Abstract
Background: Insomnia is highly prevalent in patients with substance use disorders (SUD), and it has been related to a worse course of addiction. Insomnia during detoxification in a hospital has not been adequately studied. This study aims to compare sociodemographic, clinical, and psychopathological characteristics of SUD patients undergoing a detoxification program, by comorbidity and insomnia symptoms.
Methodology: We recruited 481 patients who received pharmacological and psychotherapeutic treatment for detoxification. They were evaluated through semi-structured interviews, standardized questionnaires, and a specific sleep log. A bivariate and multivariate analysis of the data was performed.
Results: Insomnia was reported by 66.5% patients, with sleep-maintenance insomnia the most frequent issue, followed by early morning awakening and sleep-onset insomnia. Patients with alcohol use disorder and cannabis use disorder had higher prevalence of sleep-onset insomnia. Patients with cocaine and heroin use disorder had higher prevalence of sleep-maintenance insomnia. Independent factors that allowed the identification of insomnia symptoms included being female (OR: 3.43), polysubstance use (OR: 2.85), comorbid anxiety disorder (OR: 2.02), and prior admission for detoxification (OR: 1.22).
Conclusions: Insomnia symptoms are very prevalent in patients admitted for detoxification. The diagnosis and therapeutic strategies for the insomnia symptoms should be improved, especially in women and in patients with greater addiction severity and with anxiety disorders.
Keywords: addiction, insomnia, sleep disorders, women, detoxification process, anxiety disorders
Introduction
Insomnia has been defined as a sleep disorder characterized by difficulty with sleep initiation, duration, consolidation, or quality that occurs despite circumstances favorable for sleeping. In addition, there could be daytime impairment symptoms, including fatigue, sleepiness, mood disturbances, physical symptoms and concerns about or dissatisfaction with sleep (1).
Insomnia is estimated to affect between 20 and 35% of the general population (2–6) and 40–90% of patients with psychiatric disorders other than addictions (7–10). Individuals with substance use disorders (SUD) also have a higher prevalence of insomnia than the general population (11, 12). The relationship is bidirectional; people with insomnia are also more prone to SUD (13–15). Insomnia is suffered by between 30 and 85% of SUD patients, depending on the primary substance of abuse and other methodological factors (16–19). Alcohol use disorder is the problem most studied regarding insomnia symptoms, and the rates described for those patients are between 30 and 60% (20–22). Sleep in this population is influenced by numerous substance use-related factors, such as type and amount of drug used, duration of addiction, route of administration, state of intoxication or withdrawal, and simultaneous consumption of stimulants and depressants.
In the general population, insomnia is more likely to affect women, people over 65 years old, and shift and night workers (23–25). Likewise, patients with medical and psychiatric comorbidities are more susceptible to nocturnal sleep disturbances (4, 7).
Insomnia has been linked to a worsening of addiction (26, 27); however, few studies have analyzed risk factors for insomnia in patients with SUD. It has been identified that comorbid anxiety disorder, medical comorbidities, and early onset of dependence increase the risk of insomnia during active substance use (28).
Detoxification is frequently required among SUD patients, who could be done in an outpatient or hospital setting. The detoxification process is a critical time to evaluate and propose therapeutic approaches, including insomnia symptoms. It has been found that symptoms of insomnia during a detoxification process are a risk factor to early relapses (26). To our knowledge, however, risk factors of insomnia symptoms during detoxification process have not been described. Therefore, this study aimed to compare sociodemographic, clinical, and psychopathological characteristics of SUD patients undergoing a detoxification program according to the presence/absence of insomnia symptoms. It was hypothesized that symptoms of insomnia would be common in this population and that patients with insomnia symptoms would have higher rates of psychiatric comorbidity and more severe addiction.
Methods and Materials
Participants
In this study 481 SUD inpatients participated in the detoxification unit of Vall d'Hebron University Hospital in Barcelona, Spain. The recruitment period was from June 2013 to May 2018.
The inclusion criteria were substance dependence (excluding primary abuse of caffeine or nicotine) in the past year according to DSM criteria, active consumption up to the day before admission to the detoxification unit, and provision of signed informed consent to participate in the study. The exclusion criteria were failure to complete the detoxification program and presence of a major language barrier or severe cognitive impairment. The study was approved by the Vall d'Hebron Hospital ethics committee, according to the (29).
Procedure
Patients received appropriate detoxification treatment for their SUD. The treatment in all cases consisted of pharmacologic and psychological interventions to treat SUD (detoxification) and psychiatry comorbidity. They received decreasing doses of benzodiazepines (regardless of the substance that led to admission) and adjuvant medications to treat comorbid psychiatric symptoms. Patients participated in group psychotherapy during the detoxification program, which consisted of three sessions including psychoeducation, a motivation interview, and prevention of substance addiction relapse. Hospital stays ranged between 10 and 15 days (10.9 ± 3.2).
The assessment process consisted of an evaluation of insomnia symptoms conducted by daily interviews with a psychiatrist and through information from sleep logs kept by night-shift nurses. In addition, three interviews conducted by psychologists following the protocol to evaluate comorbidity were done.
Study Variables and Instruments
The variables recorded were insomnia symptoms, sociodemographics, substance consumption variables, and medical and psychiatric comorbidities.
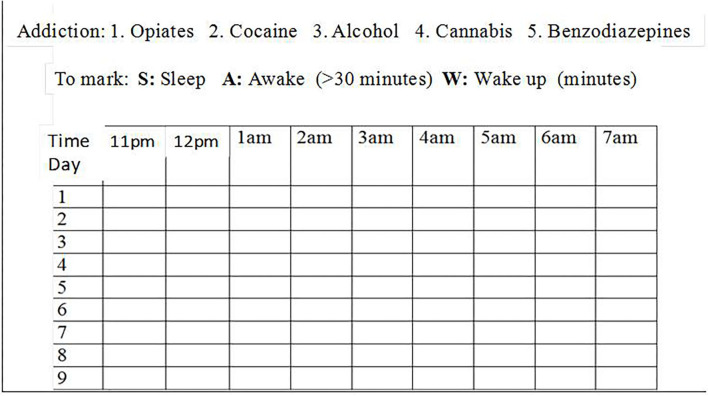
The presence of symptoms of insomnia was evaluated by the psychiatrist according to clinical criteria, based on daily interviews and complementary information from a sleep log. The sleep log is a tool where the night-shift nurses recorded how each patient slept for each hour between 11 p.m. and 7 a.m. was considered in order to diagnose insomnia symptoms (Figure 1). A distinction was made between the following types of insomnia: sleep-onset insomnia (failure to fall asleep within the first half hour of going to bed), sleep-maintenance insomnia (two or more awakenings a night), early awakening (awakening at least 1 h before the usual time), poor sleep quality (none of the above but presence of diurnal effects, such as daytime sleepiness, fatigue, irritability, nervousness, decreased concentration, muscle tension, and headache).
Figure 1.
Nighttime sleep log. S, sleep; A, awake (>30 min); W, wake up (minutes).
Patients who were diagnosed with insomnia symptoms were prescribed specific treatment according to their profile and the judgment of the clinicians responsible for their care.
Psychiatric comorbidity was evaluated using semi-structural diagnostic interviews. SCID-I (Structured Clinical Interview for the DSM-IV Axis I Disorders), SCID-II (Structured Clinical Interview for the DSM-IV Axis II Disorders), and CAADID (Conners' Adult ADHD Diagnostic Interview for DSM-IV) were used to diagnose attention deficit hyperactivity disorder (ADHD). Urinalysis and alcohol breath test results were used to evaluate substance consumption at the first day of the detoxification process.
Statistical Analysis
First of all, the main variables of the sample were analyzed using descriptive statistics (mean, standard deviation, and frequency tables) and bivariate analyses. Later, in order to conduct comparisons, the sample was divided into two groups (patients with insomnia symptoms vs. patients without insomnia symptoms). The chi-square test was used to compare categorical variables between these groups, while Student's t-test was used to compare continuous variables. Afterward, to reduce false positive results, a Bonferroni correction for multiple tests was applied according to the number of tests in each bivariate analysis. Variables that retained statistical significance after Bonferroni correction were included in the multivariate analysis. Finally, logistic regression, with the enter method, was used to identify the independent effect of the variables of the insomnia symptoms (present of insomnia = 1). Data were entered and analyzed in SPSS version 18.0. In all cases, statistical significance was set at p < 0.05.
Results
Description of the Sample
A total of 552 patients were admitted to the detoxification unit during the study period. Fifty patients requested voluntary discharge before completion of the program, and 21 were not included because of language barriers or severe cognitive impairment. Hence, the final sample consisted of 481 patients.
Table 1 summarizes the sociodemographic, clinical, and treatment characteristics of the sample. The most common primary substance of use was alcohol (42.4%), followed by cocaine (32.8%), opiates (12.9%), cannabis (7.1%), and benzodiazepines (4.8%). Polysubstance dependence (three substance use disorders within the past 12 months) was reported for 46.4% patients. Polysubstance dependence (three substance use disorders within the past 12 months) was reported for 46.4% patients. The distribution of substance consumption across the lifespan of the polysubstance dependent patients was 85.8% cocaine, 77.7% alcohol, 75.2% cannabis, 56.7% opioids, and 54.1% benzodiazepines.
Table 1.
Description of study participants.
| Sociodemographic variables | Total (n = 481) | Total (n = 481) | |
|---|---|---|---|
| Age (years) | 40.9 ± 10.3 | Employed (working) | 16.2% |
| Gender (male) | 72.3% | Marital status (married) | 33.1% |
| Nationality (foreign) | 9.8% | Living with someone | 34.1% |
| Education (primary education) | 66.7% | Criminal record (prison) | 20.6% |
| Clinical variables related to comorbidities | |||
| Medical history | 60.7% | Axis II disorders | 44.7% |
| Psychiatric history | 62.2% | Cluster B | 28.7% |
| Axis I disorders | 43.7% | Other personality disorder | 9.3% |
| Anxiety disorder | 15.6% | Cluster C | 4.8% |
| Depressive disorder | 14.1% | Cluster A | 1.9% |
| Attention deficit hyperactivity disorder | 13.1% | ||
| Psychotic disorder | 8.5% | Prior psychiatric admissions | 15.6% |
| Bipolar disorder | 3.1% | ||
| Clinical variables related to consumption | |||
| Age at start of consumption | 17.8 ± 6.4 | Polysubstance users | 46.4% |
| Age at onset of substance use disorder | 24.1 ± 8.2 | Binge consumption prior to admission | 55.3% |
| Years of addiction | 16.6 ± 11.3 | Positive breath alcohol test on admission | 25.2% |
| Main Substance Use Disorder | Positive urinalysis on admission | 55.9% | |
| Alcohol | 42.4% | Prior detoxification admissions | 52% |
| Cocaine | 32.8% | ||
| Heroine | 12.9% | ||
| Cannabis | 7.1% | ||
| Benzodiazepines | 4.8% | ||
| Psychopharmacological and Psychological treatment | |||
| Antiepileptic | 69% | ADHD drugs | 4.7% |
| Antidepressant | 60.1% | Opioid agonists | 12.9% |
| Antipsychotic | 44.9% | Disulfiram/Namelfeno | 20.8% |
| Benzodiazepines | 6.9% | Group Psychotherapy | 81.1% |
| Insomnia symptoms | |||
| No insomnia symptoms during detoxification process | 33.5% | Type of insomnia | |
| Sleep-maintenance insomnia | 45.1% | ||
| Early morning awakening | 25.4% | ||
| Insomnia symptoms during detoxification process | 66.5% | Sleep-onset insomnia | 16.4% |
| Poor quality of nocturnal sleep | 12.3% | ||
Insomnia symptoms were reported by 66.5% of patients (n = 320) during the detoxification process and 84.3% reported previous insomnia symptoms. Sleep-maintenance insomnia was the most common type of insomnia overall, followed by early morning awakening, sleep-onset insomnia, and poor quality of nocturnal sleep. At discharge, insomnia symptoms were considered to have been alleviated in 63.8% of patients
On the other hand, the relationship among type of insomnia symptoms and main SUD was analyzed. Patients with alcohol use disorder had higher prevalence of sleep-onset insomnia (44.7 vs. 30.8%, p < 0.02), early awakening (45.4 vs. 33.6%, p < 0.02) and poor sleep quality (44.2 vs. 11.5%, p < 0.001) than other SUD patients. Patients with cocaine use disorder had higher rates of sleep-maintenance insomnia (37.5 vs. 27.2%, p < 0.02) and poor sleep quality (57.7 vs. 31.4%, p < 0.006). Patients with heroin use disorder were more likely to experience sleep-maintenance insomnia (21.2 vs. 6.1%, p < 0.0001). Finally, patients with cannabis use disorder had higher prevalence of sleep-onset insomnia (14.1 vs. 5.7%, p < 0.008), while patients with benzodiazepine use disorder had higher prevalence of sleep-maintenance insomnia (8.3 vs. 1.9%, p < 0.001) and early awakening (8.2 vs. 3.6%, p < 0.04) than patients with other SUD.
Insomnia Symptoms According to Sociodemographic and Clinical Variables
As is shown in Table 2, insomnia symptoms were more frequently present in women and older individuals. Patients with heroin use disorders had significantly more insomnia symptoms than patients with another substance use disorders. Also, polysubstance users and patients with medical conditions had significantly more insomnia symptoms. When comorbidity psychiatry was compared for insomnia symptoms, that anxiety disorders, ADHD, cluster B personality disorder, and prior admissions for detoxification more were found frequently (see Table 2).
Table 2.
Insomnia symptoms according to sociodemographic and clinical variables during detoxification process.
| Sociodemographic variables | Insomnia symptoms (n = 320) | No insomnia symptoms (n = 161) | p |
|---|---|---|---|
| Age (years) | 44.4 ± 11.8 | 40.2 ± 9.3 | 0.04* |
| Gender (female) | 34.7 | 13.7 | 0.0001*, ** |
| Nationality (foreign) | 9.1 | 11.2 | 0.46 |
| Education (primary education) | 32.5 | 34.8 | 0.62 |
| Employed (working) | 88.3 | 86.6 | 0.52 |
| Marital status (married) | 30.3 | 38.5 | 0.07 |
| Living with someone | 30.6 | 31 | 0.21 |
| Criminal record (prison) | 24.9 | 23.4 | 0.78 |
| Clinical variables related to comorbidities | |||
| Medical history | 64.7 | 52.8 | 0.01* |
| Psychiatric history | 68.1 | 60.3 | 0.10 |
| Axis I | 49.4 | 42.3 | 0.18 |
| Anxiety disorder | 19.4 | 8.1 | 0.001* |
| Psychiatric history | 68.1 | 60.3 | 0.10 |
| Axis I | 49.4 | 42.3 | 0.18 |
| Anxiety disorder | 19.4 | 8.1 | 0.001*, ** |
| Depressive disorder | 19.6 | 16.6 | 0.32 |
| Attention deficit hyperactivity disorder | 15.3 | 8.7 | 0.04* |
| Psychotic disorder | 8.4 | 8.7 | 0.92 |
| Bipolar disorder | 3.8 | 1.9 | 0.26 |
| Axis II | 51.6 | 43.1 | 0.09 |
| Cluster B | 33.1 | 19.9 | 0.002*, ** |
| Other personality disorder | 11.6 | 10.1 | 0.81 |
| Cluster C | 5 | 4.3 | 0.75 |
| Cluster A | 1.9 | 1.9 | 0.99 |
| Prior psychiatric admissions | 26.8 | 20 | 0.09 |
| Clinical variables related to consumption | |||
| Age at start of consumption | 17.9 ± 6.4 | 17.5 ± 6.4 | 0.44 |
| Age of onset of substance use disorder | 24.3 ± 8.04 | 23.8 ± 8.6 | 0.55 |
| Years of addiction | 19.6 ± 10.2 | 18.6 ± 13.0 | 0.87 |
| Main Substance Use Disorder | % | % | |
| Alcohol | 57.8 | 51.6 | 0.40 |
| Cocaine | 31.9 | 34.8 | 0.52 |
| Heroine | 16.6 | 5.6 | 0.001*, ** |
| Cannabis | 6.6 | 8.1 | 0.54 |
| Benzodiazepines | 7.2 | 5.2 | 0.11 |
| Polysubstance users | 56.6 | 26.1 | 0.0001*, ** |
| Prior detoxification admissions | 59.7 | 36.6 | 0.0001*, ** |
| Binge consumption prior to admission | 53.3 | 53.3 | 0.99 |
| Positive breath alcohol test | 23.8 | 28 | 0.32 |
| Positive urinalysis | 61.3 | 55.3 | 0.08 |
| Psychopharmacological and psychological treatment | |||
| Antiepileptic | 71.3 | 82.2 | 0.45 |
| Antidepressant | 59.3 | 76.3 | 0.38 |
| Antipsychotic | 45.3 | 57.2 | 0.21 |
| Benzodiazepines | 6.9 | 6.8 | 0.986 |
| Opioid agonists | 9.3 | 16.3 | 0.08 |
| Interdictors | 17.9 | 23.8 | 0.73 |
p < 0.05;
Statistically significant after Bonferroni correction.
The following variables were included in the logistic regression analysis after Bonferroni correction: gender (female), polysubstance users, anxiety disorder, prior admission for detoxification, admission for heroin detoxification, and cluster B personality disorder. Independent factors that allowed for identification of insomnia symptoms were female, polysubstance use, prior admission for detoxification, and comorbid anxiety disorder. Women were 3.43 times more likely to suffer from insomnia. Patients with a history of polysubstance use were 2.85 times more likely more likely to suffer from insomnia, and patients with anxiety disorders were 2.02 times more likely to suffer from insomnia. Finally, patients with history of prior admission for detoxification were 1.22 times more likely to suffer from insomnia during the detoxification process (see Table 3).
Table 3.
Variables independently associated with insomnia symptoms during detoxification process.
| OR | 95% CI | p | |
|---|---|---|---|
| Gender (female) | 3.43 | 2.01–5.86 | 0.0001 |
| Polysubstance users | 2.85 | 1.79–4.54 | 0.0001 |
| Anxiety disorder comorbidity | 2.09 | 1.06–4.12 | 0.03 |
| Prior admission for detoxification | 1.22 | 1.07–1.38 | 0.002 |
| Admission for heroin detoxification | 1.77 | 0.80–3.94 | 0.16 |
| Cluster B personality disorder | 1.22 | 0.74–2.03 | 0.44 |
Discussion
We detected a high prevalence of insomnia symptoms (66.5%) in the early stages of substance withdrawal in patients admitted to a hospital detoxification unit. This rate is higher than the rates of 20–35% reported for the general population (2–6) and similar to rates described for patients with other psychiatric disorders (7–10, 30–32). In a previous study, we found that 84.3% of addicted patients experienced insomnia symptoms during active consumption of substances (28). It could be hypothesized, that patients actively consuming such substances have less frequent insomnia symptoms because hypersomnia is an expected withdrawal symptom of the stimulant detoxification process.
The prevalence of insomnia symptoms is high, and it ranges from 59.3 to 100%, depending on the primary substance used. These rates are consistent with insomnia prevalence described in other studies on SUD (17–22). Behavioral and psychobiological factors increase the prevalence of insomnia symptoms in SUD patients, for example, bad sleep hygiene and the interaction between the hypocretinergic and dopaminergic systems (13). As for the type of insomnia, sleep-maintenance insomnia was observed in half of the patients and was the most common type of insomnia identified. A similar rate has been reported in other substance-use disorder patients (13).
In the multivariate analysis, the independent risk factors associated with insomnia symptoms were female sex, anxiety disorder comorbidity, polysubstance use and prior admission for detoxification.
We found that women in our study have more insomnia symptoms, just as they do in the general population. According to diverse studies and revisions, insomnia in women might be increased and affected by hormonal changes such as menstruation, pregnancy, breastfeeding, or menopause (23). Another explanation is that women tend to suffer anxiety more frequently, as well as depressive disorders associated with insomnia (23). In the same way, it has been found that anxiety disorders are independently associated with insomnia symptoms in SUD patients. The relationship between insomnia and anxiety disorders is unknown; however, at the neurobiological level it has been proposed that the excitability of the right parietal cortex in patients with generalized anxiety disorder comorbid with insomnia was modulated by insomnia (33). Moreover, the inclusion of insomnia symptoms among the diagnostic criteria of anxiety and depressive disorders increases the probability for these comorbidities (34).
Polysubstance use understood as a history of addiction to three or more substances was identified as an independent risk factor for insomnia symptoms. The interaction between different withdrawal symptoms could partially explain this association. Patients who had been previously admitted for detoxification were also more likely to experience insomnia symptoms. These two factors can be considered as indicators of addiction severity that are closely associated with insomnia symptoms; therefore, insomnia could be a frequent symptom in patients with worse addiction treatment outcomes. In line with this, it is coherent that insomnia has been associated with early relapses in both alcohol use disorders and illegal substance use disorders patients (26, 27). It is important to treat insomnia symptoms because they have been identified as a risk factor for relapses after a detoxification process (26). A recent study has suggested that SUD patients who have been pharmacologically treated and have improved their insomnia symptoms maintained abstinence from substance use for longer in comparison with patients who did not improve from their insomnia symptoms (35). These findings highlight the need to treat insomnia symptoms during the therapeutic process.
Other significant factors in the bivariate analysis were age, ADHD, Cluster B personality, medical comorbidities, and heroin addiction. All these features have been identified as risk factors for insomnia in previous studies (3, 4, 7). Thus, psychiatry and medical comorbidities should be treated in order to improve insomnia symptoms and the quality of life of SUD patients (36).
Certain limitations of this study should be considered. First, electrophysiological tests such as polysomnography and actigraphy were not used to assess insomnia. However, it has been established that these objective measures should not take preference over clinical evaluation and clinical judgment. On the other hand, it should be considered that participants of this study were enrolled in a detoxification program and probably they were heavier users than patients seen in outpatient drug clinics. However, most patients with an SUD need to undergo detoxification at different stages of their addiction. It should also be noted that medications prescribed to patients during hospital detoxification may influence the presence or absence of insomnia symptoms, although all the patients in our study underwent a similar psychopharmacology approach. Unfortunately, the severity of insomnia was not included in the design; however, our future studies will include it.
Our study also has several strengths. The fact that we used psychometric tests to analyze a large sample of patients lends strength to the results, providing validity to the clinical diagnosis and the presence of insomnia symptoms. Finally, our findings also add to the limited data on the prevalence of symptoms of insomnia in patients with substance use disorders other than alcohol (12, 28).
We confirm that insomnia symptoms are very common among SUD patients during detoxification, especially the subtype sleep-maintenance insomnia (13). Polydrug use, comorbid anxiety disorder, prior admission to detoxification programs, and being female were independent factors associated with insomnia symptoms. A specific assessment and more psychotherapeutic and pharmacological strategies are needed that consider the symptoms of insomnia within the integral treatment of addictions, which is a common concern among these patients and a risk factor for relapse (12, 14, 27, 28). Sleep hygiene interventions should be included in the management of SUD patients in order to improve their quality of life and course of addiction treatment.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Psychiatry Department, Vall d' Hebron University Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to the Public Health Agency of Barcelona (ASPB), the Catalan institute of Health (ICS), and the Vall d'Hebron University Hospital for their support of the Hospital Detoxification Unit. We also thank Sonia Fuentes, Yasmina Pallares, Sira Díaz, and Nuria Tarifa from the Addiction and Dual Diagnosis Unit for their collaboration in psychometric assessment of the patients. We also thank Anne Murray for their collaboration in reviewing English language.
References
- 1.The International Classification of Sleep Disorders. Diagnostic and Coding Manual. 3rd ed Hanover: American Academy of Sleep Medicine; (2014). [Google Scholar]
- 2.Buysse DJ. Insomnia. JAMA. (2013) 309:706–16. 10.1001/jama.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung KF, Yeung WF, Ho FY, Yung KP, Yu YM, Kwok CW. Cross-cultural and comparative epidemiology of insomnia: the Diagnostic and statistical manual (DSM), International classification of diseases (ICD) and International classification of sleep disorders (ICSD). Sleep Med. (2015) 16:477–82. 10.1016/j.sleep.2014.10.018 [DOI] [PubMed] [Google Scholar]
- 4.Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. 10.1037/bul0000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamblin JE. Insomnia: an ignored health problem. Prim Care. (2007) 34:659–74. 10.1016/j.pop.2007.05.009 [DOI] [PubMed] [Google Scholar]
- 6.Cunnington D, Junge MF, Fernando AT. Insomnia: prevalence, consequences and effective treatment. Med J Aust. (2013) 199:36–40. 10.5694/mja13.10718 [DOI] [PubMed] [Google Scholar]
- 7.Sutton EL. Psychiatric disorders and sleep issues. Med Clin North Am. (2014) 98:1123–43. 10.1016/j.mcna.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 8.Khurshid KA. Comorbid insomnia and psychiatric disorders: an update. Innov Clin Neurosci. (2018) 15:28–32. [PMC free article] [PubMed] [Google Scholar]
- 9.Abad VC, Guilleminault C. Sleep and psychiatry. Dialogues Clin Neurosci. (2005) 7:291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spoormaker VI, Van den Bout J. Depression and anxiety complaints; relations with sleep disturbances. Eur Psychiatry. (2005) 20:243–5. 10.1016/j.eurpsy.2004.11.006 [DOI] [PubMed] [Google Scholar]
- 11.Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, Chen KT, et al. A study on the sleep quality of incoming university students. Psychiatry Res. (2012) 197:270–4. 10.1016/j.psychres.2011.08.011 [DOI] [PubMed] [Google Scholar]
- 12.Roncero C, Grau-López L, Díaz-Morán S, Miquel L, Martínez-Luna N, Casas M. [Evaluation of sleep disorders in drug dependent inpatients]. Med Clin. (2012) 138:332–5. 10.1016/j.medcli.2011.07.015 [DOI] [PubMed] [Google Scholar]
- 13.Cañellas F, de Lecea L. [Relationships between sleep and addiction]. Adicciones. (2012) 24:287–90. 10.20882/adicciones.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roth T. Does effective management of sleep disorders reduce substance dependence? Drugs. (2009) 69:65–75. 10.2165/11531120-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15.Teplin D, Raz B, Daiter J, Varenbut M, Tyrrell M. Screening for substance use patterns among patients referred for a variety of sleep complaints. Am J Drug Alcohol Abuse. (2006) 32:111–20. 10.1080/00952990500328695 [DOI] [PubMed] [Google Scholar]
- 16.Dimsdale JE, Norman D, DeJardin D, Wallace MS. The effect of opioids on sleep architecture. J Clin Sleep Med. (2007) 3:33–6. [PubMed] [Google Scholar]
- 17.Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. (2017) 19:23. 10.1007/s11920-017-0775-9 [DOI] [PubMed] [Google Scholar]
- 18.Schierenbeck T, Riemann D, Berger M, Hornyak M. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Med Rev. (2008) 12:381–9. 10.1016/j.smrv.2007.12.004 [DOI] [PubMed] [Google Scholar]
- 19.Dell'osso B, Lader M. Do benzodiazepines still deserve a major role in the treatment of psychiatric disorders? A critical reappraisal. Eur Psychiatry. (2013) 28:7–20. 10.1016/j.eurpsy.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 20.Irwin MR, Valladares EM, Motivala S, Thayer JF, Ehlers CL. Association between nocturnal vagal tone and sleep depth, sleep quality, and fatigue in alcohol dependence. Psychosom Med. (2006) 68:159–66. 10.1097/01.psy.0000195743.60952.00 [DOI] [PubMed] [Google Scholar]
- 21.Crum RM, Ford DE, Storr CL, Chan YF. Association of sleep disturbance with chronicity and remission of alcohol dependence: data from a population-based prospective study. Alcohol Clin Exp Res. (2004) 28:1533–40. 10.1097/01.ALC.0000141915.56236.40 [DOI] [PubMed] [Google Scholar]
- 22.Brower KJ, Krentzman A, Robinson EA. Persistent insomnia, abstinence, and moderate drinking in alcohol-dependent individuals. Am J Addict. (2011) 20:435–40. 10.1111/j.1521-0391.2011.00152.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest. (2018) 154:196–206. 10.1016/j.chest.2018.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sierra JC, Delgado-Dominguez C, Carretero-Dios H. [Internal structure of dysfuncional beliefs and attitudes about sleep scale in a Spanish shift workers sample]. Rev Neurol. (2006) 43:454–60. 10.33588/rn.4308.2005733 [DOI] [PubMed] [Google Scholar]
- 25.Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother. (2006) 4:168–92. 10.1016/j.amjopharm.2006.06.006 [DOI] [PubMed] [Google Scholar]
- 26.Grau-López L, Roncero C, Grau-López L, Daigre C, Rodríguez-Cintas L, Pallarés Y, et al. Factors related to relapse in substance-dependent patients in hospital detoxification: the relevance of insomnia. J Sleep Disor Treat Care. (2014) 3:3 10.1016/S0924-9338(14)78341-5 [DOI] [Google Scholar]
- 27.Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry. (2001) 158:399–404. 10.1176/appi.ajp.158.3.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grau-López L, Daigre C, Grau-López L, Rodriguez-Cintas L, Egido A, Casas M, et al. Administrative prevalence of insomnia and associated clinical features in patients with addiction during active substance use. Actas Esp Psiquiatr. (2016) 44:64–71. [PubMed] [Google Scholar]
- 29.World Medical Association World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. (2001) 79:373–4. [PMC free article] [PubMed] [Google Scholar]
- 30.Verkhratsky A, Nedergaard M, Steardo L, Li B. Editorial: sleep and mood disorders. Front Psychiatry. (2020) 16:981. 10.3389/fpsyt.2019.00981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steardo L, de Filippis R, Carbone EA, Segura-Garcia C, Verkhratsky A, De Fazio P. Sleep disturbance in bipolar disorder: neuroglia and circadian rhythms. Front Psychiatry. (2019) 10:501. 10.3389/fpsyt.2019.00501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faulkner S, Sidey-Gibbons C. Use of the pittsburgh sleep quality index in people with schizophrenia spectrum disorders: a mixed methods study. Front Psychiatry. (2019) 10:284. 10.3389/fpsyt.2019.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang Z, Zhan S, Chen C, Li N, Ding Y, Hou Y, et al. The effect of insomnia on cortical excitability in patients with generalized anxiety disorder. Front Psychiatry. (2019) 9:755. 10.3389/fpsyt.2018.00755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raffray T, Bond TL, Pelissolo A. Correlates of insomnia in patients with social phobia: role of depression and anxiety. Psychiatry Res. (2011) 189:315–7. 10.1016/j.psychres.2011.03.004 [DOI] [PubMed] [Google Scholar]
- 35.Grau-López L, Grau-López L, Daigre C, Palma-Álvarez RF, Rodriguez-Cintas L, Ros-Cucurull E, et al. Pharmacological treatment of insomnia symptoms in individuals with substance use disorders in Spain: a quasi-experimental study. Subst Use Misuse. (2018) 53:1267–74. 10.1080/10826084.2017.1402056 [DOI] [PubMed] [Google Scholar]
- 36.Daigre C, Grau-López L, Rodríguez-Cintas L, Ros-Cucurull E, Sorribes-Puertas M, Esculies O, et al. The role of dual diagnosis in health-related quality of life among treatment-seeking patients in Spain. Qual Life Res. (2017) 26:3201–9. 10.1007/s11136-017-1668-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.