Abstract
Parents in the United States increasingly report bed-sharing with their infants (i.e., sleeping on a shared sleep surface), but the relationship between bed-sharing and child socioemotional outcomes are not well understood. The current study examines the links between mother-infant bed-sharing at 3 months and infant affect and behavior during a dyadic challenge task at 6 months. Further, we examine nighttime mother-infant contact at 3 months as a possible mechanism that may mediate linkages between bed-sharing and infant outcomes. Using observational data from a sample of 63 mother-infant dyads, we found that infants who bed-shared for any proportion of the observation period at 3 months displayed significantly more self-regulatory behaviors during the still-face episode of the Still-Face Paradigm (SFP) at 6 months, compared to non-bed-sharing infants. Also, infants of mothers who bed-shared for the entire observation period displayed significantly less negativity during the reunion episode than non-bed-sharing infants. There was no evidence that the relations between mother-infant bed-sharing practices and infant affect and behavior during the SFP were mediated through nighttime mother-infant contact. Results suggest that infant regulation at 6 months postpartum may vary based on early nighttime experiences, with bed-sharing potentially promoting more positive and well-regulated behavior during dyadic interaction.
Keywords: sleep location, bed-sharing, mother-infant interaction, still-face paradigm
Co-sleeping is commonly defined as a child sleeping in close proximity to the parent(s), whether on the same sleep surface (bed-sharing) or in the same room on a separate sleep surface (room-sharing; McKenna, Ball, & Gettler, 2007). Parents in the United States report co-sleeping with their infants for reasons such as preference and to facilitate sleep (Tully, Holditch-Davis, & Brandon, 2015), housing/financial circumstances (e.g., space limitations, inability to purchase a crib), and infant care and breastfeeding convenience (Ball, 2002). Report of infant-caregiver bed-sharing in the United States increased from 6.5% in 1993 to 13.5% in 2010 (Colson et al., 2013); however, women also report intentionally misrepresenting their infant sleep arrangements due to anticipating bed-sharing judgement (Tully, Stuebe, & Verbiest, 2017). Most of the infant sleep literature has not distinguished between the range of co-sleeping arrangements, such as bed-sharing and room-sharing, nor trade-offs associated with such practices outside of infant feeding outcomes and mortality risk. Thus, the current paper focuses specifically on bed-sharing on an adult bed or another shared sleep surface during the nighttime as an experience that may impact infant development, as assessed by observed infant affect and behavior with the mother during a standardized challenge.
Where an infant sleeps during the night may have an influence on their developmental trajectories. Societies across the world differ in the way that they perceive bed-sharing and its impact on a child’s autonomy and independence (McKenna & McDade, 2005). Thus, cultural norms impact expectations for infant sleep and lived experiences (Shimizu & Teti, 2018). One study found that children in the United States who bed-shared early in infancy were more self-reliant and displayed more social independence at 36 to 68 months of age than children who did not bed-share (Keller & Goldberg, 2004). Similarly, a study conducted in northern Spain found that bed-sharing in childhood (ranging from age 2–6) predicted greater confidence, self-esteem, and intimacy in adulthood (Crawford, 1994). Although evidence is mixed on the relation between bed-sharing and child autonomy and independence, it is clearly important to consider the effects of bed-sharing on early child social-emotional processes. The current study is the first to our knowledge to utilize observational data to assess this link. More specifically, this study examines mother-infant bed-sharing practices at 3 months in relation to infant affect and behavior within a mother-child interaction at 6 months.
1.1. Mother-Infant Bed-Sharing Practices and Infant Affect and Behavior within the Mother Child Relationship
According to Ainsworth, Blehar, Waters and Wall (1978), mothers’ physical and psychological availability are important factors that contribute to an infant’s attachment, which is a marker of an infants’ affect and behavior within the parent-child relationship. Similarly, maternal physiology and emotions are primed for frequent, close contact with their infants. Those needs do not end at nighttime. Thus, there is reason to believe that the close proximity between bed-sharing mothers and infants may promote positive infant affect and behavior within the mother-child dyadic relationship. Only one study to date has investigated the association between infant sleep location and mother-child attachment, as indexed by infant behavior and affect (Mileva-Seitz et al., 2016). Focusing on a sample of White families in the Netherlands, the study used maternal reports at 2 months of infant age to classify infants into groups of “never bed-sharing” or “any bed-sharing.” “Never bed-sharing” was defined as maternal report of the infant never bed-sharing from birth to 2 months of age, while “any bed-sharing” was defined in the study as the mother and infant bed-sharing at least once a month from birth to 2 months of age. Those parents and infants then participated in the Strange Situation Procedure when infants were 14 months of age to assess infant attachment security. Findings revealed that children who never bed-shared were more likely to exhibit an insecure attachment with their mothers as toddlers; however, children who had bed-shared were not significantly more likely to exhibit a secure attachment. These findings suggest that bed-sharing may be protective against insecure attachment, but may not necessarily promote secure attachment.
In the study done by Mileva-Seitz et al. (2016), one possible reason for the weak links between infant sleep location and attachment, a measure of infant affect and behavior within a mother-child interaction, may be the lack of distinction around the context of bed-sharing. In the current study, full bed-sharing is operationalized as bed-sharing in which the mother is observed via video recording as having her infant sleep in the bed with her at the start of the night until the following morning, while partial bed-sharing is defined as bed-sharing that occurs when the mother brings her infant to sleep in the bed over the course of the night, such as in response to infant waking. Bed-sharing throughout the night may reflect different attitudes toward sleep practices and have varying impact compared to those who partially bed-share. For this reason, we suggest that our conceptualization of full and partial bed-sharing may roughly map onto the constructs of proactive and reactive bed-sharing that have been utilized in prior research studies. Proactive bed-sharing is generally defined as purposefully or intentionally choosing to bed-share, while reactive bed-sharing is not planning to bed-share, but doing so in response to infant nighttime needs (Messmer, Miller, & Yu, 2012; Ramos, 2003). Studies suggest that the antecedents and correlates of proactive bed-sharing may differ from those of reactive bed-sharing (Keller & Goldberg, 2004; Madansky & Edelbrock, 1990; Tully et al., 2015). Ultimately, it may be that parents who start off the night bed-sharing with their infants engage differently with their infant or have infants with differential responses to nighttime arrangements, whereas parents who begin bed-sharing later in the night navigate different feelings or child behaviors.
Although no studies have looked specifically at the relation between full and partial bed-sharing and infant affect and behavior within the mother-child relationship, one study examined whether maternal bed-sharing intent (with infants 6–12 months of age) moderated the relation between time spent bed-sharing (measured by hours bed-shared per week) and marital satisfaction (Messmer et al., 2012). Results indicated that mothers who engaged in reactive bed-sharing, defined as mothers who did not plan to bed-share, but bed-shared as a reaction to infant nighttime cues, had lower marital satisfaction as time spent bed-sharing increased. Mothers who engaged in proactive, or “intentional,” bed-sharing, however, showed no change in marital satisfaction as time spent bed-sharing increased. Another study found that reactive bed-sharers, defined as those who co-slept in response to perception of infant sleep problems, were more likely to report dissatisfaction with their sleeping arrangements (Ramos, 2003). Similarly, findings reveal that although proactive and reactive bed-sharing mothers report similar amounts of what they consider to be problematic infant behaviors during the night (e.g., infant difficult to calm during the night), reactive bed-sharing mothers perceive these behaviors as being significantly more problematic than do proactive bed-sharing mothers (Ramos, Youngclarke, & Anderson, 2007). Overall, these studies suggest that reactive bed-sharing may be associated with more perceived problematic infant behaviors and higher maternal stress, while proactive bed-sharing may be associated with less negative maternal states. These differences in maternal states (i.e., maternal perceptions and stress) may affect the way mothers behave towards their infants (Fleming, Ruble, Flett, & Shaul, 1988) – both in terms of what they do and how they feel about it. Thus, it is reasonable to conclude that full and partial bed-sharing may be differentially associated with developing infant social-emotional behavior within the mother-child relationship.
1.2. Still-Face Paradigm and Relationship Quality
To examine the association between mother-infant bed-sharing practices and infant responses within the mother-child relationship, the current study assessed infant behaviors and affect during the Still-Face Paradigm (SFP; Tronick, Als, Adamson, Wise, & Brazelton, 1978). The SFP elicits a range of infant behavior and emotional response, such that infants show increased gaze aversion (i.e., looking away from adults’ face), less positivity (i.e., less smiling), more negativity (i.e., more negative affect), and more self-regulation (i.e., sucking thumb) during the still-face episode (i.e., stressful interaction) than in the normal, or baseline, episode. Previous studies have found that child responses to the SFP (Mesman, van IJzendoorn, & Bakermans-Kranenburg, 2009) are related to the quality of parental caregiving (Tarabulsy et al., 2003) and later attachment quality (Braungart-Rieker, Garwood, Powers, & Wang, 2001). Thus, the current study uses infant responses to the SFP to assess infant emotional and behavioral responses within the dyad.
1.3. Nighttime Contact as Mediating Mechanism
Although emerging evidence suggests a link between bed-sharing and infant affect and behavior within the mother-child dyad, the mechanisms driving this relation are not well understood. Physical contact between the mother and infant is one factor that may contribute to these associations. Studies have shown that bed-sharing infants experience greater physical proximity and touch from their parents during the night than infants that do not bed-share (Baddock, Galland, Bolton, Williams, & Taylor, 2006; Buckley, Rigda, Mundy, & McMillen, 2002). Physical touch (e.g., skin-to-skin contact) and proximity of the mother is believed to provide emotional security and physical comfort to the infant (Germo, Chang, Keller, & Goldberg, 2007; McKenna & Volpe, 2007), which may explain why mother-infant physical contact has been shown to relieve infant distress and promote positive infant affect and behavior within the mother-child relationship (Feldman, Weller, Sirota, & Eidelman, 2003). Indeed, extensive parent-infant skin-to-skin contact may be considered the biological norm, as it has also been found to promote child self-regulation and parental sensitivity (Braungart-Rieker et al., 2001; Feldman, 2004; Feldman et al., 2003). The term ‘breastsleeping’ has been offered to draw attention to the deeply interconnected nature of dyadic sleep, feeding, and contact (McKenna & Gettler, 2016). Ultimately, behaviors within bed-sharing, such as the amount and degree of mother-infant contact, differ (Volpe, Ball, & McKenna, 2013); thus, the extent of contact between mother and infant during the night may promote the associations hypothesized in the current study. This is the first study to investigate the potential for nighttime maternal-infant physical contact as a mediating mechanism.
1.4. Current Study
The current study examines the links between mother-infant bed-sharing practices (i.e., full bed-sharing [FBS]; partial bed-sharing [PBS]; non-bed-sharing [NBS]) and child affect and behavior during the SFP. This study adds to the existing literature in several ways. First, the only existing study to investigate the relation between infant sleep location and attachment, a marker of infant affect and behavior, was limited by its use of questionnaires for determining infant sleep location (Mileva-Sietz et al., 2016). The current study extends the literature by using naturalistic observational methods to assess the relation between mother-infant bed-sharing practices and infant affect and behavior within the mother-child relationship; parent-infant sleep was documented by extensive video recording in participant homes as part of a larger study on biobehavioral contributors to infant sleep development. Second, the current study goes beyond considering the presence of bed-sharing and attempts to disentangle the relation between the extent of bed-sharing (i.e., FBS versus PBS) and infant emotion and behavior within the mother-child dyad, a distinction that has not been considered previously. Third, we explore mother-infant contact as a possible mechanism by which nighttime infant bed-sharing may predict later infant affect and behavior. Fourth, this study uses coded SFP data. This permitted infant affect and behavior within the mother-child dyad to be measured earlier in infant development than most studies, which are conducted at the end of the first year using the Strange Situation paradigm. Finally, our sample is comprised exclusively of African American mother-infant dyads. African Americans are at greater risk for poor sleep quality (Durrence & Lichstein, 2006) and are more likely to engage in bed-sharing (Colson et al., 2013). The current study is the first to examine these relations within an African American sample.
We hypothesized that observations of mother-infant bed-sharing practices at 3 months would be related to infant affect and behavior within the mother-infant dyadic relationship at 6 months, with bed-sharing dyads displaying more infant positivity, less negativity, more gaze towards mother, and more self-regulatory behaviors during the SFP than non-bed-sharing dyads (i.e., those who room-shared or slept in separate rooms). We expected that these relationships would particularly hold true for full bed-sharing dyads. Finally, we hypothesized that observed nighttime mother-infant physical contact would mediate any significant relationships between mother-infant bed-sharing practices and infant responses to the SFP.
2. Methods
2.1. Participants
The current study includes 63 African American mother-infant dyads who participated in a larger study of sleep development over the first year of life, which included in-home assessments when the infants were 3 (M = 3.63 months; SD = .54) and 6 months of age (M = 6.47 months; SD = .45). Using public birth records and community advertisements, researchers recruited African American mothers in the Triangle area of North Carolinawho were 18 years of age or older and gave birth to a single infant over the course of a two-year period.
Of the infants included in this study, 34 were male and 29 were female. The majority (89%) of infants were born at term (i.e., 37+0 gestational weeks or later). For infants born prior to 37 gestational weeks (n = 5; range = 32 + 5 to 35 + 5 weeks), both the 3 and 6 month visits were scheduled according to infants’ adjusted age. A minority (33%) of mothers in the sample had completed a 4-year college degree. About half (57%) of infants lived in the same household as their biological father. At 3 months of age, 51% of infants were breastfed, either partially or exclusively.
2.2. Procedure
Data were collected during home visits when infants were 3 and 6 months of age by trained research assistants. After consent procedures, multiple research activities were conducted, including video observation of a range of mother-child interactions. Mothers also completed questionnaires at both of these study time points which focused on demographic information, maternal health and well-being, and infant behavior and development, including sleep-related behaviors. Although both visits followed similar procedures, the SFP was done only at the 6 month visit, and was videotaped for offline coding.
At the end of each home visit, research assistants set up four infrared, high-definition, color Hikvision (DS-2CD2432F-IW) cameras with internal microphones to record the infant’s sleep and parent-infant nighttime interactions for one full night. Research assistants asked the mother to describe the infant’s general sleep location(s) as well as any other areas where the mother and child were likely to spend time together during the observation period. Based on this information, up to 4 cameras with night-shot capacity were set up in the designated location(s) to record mother-child interaction at bedtime and throughout the night, as well as the infant’s sleep. At least one camera was set up directly above the infant’s primary sleep location. Each of these cameras were connected to an Exacq (IPS04–1000-LC) video surveillance recorder via Power over Ethernet (PoE) ports of a NETGEAR ProSafe Plus (GS108PE) switch. Ethernet cables were secured to the floor and furniture for safety. Research assistants instructed caregivers to turn on the video equipment at 6:30pm and allow the equipment to record throughout the night; research assistants then retrieved the video equipment the following morning. Data were downloaded off the video recorder using ExacqVision Client software (version 8.4) and stored on encrypted external hard drives in secure university offices for later video coding.
Beginning the day after the home visit, mothers completed brief infant sleep diaries (Hall, Liva, Moynihan, & Saunders, 2015) over the phone with a research assistant every day for the course of a week. These sleep diaries included questions regarding the mothers’ breastfeeding practices and the infant’s sleep location and behavior during the previous night. Upon completion of each data collection time point, mothers received compensation via gift cards. All study protocols were approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
2.3. Measures
2.3.1. Videosomnography.
Sleep practices were assessed at 3 months using naturalistic video observation. Nighttime sleep practices were coded over the entire night, using a coding scheme adapted from Philbrook and Teti (2016) and Tully and Ball (2012). Coding began when the infant fell asleep for the night, which was defined as the moment that the infant laid still with closed eyes and remained that way for at least 5 minutes. Coding ended when the infant woke up the next morning, which was defined as the moment the infant’s eyes were open and the infant remained awake for at least 5 minutes. When infants’ bedtime was indeterminant due to video camera angles, the video was coded beginning at the first interval after 6:30pm when the infant met study criteria for being asleep (e.g., closed eyes, still for 5 consecutive minutes). Similarly, mothers where given instructions to turn off the video equipment when the infant woke up the next morning, but in some cases filming concluded before the infant woke up (e.g., researchers retrieved equipment or parents moved infant off camera before infant woke up). These events were rare (n = 8 of 63 cases) and always occurred in the morning hours (e.g., between 7AM and 9AM). In such instances, the infants’ wake time was considered to be the last interval where they appeared on camera.
Aspects of the infant’s sleep environment (e.g., location, surface) and certain parental behaviors (e.g., feeding, contact) were coded in 30-second intervals throughout the nighttime interval. To achieve reliability, two research assistants held weekly meetings over the course of training and coding to conference cases and discuss discrepancies. Twelve cases (19.35%) were double coded and inter-rater agreement was high, with Cohen’s kappa values above .80 for all codes.
2.3.1.1. Mother-infant bed-sharing practices.
Mother-infant bed-sharing practices were determined using video recordings that revealed the room the infant was in during the night (own room, shared bedroom with a sibling, shared bedroom with parent/s, or solitary room) and the infants’ sleep surface (attached crib, bedside crib, standalone crib, family bed, car seat, swing, or parent’s arms). Pertinent to the current investigation, bed-sharing was coded when the infant was asleep with an adult in the same bed or another shared surface (e.g., chair, couch), regardless of adult sleep status. It was no longer considered bed-sharing when shared surface was discontinued (i.e., mother got out of bed) or if the infant woke up.
On the basis of this nighttime coding, three infant bed-sharing groups were created. Infants were categorized as full bed-sharers (FBS) when the mother and infant were observed sleeping on a shared sleep surface from the start of the night through the following morning. Infants were considered to be partial bed-sharers (PBS) when the mother and infant were observed sleeping on a shared sleep surface beginning later in the night, reflecting movement from another infant sleep location to a shared surface during the night. Finally, infants were categorized as non-bed-sharers (NBS) if they were observed sleeping on their own sleep surface (i.e., crib) throughout the night or if they room-shared but were never observed bed-sharing during the night. There were two infants who fell asleep at the beginning of the nighttime interval while the mother was nursing in a bed. Although they were coded as bed-sharing for the few minutes before the mother put them down, the infants then remained on their own sleep surface for the duration of the night. Therefore, they were grouped in the non-bed-sharing group.
Given that only one night of videosomnography data was available, we used infant sleep diaries to check whether each infant’s bed-sharing categorization represented their typical sleep location. For each night over the course of a week, mothers responded to the question “Where did your baby sleep in the night?” Eighty-six percent of infants had sleep diaries indicating that the majority of nights were spent sleeping in the location observed on video (e.g., in solitary location or in parents’ bed). The remaining 14% of infants who had mismatched classifications were all observed to be partial bed-sharers, but sleep diaries indicated that infants typically did not bed-share. It is likely that these infants only bed-shared for a brief period, and thus, mothers did not report bed-sharing consistently on the sleep diaries. However, overall, there was a high level of agreement between sleep diaries and videosomnography, indicating that the majority of infants were observed sleeping in their typical sleep arrangements.
2.3.1.2. Contact.
Close and casual physical contact between the mother and infant was coded. Close contact was defined as the mother holding the infant on or next to her body, whether the infant was facing towards or away from the mother’s body (e.g., holding, cuddling, breastfeeding). Casual contact was defined as the mother and infant touching, but not closely (e.g., caressing, diaper changing, infant sitting on mother’s lap with little contact between bodies). These codes were mutually exclusive; if close and casual contact were present in an interval, close contact was coded. Proportion scores for both close and casual contact were calculated by dividing the number of intervals of target behavior by the total number of coded intervals.
2.3.2. Still-Face Paradigm (SFP).
Child affect and behavior within the mother-child dyad was assessed using the SFP. Mothers placed infants in a car seat on the floor and sat on the floor directly in front of the infant. Mothers were instructed on the three episodes of the SFP (e.g., normal, still-face, reunion), each of which were 2 minutes long (Mesman et al., 2009). During the normal episode, mothers were instructed to interact with their infants as they normally would. For the still-face episode, mothers were instructed to turn away from their infant for 15 seconds and then look back at their infant with a completely expressionless face. During this time, mothers were told not to respond to their infants in any way (e.g., smile, touch). In the reunion episode, mothers were told to turn away from their infant for 15 seconds and then turn back and resume normal interaction. Although each episode is intended to be 2 minutes long, the still-face episode was cut short if the infant cried hard for 15 seconds or more. Thus, due to the varied length of each SFP video, coded child behaviors were transformed into proportion scores that took into account the duration of each episode.
Researchers coded each of the three episodes in 5-second intervals. For each interval, the presence of infant affective expressions, vocalizations, gaze, and self-regulatory behaviors were coded. To achieve reliability, two research assistants trained with a master coder prior to the onset of coding to establish inter-rater reliability and met weekly to discuss discrepancies. Agreement was quantified using Cohen’s kappa, with coder reliability values all above .70. The still-face and reunion episodes require the infant to cope with the disruption of social engagement and repair the interaction; thus, these episodes provide a good context to assess infant ability to self-regulate and maintain positive affect during a time of stress. For this reason, the current study only considers these two episodes.
2.3.2.1. Affective expression.
For each phase of the SFP, infant negative and positive affect were coded. Negative affect was coded as present if the infant displayed a negative expression, characterized by sharply lowered brows, tightly closed eyes, or downward turned corners of the mouth. Positive affect was coded as present if the infant displayed a positive expression, characterized by raised corners of the mouth, raised cheeks, a wide mouth, a surprised expression, or a playful expression. If positive and negative facial expressions were present simultaneously (e.g., brows drawn together, but corners of mouth raised), negative affect was coded. If distinct positive and negative affective expressions were both present in the same interval, then the affect present for the majority of the interval was coded.
2.3.2.2. Vocalizations.
All episodes that included any negative vocalizations were coded as negative, including fussing, crying, screaming, and other expressions of mild fussiness (e.g., grunt). Negative affective expression and vocalizations during the still-face episodes were positively correlated (r = .85) and negative affective expression and vocalizations during the reunion episodes were positively correlated (r = .93). To capture infants’ level of negativity, z-scores were created for negative affective expressions (described in section 2.3.2.1) and negative vocalizations and averaged together to create a total composite of infant negativity.
2.3.2.3. Gaze.
Infant gaze was coded if the infant was looking toward the mother, meaning that the infant was gazing above the mother’s neck. Toward mother was the default code; thus, when the infants’ head was directed towards the mothers’ face, but it was unclear if the infants’ eyes were open or closed, towards caregiver was coded. Researchers also coded gaze toward mother if the infant gazed towards the mother, but closed his or her eyes for some duration of the interval. Gazing away from the mother was coded if the infant’s eyes were closed for the whole interval, if the infant was not looking at the mother at all, or if the infant was looking down at the mother’s hands or clothing.
2.3.2.4. Self-regulation.
Self-regulation was defined as any action an infant took to soothe him or herself or direct his or her attention away from stress or discomfort. Self-regulatory behaviors could include deliberate behavior by the infant, such as sucking on a body part (e.g., thumb), sucking on an object (e.g., chair strap), auto-manipulation (e.g., tonguing, lip-smacking), and manual manipulation (e.g., hand wringing, playing with foot). Self-regulation was coded during the reunion episode if the infant used his or her mother to self-regulate (e.g., grabbing her hand); however, self-regulation was not coded if the mother initiated the contact. Behaviors such as banging, stroking, tapping, and patting were not coded unless they were in evidence at least two times during an interval, indicating a more purposeful response pattern.
2.3.3. Covariates.
Consistent with previous research regarding bed-sharing and mother and child factors, the current study retained maternal education, infant gender, and breastfeeding status as covariates (Blair & Ball, 2004; Blair, Heron, & Fleming, 2010; Colson et al., 2013). Infant prematurity and infant negative temperament were also retained as covariates given their known associations with infant affect and behavior during the still-face paradigm (Montirosso, Borgatti, Trojan, Zanini, & Tronick, 2010; Yoo & Reeb-Sutherland, 2013). Maternal education and child gender were reported by the mother through questionnaires during the 3 month visit. Breastfeeding was determined through video observation and sleep diaries. For each night over the course of a week, mothers responded to the question “Did your infant feed in the night? If so, what did he or she have?” If mothers reported breastfeeding on the sleep diaries or were observed breastfeeding at any time during the nighttime video, they were categorized as breastfeeding. If the mother was not observed breastfeeding during the nighttime video and the mother reported formula feeding for all nights of the sleep diaries, then infants were categorized as not breastfeeding. In cases where breastfeeding was not observed and mothers had missing feeding information for any night of the sleep diaries, breastfeeding was coded as missing. Given that infants are more likely to be breastfed earlier in life, we controlled for breastfeeding at 3 months (as opposed to 6 months) to capture whether infants had ever been breastfed.
Infant gestational age (GA) was calculated from maternal report of her infant’s due date and birth date and used to categorize whether infants were premature (GA < 37 weeks) or not. Given that prematurity status can play a role in infants’ SFP outcomes (Montirosso et al., 2010), maternal psychological distress and mother-infant interactions (Gondwe, White-Traut, Brandon, Pan, & Holdistch-Davis, 2017), the current study controlled for infant prematurity. Prior research also suggests that negative reactivity can influence SFP behaviors (Yoo & Reeb-Sutherland, 2013); thus, we included infant negative temperament at 3 and 6 months as covariates, as measured by the Very Short Form of the Infant Behavioral Questionnaire-Revised (IBQ-R; Putnam, Helbig, Gartstein, Rothbart, & Leerkes, 2014). The IBQ-R negative emotionality subscale consisted of 12-items and included questions such as, “When tired, how often did your baby show distress?” and “After sleeping, how often did the baby cry if someone doesn’t come within a few minutes?” Mothers rated the frequency in which infants engaged in these behaviors on a scale from 1 (never) to 7 (always). This subscale had adequate internal consistency at both 3 months (α = .75) and 6 months (α = .81).
Additionally, mother-infant bed-sharing at 6 months was included as a covariate because many changes can occur within the bed-sharing arrangement between 3 and 6 months of age. By controlling for concurrent bed-sharing practices (i.e., at 6 months), our analyses tested the hypothesis that 3 month bed-sharing contributes to 6 month infant outcomes, above and beyond concurrent bed-sharing status. Concurrent bed-sharing practices were measured through mothers’ self-report on the sleep diaries, described earlier. Specifically, over the course of a week mothers reported where their infants slept each night (e.g., parents’ bed, own bed). We calculated the proportion of bed-sharing each dyad engaged in over the course of the week. Those that bed-shared for the majority of the nights were categorized as bed-sharers. Those who did not bed-share at all or did not bed-share for the majority of the nights were categorized as non-bed-sharers.
2.3.4. Missing data.
There were 66 mother-infant pairs that had both nighttime and SFP data. Three cases were excluded from this analysis because the infant was taken off camera for an extended period of time (> 2 hours) during the nighttime observation. As a result, it could not be determined whether the infant bed-shared for all or part of the off-camera period. Therefore, 63 infants could be grouped as FBS, PBS, or NBS and were included in analyses.
Dyads had to complete at least one episode of the SFP to be included in this study. Protocol required that research assistants stop filming the SFP if the infant cried for more than 15 seconds. For this reason, and due to unexpected problems with camera equipment or filming angles, there are some missing data for the SFP variables, particularly for the reunion episode. Among the 63 infants in the study, 8% (n = 5) were missing positive affective expression during the reunion, 11% (n = 7) were missing gaze during the reunion, 13% (n = 8) were missing self-regulation during the reunion, and 8% (n = 5) were missing negativity during the reunion. A chi-square test revealed that missing data was evenly distributed among bed-sharing and non-bed-sharing dyads, χ2(1) = 1.40, p = .237.
Considering that infants with missing data in every SFP reunion variable (10%) may be the infants exhibiting more negative behaviors (e.g., those for whom the paradigm was terminated early due to sustained crying), analyses were conducted to test group differences between infants missing all SFP reunion variables and infants with SFP reunion variables. Analyses revealed that infants with missing data did not differ from infants with complete data in terms of gender, term, breastfeeding, maternal education, or temperamental negativity. Given the presence of missing data, we used the robust maximum likelihood (MLR) estimator for all analyses. This technique is considered appropriate when data are missing at random, a tenable assumption in the current study. Additionally, MLR was used because it is distributionally robust and allows for possible non-normality in the errors of the model (MacKinnon, Lockwood, & Williams, 2004).
2.3.5. Analysis Plan.
The goal of this study was to examine the associations between mother-infant bed-sharing practices (i.e., full, partial, or none) and infant affect and behavior within a mother-child interaction, as measured by the SFP. Given that full and partial bed-sharing were not significantly related to any of the SFP outcome variables during the normal episode (with the exception of positive affective expression for partial bed-sharers), the current study only considers the still-face and reunion episodes. To investigate the relation between mother-infant bed-sharing and SFP responses, we conducted regression analyses, all of which controlled for breastfeeding at 3 months, negativity at 3 and 6 months (as measured by the IBQ-R), infant gender, infant prematurity, maternal education, and 6 month bed-sharing practices. To examine differences in SFP responses based on mother-infant bed-sharing practices at 3 months, we entered two dichotomous variables (FBS and PBS) into the regression analyses, such that NBS infants represented the reference group. For any significant associations between bed-sharing and infant outcomes, we tested the mediating mechanisms of nighttime mother-infant close and casual contact using path analysis. Descriptive statistics were conducted using SPSS 24.0 and regression and path analyses were conducted in Mplus (Muthén & Muthén, 2017). Indirect effects were tested in Mplus using bias-corrected bootstrapped confidence intervals (MacKinnon et al., 2004).
3. Results
3.1. Descriptive Statistics and Correlations
First, we examined whether there were demographic differences between NBS infants (n = 23), FBS infants (n = 20), and PBS infants (n = 20). Chi-square tests did not reveal any significant demographic differences; however, breastfeeding at 3 months, maternal education, infant prematurity, and infant gender were retained as covariates due to their known associations with either bed-sharing or SFP outcomes (Blair & Ball, 2004; Blair et al., 2010; Colson et al., 2013; Montirosso et al., 2010). Similarly, an ANOVA did not reveal any significant group differences in negativity at 3 or 6 months, but due to their known associations with SFP outcomes (Yoo & Reeb-Sutherland, 2013) they were retained as covariates. Finally, FBS and PBS infants were more likely to bed-share at 6 months (χ2 (2) = 20.89, p < .001), justifying the inclusion of 6 month bed-sharing status as an additional covariate.
Descriptive statistics for all study variables appear in Table 1. Positive affect during the still-face and reunion episodes was similar for FBS, PBS, and NBS infants. FBS (M = −.14) and PBS (M = .10) infants displayed less negativity during the still-face episode, compared to NBS infants (M = .21). A similar pattern was observed during the reunion episode, in which FBS infants (M = −.37) and PBS infants (M = −.17) had less negativity in comparison to NBS infants (M = .40). Gaze towards mother was similar across groups during the still-face episode, but was highest for PBS infants (M = .62) during the reunion episode, in comparison to FBS (M = .51) and NBS (M = .40) infants. Finally, FBS (M = .66) and PBS (M = .61) infants displayed greater self-regulation during the still-face episode when compared to NBS infants (M = .37), although self-regulation was similar across groups during the reunion episode. Concerning mother-infant contact during the nighttime, our proposed mediator variable, FBS dyads exhibited the most close (M = .31) and casual (M = .19) contact, compared to either PBS (close: M = .21; casual: M = .12) or NBS (close: M = .02; casual: M = .01) dyads.
Table 1.
Descriptive Statistics by Mother-Infant Bed-Sharing Practices
| Total Sample (N = 63) | Full (n = 20) | Partial (n = 20) | None (n = 23) | |||||
|---|---|---|---|---|---|---|---|---|
| M/% | SD | M/% | SD | M/% | SD | M/% | SD | |
| Demographics | ||||||||
| 1. Bed-Sharing, 6mo | .50 | - | .80 | - | .61 | - | .10 | - |
| 2. Gender, male | .54 | - | .45 | - | .60 | - | .57 | - |
| 3. Breastfeeding, 3mo | .51 | - | .58 | - | .58 | - | .37 | - |
| 4. Maternal Education | .34 | - | .30 | - | .35 | - | .38 | - |
| 5. Term, full | .92 | - | .85 | - | 1.00 | - | .91 | - |
| 6. Negativity, 3mo | 4.33 | 0.96 | 4.15 | 1.02 | 3.76 | 0.87 | 4.18 | 0.98 |
| 7. Negativity, 6mo | 4.29 | 0.92 | 4.52 | 0.87 | 4.11 | 1.00 | 4.25 | 0.88 |
| Still-Face Episode | ||||||||
| 1. Positive Affect | .05 | .08 | .05 | .08 | .05 | .08 | .05 | .09 |
| 2. Negativity | .00 | .96 | −.14 | 1.00 | −.10 | .97 | .21 | .92 |
| 3. Gaze | .33 | .28 | .39 | .31 | .33 | .28 | .29 | .27 |
| 4. Self-Regulation | .54 | .29 | .66 | .28 | .61 | .26 | .37 | .26 |
| Reunion Episode | ||||||||
| 1. Positive Affect | .13 | .24 | .18 | .29 | .15 | .24 | .09 | .21 |
| 2. Negativity | −.02 | .97 | −.37 | .91 | −.17 | .90 | .40 | .98 |
| 3. Gaze | .51 | .30 | .51 | .27 | .62 | .27 | .40 | .34 |
| 4. Self-Regulation | .30 | .32 | .27 | .31 | .35 | .31 | .27 | .34 |
| Mediators | ||||||||
| 1. Close Contact | .17 | .23 | .31 | .28 | .21 | .19 | .02 | .04 |
| 2. Casual Contact | .10 | .16 | .19 | .20 | .12 | .16 | .01 | .01 |
Note. Values are M for continuous variables and % for categorical variables. All negativity variables are z-scores.
Bivariate correlations between all study variables can be seen in Table 2. FBS was significantly correlated with infant self-regulation during the still-face episode (r = .29, p = .02), while PBS was significantly related to infant gaze towards mother during the reunion episode (r = .27, p = .04). Further, FBS was positively correlated with mother-infant close contact (r = .43, p < .001) and casual contact (r = .37, p < .001).
Table 2.
Correlations among Major Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Full Bed-Sharing, 3mo | — | −.47** | .44** | −.12 | .10 | −.07 | −.17 | .08 | .17 | .43** | .37** | .02 | .12 | −.10 | −.24 | .16 | .02 | .29* | −.05 |
| 2. Partial Bed-Sharing, 3mo | — | .15 | .08 | .10 | .01 | .20 | −.20 | −.14 | .10 | .08 | .02 | .03 | −.07 | −.10 | −.06 | .27* | .17 | .13 | |
| 3. Bed-Sharing, 6mo | .04 | .23 | −.12 | .07 | −.08 | .06 | .28* | .44** | .01 | .24 | −.18 | −.29* | −.04 | .19 | .27* | .06 | |||
| 4. Gender = Male | — | −.09 | .07 | −.15 | −.30* | −.08 | .01 | −.06 | .11 | .10 | −.07 | −.24 | .04 | −.03 | .04 | .05 | |||
| 5. Breastfed, 3mo | — | .41* | −.06 | .06 | .06 | .24 | .02 | .09 | .02 | −.28* | −.19 | −.08 | .00 | .03 | .13 | ||||
| 6. College degree | — | .10 | −.04 | .05 | −.05 | −.16 | .00 | .00 | .04 | −.00 | .12 | .11 | −.14 | .10 | |||||
| 7. Term, full | — | .06 | .15 | −.29* | .09 | −.11 | .07 | −.07 | −.09 | −.24 | .16 | −.01 | .07 | ||||||
| 8. Negativity, 3mo | — | .52** | .07 | .03 | .03 | .12 | −.02 | .10 | −.14 | −.20 | .02 | −.11 | |||||||
| 9. Negativity, 6mo | — | .14 | .10 | −.06 | .15 | .13 | −.05 | −.08 | .08 | .14 | −.04 | ||||||||
| 10. Close Contact | — | .14 | .06 | .05 | −.10 | −.22 | .04 | .03 | .28* | .00 | |||||||||
| 11. Casual Contact | — | .03 | .07 | .09 | −.04 | .02 | .12 | .22 | .03 | ||||||||||
| 12. Positive Affect (SF) | — | .55** | −.39* | −.46** | .05 | .15 | −.05 | .17 | |||||||||||
| 13. Positive Affect (R) | — | −.39* | −.53** | .05 | .19 | .08 | .16 | ||||||||||||
| 14. Negativity (SF) | — | .73** | .22 | .02 | −.28* | −.29* | |||||||||||||
| 15. Negativity (R) | — | .05 | −.36* | −.22 | −.23 | ||||||||||||||
| 16. Gaze (SF) | — | .41* | −.01 | .19 | |||||||||||||||
| 17. Gaze (R) | — | .04 | .26 | ||||||||||||||||
| 18. Self-Regulation (SF) | — | .51** | |||||||||||||||||
| 19. Self-Regulation (R) | — |
Note. SF = still-face episode; R = reunion episode, mo = months.
p < .05.
p < .01.
3.2. Mother-Infant Bed-Sharing Practices and Associations with SFP Outcomes
Results from all regression models are displayed in Table 3. Results indicated no significant relations between bed-sharing groups and positive affect during either SFP episode. In comparison to NBS, FBS was negatively related to infant negativity during the reunion episode (β = −.39, p = .02), whereas PBS was not related to negativity in either episode. The relation between FBS and gaze towards mother during the still-face episode of the SFP was trending toward significance (β = .28, p = .08), and the relation between PBS and gaze towards mother during the reunion episode similarly approached significance (β = .29, p = .06). Finally, FBS (β = .45, p = .01) and PBS (β = .38, p =.01) were both positively associated with self-regulation during the still-face episode. This suggests that both FBS and PBS infants displayed greater self-regulation during the still-face episode, compared to NBS infants.
Table 3.
Regression Analyses for Mother-Infant Bed-Sharing Practices Predicting SFP Responses
| Positive Affect | Negativity | Gaze | Self-Regulation | |||||
|---|---|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | β | SE | |
| Still-Face Episode | ||||||||
| 1. Full | .05 | .15 | −.18 | .14 | −28† | .16 | .45* | .16 |
| 2. Partial | .05 | .16 | −.06 | .14 | .15 | .15 | .38* | .16 |
| 3. Bed-Sharing, 6mo | −.02 | .14 | .00 | .13 | −.10 | .14 | −.01 | .15 |
| 4. Gender | .14 | .14 | −.17 | .13 | −.05 | .14 | .09 | .12 |
| 5. Breastfeeding, 3mo | .10 | .13 | −.31* | .14 | −.23 | .14 | .04 | .14 |
| 6. Maternal Education | −.04 | .14 | .16 | .12 | .24† | .13 | −.15 | .13 |
| 7. Term | −.07 | .12 | −.18 | .10 | −.25 | .10 | .00 | .08 |
| 8. Negativity, 3mo | .14 | .16 | −.16 | .14 | −.13 | .15 | .02 | .13 |
| 9. Negativity, 6mo | −.12 | .12 | .26 | .13 | .00 | .16 | .12 | .12 |
| Reunion Episode | ||||||||
| 1. Full | .10 | .18 | −.39* | .17 | .11 | .17 | −.08 | .21 |
| 2. Partial | .07 | .14 | −.23 | .15 | .29† | .16 | .03 | .18 |
| 3. Bed-Sharing, 6mo | .18 | .13 | .04 | .16 | .11 | .15 | .04 | .17 |
| 4. Gender | .15 | .11 | −.30* | .12 | −.09 | .13 | .05 | .16 |
| 5. Breastfeeding, 3mo | −.04 | .19 | −.18 | .14 | −.15 | .14 | .20 | .18 |
| 6. Maternal Education | .01 | .19 | .08 | .13 | .17 | .15 | −.01 | .14 |
| 7. Term | .05 | .10 | −.17 | .11 | .05 | .09 | .06 | .11 |
| 8. Negativity, 3mo | .17 | .13 | .05 | .14 | −.28† | .15 | −.11 | .19 |
| 9. Negativity, 6mo | .06 | .13 | −.05 | .15 | .25 | .16 | −.01 | .16 |
Note. Eight regression models are represented, each of which controlled for gender, prematurity, bed-sharing practices at 6 months, breastfeeding at 3 months, negativity at 3 and 6 months, and maternal education. Regressions were conducted using the 3 month mother-infant bed-sharing practices (full and partial bed-sharing; with non-bed-sharing as the reference group).
p < .10.
p < .05.
p < .001.
3.3. Mediation
To understand possible mechanisms that may explain significant relations between bed-sharing practices and infant SFP outcomes, we examined the mediating role of mother-infant close and casual contact during the night. Only significant regressions were considered; thus, the model retained self-regulation during the still-face episode and negativity during the reunion episode as outcomes. All covariates were included as predictors of the mediators (i.e., close and casual contact at 3 months) and SFP outcomes, with the exception of 6 month bed-sharing and 6 month infant temperament, which were only included as predictors of 6 month SFP outcomes to maintain temporal order. Due to this parameterization, our mediation model was not fully saturated. From available model fit statistics, we found that the model fit the data well: χ2 (4) = 4.68, p = .32, CFI = .99, RMSEA = .05.
There were several statistically significant direct paths between predictor and criterion variables (see Figure 1). Of primary interest, FBS (β = .56, p < .001) and PBS (β = .42, p < .001) were positively associated with mother-infant close contact. Similarly, FBS (β = .52, p < .001) and PBS (β = .30, p = .007) were positively associated with mother-infant casual contact. However, neither close nor casual contact predicted any infant SFP outcomes. Additionally, no significant indirect effects were found. These results suggest that, while FBS and PBS are associated with more mother-infant close and casual contact during the night, neither type of contact mediates the relations between bed-sharing practices and SFP outcomes.
Figure 1.
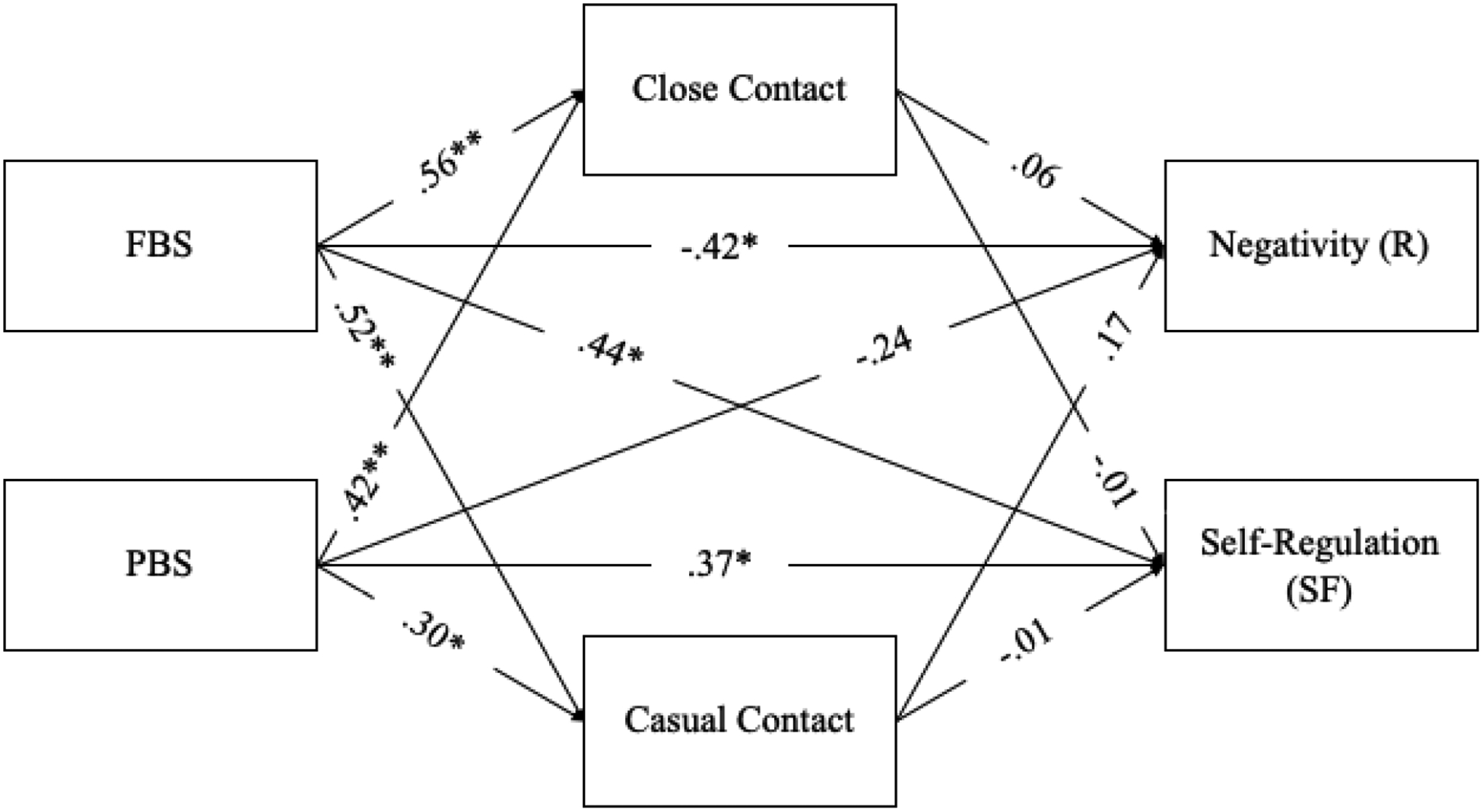
Mediational model of bed-sharing practices predicting SFP outcomes through close and casual contact. Paths show standardized regression coefficients. Model controlled for gender, breastfeeding at 3 months, concurrent bed-sharing practices, infant prematurity, negativity at 3 and 6 months, and maternal education.
*p < .05. **p < .001.
4. Discussion
This study examined the associations between mother-infant bed-sharing practices and infant affect and behavior within the mother-child relationship, as indexed by infant responses to the SFP, among African-American mother-infant dyads. Analyses revealed that infants who bed-shared with their mothers at 3 months (i.e., FBS and PBS) displayed significantly more self-regulatory behaviors during the still-face episode of the SFP at 6 months than NBS infants, including when accounting for bed-sharing at 6 months. Additionally, FBS infants displayed significantly less negativity during the reunion episode of the SFP than NBS infants. Similarly, FBS infants displayed a trend toward greater gaze towards mother during the still-face episode of the SFP than NBS infants, while PBS infants showed a trend toward greater gaze towards mother during the reunion episode of the SFP. According to these results, FBS and PBS infants show different patterns of behavior during the SFP than NBS infants. Concerning potential mechanisms, mediation analyses indicated that mother-infant contact during the night did not mediate the relationship between bed-sharing and SFP outcomes. Thus, the amount of nighttime maternal-infant contact does not explain the relations between mother-infant bed-sharing practices and infant affect and behavior during the SFP.
4.1. Mother-Infant Bed-Sharing Practices and SFP Responses
In the current study, we hypothesized that mother-infant bed-sharing practices at 3 months would predict infant affect and behavior within the mother-infant dyad at 6 months, as indexed by infant responses during the SFP. Specifically, we hypothesized that bed-sharing infants, particularly FBS infants, would have less negativity, more positivity, more gaze towards mother, and more self-regulatory behaviors than NBS infants. As expected, both FBS and PBS infants displayed more self-regulation during the SFP than NBS infants. The association between bed-sharing and self-regulatory behaviors during the still-face episode indicates that children who share a bed with their mothers during the night, regardless of the amount of time spent bed-sharing, are able to regulate their emotions more during distressing situations. Further, FBS infants displayed less negativity during the reunion episode than NBS infants. Due to the greater nighttime maternal proximity, contact, and responsiveness associated with bed-sharing (Braungart-Rieker et al., 2001; Feldman, 2004), bed-sharing infants (in comparison to NBS infants) may have had more opportunities for their mother to serve as a resource for external regulation, which in turn may have impacted the infants’ capacity to manage their feelings and emotions. Ultimately, bed-sharing may lead to better infant self-regulation during the still-face episode, and thus, less negativity during the reunion episode, particularly for FBS infants.
Moreover, FBS infants displayed a trend toward greater gaze towards mother during the still-face episode in comparison to NBS infants, while PBS infants displayed a trend toward greater gaze towards mother during the reunion episode in comparison to NBS infants. If replicated, these differences may suggest variability in infants’ ability to use social orienting based on their prior bed-sharing experiences (Wagner et al., 2016). Given that bed-sharing infants have increased access to their mother during the night, there may be interactions occurring that facilitate these emerging abilities. However, these results remain to be confirmed in future studies.
The only other study to look at the relation between infant sleep location and a measure of infant affect and behavior within the mother-child relationship (i.e., attachment) found a relation between “never bed-sharing” infants (i.e., never bed-shared from birth to 2 months) and an insecure attachment; however, the study did not find any association between “any bed-sharing” dyads (i.e., bed-sharing at least once a month from birth to 2 months) and a secure attachment (Mileva-Seitz et al., 2016). The current study, however, found that bed-sharing was related to positive outcomes (e.g., infant self-regulation). The use of self-report data by Mileva-Seitz and colleagues (2016) may have been a limitation because mothers can be biased or inaccurate in reports of nighttime interactions, as we have documented (Camerota, Tully, Grimes, Gueron-Sela, & Propper, 2018). Thus, categorizing infants as FBS, PBS, or NBS based on observable data enabled accurate and precise sleep arrangement classification. Moreover, the current study assessed infant affect and behavior within the mother-child relationship at 6 months using the SFP, while the study done by Mileva-Seitz et al. (2016) assessed infant attachment at 15 months using the Strange Situation. Although these two outcome variables are related and assess infant affect and behavior within a mother-child interaction, they have different definitions and are not necessarily the same. Thus, the discrepancies in study methods and outcome variables may account for the differing findings between the current study and previous literature.
4.2. Nighttime Contact as a Mediator
Further, the current study investigated whether mother-infant close and casual contact during the night could be driving the relations found in this study. Contrary to our hypothesis, neither close nor casual contact mediated the relation between FBS and self-regulation during the still-face episode, FBS and negativity during the reunion episode, or PBS and self-regulation during the still-face episode. Although no mediation was present, bed-sharing, including both FBS and PBS, was associated with greater levels of close and casual contact during the night. This finding was consistent with previous literature, which showed that bed-sharing infants spend a larger amount of time during the night in close physical contact with their parents (Buckley et al., 2002) and experience more touch from their parents during the night than nonbed-sharing infants (Baddock et al., 2006). Although engaging in a large degree of contact during the night at this young age is believed to provide emotional and physical comfort to the infant (Germo et al., 2007; McKenna & Volpe, 2007), observed nighttime contact was not associated with outcomes measured in the current study. It is possible that mother-infant contact may be important for different facets of infant socioemotional outcomes, measured using alternative paradigms. Thus, future studies might consider other measures of infant affect and behavior within the mother-child relationship. It is also possible that attitudes about parenting may underlie the associations between mother-infant bed-sharing practices and infant affect and behavior during the SFP. For instance, maternal closeness at night may reflect a norm of more sensitive and responsive parenting. Thus, it may not be nighttime contact that drives these associations, but rather attitudes about parenting that may include particular sleep arrangements.
4.3. Limitations and Future Directions
The current study was limited by several factors. First, our small sample size may have limited our power to detect significant differences. Also, although the current study shows longitudinal associations between bed-sharing and SFP responses, these results do not demonstrate causality. Thus, it remains unclear whether infants with greater self-regulatory abilities and less negativity are more likely to bed-share, if bed-sharing promotes these aspects of infant affect and behavior, or if the relationship is bidirectional. Further, although our use of mainly objective measures is a strength of the current investigation, several methodological limitations are worth noting. First, in the coding scheme for the SFP, when infants’ gaze was ambiguous, gazing toward mother was coded. Thus, there may be some uncertainty in the coding of infant gaze toward mother, which could be refined in future studies. Second, because 6 month nighttime coding was unavailable, we categorized 6 month bed-sharing practices based on maternal self-report, which may be subject to response bias. Repeating these analyses controlling for observed bed-sharing at 6 months would strengthen our conclusion that 3 month bed-sharing practices are particularly important for predicting infant adaptation.
Additionally, the current study focused on mothers, but future research should explore infant self-regulation outside of the mother-child relationship to investigate whether the relations between bed-sharing and infant behavior and affect extend beyond the mother. Thus, although infant SFP responses may serve as an index of infant affect and behavior within a mother-child interaction, there are other paradigms that could be used to measure infant affect and behavior more generally. These may include a stress or frustration paradigm, such as an infant arm restraint task or barrier task. Finally, future studies should go beyond how bed-sharing relates to infant affect and behavior and consider how this practice may relate to other processes, such as an infants’ biological development. Studies suggest that breastfed infants may undergo epigenetic changes that are associated with a lower stress response both during and after the SFP (Lester et al., 2018) and infants with low levels of parental bodily contact have a lower than expected epigenetic age (i.e., biological immaturity; Moore et al., 2017). Given that bed-sharing is closely related to mother-infant contact and breastfeeding, it may be important to investigate the role of bed-sharing in these processes, including the extent to which bed-sharing contributes to epigenetic changes in infants.
The current study is strengthened by its use of an African American Sample. Although studies have found that maternal-infant bed-sharing is common among African American families (Colson et al., 2013), little is known about the sleep patterns and processes as well as how early sleep practices influence later development. The current study is one of few studies to explore early infant sleep patterns within a solely African American population. However, future studies should extend upon the current findings using larger, more racially-diverse samples, to test the generalizability of these findings.
In summary, infants who bed-shared with their mothers later exhibited more self-regulation than infants who did not bed-share. Results also highlight that infants of full bed-sharing mothers had less negativity than infants of non-bed-sharing mothers. The study findings suggest that mother-infant bed-sharing practices may positively impact later infant behavior and affect within the mother-child relationship. If replicated, this knowledge may help health care providers and parents make more informed decisions about sleep locations to improve the health and well-being of both parents and children.
Highlights:
Infant bed-sharing predicted infant behavior within a mother-infant interaction.
Bed-sharing infants had greater self-regulation than non-bed-sharing infants.
Full bed-sharing infants exhibited less negativity than non-bed-sharing infants.
Mother-infant contact during the night was positively associated with bed-sharing.
Acknowledgements
We appreciate the participant’s time and willingness to share their experiences. This work was supported by the Eunice Kennedy Shriver National institute of Child Health and Development [NICHD R21 HD077146]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rachel Lerner, Clark University.
Marie Camerota, RTI International.
Kristin Tully, University of North Carolina at Chapel Hill.
Cathi Propper, University of North Carolina at Chapel Hill.
References
- Ainsworth MDS, Blehar MC, Waters E, & Wall SN (1978). Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Baddock SA, Galland BC, Bolton DPG, Williams SM, & Taylor BJ (2006). Differences in infant and parent behaviors during routine bed sharing compared with cot sleeping in the home setting. Pediatrics, 117(5), 1599–1607. doi: 10.1542/peds.2005-1636 [DOI] [PubMed] [Google Scholar]
- Ball HL (2002) Reasons to bed-share: Why parents sleep with their infants. Journal of Reproductive and Infant Psychology, 20(4), 207–221. doi: 10.1080/0264683021000033147 [DOI] [Google Scholar]
- Blair PS, & Ball HL (2004). The prevalence and characteristics associated with parent–infant bed-sharing in England. Archives of Disease in Childhood, 89(12), 1106–1110. doi: 10.1136/adc.2003.038067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair PS, Heron J, & Fleming PJ (2010). Relationship between bed sharing and breastfeeding: longitudinal, population-based analysis. Pediatrics, 126(5), e1119–e1126. doi: 10.1542/peds.2010-1277 [DOI] [PubMed] [Google Scholar]
- Braungart-Rieker JM, Garwood MM, Powers BP, & Wang XY (2001). Parental sensitivity, infant affect, and affect regulation: Predictors of later attachment. Child Development, 72, 252–270. doi: 10.1111/1467-8624.00277 [DOI] [PubMed] [Google Scholar]
- Buckley P, Rigda RS, Mundy L, & McMillen IC (2002). Interaction between bed sharing and other sleep environments during the first six months of life. Early Human Development, 66(2), 123–132. doi: 10.1016/S0378-3782(01)00243-2 [DOI] [PubMed] [Google Scholar]
- Colson ER, Willinger M, Rybin D, Heeren T, Smith LA, Lister G, & Corwin MJ (2013). Trends and factors associated with infant bed sharing, 1993–2010: the National Infant Sleep Position Study. JAMA pediatrics, 167(11), 1032–1037. doi: 10.1001/jamapediatrics.2013.2560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford CJ (1994). Parenting practices in the basque country: Implications of infant and childhood sleeping location for personality development. Ethos, 22(1), 42–82. doi: 10.1525/eth.1994.22.1.02a00020 [DOI] [Google Scholar]
- Durrence HH, & Lichstein KL (2006). The sleep of African Americans: A comparative review. Behavioral Sleep Medicine, 4(1), 29–44. doi: 10.1207/s15402010bsm0401_3 [DOI] [PubMed] [Google Scholar]
- Feldman R (2004). Mother-infant skin-to-skin contact (kangaroo care): Theoretical, clinical, and empirical aspects. Infants and Young Children, 17(2), 145–161. doi: 10.1097/00001163-200404000-00006 [DOI] [Google Scholar]
- Feldman R, Weller A, Sirota L, & Eidelman AI (2003). Testing a family intervention hypothesis: the contribution of mother-infant skin-to-skin contact (kangaroo care) to family interaction, proximity, and touch. Journal of Family Psychology, 17(1), 94–107. doi: 10.1037/0893-3200.17.1.94 [DOI] [PubMed] [Google Scholar]
- Fleming AS, Ruble DN, Flett GL, & Shaul DL (1988). Postpartum adjustment in first-time mothers: Relations between mood, maternal attitudes, and mother-infant interactions. Developmental psychology, 24(1), 71–81. doi: 10.1037/0012-1649.24.1.71 [DOI] [Google Scholar]
- Germo GR, Chang ES, Keller MA, & Goldberg WA (2007). Child sleep arrangements and family life: Perspectives from mothers and fathers. Infant and Child Development, 16(4), 433–456. doi: 10.1002/icd.521 [DOI] [Google Scholar]
- Gondwe KW, White-Traut R, Brandon D, Pan W, & Holditch-Davis D (2017). The role of sociodemographic factors in maternal psychological distress and mother-preterm infant interactions. Research in Nursing and Health, 40(6), 528–540. doi: 10.1002/nur.21816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WA, Liva S, Moynihan M, & Saunders R (2015). A comparison of actigraphy and sleep diaries for infants’ sleep behavior. Frontiers in Psychiatry, 6, 19. doi: 10.3389/fpsyt.2015.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller MA, & Goldberg WA (2004). Co‐sleeping: Help or hindrance for young children’s independence? Infant and Child Development, 13(5), 369–388. doi: 10.1002/icd.365 [DOI] [Google Scholar]
- Lester BM, Conradt E, LaGasse LL, Tronick EZ, Padbury JF, & Marsit CJ (2018). Epigenetic programming by maternal behavior in the human infant. Pediatrics, 142(4), e20171890. doi: 10.1542/peds.2017-1890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. doi: 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madansky D, & Edelbrock C (1990). Cosleeping in a community sample of 2- and 3-year-old children. Pediatrics, 86(2), 197–203. [PubMed] [Google Scholar]
- McKenna JJ, Ball HL, & Gettler LT (2007). Mother-infant cosleeping, breastfeeding and Sudden Infant Death Syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Yearbook of Physical Anthropology, 50, 133–161. doi: 10.1002/ajpa.20736 [DOI] [PubMed] [Google Scholar]
- McKenna JJ, & Gettler LT (2016). There is no such thing as infant sleep, there is no such thing as breastfeeding, there is only breastsleeping. Acta Paediatrica, 105(1), 17–21. doi: 10.1111/apa.13161 [DOI] [PubMed] [Google Scholar]
- McKenna JJ, & McDade T (2005). Why babies should never sleep alone: A review of the co-sleeping controversy in relation to SIDS, bedsharing and breast feeding. Paediatric Respiratory Reviews, 6(2), 134–152. doi: 10.1016/j.prrv.2005.03.006 [DOI] [PubMed] [Google Scholar]
- McKenna JJ, & Volpe LE (2007). Sleeping with baby: An internet-based sampling of parental experiences, choices, perceptions, and interpretations in a western industrialized context. Infant and Child Development, 16(4), 359–385. doi: 10.1002/icd.525 [DOI] [Google Scholar]
- Mesman J, van IJzendoorn MH, & Bakermans-Kranenburg MJ (2009). The many faces of the still-face paradigm: A review and meta-analysis. Developmental Review, 29(2), 120–162. doi: 10.1016/j.dr.2009.02.001 [DOI] [Google Scholar]
- Messmer R, Miller LD, & Yu CM (2012). The relationship between parent‐infant bed sharing and marital satisfaction for mothers of infants. Family Relations, 61(5), 798–810. doi: 10.1111/j.1741-3729.2012.00734.x [DOI] [Google Scholar]
- Mileva‐Seitz VR, Luijk MPCM, van Ijzendoorn MH, Bakermans‐Kranenburg MJ, Jaddoe VWV, Hofman A, … Tiemeier H (2016). Association between infant nighttime‐sleep location and attachment security: No easy verdict. Infant Mental Health Journal, 37(1), 5–16. doi: 10.1002/imhj.21547 [DOI] [PubMed] [Google Scholar]
- Montirosso R, Borgatti R, Trojan S, Zanini R, & Tronick E (2010). A comparison of dyadic interactions and coping with still‐ face in healthy pre‐ term and full‐ term infants. British Journal of Developmental Psychology, 28(2), 347–368. [DOI] [PubMed] [Google Scholar]
- Moore SR, McEwen LM, Quirt J, Morin A, Mah SM, Barr RG, … Kobor MS (2017). Epigenetic correlates of neonatal contact in humans. Development and Psychopathology, 29(5), 1517–1538. doi: 10.1017/S0954579417001213 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Author. [Google Scholar]
- Philbrook LE, & Teti DM (2016). Bidirectional associations between bedtime parenting and infant sleep: Parenting quality, parenting practices, and their interaction. Journal of Family Psychology, 30(4), 431–441. doi: 10.1037/fam0000198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam SP, Helbig AL, Gartstein MA, Rothbart MK, & Leerkes E (2014). Development and assessment of short and very short forms of the Infant Behavior Questionnaire–Revised. Journal of Personality Assessment, 96, 445–458. doi: 10.1080/00223891.2013.841171 [DOI] [PubMed] [Google Scholar]
- Ramos KD (2003). Intentional versus reactive cosleeping. Sleep Research Online, 5, 141–147. [Google Scholar]
- Ramos KD, Youngclarke D, & Anderson JE (2007). Parental perceptions of sleep problems among co-sleeping and solitary sleeping children. Infant and Child Development, 16, 417–431. doi: 10.1002/icd.526 [DOI] [Google Scholar]
- Shimizu M, & Teti DM (2018). Infant sleeping arrangements, social criticism, and maternal distress in the first year. Infant and child development, e2080. doi: 10.1002/icd.2080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarabulsy GM, Provost MA, Deslandes J, St-Laurent D, Moss E, Lemelin J, … Dassylva J (2003). Individual differences in infant still-face response at 6 months. Infant Behavior and Development, 26(3), 421–438. doi: 10.1016/S0163-6383(03)00039-0 [DOI] [Google Scholar]
- Tronick E, Als H, Adamson L, Wise S, & Brazelton TB (1978). The infant’s response to entrapment between contradictory messages in face-to-face interaction. Journal of the American Academy of Child Psychiatry, 17(1), 1–13. doi: 10.1016/S0002-7138(09)62273-1 [DOI] [PubMed] [Google Scholar]
- Tully KP, & Ball HL (2012). Postnatal unit bassinet types when rooming-in after cesarean birth: implications for breastfeeding and infant safety. Journal of Human Lactation, 28(4), 495–505. doi: 10.1177/0890334412452932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tully KP, Holditch-Davis D, & Brandon D (2015). The relationship between planned and reported home infant sleep locations among mothers of late preterm and term infants. Maternal and Child Health Journal, 19(7), 1616–1623. doi: 10.1007/s10995-015-1672-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tully KP, Stuebe AM, & Verbiest SB (2017). The fourth trimester: A critical transition period with unmet maternal health needs. American Journal of Obstetrics and Gynecology, 217(1), 37–41. doi: 10.1016/j.ajog.2017.03.032 [DOI] [PubMed] [Google Scholar]
- Volpe LE, Ball HL, & McKenna JJ (2013). Nighttime parenting strategies and sleep-related risks to infants. Social Science & Medicine, 79, 92–100. doi: 10.1016/j.socscimed.2012.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner NJ, Mills-Koonce WR, Propper CB, Willoughby MT, Rehder PD, Moore GA, & Cox MJ (2016). Associations between infant behaviors during the face-to-face still-face paradigm and oppositional defiant and callous-unemotional behaviors in early childhood. Journal of Abnormal Child Psychology, 44(8), 1439–1453. doi: 10.1007/s10802-016-0141-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo K, & Reeb-Sutherland BC (2013). Effects of negative temperament on 5-month-old infants’ behavior during the still-face paradigm. Infant Behavior and Development, 36(3), 344–348. doi: 10.1016/j.infbeh.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]


