Abstract
Objectives:
The Resuscitation & Critical Care Unit (ResCCU) is a novel ED-based ICU designed to provide early critical care services. This study sought to identify characteristics of poisoned patients treated in the ResCCU.
Methods:
We conducted a retrospective, single-center case study of poisoned patients over the age of 18 years old over a 16-month period. Patient demographics, drug concentrations, and severity of illness scores were extracted from electronic medical records. Patients were divided into two groups, those who required short term ICU level care (< 24 hours) and prolonged ICU care (> 24 hours).
Results:
A total of 58 ED visits with a tox-related illness were analyzed. There were 24 women (41%) and 34 men (59%). There were 42 patients (72%) who required short term ICU level care and 16 patients (28%) who required prolonged ICU care. In the short-term ICU group, 13 patients (31%) were discharged home directly from the ResCCU, 29 patients (69%) were sent to the inpatient floor, and 1 of the admitted floor patients expired. There were no patients admitted to the floor that required a step-up to the inpatient ICU. 56 patients (97%) were alive at post-admit day 7 and 28, and only 8 (14%) were re-admitted within 30 days.
Conclusions:
Patients who were treated in the ED-based ICU for toxicology-related illnesses were frequently able to be either discharged home or admitted to a regular floor after their initial stabilization and treatment, and none that were sent to the floor required an ICU step-up.
Keywords: ICU, toxicology, emergency medicine
Introduction
Substance use and abuse remains a growing public health concern throughout the world, with use only predicted to continue increasing as novel agents become increasingly available. The Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS) reported that the rate of drug overdose deaths is a leading cause of injury related death (1–2). Polysubstance use is associated with a higher rate of death from overdose compared to single substance use, and in many of these cases novel substances elude detection with conventional methodology (2). However, while substance related deaths are a serious issue, there are other significant health related consequences from non-fatal overdoses, such as hypoxic brain injury and traumatic injuries sustained that can occur during poisoning (2).
Many emergency department visits related to toxicology are commonly from ethanol or other drugs of abuse such as opioids (1). These patients, whether presenting with acute ethanol intoxication or withdrawal, typically improve over a period less than 24 hours (3). In the emergency department, many of these cases that require prolonged observation may require a hospital admission, as the ED rarely has the resources to hold patients for an extended period. For patients with acute toxicologic problems that require ICU level of care, such as respiratory depression necessitating intubation, vasoactive medications, or acute ingestions requiring enhanced elimination, many of these cases often recover quickly with proper supportive care (2).
Emergency department-based intensive care units (ED-ICUs) are an emerging entity within the field of emergency medicine. ED-ICUs primarily provide early critical care services within the broader context of emergency department care (4). The main goals of these ED-ICUs are to provide immediate ICU-level care, reduce ICU admission rates by downgrading patients with initial ICU-level needs, and minimize inpatient hospital length of stay (4). The Resuscitation and Critical Care Unit (ResCCU) is an ED-ICU that opened at our institution in February 2017. The ResCCU is a clinical space, within our existing emergency department, designed to treat critically ill patients who require short-term ICU care, defined as ICU care for less than 24 hours.
The objective of this observational study was to identify characteristics of patients presenting to our emergency department with an acute toxicologic issue requiring ICU level of care for under 24 hours and treated in our ResCCU. We examined patient demographics, types of poisonings, physiologic variables, and patient outcomes of those receiving short-term ICU care.
Material and Methods
Study Design
We conducted a retrospective, single-center case study of poisoned patients over the age of 18 years old, presenting to an urban, quaternary, academic hospital emergency department (>70,000 visits/year) over a 16-month period, and treated in the ResCCU. This study was designed and prepared according to STROBE guidelines (5). Patients whose presenting complaint of ingestion, drug abuse, overdose, withdrawal, or other toxicologic exposure, were included in the study. Patient demographics, presenting chief complaint, relevant laboratory values, physiologic variables, SOFA and APACHE-II scores were extracted from the electronic medical record. ICU level care was defined as treatment in the ResCCU or inpatient ICU. We obtained institutional review board approval and the study was determined to be exempt.
Study Setting and Population
The ResCCU is a 6 bed ED-based intensive care unit, and our medical ICU (MICU) is an 18-bed unit, in an urban, quaternary care, university-affiliated hospital. The ResCCU is staffed by critical care trained emergency physicians, a nursing ratio similar to our inpatient ICU’s (maximum 2 patients to 1 nurse ratio). The ResCCU can deliver ICU level care beyond the initial resuscitation period within the emergency department. Patients treated in the ResCCU are not considered to be inpatients, as they are still under the care of emergency department physicians, so any stay in the ResCCU does not count as a hospital admission or inpatient ICU stay. Since its opening in February 2017, the ResCCU has been operating in a pilot period where it is open 24-hours, Monday through Friday. On weekends, critical patients presenting to the emergency department who would otherwise meet the criteria for treatment in the ResCCU are admitted to an inpatient ICU.
Study Protocol
Study investigators reviewed patient charts using their institution’s electronic medical record systems and extracted patient demographics, medical history, emergency department encounter and hospital admission time points, vital signs, laboratory values, and follow-up data. Ten percent of the patient records, including 42 individual demographic, physiologic, clinical diagnoses, and disposition data elements along with 12 coded elements were reviewed by the PI (AM) to determine data accuracy and adequate inter-rater reliability (IRR) using Cohen’s Kappa statistic (>90%)
We obtained available demographic data (age, race, ethnicity, and gender), type of poisoning, initial laboratory values (blood glucose level, electrolytes, anion gap [AG], creatinine, and lactate), and basic toxicology labs (acetaminophen, aspirin, ethanol, urine drug screen and specific drug concentrations when applicable). We calculated a severity of illness score, using both the Sequential Organ Failure Assessment (SOFA) and the Acute Physiology and Chronic Health Evaluation II (APACHE II) scoring system. We recorded critical care interventions including the use of mechanical ventilation (intubation and noninvasive positive pressure ventilation), vasopressor therapy, volume of fluid resuscitation given in the first 6 hours after presentation, and the use of renal replacement therapy. We collected follow-up data after initial ResCCU resuscitation, including final disposition, ICU step-ups on patients admitted to the inpatient floor, post discharge survival at 7 and 28 days, and 30-day readmissions. Frequencies were compared using Chi-squared and Fisher’s exact test.
Key Outcome Measures
The primary outcome of interest was the requirement of ICU level care for under 24 hours. We divided patients into two groups based on their required duration of ICU level of care: more than 24 hours of ICU-level care (treatment in ResCCU and inpatient ICU), or less than 24 hours of ICU-level care (treatment in ResCCU and then either admitted to the inpatient floor or discharged home). We defined ICU-level care as treatment in the ResCCU or inpatient medical ICU. The group with less than 24 hours of ICU time included patients admitted to the inpatient floor from the ResCCU or patients directly discharged from the ResCCU without any inpatient level of care.
Results
A total of 58 emergency department visits due to an acute toxicologic problem were identified during the study period and included in the analysis. There were 16 cases (16/58, 28%) that required prolonged ICU level of care, defined as ICU needs for greater than 24 hours, and 42 cases (42/58, 72%) that required short term ICU level of care, defined as less than 24 hours of ICU level care in the ResCCU and subsequent admission to the inpatient floor or discharge directly from the emergency department. Details of the two study groups, including demographics, diagnoses, interventions, laboratory values, and clinical severity scores are shown in Table 1. The final dispositions for all patients are outlined in Figure 1. The majority of toxicologic problems in the entire cohort were acute drug ingestions or overdoses, which included suicide attempts with over the counter or prescription drugs, (16/58), followed by alcohol withdrawal (13/58), and most commonly acute alcohol intoxication (8/58). The remainder of cases were a mixture of polysubstance abuse (5/58), heroin use (2/58), carbon monoxide (2/58), other withdrawal (1/58), and other (12/58). The cases classified as “other” are described in detail in Table 2. None of the patients who were sent to the inpatient floor from the ResCCU had an ICU step-up, at either 24-hours or 72-hours after admission. Out of the 58 patients treated in the ResCCU during this time period, 56 (56/58, 97%) were alive at post-admit day 7 and 28. There were 8 patients (8/58, 14%) who were re-admitted to the hospital within 30 days.
Table 1:
Clinical characteristics of patients treated in the ResCCU
| Prolonged ICU Stay (> 24 hours) | Short ICU Stay (< 24 hours) | p | |
|---|---|---|---|
| (n=16) | (n=42) | ||
| Demographics | |||
| Male | 8 (50%) | 26 (62%) | --- |
| Working Diagnosis | |||
| Ingestion/Overdose | 5 (31%) | 11 (26%) | --- |
| CO Poisoning | 0 | 2 (5%) | --- |
| ETOH Abuse | 1 (6%) | 7 (17%) | --- |
| ETOH Withdrawal | 3 (19%) | 10 (23%) | --- |
| Heroin Abuse | 0 | 2 (5%) | --- |
| Polysubstance | 2 (13%) | 3 (7%) | --- |
| Other Withdrawal | 1 (6%) | 0 | --- |
| Other | 4 (25%) | 7 (17%) | --- |
| Clinical Data | |||
| Glascow Coma Scale | 7 [4–12] | 15 [11–15] | 0.002 |
| Temp, C | 36.8 (±1.0) | 37.0 (± 0.9) | 0.60 |
| Heart Rate, bpm | 115 (±37) | 91 (±27) | 0.01 |
| Mean Arterial Pressure, mmHg | 91 (±42) | 85 (±29) | 0.53 |
| WBC (103/μL) | 12.9 (±6.4) | 9.7 (±3.8) | 0.02 |
| HCT, % | 39.3 (±9.0) | 36.9 (±9.2) | 0.37 |
| Lactate, mmol/dL | 4.6 (±3.8) | 3.0 (±2.2) | 0.04 |
| Vasopressors | |||
| Required | 6 (38%) | 2 (5%) | 0.0012 |
| Mechanical Ventilation | |||
| Required | 11 (69%) | 6 (14%) | <0.0001 |
| Severity of Illness | |||
| APACHE II | 21 [15–28] | 20 [11–42] | 0.29 |
| SOFA, Initial | 7 [5–8] | 2.5 [1–4] | <0.0001 |
| SOFA, 48-hour | 2 [5–7] | 0 [0–2] | 0.03 |
| Survival | |||
| Day 7 | |||
| Yes | 16 (100%) | 41 (98%) | 0.53 |
| Day 28 | |||
| Yes | 16 (100%) | 41 (98%) | 0.53 |
Figure 1:
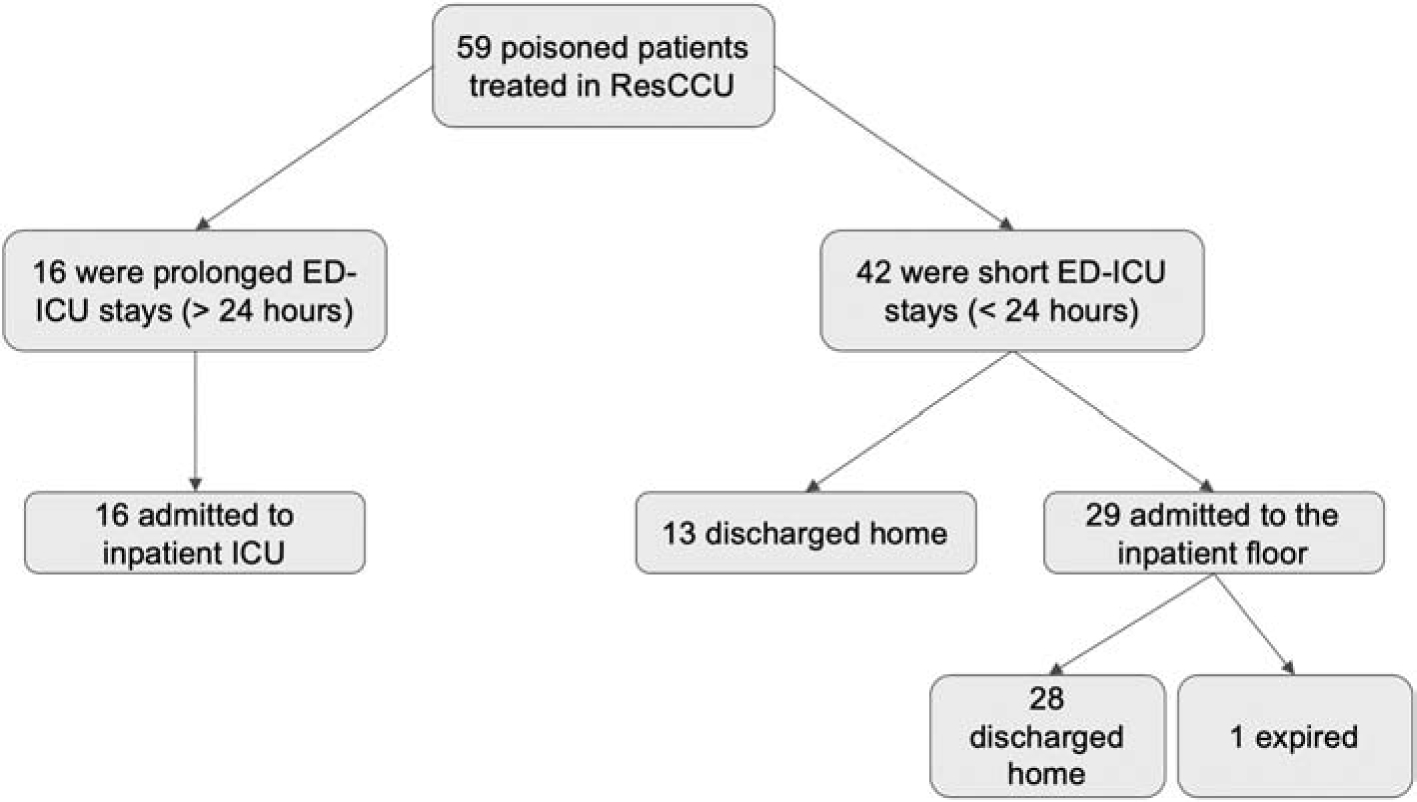
Final disposition of patients treated in the ResCCU
Table 2:
Details on toxicologic cases classified as “other”
| Sex | ED Diagnosis | Vasopressors | Mechanical Ventilation | Final Diagnosis | |
|---|---|---|---|---|---|
| Prolonged ICU | |||||
| Male | Altered Mental Status | No | Yes | Tricyclic Antidepressant Overdose, Acute Respiratory Failure, Hypothermia | |
| Male | Cardiac Arrest, Respiratory Failure | Yes | Yes | Anoxic Brain Injury, Cardiac Arrest, Cocaine Intoxication | |
| Female | Aspiration Pneumonia, Hypoxic/Hypercarbi c respiratory failure | Yes | Yes | Aspiration Pneumonia, Overdose | |
| Female | Hypoxic/Hypercarbi c Respiratory Failure, | Yes | Yes | Hypertensive Emergency, Hypoxic Respiratory | |
| Hypertensive Emergency | Failure, Cocaine Intoxication, Prolonged QT | ||||
| Short ICU | |||||
| Female | Lactic acidosis | No | No | Alcohol Withdrawal, Sick Euthyroid Syndrome | |
| Male | Digoxin Toxicity, Decompensated ETOH Cirrhosis, Acute Kidney Injury, Hyperkalemia | No | No | Type I Hepatorenal Syndrome, Decompensated Alcoholic Cirrhosis, Hyperkalemia | |
| Male | Altered Mental Status, SIRS | No | No | Polysubstance Abuse, Systolic and Diastolic Heart Failure, Rhabdomyolysis | |
| Female | Pneumothorax, COPD exacerbation | No | No | Hydropneumothorax, COPD Exacerbation, Opioid Abuse | |
| Female | Sepsis, Hypercarbic Respiratory Failure, Pulmonary edema, Drug Reaction to Vancomycin | No | Yes | Skin/Soft tissue Infection, Severe Sepsis, Hypercarbic Respiratory Failure | |
| Female | Pneumonia, SIRS | No | No | Pneumonia, Polypharmacy | |
| Female | Upper GI bleed | No | No | GI hemorrhage, Hypovolemic Shock, Alcohol Abuse |
Discussion
Our study examined the characteristics and disposition of acutely poisoned patients treated in our novel ED based ICU. We found that approximately half of the 58 patients treated in our ResCCU during the time period of the study were able to be admitted directly to the inpatient floor, bypassing the inpatient ICU entirely, without a risk of ICU step-up after admission. There was also a cohort of patients, (13/58, 22%), who were able to be discharged home directly from the ResCCU without requiring inpatient admission. Overall, patients requiring prolonged ICU stays were more critically ill compared to those requiring short ICU stays, as evidenced by the higher percentage of patients with low GCS, elevated lactate, and requirements for vasoactive agents and mechanical ventilation in the prolonged ICU group. However, the ResCCU was able to successfully resuscitate a subset of patients in the short ICU cohort, including some who required vasoactive agents and mechanical ventilation, and prevent an inpatient ICU admission. Prior to the opening of the ResCCU, all of these patients would have been admitted to the inpatient ICU in our hospital.
Poisoned patients represent a significant percentage of cases presenting to the emergency department. Reports show that acute drug intoxications represent anywhere from 0.6–2.1% of all emergency department visits, and account for 3–14% of ICU admissions (6–9). A significant number of emergency department visits for poisoning are admitted to the hospital, and a good proportion of those patients require ICU level of care which will depend on various factors such as patient population (10). While a proportion of these patients require critical care level procedures, such as temporary mechanical ventilation for airway protection, vasopressor therapy, or hemodialysis, the majority of patients are sent to the ICU for observation (10). One study found that 20% of their ICU admissions (168/852 patients) were associated with substance abuse (102 related to alcohol, 66 related to other drugs), and rose to 50% in patients under the age of 40 (11). These patients had a higher severity of illness on presentation, fewer pre-existing medical conditions, and an overall shorter duration of time spent on mechanical ventilation (11).
The cost of hospital admissions for poisoned patients is significant, with the cost of ICU level care at most hospitals substantially higher than floor level or emergency care. In 2008, the estimated cost for overdose patients treated in hospitals in the United States was roughly $737 million (12). These figures have been further supported by individual hospital studies looking at the cost of care for substance abuse related ICU admissions. A 1993 study looked at ICU admissions at a single academic center and found that 28% of admissions were related to substance abuse and made up 39% of the costs (13). A 2016 study in New York City showed that 19% of all ICU admissions were related to substance abuse, resulting in a total cost of over $1 million (2). This study was replicated in 2019, taking into account the rising prevalence of substance use and healthcare costs, and found that 25.7% of ICU admissions over an eight month period were related to substance abuse and constituted 23.1% of the total ICU costs, which amounted to almost $75 million (14). The significant cost burden associated with the care and treatment of acutely poisoned patients remains significant, especially as most of them end up requiring ICU level of care at some point during their hospitalization. While our study did not include a cost analysis, the idea behind utilizing the ResCCU to treat poisoned patients and decrease the number of inpatient ICU admissions could have the potential to decrease costs associated with caring for those patients. Future directions could include a specific cost analysis of patients treated in the ED-based ICU compared to a conventional ICU to see if there is any cost savings.
There has been an attempt to decrease unnecessary ICU admissions by developing a risk stratification scoring system to identify which acutely poisoned patients would require critical care (10). In a retrospective cohort study, the authors found that the strongest predictors of requiring ICU level of care were respiratory insufficiency, age over 55 years, and an initial Glasgow Coma Scale less than 6 (10). This scoring system, however, is in the early stages of development and still requires additional validation. One validation study has been performed thus far and showed that a negative score virtually excluded the need for ICU level care, but a positive score was not as useful in risk stratifying patients who needed ICU versus step-down care (15). Until more validation studies are performed, many poisoned patients will continue to be admitted to ICUs for a period of observation or brief critical care.
Limitations
This was a retrospective, single center study, and thus our patient population was limited to those presenting to a quaternary, urban, academic medical center. The geographic location of our hospital additionally affected the type of drug intoxication and overdoses that presented to the emergency department. Finally, the small sample size and retrospective nature of the study precludes it from being used to make a predictive model. Another limitation to consider is whether the SOFA or APACHE II scoring systems are valid for poisoned patients. As many of these patients received ICU-level care, we did include this information as it may be useful for future studies.
Conclusion
Patients who were treated in the ED-based ICU for toxicology related illnesses were frequently able to be either discharged home directly from the ResCCU or admitted to a regular inpatient floor after their initial stabilization.
Funding
1. NIH grant K08HL136858 (Jang)
2. NIH grant R21ES031243 (Jang)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gummin DD, Mowry JB, Spyker DA, Brooks DE, Beuhler MC, Rivers LJ, … & Ryan ML (2019). 2018 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th Annual Report. Clinical toxicology, 57(12), 1220–1413. [DOI] [PubMed] [Google Scholar]
- 2.Orsini Jose, Din Nanda, Elahi Ershad, Gomez Anthony, Rajayer Salil, Malik Ryan & Jean Elie (2017) Clinical and epidemiological characteristics of patients with acute drug intoxication admitted to ICU, Journal of Community Hospital Internal Medicine Perspectives, 7:4, 202–207, DOI: 10.1080/20009666.2017.1356189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Otero R, Long B, Sozener C, Bassin B, Gunnerson K, & Cranford J (2016). 874: IMPACT OF AN EMERGENCY CRITICAL CARE UNIT ON THE DISPOSITION OF CRITICALLY ILL TOXICOLOGY PATIENTS. Critical Care Medicine, 44(12), 294. [Google Scholar]
- 4.Jeong H, Jung YS, Suh GJ, et al. Emergency physician-based intensive care unit for critically ill patients visiting emergency department [published online ahead of print, 2019 Nov 16]. Am J Emerg Med. 2019;S0735–6757(19)30605–9. doi: 10.1016/j.ajem.2019.09.021 [DOI] [PubMed] [Google Scholar]
- 5.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiol Camb Mass. 2007. November;18(6):805–35. [DOI] [PubMed] [Google Scholar]
- 6.Cook R, Allcock R, Johnston M. Self-poisoning: current trends and practice in a U.K. teaching hospital. Clin Med. 2008;8(1):37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henderson A, Wright M, Pond SM. Experience with 732 acute overdose patients admitted to an intensive care unit over six years. Med J Aust. 1993;158(1):28–30. [DOI] [PubMed] [Google Scholar]
- 8.Hendrix L, Verelst S, Desruelles D, et al. Deliberate self-poisoning: characteristics of patients and impact on the emergency department of a large university hospital. Emerg Med J. 2012;30(1):e–9. [DOI] [PubMed] [Google Scholar]
- 9.McMahon A, Brohan J, Donelly M, et al. Characteristics of patients admitted to the intensive care unit following self-poisoning and their impact on resource utilization. Ir J Med Sci. 2014;183(3):391–395. [DOI] [PubMed] [Google Scholar]
- 10.Brandenburg Raya, Brinkman Sylvia, de Keizer Nicolette F., Kesecioglu Jozef, Meulenbelt Jan & de Lange Dylan W. (2017) The need for ICU admission in intoxicated patients: a prediction model, Clinical Toxicology, 55:1, 4–11, DOI: 10.1080/15563650.2016.1222616 [DOI] [PubMed] [Google Scholar]
- 11.Tollisen KH, Bjerva M, Hadley CL, Dahl GT, Högvall LM, Sandvik L, … & Jacobsen D (2019). Substance abuse-related admissions in a mixed Norwegian intensive care population. Acta anaesthesiologica Scandinavica. [DOI] [PubMed] [Google Scholar]
- 12.White AM, Hingson RW, Pan IJ, et al. Hospitalizations for alcohol and drug overdoses in young adults ages 18–24 in the USA, 1999–2008: results from the Nationwide Inpatient Sample. J Stud Alcohol Drugs. 2011;72(5):774–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldwin WA, Rosenfeld BA, Breslow MJ, Buchman TG, Deutschman CS, & Moore RD (1993). Substance abuse-related admissions to adult intensive care. Chest, 103(1), 21–25. [DOI] [PubMed] [Google Scholar]
- 14.Westerhausen D, Perkins AJ, Conley J, Khan BA, & Farber M (2020). Burden of Substance Abuse-Related Admissions to the Medical ICU. Chest, 157(1), 61–66 [DOI] [PubMed] [Google Scholar]
- 15.Regina Böll Katrin Romanek, Schmoll Sabrina, Stich Raphael, Ott Armin, Stenzel Jochen, Geith Stefanie, Eyer Florian & Rabe Christian (2018) Independent validation of the ICU requirement score in a cohort of acutely poisoned adults, Clinical Toxicology, 56:7, 664–666, DOI: 10.1080/15563650.2017.1401635 [DOI] [PubMed] [Google Scholar]


