Abstract
Parathyroid exploration via a focused approach or bilateral neck exploration should be considered in the management of all types of hyperparathyroidism. Eutopic and ectopic, single or multiple glands can pose challenges to the surgeon and available preoperative imaging modalities may not be equally applicable or appropriate in all cases. We report an interesting case of parathyroid surgery where the patient presented with a rare ectopic adenoma in the form of a hyperparathyroid crisis.
Keywords: Ectopic, Submandibular, Parathyroid glands, Hyperparathyroid crisis, Explorations
Background
Hyperparathyroidism is a relatively common endocrine disorder which can be broadly divided into primary, secondary or tertiary types.1 Single or, rarely, multiple glands become hyperactive and they are usually classified as adenomas. Prolonged hypocalcaemia resulting in hyperplasia of usually multiple glands gives rise to secondary hyperparathyroidism, while one or more glands becoming autonomous in a scenario of secondary hyperparathyroidism is referred to as tertiary hyperparathyroidism. Secondary and tertiary hyperparathyroidism are more common in patients with chronic kidney disease who are dependent on haemodialysis.
Case history
A 69-year-old man was admitted to the emergency department with delirium, hypovolaemia and renal failure. He was found to have an elevated total serum calcium level of 5.74mmol/l on evaluation (normal range 2.2–2.6mmol/l). He was resuscitated and a diagnosis of hyperparathyroid crisis was made due to his high intact parathyroid hormone (i-PTH) value (200.2pmol/l; normal range 1.6–6.9pmol/l). He had no previous diagnosis of hyperparathyroidism, although he had been treated for vague abdominal symptoms and body ache. High-frequency ultrasound and non-contrast computed tomography (CT; [contrast study was avoided due to elevated serum creatinine]) showed a 1cm swelling behind the lower pole of thyroid right lobe.
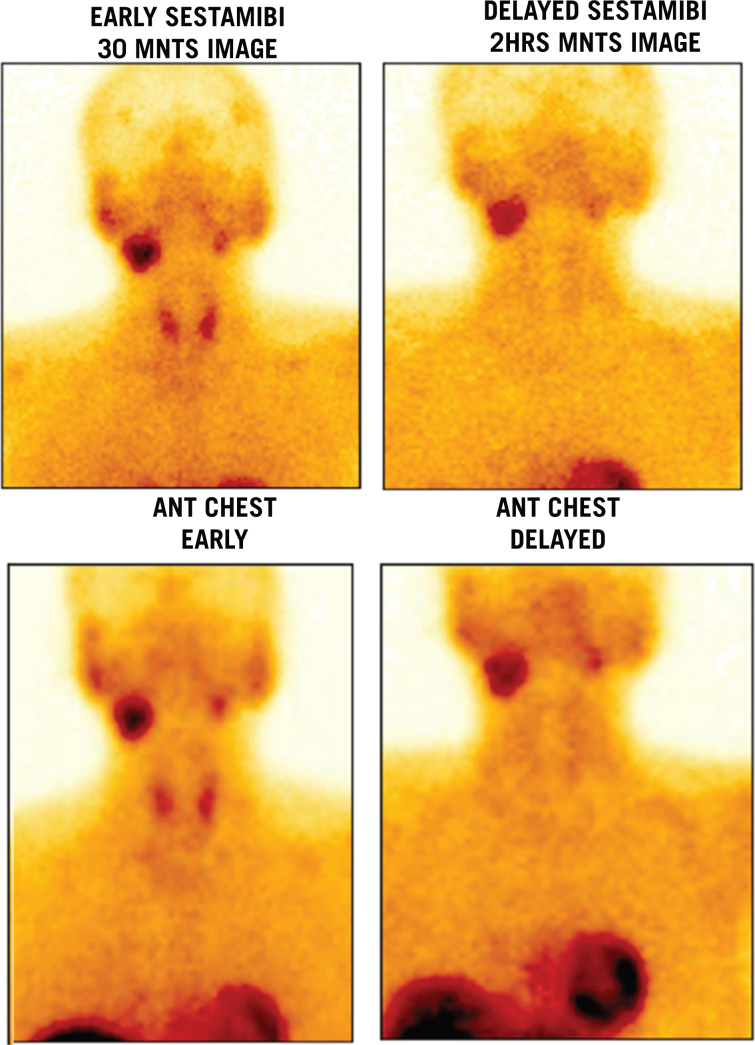
The swelling was successfully removed through a mini-incision in the right lower neck. His i-PTH value immediately reduced to 84.8pmol/l but went up back to 198pmol/l the next morning. High-frequency ultrasound of the neck was repeated the following day, which picked up a submandibular swelling that was masked in the first scan due to the right internal jugular vein catheter and its adhesive dressings. This was removed prior to anaesthesia on securing a central venous line. Tc-99m Sestamibi imaging (Fig 1) and fine-needle aspiration cytology were performed to confirm the diagnosis prior to re-exploration, as four-dimensional (4D) CT (a multiplanar CT scan with a fourth dimension consisting of changes in contrast attenuation over periods of time) is not considered safe in impaired renal function.
Figure 1.
Tc-99 Sestamibi scan of right submandibular ectopic parathyroid gland
The pathology report became available on the fifth day. The report indicated that the removed nodule as nonspecific lymphadenitis. The fine-needle aspiration cytology from the submandibular swelling detected parathyroid cells. The submandibular swelling of 3 × 3 × 2cm was removed the following week (Fig 2). The patient’s i-PTH was down to 0.42pmol/l and the biopsy was consistent with parathyroid adenoma.
Figure 2.

The excised parathyroid gland
Discussion
Hyperparathyroidism is a relatively common endocrine disorder after diabetes and thyroid disorders.1 It can be broadly classified into primary, secondary and tertiary hyperparathyroidism. In primary hyperparathyroidism, a single or, less commonly, multiple glands are autonomously hyperactive, although multiglandular hyperplasia or parathyroid carcinoma can also be rare causative factors. In secondary and tertiary hyperparathyroidism, multiple gland involvement is common and hence surgery can be more challenging.
Diagnosis of hyperparathyroidism is based on biochemical values but localisation is important in surgery for single-gland disease. Re-explorative surgery is not uncommon in parathyroid surgery, especially in ectopic and supernumerary gland pathologies.2 High-frequency ultrasound, Tc-99m Sestamibi imaging and 4D CT are currently the most useful preoperative localising tests.3 single-photon emission CT, magnetic resonance imaging, selective angiography and selective venous sampling are the other available tests.3 Notoriously operator dependent in parathyroid, high-frequency ultrasound continues to be a useful basic test which can assess thyroid and other neck structures simultaneously and often helps in a guided aspiration if indicated. It can also be safely repeated as many times as needed and even during a surgery. Sestamibi is a functional test lacking anatomical details but shows high sensitivity and specificity in lateralising the pathological gland to one side or even to unsuspected ectopic sites. 4D CT, which combines great anatomical delineation with functional assessment, is a more realistic tool especially in a redo procedure.4 Two tests being concordant is more dependable than a single test with sophistication.3
Despite all these tools, a surgeon can miss a gland during surgery but, more often, a supernumerary or ectopic gland makes things difficult and more reoperations may be needed for persistent or recurrent hyperparathyroidism. Ectopic parathyroid gland is a rare entity,4 and hyperparathyroid crisis is an uncommon complication of primary hyperparathyroidism.5 Interestingly, both conditions coexisted in our case.
Among ectopic sites, the submandibular triangle is a rare location, which has been attributed to arrest of the descend of the inferior parathyroid developing from the third pharyngeal pouch.4 Hyperparathyroid crisis, unless promptly managed, can lead to lethal complications and therefore the localisation of parathyroid was first attempted in intensive care.5
Unfortunately, the adhesive bandage in the submandibular triangle of an internal jugular vein catheter placed as a life-saving measure in the emergency department prevented the radiologist from making a surprise diagnosis of an ectopic gland in the submandibular triangle, as the treating physicians had no reason to suspect this rare condition in an acutely ill patient. CT took precedence over Tc-99mm Sestamibi in a hypovolaemic patient and a positive finding concordant with positive high-frequency ultrasound finding prevented the Sestamibi imaging being performed once hypovolaemia was corrected. A portable mini-gamma-camera, which can be used to locate active glands during surgery, was not used in this case. As a result, the first surgery became futile with the recovery of a lymph node alone in minimally invasive surgery. This was not detrimental to the patient because a re-exploration away from the first surgery site in the neck led to cure of the disease. This is in contrast with a normal re-exploration in the neck where a second surgery in and around the thyroid is a difficult procedure.
Conclusion
Parathyroid surgery due to single-gland disease requires accurate localisation prior to surgery. Localisation can become tricky in life-threatening situations such as acute hyperparathyroid crisis where the selection of imaging tests has limitations and re-evaluation and re-exploration may be required for a successful surgical outcome. Attempting localisation of the gland in the acute illness, overlooking the need for Sestamibi or 4D CT prior to the first surgery and not using intraoperative gamma camera were limitations in our surgical protocol.
References
- 1.DeLellis RA, Mazzaglia P, Mangrey S. Primary hyperparathyroidism: a current perspective. Arch Pathol Lab Med 2008; : 1251–1262. [DOI] [PubMed] [Google Scholar]
- 2.Alam S, Volsky PG, Wadsworth JT, Karakla DW. Consideration of submandibular (undescended) ectopic parathyroid glands in surgery and localization studies. JAMA Otolaryngol Head Neck Surg 2015; : 943–944. [DOI] [PubMed] [Google Scholar]
- 3.Kowa XY, Richards P, Waterhouse M et al. Atypical presentations of parathyroid gland pathology: a pictorial review. Eur J Radiol Open 2019; : 320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanack MD, Maawy AA, Oh DK, Bouvet M. Undescended parathyroid adenoma. BMJ Case Rep 2015; : bcr2014208277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh DN, Gupta SK, Kumari N et al. Primary hyperparathyroidism presenting as hypercalcemic crisis: twenty-year experience. Indian J Endocrinol Metab 2015; : 100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]