Background
Worldwide, laparoscopic cholecystectomies are rapidly increasing, so are inadvertent iatrogenic bile duct injuries (IBDI).1,2 These devastating injuries mostly have non-dilated common bile duct (CBD),3 usually not more than 6mm in diameter.4 Hence, their immediate repairs are overtly demanding and often generate considerable perioperative anxiety. Nevertheless, primary choledochorrhaphy over a T-tube and timely referral to expertise may rescue both, the patient and the surgeon.1 Here, a T-tube, as large as 14-Fr, is recommended considering future interventional radiological procedures.5 We describe a simple and effective technique of housing a 14-Fr T-tube in a non-dilated CBD.
Technique
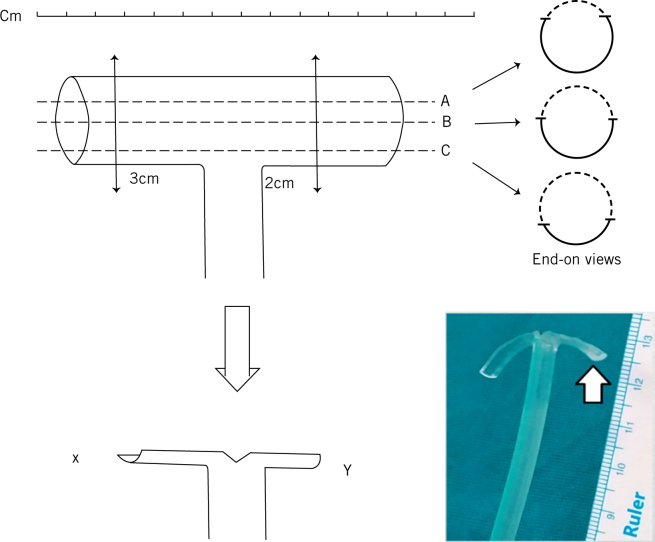
The T-tube’s horizontal limb is reduced to 2cm (duodenal side) and 3cm (hepatic confluence side) on either side of the vertical limb. Then, about 80% of its back-wall circumference is excised with sharp scissors before making a small V-cut at the T-junction to complete the procedure (Fig 1).
Figure 1.
Preparation of 14-Fr T-tube. Note, the conventional excision methods (A and B) leave 50-60% circumference of the horizontal arm intact; such a bulky remnant is unlikely to fit into a non-dilated bile duct without almost completely occluding its lumen as well as the blood supply. Also, note that excision of about 80% circumference (C), as in our technique, strategically leaves just a strip of remnant (white arrow, inset) that is long enough to prevent extra-luminal dislodgement, short enough to abstain trans-luminal displacement towards hepatic ducts (X) or duodenum (Y), and wide enough to make it self-retaining without obstructing the bile duct.
Discussion
Contrary to common practice of excising half the back-wall,5 our technical modification has several advantages. It satisfactorily splints a collapsed CBD without occluding the biliary outflow. While preserving the fundamental purpose to be self-retaining, its design prevents dislodgement and displacement.5 The severity of luminal foreign-body reaction and its associated morbidity decreases. It can be extracted easily and the resultant sinus track possesses adequate width for radiologic interventions postoperatively.5 Lastly, its learning curve is just two cases. We have successfully used it in five cases of IBDIs, hence propose it further for blunt/penetrating biliary trauma and liver transplant patients having non-dilated bile ducts to repair.
References
- 1.Wang L, Dong P, Zhang Y et al. Iatrogenic bile duct Injury with a retained T-tube in common bile duct for 10 years: A case report. Medicine (Baltimore) 2019; : e15127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Renz BW, Böch F, Angele MK. Bile Duct Injury after Cholecystectomy: Surgical Therapy. Visc Med 2017; : 184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunt DR. Common bile duct stones in non-dilated bile ducts? An ultrasound study. Australas Radiol 1996; : 221–222. [DOI] [PubMed] [Google Scholar]
- 4.Skoczylas K, Pawełas A. Ultrasound imaging of the liver and bile ducts - expectations of a clinician. J Ultrason 2015; : 292–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah KN, Clary BM. Stones in the bile duct: Clinical features and open surgical approaches and techniques In: Jarnagin WR, Belghiti J, Blumgart LH, eds. Blumgart’s Surgery of the Liver, Biliary Tract and Pancreas. Philadelphia: Elsevier Saunders; 2017. pp585–603. [Google Scholar]