Abstract
Gentrification in the largest 50 US cities has more than doubled since the 1990s. The process of gentrification can bring about improved neighborhood conditions, reduced rates of crime, and property value increases. At the same time, it can equally foster negative conditions associated with poorer health outcomes, such as disrupted social networks from residential displacement and increases in stress. While neighborhood environment is consistently implicated in health outcomes research, gentrification is rarely conceptualized as a public health issue. Though research on gentrification is growing, empirical studies evaluating the health impacts of gentrification in the US are poorly understood. Here we systematically review US population-based empirical studies examining relationships between gentrification and health. Electronic databases (PubMed, Embase, CINAHL, PsycINFO, Scopus, Web of Science, and Academic Search Complete) were searched using a combination of terms to identify peer-reviewed studies published on or before July 9, 2018, reporting associations between gentrification and health. Study title and abstract screenings were followed by full-text review of all studies meeting the following inclusion criteria of: ≥ 1 quantitative measure of association for a health outcome, within the context of gentrification; peer-reviewed research; located in the US; and English language. Of 8937 studies identified, 6152 underwent title and abstract screening, and 50 studies underwent full-text screening, yielding six studies for review. Gentrification exposure measures and health outcomes examined varied widely. Most studies reported little to no overall association between gentrification and health outcomes; however, gentrification was repeatedly associated with undesirable health effects among Black and economically vulnerable residents. Despite seemingly overall null associations between gentrification and health, evidence suggests that gentrification may negatively impact the health of certain populations, particularly Black and low-income individuals. Complexities inherent in operationalizing gentrification point toward the need for validated measures. Additionally, understanding how gentrification-health associations differ across health endpoints, race/ethnicities, socioeconomic status, and life course can provide insight into whether this process contributes to urban inequality and health disparities. As gentrification occurs across the US, it is important to understand how this process impacts health. While aging cities reinvest in the revitalization of communities, empirical research examining relationships between gentrification and health can help inform policy decisions.
Keywords: Gentrification, Health, Systematic review
Introduction
Gentrification can be defined as “the process in which neighborhoods with low SES experience increased investment and an influx of new residents of higher SES” [1]. Differing perspectives of policy makers, urban planners, sociologists, environmental scientists, economists, residents, and more have led to debates as to whether gentrification is ultimately of net benefit or harm. Though gentrification is associated with increased proximity to material resources, such as green space, recreational facilities and new businesses, income and education may remain a barrier to accessing these resources [2]. Changes often accompanying gentrification (i.e., limited affordable healthy housing, food insecurity from the need to pay high rent on limited income, increased stress, and changes in social networks) may negatively affect certain residents [3–7]. For original residents of formerly impoverished, newly gentrified neighborhoods, the combination of lingering effects from prior neighborhood conditions [8] may result in deepened inequality. Taken wholly, the benefits of gentrification, such as decreases in crime rates, are counterbalanced by other factors like the displacement of existing residents. These changes in neighborhood conditions can affect physical resources and social practices, both of which are upstream determinants of health [9]. Heightened perceptions of discrimination, differential access to resources, increased financial burdens from rising costs of living, and dismantled social networks can all affect psychological and physiological stress [4], which are risk factors for health [10–12]; thus, the premise that gentrification itself impacts health is both reasonable and biologically plausible [13, 14].
Given the large body of literature documenting neighborhood environment impacts on health [9], understanding the role of gentrification on US health outcomes is an imperative. The percentage of gentrified low-income census tracts in the largest 50 US cities has more than doubled since the 1990s [15]. Exact driving forces behind gentrification are debatable, with contributing factors including market forces, government policies, and crime rates [1, 16]. Neighborhoods that have previously undergone disinvestment are prime targets for gentrification. In the US, mechanisms such as redlining and de jure (by law) segregation led to decreased mortgage lending, lower home values, denial of services, and withdrawal of capital [17, 18]. This means an intrinsic tie between neighborhood gentrification and racial housing discrimination. Thus, the process of gentrification converges on predominantly minority and economically disadvantaged communities.
Much of the research pointing toward a link between gentrification and health does not directly measure outcomes. Prior reviews of gentrification literature arise primarily from the social sciences perspective, leaning toward the psychosocial consequences of this process based largely on qualitative research. These reviews provide context for resident’s perceptions of how neighborhood changes may influence health outcomes but fail to capture the extent of gentrifications impact on physical health. Literature reviews that have examined the impacts of gentrification on health were not systematic in nature and included exposures such as disadvantaged neighborhoods and evictions to draw conclusions about the gentrification-health relationship [13]. Furthermore, these reviews on gentrification and health also include both US and non-US-based studies [19, 20], making inferences on the health impacts of gentrification in the US problematic. Studies of gentrification and health outside of the US are not necessarily comparable with the US general population as the historical context, processes, and mediating factors associated with gentrification vary and may skew conclusions [21].
Renewed desires to return to city centers, nationally reported increases in gentrification, and potentially harmful effects to vulnerable residents make understanding the impacts of gentrification on health paramount. Despite the Centers for Disease Control and Prevention deeming gentrification a public health concern [7], little has been done to establish a consensus on the impacts of gentrification on the health and wellbeing of the US population. In this review, we synthesize findings from US population-based, peer-reviewed studies which examine associations between gentrification and health, highlighting both needs and strengths of existing research, and provide suggestions for expanding this body of work.
Methods
We completed this systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines [22]. Articles were considered eligible for review if they reported quantitative measures of association for one or more health outcomes in any context of gentrification. While qualitative analyses can offer insights into how the gentrification process occurs, quantitative analyses are critical for establishing measurable, repeatable, and generalizable associations between gentrification and health. Quantitative studies are also able to investigate causal relationships between gentrification and health. Thus, we chose to focus exclusively on empirical quantitative studies for this review.
The following electronic databases were searched on July 9, 2018, to identify peer-reviewed studies reporting associations between gentrification and health: PubMed, Embase, CINAHL, PsycINFO, Scopus, Web of Science, and Academic Search Complete. Due to variations in the language often used to describe the process of gentrification, we utilized a broad search strategy to obtain peer-reviewed research articles. Searches were conducted using the following title, abstract, keyword, and Medical Subject Heading (MeSH) terms: (gentrif* or residential displacement or forced displacement or involuntary mobility or urban development) or ((relocat*) and (housing or house or neighborhood* or neighborhood* or residen* or communit*)) or ((neighborhood or neighborhood or urban) and (renewal or revitaliz* or restructur* or redevelop* or regenerat*)) and health. Truncated terms were used to capture variation in terminology. For example, gentrif* will catch the terms: gentrification, gentrified, gentrifies, gentrify, and gentrifying.
For the purposes of study selection, we included studies that included gentrification as an exposure, not an outcome. Since there is no consensus on a definition of gentrification, we include the presence of this phenomenon and exposure as defined by the original study authors. Thus, if the paper indicates that gentrification is present or assessed in any manner (i.e., within or between gentrified neighborhoods, levels of gentrification, types of gentrification, pre- or post-gentrification, etc.), the study is eligible for inclusion in this review. Unless authors explicitly referred to gentrification, general measures of neighborhood improvement, such as greening or parks, were not eligible for inclusion as these processes are not in and of themselves indicative of gentrification. Also, studies focused on populations moving to middle class neighborhoods (i.e., Moving to Opportunity Study [23]) were not included unless it was reported that residents moved specifically to a gentrified community.
Articles eligible for review reported effect estimates for at least one health outcome within the context of gentrification. Studies which focused on indicators of health (homicides, violence, etc.), but not actual health outcomes, were excluded. The process of gentrification in the US has unique features, and studies of gentrification in other countries may not be generalizable to the US context, thus we excluded non-US-based studies. Non-peer reviewed reports (including conference abstracts, dissertations, commentaries, etc.) were also excluded from the review.
Covidence web-based software [24] was used for screening and extracting data. Study title and abstract screenings were completed by GS and HB using eligibility criteria. Conflicts in study eligibility assignments were resolved by RT. Following initial screen, the full text of each potentially eligible article was independently reviewed by GS and HB, with ties resolved by RT. Data extracted from each research article at the study level include the study population, study design, gentrification exposure measure, health outcome(s), measure of association between gentrification and health outcome, and statistical significance.
Results
Based on search criteria, we initially identified 8937 studies, of which 2785 were duplicates (Fig. 1). Of 6152 studies that underwent title and abstract screening, 6102 were excluded. Fifty studies underwent full-text screening. Only six studies [25–30] (Table 1) met all eligibility requirements for inclusion in this literature review.
Fig. 1.
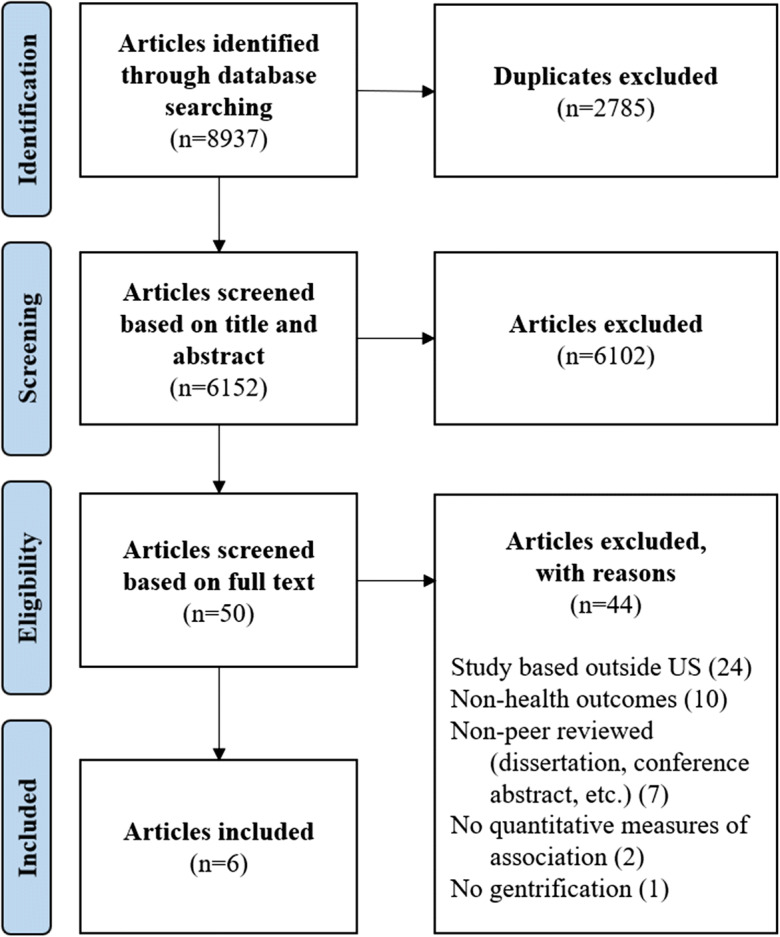
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram to identify quantitative studies of gentrification and health in the US
Table 1.
Characteristics of quantitative studies on associations between gentrification and health outcomes in the US
| Author (year) | Study design and methods | Study population | Study location | Definition and sources of data for gentrification measure | Health outcome | Findings |
|---|---|---|---|---|---|---|
| Huynh (2014) | Cross-sectional, multilevel, generalized estimating equations | 126,165 infants born to women age 20+, 2008–2010 (excl. multiple births, multiparas, infants with congenital anomalies, and non-specified race/ethnicity) | New York City |
Gentrification = ↑ in residents with a college education and ↑ in median household income and ↓ in residents living below the poverty line from 1990 to 2009 across 59 community districts Sources: 2005–2009 American Community Survey and the 1990 Census |
Preterm birth | Gentrification not associated with preterm birth across races (AOR = 0.96 (95% CI: 0.87, 1.06) for very high vs very low); very high gentrified neighborhoods (vs. very low) had increased odds preterm birth for Black mothers (AOR = 1.16 (95% CI: 1.01, 1.33)), and decreased odds of preterm births for White mothers (AOR = 0.78 (95% CI: 0.64, 0.94)) |
| Mair (2015) | Cohort, multilevel | 548 Multi-Ethnic Study of Atherosclerosis (MESA) participants (men and women aged 45 to 84) | New York City |
Changes in five neighborhood dimensions between 2002 and 2007 across 104 census tracts: social cohesion, stress, violence, safety, and the esthetic environment Source: MESA Community Surveys |
Depressive symptoms |
No significant associations between gentrification (changes in neighborhood dimensions) and depressive symptoms: social cohesion ß = − 2.82 (95% CI: − 6.10, 0.46); stress ß = 1.75 (95% CI: − 1.10, 4.60); violence ß = 0.52 (95% CI: − 1.99, 3.03); safety ß = − 1.34 (95% CI: − 3.47, 0.78); esthetic environment ß = − 2.00 (95% CI: − 4.60, 0.60) |
| Gibbons (2016) | Cross sectional, multilevel | 19,279 respondents in the 2008 Philadelphia Health Management Corporation’s Southeastern Pennsylvania Household Health Survey | Philadelphia |
Changes in the citywide median values from 2000 to 2009 across 968 neighborhoods (census tracts), classified as follows: Gentrifiable = median household income below city median Gentrifying = gentrifiable and ↑ (gross rent or median income above the citywide median) and ↑ college-educated residents above the citywide median Black Gentrification = gentrifying and ↑ in % Black White Gentrification = gentrifying and ↑ in %White, ↓ in % Black Sources: 2000 Decennial Census and the 2006–2010 American Community Survey |
Self-rated health | Gentrification associated with lower odds of poor/fair health across races (OR = 0.81, p ≤ 0.10); being Black (OR = 1.73, p ≤ 0.05) or being in a neighborhood of Black gentrification associated with greater odds (OR = 1.74, p ≤ 0.10) of poor/fair self-rated health |
| Lim (2017) | Cohort, negative binomial regression | 12,882 residents of gentrifying neighborhoods in 2006 with records of emergency department visits or hospitalization ≥ 1 every 2 years, 2006–2014 | New York City |
Changes from 2005 to 2014 in 55 neighborhoods, classified as follows: Gentrifying = neighborhoods with low initial rankings (i.e., low median household income, median rental price, and proportion of college graduates in 2005) and high rankings of growth (i.e., rapid ↑ in median household income, median rental price, and proportion of college graduates) determined by principle component analysis Non-gentrifying, poor = neighborhoods with low initial and growth rankings as determined by principle component analysis Source: Public Use Microdata Area boundaries from 2014 American Community Survey |
Emergency department (ED) visits, hospitalizations, mental health-related visits |
Displaced residents (vs. remaining in gentrified neighborhoods) had higher rates of ED visits (RR = 1.1 (95% CI: 1.0, 1.2)), hospitalizations (RR = 1.3 (95% CI: (1.2, 1.4)), and mental health-related visits (RR = 1.8 (95% CI: 1.5, 2.2)) Displaced residents from gentrifying neighborhoods (vs. only living in non-gentrifying neighborhoods) had higher rates of ED visits (RR = 1.2 (95% CI: 1.1, 1.2)), Hospitalizations (RR = 1.2 (95% CI: (1.1, 1.3)), and mental health-related visits (RR = 1.7 (95% CI: 1.4, 2.0)) |
| Smith (2017) | Quasi-experimental | 6,810 Medicare beneficiaries aged 65 or older (first wave respondents in National Health & Aging Trends Study) | US |
Change from 2000 to 2010 in neighborhoods, defined by census tracts as follows: Gentrifying = neighborhoods in the < 40th percentile of the metropolitan area who experienced increase over the last 10 years of (a) median household income, (b) percent of college-educated residents, (c) median owner-occupied housing values, and (d) median rent Source: 1970–2010 National Neighborhood Change Database (NCDB) |
Self-rated health, depression and anxiety symptoms |
In gentrifying neighborhoods (compared with low-income neighborhoods): economically vulnerable (EV) residents had higher self-rated health (ß = 1.81 (95% CI: 1.10, 2.51)), but high income (HI) residents had worse mental health (ß = 3.62 (95% CI: 2.84, 4.41)) EV and HI residents had more depression/anxiety than counterparts in affluent areas (ß = 4.79 (95% CI: 2.79, 6.78) and ß = 3.64 (95% CI: 2.87, 4.41)), respectively |
| Izenberg (2018) |
Cross-sectional, survey-adjusted multivariable logistic regression |
60,196 adults age ≥ 18 (respondents in California Health Interview Survey, 2013–2015) | California |
Change in 7992 census tracts from 2010 to 2015, classified as follows: Gentrifiable = median household income below the metropolitan area median defined by the Census-Based Statistical Area (CBSA), a proportion of pre-1980 building stock exceeding that of the median tract for the CBSA, and ≥ 50% of census block groups urbanized. Gentrifying = ↑ median rent (2015-adjusted dollars); [2] ↑ percentage adults with bachelor’s degrees (relative to the tract’s CBSA) Stable = gentrifiable at baseline, but did not gentrify Not gentrifiable = not gentrifiable at baseline Sources: 2006–2010 and 2011–2015 American Community Surveys |
Self-rated health | Gentrification not associated with lower poor/hair health across races (AOR = 0.93 (95% CI: 0.76, 1.14)); being Black in a gentrifying neighborhood associated with over double the odds of fair/poor self-rated health (AOR = 2.44 (95% CI: 1.36, 4.37)) |
AOR, adjusted odds ratio; OR, odds ratio; RR, rate ratio; ß, coefficient estimate on linear scale; CI, confidence interval
Study Designs and Methods
The six empirical studies reviewed varied in design. Three studies were cross-sectional, two were cohort studies, and one quasi-experimental design.
The studies identified also examined several health outcomes in relation to gentrification. Many of these outcomes were not examined directly, instead proxies were relied upon for assessment. The most commonly analyzed health outcomes were self-rated health (33.3%) and mental health (33.3%). Only one study examined a specified health outcome (preterm birth). While the outcomes examined were varied, studies offered similar biological rationale for mechanisms of gentrification impacting health through multiple pathways, including psychosocial stress, access to resources and opportunity, and collective efficacy.
Study Populations and Settings
Most of the reviewed studies consisted of adult populations, including the elderly. One study focused specifically on the older adult population (age 65 and older). Another investigation examined preterm birth in infants. None of the identified studies examined health impacts of gentrification among children.
Sample size for quantitative studies on gentrification and health ranged from 548 individuals to a population of more than 100,000. Only one study population was less than 1000.
All studies included in the review centered on urban populations. Four studies were in large population centers in the Northeastern US (three in New York City, one in Philadelphia). One statewide investigation occurred in California. We identified only one national study of gentrification and health for inclusion in the review.
Gentrification Exposures
Gentrification exposure definitions were varied across the research studies, but each included some composite of the change in several neighborhood level measures from baseline to the end of the study period. The scale (the city/area/district/census tract) at which gentrification was measured varied; four research investigations used census tracts as the geographic unit of analysis [26–29], one used Public Use Microdata Areas [30], and one used community districts [25]. All eligible studies incorporated median household income and college education into the measure of gentrification. All but one investigation used some measure of rent to construct the gentrification variable. Other factors utilized when defining gentrification included neighborhood level poverty, housing values, age of building stock proportion, and urbanization.
Following specified criteria for gentrification eligibility, most studies categorized geographic units of analysis as undergoing gentrification or not (i.e., stable, non-gentrifying, or non-gentrifying poor). This was mostly classified using an increase in specified sociodemographic variables; one study incorporated principle components analysis into this process. A single study further classified this exposure by defining Black gentrification (gentrifying and an increase in percent Black population) and White gentrification (gentrifying and increase in percent White population but a decrease in percent Black population). Alternatively, gentrification exposure was defined in one study by utilizing z-scores to assign quintiles of gentrification exposure (very high, high, medium, low, and very low). Another study utilized an entirely different approach by measuring five neighborhood dimensions (social cohesion, stress, violence, safety, and esthetic quality) related to gentrification.
Health Outcomes
Studies exploring the impacts of self-rated health on gentrification found negligible effects on self-rated health in the general adult study population. In both studies, however, Blacks fared worse compared with Whites [26, 28]. In a California statewide investigation, gentrification was associated with fair/poor self-rated health, while no patterns of significant associations were observed for either Hispanics, Asian/Pacific Islanders, and multiple/other races. Only one study considered the differential impacts of the residents that were gentrifying these neighborhoods and observed Black gentrification was associated with worse self-rated health for Black residents. These findings are supported by research on gentrification and neighborhood/city health (published after the search date), reporting negative associations between gentrification and poor self-rated health at the neighborhood level, but significantly higher rates of poor self-rated health in census tracts with larger Black and Hispanic populations [31]. Among a national sample of Medicare beneficiaries (age 65 and older), economically vulnerable individuals in gentrifying neighborhoods reported better self-rated health compared with those in low-income neighborhoods. There were no significant associations between gentrification and self-rated for higher income adults.
Three studies examined associations between gentrification and mental health, all utilizing different health endpoints, two examining mental health symptoms via validated questionnaires, and another examining mental health-related emergency department visits and hospitalizations. Older adults in gentrifying neighborhoods experienced more symptoms of anxiety and depression than their counterparts in moderate-to-high income neighborhoods, regardless of individual income status. Older adults living in high-income gentrifying neighborhoods still had more anxiety and depression symptoms than older adults living in low-income neighborhoods that were not gentrifying. Depression scores (Center for Epidemiologic Studies Depression (CES-D) Scale) decreased over time for adult residents of changing neighborhoods experiencing increases in social cohesion, while depression scores increased for adults experiencing adverse neighborhood changes, though not statistically significant. Residents displaced from gentrifying neighborhoods had higher rates of emergency department visits and hospitalizations, in comparison with residents remaining in gentrifying neighborhoods, mostly attributed to mental health. Among original residents of gentrifying neighborhoods, those who moved to non-gentrifying, poor neighborhoods had a greater number of clinically classified mental health-related visits compared with those that remained in the gentrifying neighborhood, an effect which persisted 5 years after displacement. Mental health emergency department visits and hospitalizations were similar among gentrifying neighborhoods and non-gentrifying poor neighborhoods.
A study on gentrification and preterm birth [25] found no associations in the general population. However, residence in a very high gentrified neighborhood was protective for non-Hispanic Whites (compared with residence in a very low gentrified neighborhood), but adversely associated with preterm birth for Non-Hispanic Blacks.
Discussion
The objective of this systematic review was to synthesize and critique empirical research studies examining relationships between gentrification and health among the US population. Subsequent sections summarize the existing gentrification-health literature, strengths and weaknesses of this research, and recommendations for future inquiry.
Summary of Findings
A chief finding from this literature review is that the quantifiable relationship between gentrification and health outcomes in the US is gravely understudied, as our search yielded only six empirical studies (all in US urban populations). The health effects examined were too varied to draw any general conclusions; however, these studies mostly revealed null associations between gentrification and health outcomes. This aligns with previous research conducted outside of the US that indicates the process of gentrification does little to improve population health [19, 20]. Like research from abroad, this review unmasked differences in how gentrification impacts the health of different populations. Though gentrification seemingly has little to no impact on health overall, within different subpopulations (especially Blacks), there was a consistent pattern of undesirable health effects. These findings generate concerns of whether gentrification has become a potential tool for deepening urban inequality and related health disparities. As city planning, zoning ordinances, budget allocation, business development, and regulations make way for local development and revitalization, there is a need for public health research to be conducted which can inform these decision-making processes.
Measures of Gentrification
The lack of consensus on how gentrification is defined and measured reverberates throughout this review, as the authors of each paper developed different measures of gentrification. Most adapted existing gentrification measures from Freeman [32] which incorporate publicly available data and reproducible methods, but confines gentrification to urban environments—disregarding the less studied phenomenon of rural gentrification [33]. And while gentrification is not merely a yes/no phenomenon, these strategies result in eligible neighborhoods being classified as gentrified or not. Even so, variations in the individual components used to create these gentrification measures can yield vast differences in a seemingly straightforward classification [14, 32, 34]. Further insight into health impacts of the gentrification process (i.e., through stages, severity, mechanisms, speed, etc.) requires more complex, non-binary measures and warrants further examination in the literature.
These difficulties inherent in gentrification measurement are not unique to the public health arena. Gentrification measures vary across fields and literature with studies using metrics ranging from property values [35] to the frequency of coffee shops [36]. Though changes in the built environment are elements often used to recognize the presence of gentrification, none of the studies included in this review utilized measurements of the built environment. Incorporating local information may more accurately capture the process of gentrification [37], but would also be more labor intensive and limit reproducibility. As this area of study progresses, researchers must weigh the comparability of a simplified measure to the local relevance of a more nuanced and precise measure.
The scale at which these gentrification measures are applied also varies. Several of these investigations use census tract data as proxies for neighborhoods, which is easily available and enhances the ability to compare results across studies but may not be meaningful in practice. Such strategies also result in concerns over the and Modifiable Areal Unit Problem, where the aggregation of smaller data points into larger units alters the variance of the data and can lead to inflated effect estimates [38]. As these measurements can impact policy, it is important that they are both theoretically sound and materially relevant. Using a coherent, consistent exposure measure has its benefits in policy creation, though this is not always feasible. Thus current gentrification measurement is problematic, suffering the same difficulties inherent in any neighborhood focused research, and highlighting the need for validated measures of gentrification [14].
Methodological Considerations
The existing gentrification-health literature includes numerous study designs resulting in a variety of statistical methods and model stipulations. Because cross-sectional designs prevent drawing conclusions about the impact of gentrification on any health outcome, future literature would benefit from the use of more longitudinal studies designs in the future since these designs can detect changes over time. In instances where cross-sectional studies are employed, investigators should consider strategies such as multilevel modeling, which allow for the assessment of both individual and neighborhood-level factors [39].
All of the studies [25–30] relied on large sample sizes, but only one [27] actually drew upon a nationally representative sample, hindering the generalizability of results. The limited geographic regions in which this research was conducted may also impact the extent to which this research is generalizable to other areas of the nation as gentrification may operate differently across various geopolitical environments (i.e., political power wielded by demographic, economic, and geographic factions in the US). Additional studies are needed that yield findings which are generalizable to larger portions of the US population. While local gentrification and health studies may be most desirable for creating the tailored public health solutions, the impacts of larger (even nationwide) research investigations must not be discounted as national studies can provide a basis for federal policy mandates. And while gentrification occurs in both rural and urban areas [33, 40, 41], these studies focused solely on urban populations, bringing about additional concerns of urban-rural biases. Future research should also consider the role of geography and urbanicity in the gentrification-health association.
Most studies lacked a theoretical framework clearly outlining which factors would be confounders, mediators, or moderators of the gentrification-health relationship. Complex statistical methods can be used for mediation analysis to enhance our knowledge of the mechanisms through which gentrification affects health. For example, future studies can examine factors such as green space, food (in) security, and psychosocial stressors as pathways by which gentrification can influence biological processes in the body to impact health. Examining mediating effects of the gentrification-health association will enable research to move beyond merely describing these associations to understanding processes and potential points of intervention.
Gentrification has social, political, and economic consequences which can differ across groups of individuals; thus, examining potential modifiers are important for pointing toward populations particularly vulnerable to health impacts of gentrification. This review exposes racial disparities in the gentrification-health associations. As gentrification often descends on high minority resource deprived neighborhoods, prior inequities may persist despite neighborhood revitalization. More research is needed to disentangle the independent and joint influences of gentrification and race on health. Additional differences observed among the economically vulnerable are backed by previous research indicating poorer health status among low-income residents of gentrified neighborhoods outside the US [19, 20]. Other factors that potentially modify the associations between gentrification and health include age, educational attainment, pre-existing health, and immigrant status. In some instances, gentrification has ultimately reinforced and upheld mechanisms of structural racism, elitism, and power dynamics so understanding how this process may impact different populations is imperative [42].
This systematic review is not without limitations. All but one [27] of these studies evaluates the health impacts of gentrification occurring in the past 20 years, narrowing the window in which any conclusions can be drawn. A lack of consistency between health outcomes examined and methods of assessing these outcomes further prevented drawing any solid conclusions on these associations. Also, due to the small number of articles identified in this review, we were unable to assess risk of bias for this literature [43].
Conclusion
This review undoubtedly reveals a massive gap in the literature surrounding the public health implications of gentrification, a process that is increasingly occurring throughout the US. As this area of research is in its infancy, there is much room for growth. Gentrification is easily identified though not readily operationalized; hence, the development of validated measures can greatly advance gentrification-health research. Gentrification should be examined as both a threshold and gradient. While gradient measures will provide more detailed information on how health may be impacted over the continuum of gentrification, the inclusion of threshold measures may be necessary for the implementation of public health policies impacting gentrifying neighborhoods. Future studies should examine how processes (i.e., mechanisms, speed, stages, etc.) of gentrification impact health, populations most affected, and whether this contributes to deepening health disparities. In lieu of increased reports of gentrification throughout the US, understanding how this process may promote or prevent health is essential to ensuring the well-being of our nation. Empirical research examining relationships between gentrification and health is necessary to inform policy as aging cities reinvest in the revitalization of communities.
Acknowledgements
Research was supported by grants from the National Institute for Minority Health and Health Disparities (P60MD000214), the National Institute on Aging (1K02AG059140), the Hopkins Center for Health Disparities Solutions Pilot Project Award (U54MD000214), the National Cancer Institute grant (K01CA184288), National Institute of Mental Health (R25MH083620), and the Sidney Kimmel Cancer Center grant (P30CA006973).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hwang J, Lin J. What have we learned about the causes of recent gentrification? Cityscape. 2016;18(3):9–26. [Google Scholar]
- 2.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 3.Bates LK. Gentrification and displacement study: implementing an equitable inclusive development strategy in the context of gentrification. Urban Studies and Planning Faculty Publications and Presentations. Portland State University PDXScholar; Portland, Oregon; 2013;83.
- 4.Cassel J. The contribution of the social environment to host resistance. The fourth Wade Hampton frost lecture. 1976. Am J Epidemiol. 1995;141(9):798–814. doi: 10.1093/oxfordjournals.aje.a117515. [DOI] [PubMed] [Google Scholar]
- 5.Baum F. Social capital: is it good for your health? Issues for a public health agenda. J Epidemiol Community Health. 1999;53(4):195–196. doi: 10.1136/jech.53.4.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knotts HG, Haspel M. The impact of gentrification on voter turnout. Soc Sci Q. 2006;87(1):110–121. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Health Effects of Gentrification. 2013 [Available from: https://www.cdc.gov/healthyplaces/healthtopics/gentrification.htm. Accessed 2 Jul 2019.
- 8.Cozier YC. Invited commentary: the enduring role of "place" in health-a historic perspective. Am J Epidemiol. 2017;185(11):1203–1205. doi: 10.1093/aje/kwx085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian S. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geronimus AT, Hicken M, Keene D, Bound J. "Weathering" and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McEwen BS. Protective and damaging effects of stress mediators: the good and bad sides of the response to stress. Metab Clin Exp. 2002;51(6 Suppl 1):2–4. doi: 10.1053/meta.2002.33183. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosschot JF, Thayer JF, Christenfeld N, Linden W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 2003;65(1):22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- 13.Venis Wilder A-LM, Makoba E, Arniella G. The Health Impact of Gentrification. 2017;4:1981–91.
- 14.Mujahid MS, Sohn EK, Izenberg J, Gao X, Tulier ME, Lee MM, et al. Gentrification and displacement in the San Francisco Bay area: a comparison of measurement approaches. Int J Environ Res Public Health. 2019;16(12):2246. doi: 10.3390/ijerph16122246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maciag M. Gentrification in America Report 2015 [Available from: https://www.governing.com/gov-data/census/gentrification-in-cities-governing-report.html. Accessed 23 Jul 2019.
- 16.Lees L, Slater T, Wyly EK. Gentrification: Routledge; 2008.
- 17.Wyly EK, Hammel DJ. Gentrification, segregation, and discrimination in the American urban system. Environ Plan A. 2004;36(7):1215–1241. [Google Scholar]
- 18.Mitchell B, Franco J. HOLC “REDLINING” MAPS: the persistent structure of segregation and economic inequality. National Community Reinvestment Coalition; Washington, DC; 2018.
- 19.Mehdipanah R, Marra G, Melis G, Gelormino E. Urban renewal, gentrification and health equity: a realist perspective. Eur J Pub Health. 2017;28(2):243–248. doi: 10.1093/eurpub/ckx202. [DOI] [PubMed] [Google Scholar]
- 20.McCartney G, Hearty W, Taulbut M, Mitchell R, Dryden R, Collins C. Regeneration and health: a structured, rapid literature review. Public Health. 2017;148:69–87. doi: 10.1016/j.puhe.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 21.Slater T. North American gentrification? Revanchist and emancipatory perspectives explored. Environ Plan A. 2004;36(7):1191–1213. [Google Scholar]
- 22.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Development USDoHaU. Moving to opportunity for fair housing [Available from: https://www.hud.gov/programdescription/mto.
- 24.Babineau J. Product review: Covidence (systematic review software) Journal of the Canadian Health Libraries Association/Journal de l'Association des bibliothèques de la santé du Canada. 2014;35(2):68–71. [Google Scholar]
- 25.Huynh M, Maroko AR. Gentrification and preterm birth in new York City, 2008-2010. J Urban Health. 2014;91(1):211–220. doi: 10.1007/s11524-013-9823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gibbons J, Barton MS. The Association of Minority Self-Rated Health with black versus white gentrification. J Urban Health. 2016;93(6):909–922. doi: 10.1007/s11524-016-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith RJ, Lehning AJ, Kim K. Aging in place in gentrifying neighborhoods: implications for physical and mental health. The Gerontologist 2017;58(1):26–35. 10.1093/geront/gnx105. [DOI] [PubMed]
- 28.Izenberg JM, Mujahid MS, Yen IH. Health in changing neighborhoods: a study of the relationship between gentrification and self-rated health in the state of California. Health Place. 2018;52:188–195. doi: 10.1016/j.healthplace.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mair C, Diez Roux AV, Golden SH, Rapp S, Seeman T, Shea S. Change in neighborhood environments and depressive symptoms in new York City: the multi-ethnic study of atherosclerosis. Health Place. 2015;32:93–98. doi: 10.1016/j.healthplace.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lim S, Chan PY, Walters S, Culp G, Huynh M, Gould LH. Impact of residential displacement on healthcare access and mental health among original residents of gentrifying neighborhoods in New York City. PloS one. 2017;12(12):e0190139. doi: 10.1371/journal.pone.0190139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gibbons J, Barton M, Brault E. Evaluating gentrification’s relation to neighborhood and city health. PloS one. 2018;13(11) [DOI] [PMC free article] [PubMed]
- 32.Freeman L. Displacement or succession?: residential mobility in gentrifying neighborhoods. Urban Aff Rev. 2005;40:463–491. [Google Scholar]
- 33.Bernt M. Gentrification between urban and rural. Dialogues Hum Geogr. 2018;8(1):31–35. [Google Scholar]
- 34.Barton M. An exploration of the importance of the strategy used to identify gentrification. Urban Stud. 2016;53(1):92–111. [Google Scholar]
- 35.Lin J, editor Gentrification and transit in northwest Chicago. Transportation Quarterly. 2002;56:175–191.
- 36.Papachristos AV, Smith CM, Scherer ML, Fugiero MA. More coffee, less crime? The relationship between gentrification and neighborhood crime rates in Chicago, 1991 to 2005. City Community. 2011;10(3):215–240. [Google Scholar]
- 37.Hwang J. Gentrification in changing cities: immigration, new diversity, and racial inequality in neighborhood renewal. Ann Am Acad Pol Soc Sci. 2015;660(1):319–340. [Google Scholar]
- 38.Wong DW. The modifiable areal unit problem (MAUP). WorldMinds: geographical perspectives on 100 problems: Springer; 2004. p. 571–5.
- 39.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21(1):171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 40.Nelson PB, Hines JD. Rural gentrification and networks of capital accumulation—a case study of Jackson, Wyoming. Environ Plan A. 2018;50(7):1473–1495. [Google Scholar]
- 41.Nelson PB, Oberg A, Nelson L. Rural gentrification and linked migration in the United States. J Rural Stud. 2010;26(4):343–352. [Google Scholar]
- 42.Kirkland E. What's race got to do with it? Looking for the racial dimensions of gentrification. West J Black Stud. 2008;32(2)
- 43.Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open. 2018;8(3):e019703. doi: 10.1136/bmjopen-2017-019703. [DOI] [PMC free article] [PubMed] [Google Scholar]


