 23 to April 8 in the enrolled centers across China. COVID-19, Coronavirus Disease 2019; CDC, Centers for Disease Control and Prevention; PPE, personal protective equipment.
Because of the impact of COVID-19, follow-up data for children in group C were collected from the parents by phone call or social media app (WeChat). We first send questionnaires (Table E1) to parents or guardians and collect the feedback data. In case of no feedback, we recontact the parents via phone or WeChat to complete the follow-up. If we are unable to contact the parents or guardian by telephone and WeChat, and cannot obtain follow-up records, this case is considered to be lost to follow-up. We contact all of the survivors' parents or guardians, asking about the follow-up modes and the degree of family anxiety during the COVID-19 outbreak. The definition of CCHD and detailed types have been reported by our group.18
Outcomes
For the follow-up cohort, the composite end point was all-cause mortality and unplanned readmission events during follow-up. All-cause mortality was defined as death from any causes that occurred after discharge. Unplanned readmission was defined as admission to a healthcare facility for any unexpected reason during follow-up. Deaths and unplanned readmissions in groups A and B were confirmed in the hospital medical record and self-reported in group C.
Statistical Analysis
Data normality was tested for each continuous variable. Summary statistics were reported as median (interquartile range [IQR]) or number (%). Patient characteristics were compared through the Kruskal–Wallis test for continuous variables and chi-square test for categorical variables. Kaplan–Meier curve was performed to show the difference in the cumulative probability of death or unplanned readmission among the 3 follow-up groups. A linear regression was performed to show the correlation between MSI (partially reflecting the traffic ban) and decrease in surgical volume as well as outpatient visit volume. All reported P values are 2-sided. All analyses are performed using SPSS version 24.0 (SPSS Inc, Chicago, Ill) and R version 4.0.0.
Results
Of the 13 hospitals, 5 were designated as hospitals to treat pediatric patients with COVID-19. A total of 47 nurses (7.5%) were assigned to support other departments in the same hospital, such as the infectious department or fever clinic, whereas no pediatric cardiologist or surgeon was assigned to support other departments. Only 1 hospital's congenital heart surgery program subsidiary intensive care unit was requisitioned for the treatment of children with COVID-19. There was a scarcity of nucleic acid and serologic antibody testing during the study period, so the majority of the staff except those in Wuhan Children's Hospital were not screened with swabs or serologic testing.
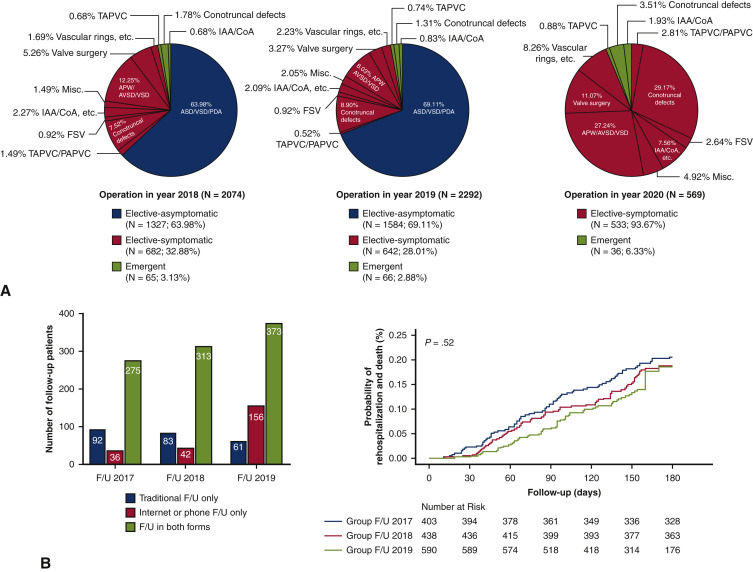
The median surgical volume per center during the COVID-19 era was 25 cases (IQR, 12-63), which was significantly lower than the volume in 2018 (148 cases; IQR, 83-198) and in 2019 (158 cases; IQR, 81-225) (P = .009). During this pandemic, the decrease in the surgical volume or outpatient visit volume in each center was not correlated with the number of confirmed COVID-19 cases in the province or municipality where the center was located (r = 0.374, P = .209 and r = 0.351, P = .436, respectively), but was positively correlated with the decrease in the Baidu MSI in the city where the center was located (r = 0.643, P = .018 and r = 0.614, P = .026) (Figure 1 ). The total number of both emergency and elective surgeries during the pandemic was less than those in the last 2 years (Table 1 , Figure 2 ). There was a change in case mix during the COVID-19 era (Figure 3 , A). First, as a proportion of total surgical volume, there was a relative increase of emergency operations (6.3% in group III vs 3.1% in group I and 2.9% in group II). Second, elective operation for patients with asymptomatic CHDs (eg, isolated atrial septal defect, ventricular septal defect, patent atrial duct) was found to be curtailed in group III. No significant differences were found among the 3 surgical groups concerning the number of patients requiring the support of extracorporeal membrane oxygenation and the mortality of patients undergoing emergency surgery.
Figure 1.
The scatter plot shows a correlation between decrease in MSI and decrease in surgical volume/outpatient visit volume. A, A positive correlation was found between decrease in surgical volume and decrease in MSI in the municipality where the center is located (r = 0.643, P = .018). B, A positive correlation was found between the decrease in outpatient visit volume and decrease in MSI (r = 0.614, P = .026).
Table 1.
Survey for pediatric cardiovascular surgery program from January 23 to April 8 in 2018, 2019, and 2020
| Group I (2018) | Group II (2019) | Group III (2020) | P value | |
|---|---|---|---|---|
| Outpatient cases (median, IQR) | 19,398 | 19,620 | 4740 | / |
| Internet access times (THS, IQR) | 26 (6-41) | 24 (7-51) | 55 (17-67) | .004 |
| Total operation cases | 2076 | 2292 | 569 | / |
| Emergency surgery (%) | 65 (3.1%) | 66 (2.9%) | 36 (6.3%) | .000 |
| Total anomalous pulmonary vein connection | 14 (0.68%) | 17 (0.74%) | 5 (0.88%) | .876 |
| Pulmonary atresia | 14 (0.68%) | 10 (0.44%) | 6 (1.05%) | .207 |
| Interrupted aortic arch | 3 (0.14%) | 5 (0.22%) | 2 (0.35%) | .608 |
| Transposition of great arteries | 12 (0.58%) | 6 (0.26%) | 5 (0.88%) | .095 |
| Coarctation | 11 (0.53%) | 14 (0.61%) | 9 (1.58%) | .022 |
| Tetralogy of Fallot | 11 (0.53%) | 14 (0.61%) | 9 (1.58%) | .022 |
| Selective surgery (%) | 2009 (96.9%) | 2226 (97.1%) | 533 (93.7%) | .000 |
| ECMO cases of surgery (%) | 16 (0.8%) | 11 (0.5%) | 4 (0.7%) | .463 |
| Mortality (%) | 1 (1.5%) | 2 (3.0%) | 0 (0%) | .535 |
| Emergency | 1 (1.5%) | 2 (3.0%) | 0 (0%) | .535 |
| Elective | 32 (1.6%) | 37 (1.7%) | 8 (1.5%) | .960 |
| No. of transfers (median, IQR) | N/A | 2 (1∼6) | 0 (0∼1) | .004 |
| Baidu Migration Index (median, IQR) | N/A | 319 (156-554) | 138 (54-216) | .004 |
| Blood product volume in hospital (packets, median, IQR) | 794 (458-1365) | 923 (602-1555) | 595 (389-1127) | .032 |
Values are n (%) or median (IQR). IQR, Interquartile range; THS, thousand; ECMO, extracorporeal membrane oxygenation; N/A, not available.
Figure 2.
The change of surgical volume in 2018, 2019, and 2020. The stacked bar chart shows the respective total surgical volume of 13 participating hospitals between January 23 and April 8 in 2018 (N = 2076), 2019 (N = 2292), and 2020 (N = 569), which indicates a substantial decrease in total volume during the COVID-19 era compared with the same period in 2018 and 2019.
Figure 3.
A, The redistribution of case mix in 2018, 2019, and 2020. The diagnosis of surgical cases between January 23 and April 8 in 2018, 2019, and 2020. Areas in green, red, and blue indicate the emergency cases, symptomatic elective cases for which surgery should be performed as early as possible, and asymptomatic elective cases for which surgery can be postponed, respectively. During the COVID-19 pandemic, all of the recruited centers have postponed asymptomatic elective cases. In 2020, emergency cases accounts for 6.3% of the total cases, which is statistically greater than 2.9% in 2019 and 3.1% in 2018 (P < .0001). B, The CHD follow-up program in 2017 (group A), 2018 (group B), and 2019 (group C). The bar chart shows the total number of follow-up in patients with CCHD in 2017, 2018, and 2019 in 3 follow-up forms (traditional follow-up only, internet or phone follow-up only, and follow-up in both forms). There was a significantly higher proportion of patients who only followed up through the internet or phone in group C (26.4% in group C vs 9.6% in group B and 8.9% in group A; P < .0001). The Kaplan–Meier curve showed that there was no significant difference in the cumulative probability of death or unplanned readmission among the 3 groups (P = .52). TAPVC, Total anomalous pulmonary venous connection; IAA, interrupted aortic arch; CoA, aortic coarctation; APW, aortopulmonary window; VSD, ventricular septal defect; AVSD, atrioventricular septal defect; Misc., miscellaneous; ASD, atrial septal defect; PDA, patent ductus arteriosus; FSV, functional single ventricle; PAPVC, partial anomalous pulmonary venous; F/U, follow-up.
During the COVID-19 pandemic, there was a substantial reduction in the total number of outpatient visits (Table 1). The median number of transshipments received by the centers from other hospitals was 0 to 1, significantly lower than in 2019 (P = .004) (Table 1). Furthermore, the Baidu MSI of 13 hospital cities was 138 (IQR, 54-216), significantly lower than the same period in 2019 (319 [IQR, 156-554], P = .004). The median number of blood products received by 13 hospitals from the city central blood station was 595 packets (IQR, 389-1127), significantly lower than in the same period in 2018 and 2019 (P = .032). Data from the Good-doctor website showed a median of 55,000 (IQR, 17,000-67,000) online access times during the COVID-19 pandemic, which was significantly higher than in the same periods in 2018 and 2019 (P = .004).
Of the 1475 patients in follow-up group, 44 (3%) were lost to follow-up, including 11 cases in group A, 13 cases in group B, and 20 cases in group C. There was no significant difference in age, weight, and primary diagnosis among the 3 groups (Table 2 ). Patients in group C had a higher proportion of palliative operations than patients in groups A and B (P = .019). The median duration of follow-up time in group C was 155 days (IQR, 110-180). There was a higher proportion of online or telephone follow-up in group C than in groups A and B. There was no difference in cumulative probability of death or unplanned readmission during the first 180 days among the 3 groups (P = .52) (Figure 3, B). The scores of anxiety index of the patients' parents in group C were 3.5 times higher than in groups A and B. The patients' parents from group C had the highest frequency to use phone or internet for follow-up (Table 3).
Table 2.
Baseline characteristics of follow-up cohort
| Group A (n = 403) | Group B (n = 438) | Group C (n = 590) | P value | |
|---|---|---|---|---|
| Age (d) (median, IQR) | 204 (69-541) | 196 (90-649) | 191 (67-557) | .203 |
| Male (%) | 28.7% | 32.7% | 38.6% | .061 |
| Weight, kg (median, IQR) | 7 (4.7-10) | 7 (4.9-11) | 6.8 (4.4-10) | .061 |
| Primary diagnosis | ||||
| Tetralogy of Fallot | 119 (29.5%) | 136 (31.1%) | 165 (28.0%) | .559 |
| Total anomalous pulmonary vein drainage | 53 (13.2%) | 66 (15.1%) | 59 (11.2%) | .184 |
| Coarctation/VSD | 54 (13.4%) | 55 (12.6%) | 100 (16.9%) | .103 |
| Double outlet right ventricle | 43 (10.7%) | 38 (8.7%) | 54 (9.2%) | .586 |
| Pulmonary atresia | 32 (7.9%) | 33 (7.5%) | 77 (13.1%) | .004 |
| Transposition of great arteries | 25 (6.2%) | 27 (6.2%) | 38 (6.4%) | .980 |
| Single ventricle | 18 (4.5%) | 20 (4.6%) | 26 (4.4%) | .993 |
| Atrioventricular septal defect | 35 (8.7%) | 30 (6.8%) | 31 (5.3%) | .104 |
| Interrupted aortic arch | 11 (2.7%) | 9 (2.1%) | 13 (2.2%) | .790 |
| Miscellaneous | 13 (3.2%) | 24 (5.5%) | 20 (3.4%) | .156 |
| Operation type | ||||
| Biventricular repair | 353 (87.6%) | 385 (87.9%) | 498 (84.4%) | .191 |
| Palliative operation | 34 (8.4%) | 37 (8.8%) | 77 (13.1%) | .019 |
| Sing ventricle repair | 16 (4.0%) | 16 (3.3%) | 15 (2.4%) | .405 |
Values are n (%) or median (IQR). IQR, Interquartile range; VSD, ventricular septal defect.
Table 3.
Outcomes of the follow-up population after complex congenital heart disease surgery among the 3 groups
| Group A (n = 403) | Group B (n = 438) | Group C (n = 590) | P value | |
|---|---|---|---|---|
| Death | 8 (2.0%) | 7 (1.60%) | 5 (0.8%) | .296 |
| Unplanned readmission | 67 (16.6%) | 68 (15.5%) | 74 (12.6%) | .163 |
| GAD-7 | .000 | |||
| 0-4 | 164 (41.6%) | 168 (39.0%) | 208 (35.6%) | |
| 5-9 (mild) | 171 (43.4%) | 173 (40.1%) | 210 (35.9%) | |
| 10-14 (moderate anxiety) | 37 (9.4%) | 55 (12.8%) | 113 (19.3%) | |
| 15-21 (severe anxiety) | 22 (5.6%) | 35 (8.1%) | 54 (9.2%) | |
| Follow-up forms | .000 | |||
| Traditional follow-up only | 92 (22.8%) | 83 (18.9%) | 61 (10.3%) | |
| Internet or phone follow-up only | 36 (8.9%) | 42 (9.6%) | 156 (26.4%) | |
| Follow-up in both forms | 275 (68.2%) | 313 (71.5%) | 373 (63.2%) | |
| Satisfactory of follow-up via internet or phone | .091 | |||
| Unsatisfied | 8 (2.6%) | 19 (5.4%) | 26 (4.9%) | |
| Satisfied | 231 (74.3%) | 234 (68.5%) | 349 (66.0%) | |
| Very satisfied | 72 (23.2%) | 93 (26.2%) | 154 (29.1%) |
Values are n (%) or median (IQR). The GAD-7 score is calculated by assigning scores of 0, 1, 2, and 3, to the response categories of not at all, several days, more than half the days, and nearly every day, respectively. Scores of 5, 10, and 15 represent cut points for mild, moderate, and severe anxiety, respectively. GAD-7, Generalized Anxiety Disorder-7.
Discussion
To our best knowledge, this is the first nationwide multicenter study to investigate the impact of COVID-19 on pediatric congenital heart programs (Figure 4). Our main findings include that (1) COVID-19 has greatly affected the perioperative care for patients with CHD, including a substantial number of case delays and limited access to routine follow-up hospital visits; and (2) tele- and network follow-up might be an effective alternative to the conventional hospital visit in terms of potentially mitigating the risk of postrepair adverse outcomes.
Figure 4.
This retrospective study includes 13 children's hospitals and aims to investigate the impact of the early COVID-19 outbreak on the CHD surgery program in China. The main findings of this study are that the COVID-19 pandemic has resulted in a substantial decrease in total surgical volume and that a redistribution of the case mix and online follow-up care strategy appears to be effective during the COVID-19 era. Our results provide a platform for further study of better serving patients with CHD in terms of patient triage, tiered precautions, and optimizing allocation of resources during the COVID-19 era.
According to the recent report from the National Health Commission, the numbers of diagnosis and treatment offered by the tertiary center in China were dramatically decreased by 51% during the COVID-19 era.19 Correspondingly, there was also a substantial decrease in pediatric congenital heart surgery compared with the same period in 2018 and 2019. Further, as a proportion of total surgical volume, there was a relative increase in emergency operations. Such change in case mix may largely ascribe to the strict restriction placed on each enrolled hospital that elective operation for patients with asymptomatic simple CHDs was not allowed during the COVID-19 era. Further subdivided by the disease category, a significant difference can be found only in those with coarctation of aorta and tetralogy of Fallot. However, there was a trend for a higher percentage of patients in the other categories, and failure to find statistical differences may be partly due to the relatively low prevalence of these diseases. Notably, given the regionalization of congenital heart surgery services in China, where there is a growing CHD population with limited specialist resources, the majority of patients with CHD moved from other cities or rural areas to undergo surgical repair in a few tertiary centers.20 During the COVID-19 era, such patient transfer was greatly restricted by the travel ban, explaining the decrease in surgeries, even in emergency cases. Additionally, parents' reluctance to seek care during this pandemic and the 14-day preadmission quarantine before surgery are other potential factors in such a decrease. Chinese government has implemented aggressive actions13 , 21 to control the spread of COVID-19, including strict control of entering or leaving from cities and rural areas, and reducing/shutting down the city public transportation and inter-city airline or high-speed railways. The decrease in emergency surgery raises substantial concerns. Critical CHDs (eg, duct-dependent CCHDs) usually constitute a large proportion of the emergency cases in which dramatic changes after birth may lead to rapid hemodynamic compromise and preoperative attrition. From the standpoint of clinical practice, there is only a narrow temporal window for these patients, and timely lifesaving surgical intervention is definitely required. Lack of surgical care in early life potentially poses a big threat to this patient population.
Guidelines related to adult patients undergoing cardiac surgery22 or heart transplant23 in the context of the current pandemic have been published. These statements have recommended deferral of elective surgery during the COVID-19 era. Recent Taskforce and Society guidance statements24 have also stressed the necessity of deferring elective surgeries in efforts to control the spread of COVID-19 and preserve or redirect limited resources and personnel for the treatment of patients infected by COVID-19. Although there was an expected decrease in elective surgery in this cohort, some may still argue that maintaining elective surgery is not appropriate given that the potential harm in terms of COVID-19 transmission would seem extremely high and clearly unjustified when compared with the benign prognosis associated with deferring elective pediatric cardiac operations. First, we should clarify that surgery for patients with asymptomatic simple CHDs was heavily restricted. The elective cases in this study include some patients with tetralogy of Fallot or coarctation of aorta who presented with relatively stable clinical manifestations and infantile patients with large ventricular septal defects or complete atrioventricular septal defects who had signs of impaired heart function, a history of recurrent repertory infection, and failure to thrive. Postponing surgery in these patients might result in a cyanotic spell and severe heart failure during the waiting time, potentially increasing the perioperative mortality. The implications of deferred cardiac surgical operations remain unknown,25 and comprehensive as well as careful risk-benefit evaluation should be made instead of making decisions solely on the basis of COVID-associated risks.26 The policymakers should not prioritize needs to maximize the number of patients' care at the cost of disregarding care for vulnerable individuals.27 On the other hand, we recognize that the significance of the potential damage of COVID-19 in patients undergoing cardiac surgery cannot be underestimated. Because of the lack of availability of nucleic acid testing during the early COVID-19 outbreak, every elective case and their parents must be observed for 2 weeks before surgery given the rationale that incubation period of COVID-19 is generally within 14 days after exposure.
According to the results, resource scarcities and the phenomenon of medical system breakdown were less common. For instance, resources in cardiac intensive care unit and the extracorporeal membrane oxygenation facilities were not allocated to those infected cases in the majority of the recruited hospitals. Only a small number of doctors/nurses were assigned to assist in the care management of patients infected by COVID-19, which is in line with a recent report that a small fraction of pediatric cardiologists from 56 US centers are reassigned to provide clinical services outside their scope of practice.6 There may be several explanations. First, the study period can be considered as an early phase in which resources were relatively plentiful compared with the peak phase,28 and the majority of the hospitals were not at the epicenter. Second, pediatric patients constitute a small portion of cases infected by COVID-19 compared with adult patients.29 Thus, there was a lower burden of hospitalized patients with COVID-19 in children's hospitals. However, these results should be interpreted with caution because as this pandemic continues to a peak time, postponing elective surgery after careful patient triage should undoubtedly be advocated in efforts to preserve scarce resources. Of note, although there was a substantial decrease in blood donation during the COVID-19 era, it did not appear to be a main reason for the decrease in surgical volume given the liberal use of priming without blood and blood salvage in congenital heart surgery.30
Preoperative and postoperative nucleic acid testing are both important because a recent case report found that COVID-19 infection was confirmed on postoperative day 13 in a patient undergoing the Fontan operation. There was a lack of testing kits in the early period of COVID-19 outbreak, and it was not until April 24, 2020, that nucleic acid testing was uniformly performed in China.31 Thus, the majority of the patients in this cohort did not undergo regular preoperative and postoperative testing. Although we used strict methods to control the spread of COVID-19 in patients undergoing congenital heart surgery in this series, we cannot rule out the possibility that there may be asymptomatic carriers because preoperative nucleic acid testing for COVID-19 was not routinely performed in patients and their parents. We recognize the significance of the potential damage of COVID-19 in patients undergoing cardiac surgery; however, as mentioned, the balance between postponing or curtailing surgery and potentially putting the vulnerable individuals at risk of deterioration of some specific CHDs requires a second ethical consideration. There was still a high overall surgical volume performed during the COVID-19 era in this series. There are several potential rationales and reasons for our relatively aggressive attitude toward performing surgery for those who may have a high risk of mortality and morbidity during the waiting time. First, the Chinese government has taken strict, far-reaching antiepidemic actions, particularly in Wuhan, which was the first outbreak area in China, which may effectively help to control the transmission of the disease. Second, given the rationale that the incubation period of COVID-19 is generally within 14 days after exposure, we strictly required an observation for 2 weeks (including both patients and their parents) before surgery. As for some emergency cases, operations must be performed in COVID-19–designated operating rooms (eg, negative pressure operation room) plus personal protective equipment. Such strict institutional protocols may be helpful to control the spread of COVID-19. Third, the study has shown that pediatric patients constitute a relatively small portion of cases infected by COVID-19 and usually have less severe clinical manifestations. A recent study32 from a Boston group indicated that the differences in expression of angiotensin-converting enzyme 2 or transmembrane serine protease 2 between younger and adult patients may potentially result in less vulnerability to the COVID-19 infection in pediatric patients. Although preoperative testing for COVID-19 is currently mandatory in the majority of countries, it should be acknowledged that the availability of testing and its implementation are still not uniform around the world. In this sense, our experience may be of potential value. Finally, we should clarify that since April 24, 2020, we have changed our protocol by performing nucleic acid tests, instead of 14-day quarantine, in all pediatric patients undergoing surgery and their parents.
Orchestrated follow-up mechanism is crucial to the patients undergoing complex congenital heart surgery.33 In this study, the aforementioned traffic control, social distancing policy, and parents' anxiety about being infected by COVID-19 were associated with a dramatic decrease in postoperative clinic visits. However, there is no increase in mortality or unplanned rehospitalization during the follow-up period compared with the rate in the previous 2 years. Our data indicate an increasing interaction between parents and CHD specialists via tele- and network follow-up visits. During the outbreak of COVID-19, the government has promoted the establishment of virtual hospitals, advocating tertiary hospitals to provide medical services via network and advocate dispensing by express delivery.34 Meanwhile, some private third-party network platforms (eg, Haodaifu network) have provided point-to-point healthcare services between doctors and patients. Such liberal use of the tele- and network follow-up visits is helpful to provide better postrepair care for patients with CHD and partially explain why there is no difference regarding mortality or rehospitalization during this pandemic. Our finding is also in line with the guideline statement22 that other types of follow-up visit are required to help reduce the undue risk for hospital-acquired transmission. However, conventional hospital visits are still required in a portion of patients with CHD because they may need computed tomography angiography or invasive catheterization evaluation. The duration of the follow-up period in this study was relatively short. There is the possibility that the lack of hospital visits may be related to an increase in mortality and rehospitalization during the longer follow-up if the medical service cannot return to normal. Thus, innovative methods, including wearable monitor devices designed for children and telemedicine between specialized hospitals and local clinics may become a main follow-up strategy post–COVID-19 era.
Study Limitations
First, data regarding the number of neonates born with CHD during the study period cannot be obtained, so detailed information regarding neonatal patients who died because of a lack of health care was not available. It is possible that lack of access to timely surgical intervention in some neonates with critical CHDs may result in increased mortality. Second, we lack information about the patients who potentially require surgical interventions during the COVID-19 era so that the association between their parent's psychologic factors and the decrease in surgical volumes cannot be identified. Third, we only follow up the patients via telephone or social media apps during the COVID-19 era, so we cannot definitely verify the death or unplanned readmission in group C. Fourth, the Shanghai Children's Medical Center and Beijing Children's Hospital were both national children's medical centers, so there were more patients coming from other areas to seek treatments for CHD in these 2 hospitals. There may be variations in institutional management care (eg, surgical experiences, postrepair intensive care), which may bias the results. Fifth, further study is required to obtain more robust data (eg, travel distance, data directly reflecting the status of traffic restriction) to help confirm the hypothesis that travel restrictions are a main barrier to CHD care during the early outbreak of COVID-19 in China. Finally, except for Wuhan Children's Hospital, all of the patients and members of the healthcare provider team outside the epicenter in this cohort did not undertake nucleic acid testing during the early outbreak of COVID-19 pandemic, so we cannot rule out the possibility that there may be asymptomatic carriers.
Conclusions
Although resource scarcities and the phenomenon of medical system breakdown were less common in children's hospitals during the COVID-19 era, there was a substantial decrease in both elective and emergency operations. The unprecedented measures taken by the governments, including traffic restrictions, bring a challenge to the regionalization of congenital heart surgery service. The online follow-up surveillance appears to be effective during such a public health crisis. Our study provides some valuable information regarding the impact of the ongoing COVID-19 pandemic on crisis management for CHD, highlighting the importance and challenge of serving this subgroup patient under a public health crisis.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Acknowledgments
The authors thank Drs Xiao, Huang, St Louis, Ming, Huang, Liu, Zhao, Tian, Chen, Guo, Tang, and Chen, nurse Chen, and the social workers who contributed to this study.
This study recruited the major children's hospitals in the National Association of Pediatric Cardiology and Cardiac Surgery in China, including Shanghai Children's Medical Center, Hunan Children's Hospital, Jiangxi Children's Hospital, Wuhan Children's Hospital, Shanxi Children's Hospital, Yuying Children's Hospital, The Second Hospital affiliated to Harbin Medical University, Hainan Women and Children Medical Center, Xi'an Children's Hospital, Yan'an Hospital, Guangzhou Woman and Children's Hospital, Beijing Children's Hospital, National Center for Children Health, Beijing, China, and Shenzhen Children's Hospital.
Footnotes
Collaborators: Dongyu Xiao, MD,g Guojin Huang, MD,h Teng Ming, MD,h Peng Huang, MD,g Caixia Liu, MD,i Qifeng Zhao, MD,j Hai Tian, MD,k Renwei Chen, MD,l Jianjun Guo, MD,m Jian Tang, MD,n WeinMin Chen, BS,a and Huiwen Chen, MD, PhDa,b
G.S. and J.H. contributed equally to the study.
Funding: Sanming Project of Medicine in Shenzhen (SZSM201612003 to Y.D. and H.Z.), National Science Fund for Distinguished Young Scholars (81525002 to H.Z.), and Program for Shanghai Outstanding Medical Academic Leader (2019LJ22 to H.Z.).
Contributor Information
National Association of Pediatric Cardiology and Cardiac Surgery Working Group:
Dongyu Xiao, Guojin Huang, Teng Ming, Peng Huang, Caixia Liu, Qifeng Zhao, Hai Tian, Renwei Chen, Jianjun Guo, Jian Tang, WeinMin Chen, and Huiwen Chen
Appendix E1
Table E1.
Questionnaire for all the parents or guardian with children who survived after complex congenital heart surgery
|
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 50. Available at: https://apps.who.int/iris/handle/10665/331450. Accessed March 10, 2020.
- 2.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossano J.W. Congenital heart disease: a global public health concern. Lancet Child Adolesc Health. 2020;4:168–169. doi: 10.1016/S2352-4642(19)30429-8. [DOI] [PubMed] [Google Scholar]
- 4.Desmond C., Watt K., Saha A., Huang J., Lu C. Prevalence and number of children living in institutional care: global, regional, and country estimates. Lancet Child Adolesc Health. 2020;4:370–377. doi: 10.1016/S2352-4642(20)30022-5. [DOI] [PubMed] [Google Scholar]
- 5.Stephens E.H., Dearani J.A., Guleserian K.J., Overman D.M., Tweddell J.S., Backer C.L., et al. COVID-19: crisis management in congenital heart surgery. Ann Thorac Surg. 2020;160:522–528. doi: 10.1016/j.jtcvs.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S., et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raissadati A., Haukka J., Pätilä T., Nieminen H., Jokinen E. Chronic disease burden after congenital heart surgery: a 47-year population-based study with 99% follow-up. J Am Heart Assoc. 2020;9:e015354. doi: 10.1161/JAHA.119.015354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morray B.H., Gordon B.M., Crystal M.A., Goldstein B.H., Qureshi A.M., Torres A.J., et al. Resource allocation and decision making for pediatric and congenital cardiac catheterization during the novel coronavirus SARS-CoV-2 (COVID-19) pandemic: a U.S. multi-institutional perspective. J Invasive Cardiol. 2020;32:E103–E109. doi: 10.25270/jic/20.00189. [DOI] [PubMed] [Google Scholar]
- 9.Haft J.W., Atluri P., Alawadi G., Engelman D., Grant M.C., Hassan A., et al. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg. 2020;110:697–700. doi: 10.1016/j.athoracsur.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Backer C.L., Pasquali S.K., Dearani J.A. Improving national outcomes in congenital heart surgery: the time has come for regionalization of care. Circulation. 2020;141:943–945. doi: 10.1161/CIRCULATIONAHA.119.045542. [DOI] [PubMed] [Google Scholar]
- 11.Welke K.F., Pasquali S.K., Lin P., Backer C.L., Overman D.M., Romano J.C., et al. Regionalization of congenital heart surgery in the United States. Semin Thorac Cardiovasc Surg. 2020;32:128–137. doi: 10.1053/j.semtcvs.2019.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Wuhan Municipal Health Commission. http://wjw.wuhan.gov.cn/front/web/showDetail/2020011109036 Available at:
- 13.Kraemer M.U.G., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Z., Huang S., Lu W., Su Z., Yin X., Liang H., et al. Modeling the trend of coronavirus disease 2019 and restoration of operational capability of metropolitan medical service in China: a machine learning and mathematical model-based analysis. Glob Health Res Policy. 2020;5:20. doi: 10.1186/s41256-020-00145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.A brief introduction of Good-doctor platform. https://www.haodf.com/info/aboutus.php Available at:
- 16.Zhu T., He D., Zhan J., Chen Y., Yang X., Duan X., et al. Consensus on pediatric surgery during the COVID-19 pandemic. Chin J Pediatr Surg. 2020;41:289–292. [Google Scholar]
- 17.Mou X., Dong N. National consensus on perioperative management with congenital heart disease in children infected with 2019-novel coronavirus. Chin J Pediatr Surg. 2020;41 E003-E003. [Google Scholar]
- 18.Xiang L., Su Z., Liu Y., Zhang X., Li S., Hu S., et al. Effect of family socioeconomic status on the prognosis of complex congenital heart disease in children: an observational cohort study from China. Lancet Child Adolesc Health. 2018;2:430–439. doi: 10.1016/S2352-4642(18)30100-7. [DOI] [PubMed] [Google Scholar]
- 19.Report of the National Medical Service during February 2020. http://med.china.com.cn/content/pid/171991/tid/1022 Available at:
- 20.He Y., Xu W., Su Z., Liu K., Zhang H. Addressing the rising burden of congenital heart disease in China. Lancet Child Adolesc Health. 2020;4:e7. doi: 10.1016/S2352-4642(20)30061-4. [DOI] [PubMed] [Google Scholar]
- 21.Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S., et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hassan A., Arora R.C., Adams C., Bouchard D., Cook R., Gunning D., et al. Cardiac surgery in Canada during the COVID-19 pandemic: a guidance statement from the Canadian Society of Cardiac Surgeons. Can J Cardiol. 2020;36:952–955. doi: 10.1016/j.cjca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeFilippis E.M., Farr M.A., Givertz M.M. Challenges in heart transplantation in the era of COVID-19. Circulation. 2020;141:2048–2051. doi: 10.1161/CIRCULATIONAHA.120.047096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haft J.W., Atluri P., Ailawadi G., Engelman D.T., Grant M.C., Hassan A., et al. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. J Thorac Cardiovasc Surg. 2020;160:452–455. doi: 10.1016/j.jtcvs.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ad N., Luc J.G.Y., Nguyen T.C., Arora R.C., Balkhy H.H., Bender E.M., et al. Cardiac surgery in North America and coronavirus disease 2019 (COVID-19): regional variability in burden and impact. J Thorac Cardiovasc Surg. 2020 doi: 10.1016/j.jtcvs.2020.06.077. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drake D., Morrow C.D., Kinlaw K., De Bonis M., Zangrillo A., Sade R.M., Cardiothoracic Ethics Forum Cardiothoracic surgeons in pandemics: ethical considerations. Ann Thorac Surg. 2020;110:355–358. doi: 10.1016/j.athoracsur.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George I., Salna M., Kobsa S., Deroo S., Kriegel J., Blitzer D., et al. The rapid transformation of cardiac surgery practice in the coronavirus disease 2019 (COVID-19) pandemic: insights and clinical strategies from a center at the epicenter. J Thorac Cardiovasc Surg. 2020;160:937–947. doi: 10.1016/j.jtcvs.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Tong S. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;45 doi: 10.1542/peds.2020-0702. e20200702. [DOI] [PubMed] [Google Scholar]
- 30.Goel R., Cushing M.M., Tobian A.A. Pediatric patient blood management programs: not just transfusing little adults. Transfus Med Rev. 2016;30:235–241. doi: 10.1016/j.tmrv.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Chinese government requires the performance of nucleic acid test in a large scale. https://xw.qq.com/cmsid/20200423A0M0VV00 Available at:
- 32.Ziegler C.G.K., Allon S.J., Nyquist S.K., Mbano I.M., Miao V.N., Tzouanas C.N., et al. SARS-CoV-2 receptor ACE2 ss an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181:1016–1035. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gaydos S.S., Chowdhury S.M., Judd R.N., McHugh K.E. A transition clinic intervention to improve follow-up rates in adolescents and young adults with congenital heart disease. Cardiol Young. 2020;30:633–640. doi: 10.1017/S1047951120000682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Utilization of internet consultation in healthcare during the COVID-19 era. http://www.nhc.gov.cn/xcs/zhengcwj/202002/ec5e345814e744398c2adef17b657fb8.shtml Available at: