Abstract
Background:
Ambulatory oncology practices treat thousands of Americans on a daily basis with high-risk and high-cost antineoplastic agents. However, we know relatively little about these diverse practices and the organizational structures influencing care delivery.
Objective:
To examine clinician-reported factors within ambulatory oncology practices that affect care delivery processes and outcomes for patients and clinicians.
Methods:
Survey data were collected in 2017 from 298 clinicians (nurses, physicians, nurse practitioners, and physician assistants) across 29 ambulatory practices in Michigan. Clinicians provided written comments about favorable and unfavorable aspects of their work environments that affected their ability to deliver high-quality care. We conducted inductive content analysis and used the Systems Engineering Initiative for Patient Safety (SEIPS) work system model to organize and explain our findings.
Results:
Clinicians reported factors within all five work system components of the SEIPS model that affected care delivery and outcomes. Common themes surfaced, such as unfavorable aspects including staffing inadequacy and high patient volume, limited physical space, electronic health record (EHR) usability issues, and order entry. Frequent favorable aspects focused on the skills of colleagues, collaboration, and teamwork. Some clinicians explicitly reported how work system factors were relational and influenced patient, clinician, and organizational outcomes.
Conclusions:
These findings show how work system components are interactive and relational reflecting the complex nature of care delivery.
Implications for Nursing Practice:
Data obtained from front-line clinicians can support leaders in making organizational changes that are congruent with clinician observations of practices’ strengths and opportunities for improvement.
Keywords: Organization of care, ambulatory oncology, health care quality
Introduction
There is much to be discovered about the complex and dynamic nature of ambulatory oncology settings, particularly around organizational structure and processes of care. In the United States, an estimated 19 million of the 23 million chemotherapy visits that take place each year occur in ambulatory oncology settings.1 The 1.7 million newly diagnosed patients with cancer in the U.S. will receive chemotherapy treatments primarily at ambulatory oncology settings.1 Ambulatory oncology settings are primarily located in outpatient facilities in close proximity to hospitals and community-based practices.2
Previous work has shed light on important factors in ambulatory oncology care, including nurse-physician relationships, the nurse practice environment, and clinician perceptions of the electronic health record (EHR).3-6 However, there remains a knowledge gap in understanding structural factors affecting the clinician-reported quality of patient care in ambulatory oncology settings.
Ambulatory oncology settings face external challenges to delivering high-quality patient care as increasing financial pressures have led to practice closure and consolidation.2,7 Since 2008, 1,653 community oncology practices in the United States have closed, been acquired by hospitals, merged, or reported financial struggles.2 Michigan has been particularly susceptible to external pressures as statewide it had the third highest number of clinic closures in 2018 (36) and the most practices struggling financially (42), making it a fitting setting to study changing ambulatory oncology practice environments.2 In addition, the field faces a shrinking workforce responsible for caring for an ever-expanding population of cancer patients, expected to double by 2030.8 The result has been described as a ‘system in crisis’ that, despite attempts at change over the past decade, continues to present significant challenges to clinicians, patients, and management alike.8 It is within this evolving environment of ambulatory oncology settings that care delivery must be better understood so that policies and interventions might be incorporated as new practice models are being implemented.
This study aims to help fill the gap in knowledge by describing clinician-reported structural factors affecting the quality of patient care in ambulatory oncology practices throughout Michigan. Through examining clinician-reported structural barriers and facilitators to high-quality ambulatory oncology care, this study aims to help inform system interventions for quality improvement to reduce variation in outcomes and improve patient safety. The current inquiry also informs efforts to improve clinician practice environments to decrease the likelihood of clinician burnout and promote well-being.9 A more thorough understanding of the interconnected, structural composition of ambulatory oncology practices will highlight how attention to particular factors can affect and improve organizations as a whole. We join Alexander and Hearld’s10 call for ‘robust’ and ‘clear’ research that can be transferred into practice through dialogue around quality improvement, particularly relating to future research in ambulatory oncology care.
Methods
Sample and Survey
This study was part of a larger effort to explore communication technologies, clinician communication, and patient outcomes in ambulatory oncology practices. The sampling frame consisted of 48 ambulatory oncology practices that participate in the Michigan Oncology Quality Consortium (MOQC), a state-wide program focused on improving the care of cancer patients in Michigan. Twenty-nine ambulatory oncology practices agreed to participate (4 academic and 25 community). The survey data were collected over a 6-week period in 2017 via anonymous paper surveys, which were distributed by site leads. This study was reviewed and approved by the [University’s] Institutional Review Board.
The survey was administered to 438 clinicians (registered nurses, physicians, nurse practitioners, and physician assistants) who managed patient care before, during, and after chemotherapy infusion treatments. Survey packets contained a cover letter, the survey, a $10 cash incentive, and a self-addressed stamped envelope for returning completed surveys to the investigative team. The overall survey response rate was 68%. Registered nurses were asked several questions specific to their clinical role. Hence, prescribers (physicians, nurse practitioners and physician assistants) received a slightly different survey from registered nurses.
Following preliminary participant questions, there was an identical section in both prescriber and nurse surveys where clinicians were asked to write in open-text responses to two questions. In this section, titled ‘Your Work Environment,’ clinicians were asked: 1) ‘What unfavorable aspects of your environment decrease your ability to deliver high-quality care?’ and 2) ‘What favorable aspects of your environment enable you to deliver high-quality care?’ Text boxes had several lines for hand-written comments. Participants were not provided a definition of favorable and unfavorable, which enabled them to report from their own perspective. The choice of the words “favorable and unfavorable” for the survey stem from earlier conceptual and measurement work by Lake (2002) as to how to characterize clinical practice environments11. Of the 298 surveys received, 254 participants (157 nurses and 97 physicians, nurse practitioners, or physician assistants) provided text comments ranging from one to 122 words.
Analytic Approach
We entered open-text comments into a spreadsheet, organized by ‘favorable’ and ‘unfavorable’ responses. Using an inductive content analysis approach, [Author A] read through the responses and developed categories from the open-text comments. Sub-categories were also created to reflect the nuances within the responses. All responses were then sorted into these categories and subcategories.12 For example environment was a category that included physical space and cleanliness as subcategories, as they are specific characteristics of the environment that were common in the responses. Unlike a deductive approach that relies on a theoretical lens through which to analyze data, our inductive analysis of raw data allowed us to identify dominant categories important to respondents. We then reviewed the literature to find a work system model to better understand and organize the data. We found that the Systems Engineering Initiative for Patient Safety (SEIPS) model reflected our data and would be useful in explaining our findings.13
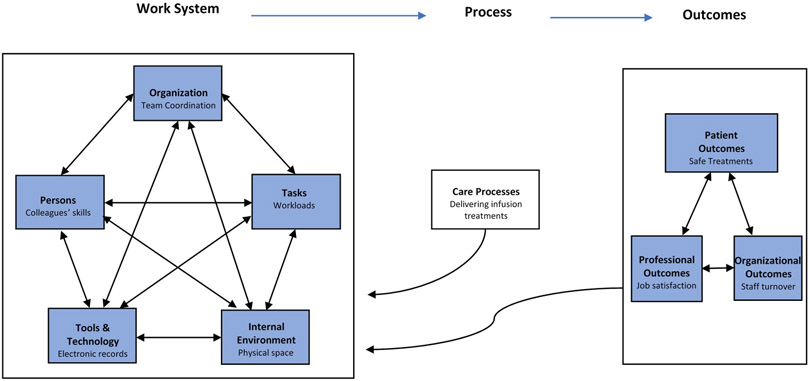
SEIPS expands upon Donabedian’s classic structure-process-outcome framework through a deeper focus on structural elements, specifically work system design and interactions between components that affect processes and subsequent outcomes (Figure 1).14 The work system consists of five components: persons (clinicians), organization, tools and technology, tasks, and internal environment. Examples of factors comprising each component are provided in the Table. The SEIPS model considers how components within work systems and processes can impact not only outcomes related to patients, but also professional outcomes such as the safety, satisfaction, burnout, and turnover of employees, as well as organizational outcomes like profitability.15 Applying this lens to ambulatory oncology practices, we can understand clinician-reported factors of their environments and how clinicians relate these factors to care delivery outcomes.
Figure 1.
SEIPS model of work system and partient safety, with exemplars from study from study data
Table.
Components and Factors of the SEIPS Model
| Work System (Structure) |
Model
Components |
Factors Cited by Survey Respondents |
| Persons | Skills, Knowledge, Expertise of colleagues | |
| Organization | Coordination, Collaboration, Communication Teamwork, Collegiality Patient safety culture Supervisor and management support | |
| Tasks | Job demand (workload, cognitive load) Adequate staffing, Patient volume | |
| Internal Environment | Physical space and design Sound, Lighting, Cleanliness | |
| Tools & Technology | Electronic Health Record, Computerized Provider Order Entry Clinical equipment, Materials | |
| Process | Care Processes | Care processes |
| Outcomes | Patient | Safety, Privacy |
| Professional | Safety, Well-being, Job satisfaction, Burnout | |
| Organizational | Staff turnover, Profitability |
Abbreviation: SEIPS, Systems Engineering Initiative for Patient Safety 15
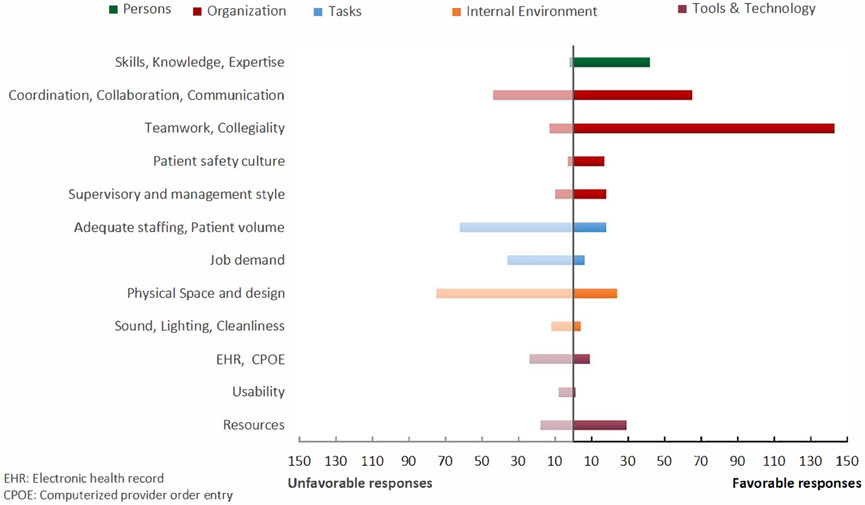
Using our analytical categories that matched the five SEIPS components, we defined the factors of each component based on our subcategories. For example, subcategories such as teamwork and supervisor support were included as factors of organization to reflect our data. The components and related factors from our responses are displayed in the Table. If a write-in response listed multiple factors (e.g. limited space and poor communication), each factor was coded to the corresponding SEIPS component (e.g. internal environment and organization). If a respondent listed several examples of the same factor (e.g. collaboration and teamwork), the response was only included as one code for the related SEIPS component (organization). As survey data were coded to reflect the participant’s practice, we also report the number of practices where survey participants provided comments that correspond to respective factors. To ensure reliability, data were analyzed and sorted by a second reviewer, and any discrepancies in categorization were resolved through a consensus approach. This collaborative process was used as a means to assess the rigor and trustworthiness of the data and subsequent analysis.3 The favorable and unfavorable responses by clinicians in this study are organized into components and factors of the work system in Figure 2.
Figure 2.
Work System Components and Factors: Unfavorable and Favorable Responses
Results
Our analysis revealed common themes across a majority of practices. As shown in Table 1, clinicians reported factors representing all five work system components: person (such as skills of colleagues); organization (such as coordination and collaboration with colleagues); tasks (job demand, adequate staffing, and patient volume); environment (physical space, lighting, and sound); and technologies and tools (EHR, CPOE, and usability).
Participants cited similar factors with both positive and negative comments, and often clinicians’ comments identified overlapping themes, highlighting the relational dimensions of care delivery. Figure 2 displays the total ‘favorable’ and ‘unfavorable’ responses organized by work system components and their factors, illustrating the frequency factors were reported across a variety of practices.
Some clinicians explicitly reported how particular work system factors influenced outcomes such as patient safety, patient privacy, and employee well-being. In the following sections we describe the findings, organized by the corresponding work system components, and provide verbatim examples of clinician-reported factors. The associated outcomes clinicians reported are described as they relate to each component of the SEIPS model.
Organization- Coordination, teamwork, and communication
Collegiality and collaboration were widely reported as facilitators to high-quality patient care. Organizational factors were cited favorably across 26 of the 29 participating practices (90 percent). Clinicians also reported the quality of communication with colleagues as a factor influencing patient care, both favorably and unfavorably.
Many respondents said they felt supported by colleagues. Nurses wrote about the importance of collaboration with other nurses, in comments such as: ‘Team nursing work environment allows for safe and consistent flow of care to patients.’ Clinicians also referred to the importance of collaboration between co-workers across all roles. For instance, one nurse wrote: ‘Team atmosphere. Able to question providers without negative feedback.’ Prescribers contributed similar responses such as: ‘Excellent healthcare team, support staff is great;’ and ‘Good staff, team approach to care.’
Communication was highly cited as both a facilitator and a barrier to high-quality patient care. Favorable aspects of communication included comments such as: ‘Cohesive team, great communication amongst team members;’ and ‘Communication between different areas (pharmacy, infusion, etc.);’ and ‘Communication with other RNs, MAs, front desk and billing department.’
Many unfavorable comments addressed poor communication across roles and departments and difficultly getting responses from colleagues. Responses from ten of the 29 practices cited communication challenges. For instance, one nurse wrote: ‘Miscommunication between clinic & infusion nurses/ staff.’ Nurses comments often referenced communication challenges with physicians, such as: ‘Delayed/ lack of communication from physicians and management;’ ‘Physicians not always helpful or reachable for patient issues;’ and ‘Sometimes physicians can be difficult to reach when off-site, when quick response is needed for patient care.’
Persons- Skills, knowledge, and expertise of team members
In the ‘favorable aspects’ responses, clinicians overwhelmingly reported having highly-skilled, knowledgeable team members with whom they worked across a variety of roles. Rated positively across 13 of the 29 practices, nurses wrote responses such as: ‘Great Drs & nurses providing care;’ ‘Working with a team of experienced, caring practitioners/nurses;’ ‘Excellent docs and providers and RNs;’ and ‘Many knowledgeable colleagues at many different levels.’ Prescribers (physicians, nurse practitioners, and physician assistants) commented: ‘Excellent nurses, Experienced colleagues;’ ‘Quality support staff;’ and ‘staff [has] excellent knowledge of up-to-date oncology care.’
Task- Job demand, staffing, and patient volume
Despite many clinicians reporting their colleagues’ skills and expertise as an asset to their practices, they also frequently identified a shortage of staffing, high patient volume, and issues with patient scheduling as factors hindering their ability to provide high-quality care. Concerns for staffing and workloads were reported by 21 of the 29 participating practices. Clinicians reported that the outcomes of staffing shortages and high patient volume were delays in patient care, lack of available appointments, and a lack of support services. Furthermore, the high patient volume and poor scheduling contributed to limited physical space and availability of infusion chairs in many practices. Some clinicians linked variable workloads to clinician and patient outcomes, such as: ‘High turnover of nursing which leads to breaks in care for patients. Causes providers to do more tasks and less direct patient care.’
Many comments from clinicians focused on a shortage of nurses, which they felt affected patient care. For instance, nurses wrote answers such as: ‘RN shortage. I feel like we aren’t staffed appropriately to deliver high quality care on most days;’ and ‘Not enough nurses when chemo is running.’ Nurses reported staffing shortages, and even cuts, despite an increasing volume of patients: ‘Decreased staff when our patient numbers increase 30%.’ Prescribers similarly reported: ‘Not enough staff to triage patients over the phone;’ and ‘Pressure to see an unreasonable number of patients in clinic.’
Clinicians reported problems with patient scheduling that led to too many patients needing care simultaneously, particularly in infusion areas. Nurses wrote: ‘Too many patients scheduled at same time or arrive at same time;’ ‘Patient scheduling has been as issue for the last several months. We are top heavy, sometimes having 5–6 patients at once;’ ‘Continually overbooked AM schedule by at least 6-8 patients;’ and ‘Patients being scheduled too close together. Ex. 9 or 10 from 7:30 am to 8:30 with only 4 or 5 nurses and 1 [medical assistant].’
The shortage of support staff and services also hindered the ability to provide quality patient care. For instance, a nurse reported: ‘Lack of services- home care coordinator, dietician, social worker not available expect once/ week …’ Prescribers wrote responses such as: ‘Lack of support staff;’ and ‘Limited staff at check in/ check out- delay patient care. Limited staff to perform blood draws in timely manner.’
Internal Environment- Space, design layout, and other environmental factors
Clinicians frequently reported aspects of their practice environments as a barrier to providing quality patient care. Clinicians in 15 of the 29 participating practices reported limited space in many of their practices, which they said contributed to patient overcrowding, delays of care, and limited patient privacy. Other characteristics of their practice environments such as noise, cleanliness, and lighting that affect patient comfort and healing were concerns for clinicians.
Clinicians often commented that there was a lack of adequate space in their practices, both in infusion areas and exam rooms. Nurses also reported a limited number of infusion chairs with comments such as: ‘Not enough chemo chairs to accommodate patients as needed at all times.’ Some nurses wrote that their own work space was cramped and difficult to work in. Prescribers commented that the lack of available exam rooms had work flow consequences: ‘Patients are often not roomed in a timely fashion, either due to lack of open exam rooms or medical assistants not working to room patients quickly, this results in us running behind.’
The high volume of patients plus limited space contributed to concerns about patient privacy, such as a nurse reported: ‘Patients have minimal privacy, we are very busy and space is crowded.’ Other clinicians reported: ‘Major HIPAA violations due to close proximity of [patients];’ ‘Too crowded, some patient comfort and privacy concerns;’ and ‘Very small clinic infusion room with close seating between patients- difficult maintaining privacy/ confidentiality.’
Clinicians reported other environmental factors such as noise, cleanliness, and lighting as having a negative impact on patient experience. One nurse who commented on the lack of privacy for patients also pointed out that it is a ‘noisy environment’ and that some rooms have no windows. Other clinicians mentioned: ‘Very dirty and too small of a space;’ and ‘Lighting is not the best.’ One clinician pointed out how the messy practice environment had direct consequences for the patient healing process: ‘Very messy. Extra poles, rolling chairs, wheelchairs are stored in patient area. It’s not an area that welcomes rest and healing, it’s a mess.’
Tools and Technology- EHR, CPOE, and usability
Clinicians commented on problems with the EHRs in their practices. Many respondents simply listed ‘EHR’ in their comments, signaling an overall discontent with the system and software without describing specific challenges. EHR challenges and concerns were reported across 14 of the 29 participating practices. Common EHR challenges were related to usability and navigation, clinician use and order entry, and complex care coordination.
Several clinicians reported that their EHRs hindered effective patient documentation and were prone to error; for instance: ‘Current documentation system- I’ve seen errors occur because the system doesn’t perform certain functions;’ and ‘Problems with electronic charting.’
Furthermore, prescribers and nurses commented that there is inconsistent documentation by staff and that physicians in particular are not using EHRs correctly for plans of care and chemotherapy orders. Some clinicians reported that physicians enter unclear orders, which must then be clarified, taking time away from direct patient care. For instance, a prescriber wrote: ‘MDs don’t use [EHR] well.’ Nurses wrote: ‘Much time is involved in clarifying physician orders;’ and ‘Unclear doctor progress notes/ orders.’ One nurse reported problems with both the use and functionality of the EHR: ‘Physicians not using [EHR] efficiently. [EHR] is not that user friendly and created delays in patient care.’
These comments suggest a lack of adequate clinician training on EHR systems, as one nurse reported there was ‘not any training on [EHR].’ Incorrect or delayed progress notes and orders also seem to occur in part due to lack of physician accountability or standardized EHR policies in particular practices, as a nurse articulated: ‘Inability to hold physicians accountable for completing safe, clear orders.’
Clinicians reported problems coordinating patient care via EHR with other health services outside of and within their own practices. Even when coordinating with the same EHR, one nurse reported: ‘Our [EHR] and system of communication between oncology office and infusion, I feel a lot gets lost.’ Some practices use various electronic systems for charting, order entry, chemotherapy scheduling, and labs, which further complicates coordination of care. For example, at one practice, all of the nurse respondents wrote that there were ‘too many’ or ‘multiple’ computer systems to access for patient care. A nurse at another practice wrote: ‘We are a server based electronic record and sometimes they don’t cross, causing errors with chemotherapy orders/ dosing.’ One practice had a separate program for lab orders, which a nurse wrote were transferred to another program by a non-clinician, resulting in frequently-missed lab orders.
Discussion
These results from a large, diverse sample of clinicians practicing in ambulatory oncology settings show that factors from all five work-system components outlined in the SEIPS model (persons, organization, tools and technology, tasks, and internal environment) impact clinicians’ abilities to deliver high-quality care in ambulatory oncology practices. Within each component, clinicians reported factors that have implications for patient outcomes such as safety and privacy. For instance, clinicians had concerns around patient privacy outcomes and potential HIPPA violations stemming from increasing patient volume, poor patient scheduling, and lack of adequate space, particularly in infusion areas. In addition, staffing and organizational outcomes, such as the reported outcome of staff turnover, suggest clinician well-being may be suffering. Staff turnover also has financial implications for health care organizations, as the cost to replace a nurse who resigns, for instance, is 1.2 to 1.3 times their salary.16 These findings demonstrate how various components within work systems are interactive and relational, reflecting the complex nature of care delivery. Patient, professional, and organizational outcomes are all intertwined.
Factors related to staffing were widely reported throughout the practices, including inadequate staffing, high patient volume, heavy workloads, scheduling challenges, and suboptimal staffing support services. These findings are consistent with other studies that have identified pervasive staffing and workload challenges in ambulatory infusion settings.17,18 In a 2016 Oncology Nursing Society member survey, 64% of respondents reported ‘appropriate staffing levels’ and 50% reported ‘staff training and education’ as the most pressing challenges facing their practices.18 While attention has been paid to staffing within the inpatient setting, staffing in the outpatient setting has received less attention. This inattention has implications for clinician burnout, which has been attributed to high patient to nurse ratios.19 Furthermore, excessive workloads and poor staffing that affect clinician well-being also threaten patient safety.20 For instance, errors in medication administration have been linked with excessive workloads and nursing shortages in several studies.21,22
There are risks associated with computer order entry systems that can produce medication errors.23 Our results also suggest there are challenges for clinicians to use EHRs effectively to coordinate and document care. Practices use a variety of technologies, which increases the complexity and coordination of chemotherapy delivery while providing few safeguards against errors. Many clinicians reported inconsistencies and confusion around patient plans of care and chemotherapy orders, which delayed patient care. Some clinicians linked these problems with inadequate physician training on EHR and lack of accountability for complying with standardized EHR policies.
Regular use of multiple electronic systems to provide patient care can disrupt the work flow of clinicians and create frequent interruptions, creating more opportunities for potential errors. Clerical burden, caused by excessive time spent on tasks such as computerized order entry and documentation, can contribute to clinician burnout.9 Physicians treating oncology patients may be especially affected, as one study found radiation oncology among the four specialties least satisfied with their EHRs.9
It is important to consider the study findings in the context of the national landscape for ambulatory oncology care. In a 2018 trends analysis, the Association of Community Cancer Centers surveyed cancer care professionals from 161 organizations, and 41% of respondents ranked care coordination as a top three opportunity for cost savings.17 Yet a majority of respondents endorsed that EHRs ‘somewhat improved’ care coordination, which suggests that the full potential of EHRs to improve coordination in ambulatory oncology settings has yet to be fulfilled. Moreover, 59% of surveyed respondents agreed that EHRs have ‘significantly’ or ‘somewhat’ worsened clinician well-being.17
Safe chemotherapy delivery requires effective communication among clinicians to identify and manage adverse events before lethal complications ensue. Our results show the importance of clinician collaboration and collegiality in delivering care to patients with cancer. This finding aligns with previous research studies that found favorable nurse physician relationships in ambulatory oncology practices correlated significantly with favorable work environments and higher nurse-reported quality of care.3,6
Limitations
This study has several limitations. The survey was designed to collect quantitative data and was not designed a priori for qualitative analyses. These text comments are limited in depth, length, and context, compared to interviews for instance, and ambiguous comments were challenging to interpret on occasion. However, these emic comments illuminate key issues clinicians felt strongly about across a diverse array of practices that they would otherwise not be able to voice in a survey with pre-selected questions deemed important by the survey designers. Given that the survey was administered within one state in the Upper Midwest, it may not be generalizable to ambulatory oncology settings in other areas. Our aim is not to generalize these responses to the views of all clinicians in ambulatory oncology settings, but rather to use the respondents’ comments in this sample to illuminate potential areas for improvement. In future research, methods to collect and analyze detailed data on staffing models, physical layout, and EHR software and use would inform subsequent intervention development. Observation across various practice settings would provide a better understanding of care delivery in situ, which has been largely overlooked.
Practice Implications
While some changes to work systems may be unrealistic for practices to address due to cost, some changes might be easier to implement at little to no cost, such as minor alterations to the physical environment. For instance, attention to noise reduction, improved lighting, and other minor physical adjustments within clinical settings could provide a more comfortable and healing environment for patients, who are often receiving chemotherapy treatments for many hours at a time. Practice environment changes, such as involving clinicians in key operational decisions, could also help influence clinician well-being and job satisfaction, reducing the likelihood of burnout and staff turnover. Physical plant limitations could be addressed through re-organizing staff assignments and patient scheduling to promote visibility and increase efficiency of patient flow.
Our study findings highlight important organizational changes to improve clinician satisfaction with EHRs and reduce risk of errors and treatment delays. These include increased attention to maximizing clinician function and use, providing adequate training, particularly to physicians, and establishing a floor for minimum documentation standards and timetables. Practice leaders could coach and support clinicians who are not meeting these standards and timetables.
Our findings suggest that EHR systems designed for large, multi-specialty health care organizations lack the nuances preferred by oncology clinicians. Understanding which EHR functions are most challenging and burdensome for clinicians can help inform system modifications and redesign. Perhaps unique to oncology, completion of provider notes before chemotherapy orders are transmitted is an essential ingredient to timely treatment. One promising approach to ease clerical burden is adopting advanced care team models, which have been shown to improve documentation and quality of care.24,25 In these collaborative models, a clinically-trained assistant, such as a registered nurse, helps with documentation during the patient visit, which ensures EHR progress notes and orders are current while simultaneously increasing the efficiency of patient flow.
These findings suggest that practice leaders should strive to support good working relationships and teamwork among clinicians as a strategy to foster quality patient care and clinician well-being. Congruent with positive organizational scholarship, this is an opportunity to build on strengths of the practice and clinicians to facilitate collaborative problem solving.26,27
Implications for Cancer Nursing Practice
This study provides novel insight into a diverse sample of oncology clinicians as to the supportive and prohibitive features of their clinical settings. Such data provide practice administrators with a relatively narrow target of positive attributes that may be fruitful to build upon. Conversely, this large sample of clinicians also provide ample, but actionable areas to strengthen. Solicitation of candid feedback from clinicians is a promising strategy to prioritize efforts to improve quality, support organizational resilience, and promote optimal clinician and patient outcomes. Within the context of oncology nursing shortages, increased patient volumes and clinical acuity, and the explosive growth of novel treatments, deliberate attention to work environment attributes may stem clinician burnout and turnover, which in turn negatively affect the workplace and the capacity to deliver safe and effective cancer nursing services.28,29
Conclusion
Research illuminating clinicians’ perspectives about their practice environments and care delivery is crucial to help inform quality improvement interventions and make policy recommendations in oncology ambulatory settings. Given increased interest in pay for performance and accountable care models,30 research focused on ambulatory oncology practices will inform a road map to higher-quality care for a large patient population at risk for adverse events associated with toxic treatments. While this research has provided a better understanding of the structural factors affecting patient and clinician outcomes in ambulatory oncology settings, more research is needed observing clinicians as they navigate through day-to-day care processes and interact with system components that affect their practice and ultimate patient outcomes.
Acknowledgments:
This research was funded by the Agency for Healthcare Research and Quality- R01HS024914 and the National Cancer Institute of the National Institutes of Health- P30CA046592.
Footnotes
The authors have no funding or conflicts of interest to disclose.
Contributor Information
Megan Lafferty, University of Michigan School of Nursing, Ann Arbor, MI.
Milisa Manojlovich, University of Michigan School of Nursing, Ann Arbor, MI.
Jennifer J. Griggs, Michigan Oncology Quality Consortium; Division of Hematology/ Oncology, Internal Medicine, University of Michigan, Ann Arbor, MI.
Nathan Wright, University of Michigan School of Nursing, Ann Arbor, MI.
Molly Harrod, Ann Arbor Veterans Administration Health System, Center for Clinical Management Research.
Christopher R. Friese, University of Michigan School of Nursing, Ann Arbor, MI.
References
- 1.National Cancer Institute. Cancer Stat Facts: Cancer of Any Site.
- 2.Community Oncology Alliance. 2018 Community Oncology Alliance Practice Impact Report.; 2018.
- 3.Friese CR, Manojlovich M. Nurse-Physician Relationships in Ambulatory Oncology Settings. J Nurs Scholarsh. 2012;44(3):258–265. doi: 10.1111/j.1547-5069.2012.01458.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamimura A, Schneider K, Lee CS, Crawford SD, Friese CR. Practice Environments of Nurses in Ambulatory Oncology Settings: A Thematic Analysis. Cancer Nurs. 2012;35(1):E1–E7. doi: 10.1097/NCC.0b013e31820b6efa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanauer DA, Branford GL, Greenberg G, et al. Two-year longitudinal assessment of physicians’ perceptions after replacement of a longstanding homegrown electronic health record: does a J-curve of satisfaction really exist? J Am Med Informatics Assoc. 2016;24(e1):ocw077. doi: 10.1093/jamia/ocw077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Friese CR, Siefert M Lou, Thomas-Frost K, Walker S, Ponte PR. Using data to strengthen ambulatory oncology nursing practice. Cancer Nurs. 2016;39(1):74–79. doi: 10.1097/NCC.0000000000000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Towle EL, Barr TR, Senese JL. The National Practice Benchmark for Oncology, 2014 Report on 2013 Data. J Oncol Pract. 2014;10(6):385–406. doi: 10.1200/JOP.2014.001826 [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, D.C.: National Academies Press; 2013. doi: 10.17226/18359 [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship Between Clerical Burden and Characteristics of the Electronic Environment With Physician Burnout and Professional Satisfaction. Mayo Clin Proc. 2016;91(7):836–848. doi: 10.1016/j.mayocp.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 10.Alexander JA, Hearld LR. The Science of Quality Improvement Implementation: Developing Capacity to Make a Difference. Med Care. 2011;49:S6–S20. doi: 10.1097/MLR.0b013e3181e1709c [DOI] [PubMed] [Google Scholar]
- 11.Lake ET. Development of the practice environment scale of the nursing work index. Res Nurs Heal. 2002;25(3):176–188. doi: 10.1002/nur.10032 [DOI] [PubMed] [Google Scholar]
- 12.Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative Content Analysis: A Focus on Trustworthiness. SAGE Open. 2014. doi: 10.1177/2158244014522633 [DOI] [Google Scholar]
- 13.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–1686. doi: 10.1080/00140139.2013.838643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donabedian A The Quality of Care: How Can It Be Assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.1988.03410120089033 [DOI] [PubMed] [Google Scholar]
- 15.Carayon P, Schoofs Hundt A, Karsh B-T, et al. Work system design for patient safety: the SEIPS model. Qual Saf Heal Care. 2006;15(1):i50–i58. doi: 10.1136/qshc.2005.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones CB. The Costs of Nurse Turnover, Part 2: Application of the Nursing Turnover Cost Calculation Methodology. JONA J Nurs Adm. 2005;35(1):41–49. doi: 10.1097/00005110-200501000-00014 [DOI] [PubMed] [Google Scholar]
- 17.Association of Community Cancer Centers. Highlights from the 2018 Trending Now in Cancer Care Survey.; 2019.
- 18.Nevidjon B Member Input: The Challenge of Staffing in Ambulatory Infusion Settings. Clin J Oncol Nurs. 2018;22(2):225–227. doi: 10.1188/18.CJON.225-227 [DOI] [PubMed] [Google Scholar]
- 19.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- 20.Tuna R, Baykal U, Turkmen E, Yildirim A. Planning for the Size of the Nursing Staff at an Outpatient Chemotherapy Unit. Clin J Oncol Nurs. 2015;19(6):E115–E120. doi: 10.1188/15.CJON.E115-E120 [DOI] [PubMed] [Google Scholar]
- 21.Bailey CG, Engel BS, Luescher JN, Taylor ML. Medication Errors in Relation to Education and Medication Errors in Relation to Years of Nursing Experience.; 2008.
- 22.Rinke ML, Shore AD, Morlock L, Hicks RW, Miller MR. Characteristics of pediatric chemotherapy medication errors in a national error reporting database. Cancer. 2007;110(1):186–195. doi: 10.1002/cncr.22742 [DOI] [PubMed] [Google Scholar]
- 23.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. J Am Med Assoc. 2005;293(10):1197–1203. doi: 10.1001/jama.293.10.1197 [DOI] [PubMed] [Google Scholar]
- 24.Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15(7–8). [PubMed] [Google Scholar]
- 25.Hopkins KD, Sinsky CA. Team-based care: Saving time and improving efficiency. Fam Pract Manag. 2014;(Nov-Dec 2014):23–29. [PubMed] [Google Scholar]
- 26.Luthans KW, Lebsack SA, Lebsack RR. Positivity in healthcare: relation of optimism to performance. J Health Organ Manag. 2008;22(2):178–188. doi: 10.1108/14777260810876330 [DOI] [PubMed] [Google Scholar]
- 27.Calarco MM. The Impact of Positive Practices on Nurse Work Environments: Emerging Applications of Positive Organizational Scholarship. West J Nurs Res. 2011;33(3):365–384. doi: 10.1177/0193945910380211 [DOI] [PubMed] [Google Scholar]
- 28.Friese CR, Himes-Ferris L. Nursing Practice Environments and Job Outcomes in Ambulatory Oncology Settings. JONA J Nurs Adm. 2013;43(3):149–154. doi: 10.1097/NNA.0b013e318283dc3f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friese CR. Nurse Practice Environments and Outcomes: Implications for Oncology Nursing. Oncol Nurs Forum. 2005;32(4):765–772. doi: 10.1188/05.ONF.765-772 [DOI] [PubMed] [Google Scholar]
- 30.Shortell SM, McClellan SR, Ramsay PP, Casalino LP, Ryan AM, Copeland KR. Physician Practice Participation in Accountable Care Organizations: The Emergence of the Unicorn. Health Serv Res. 2014;49(5):1519–1536. doi: 10.1111/1475-6773.12167 [DOI] [PMC free article] [PubMed] [Google Scholar]