Abstract
Melanoma differentiation-associated gene 5 (MDA5) antibody, also known as anti-CADM140 antibody is recognised to be associated with rapidly progressive interstitial lung disease, which can be fatal within 3 months. It is also known to be associated with amyopathic dermatomyositis. We report a case of MDA5 antibody-associated interstitial pneumonia with autoimmune features, without cutaneous features of dermatomyositis, in a Sudanese patient with dual positive antibodies to Ro52. The patient notably had several features associated with poor prognosis, including age, high serum ferritin level, anti-Ro52 antibodies and progressive lung infiltrates during treatment.
Keywords: connective tissue disease, interstitial lung disease, radiology, lung function, immunology
Background
Anti-melanoma differentiation-associated gene 5 (MDA5)-associated rapidly progressive interstitial lung disease is a potentially fatal and under-recognised condition that is characteristically associated with clinically amyopathic dermatomyositis (CADM) with cutaneous features of tender palmar papules, cutaneous ulceration and the absence of proximal muscle weakness.1 The antibody is recognised to be associated with rapidly progressive interstitial lung disease, which can be fatal within 3 months2 and with arthritis and arthralgia.1 The anti-MDA5 antibody is more common in Asian populations, has been reported in Caucasians but has rarely been found in patients of African ethnicity.3 The incidence of CADM is approximately 20% of classic dermatomyositis in the USA, with a higher percentage of patients being women.4 We believe this case report will be of interest to rheumatologists and respiratory physicians as early recognition of this syndrome is essential, to enable prompt and intensive treatment in a condition of known poor prognosis.
Case presentation
A 51-year-old Sudanese woman, a non-smoker, presented to the emergency department with 2 weeks of dyspnoea and polyarthralgia. Her history included intermittent polyarthralgia (with positive rheumatoid factor and anti-cyclic citrullinated peptide (CCP) without meeting the classification criteria for rheumatoid arthritis), type 2 diabetes mellitus and hypertension. She did not have a fever, rash or synovitis on physical examination. Chest auscultation revealed bilateral coarse crepitations. Upper and lower limb strengths were normal, and there were no palmar papules, cutaneous ulceration or Gottron’s papules.
She was managed for a lower respiratory tract infection with intravenous antibiotics and commenced on prednisolone 37.5 mg/day and hydroxychloroquine 400 mg daily for differential diagnosis of rheumatoid arthritis-associated interstitial lung disease, and discharged home on supplemental oxygen. She represented 1 week later with severe dyspnoea and respiratory failure, with oxygen saturation of 50% on 50 L/min flow.
Investigations
Initial investigation during her first admission revealed white cell count=3.96×109/L (normal range (NR) 4–11×109/L), erythrocyte sedimentation rate=62 mm (NR 1–15 mm), C-reactive protein=11.9 mg/L (NR <8 mg/L) and creatine kinase=197 U/L (NR <150 U/L). Her rheumatoid factor was 14 IU/mL (NR ≤13 IU/mL) and anti-CCP antibody level was 122 IU/mL (NR ≤5 IU/mL).
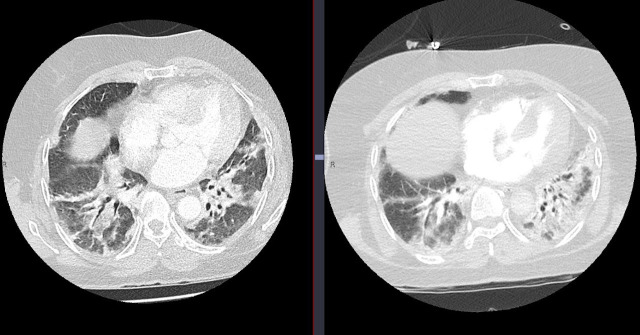
Chest X-ray revealed bilateral patchy opacity. CT scan of the chest showed patchy consolidation and ground-glass opacity in upper and lower lobes without established fibrosis. Bronchoscopy was normal apart from generalised laryngeal oedema. Septic screens, including the culture of bronchial washings and atypical infective serology, were negative.
Investigations repeated during her second presentation showed white cell count 5.32×109/L, C-reactive protein 23 g/L, erythrocyte sedimentation rate 43 mm/hour and creatine kinase 78 U/L. Antinuclear antibodies were present with cytoplasmic pattern, and myositis immunoblot identified antibodies to Ro52 and MDA5. Her ferritin level was markedly elevated 2616 µg/L (NR 30–250 µg/L). Repeat high-resolution CT of the chest showed interval development of peripheral mixed ground-glass changes and patchy consolidation (figure 1).
Figure 1.
Interval CT of the chest 4 weeks apart demonstrating the progression of patchy consolidation and ground-glass opacity despite intensive treatment.
Differential diagnosis
During her initial presentation, she was managed as pneumonia based on clinical symptoms of dyspnoea, elevated C-reactive protein and bilateral patchy consolidation on chest X-ray. She was commenced on intravenous antibiotics with clinical improvement. However, during her second admission, as there was ongoing clinical deterioration with hypoxemia despite intravenous antibiotics, a non-infective cause was entertained.
Differential diagnoses of non-infective causes considered in this patient were interstitial lung disease associated with dermatomyositis and rheumatoid arthritis-associated interstitial lung disease. In the absence of typical features of dermatomyositis such as muscle weakness, heliotrope rash, Gottron’s papules and Jo-1 antibody, interstitial lung disease associated with dermatomyositis was thought unlikely.
Rheumatoid arthritis-associated interstitial lung disease was another differential diagnosis considered given the presence of polyarthralgia, rheumatoid factor and anti-CCP antibody. However, this is generally associated with much higher levels of rheumatoid factor,5 than seen in our case. The CT of the chest tends to show a usual interstitial pneumonia pattern (honeycomb with and without traction bronchiectasis, reticular opacities and subpleural basal predominance)6 which was also not seen in our patient.
Finally, with her rapid clinical deterioration, progressive radiological changes and presence of MDA5 antibody, a diagnosis of anti-MDA5 antibody-associated rapidly progressive interstitial lung disease was made.
Treatment
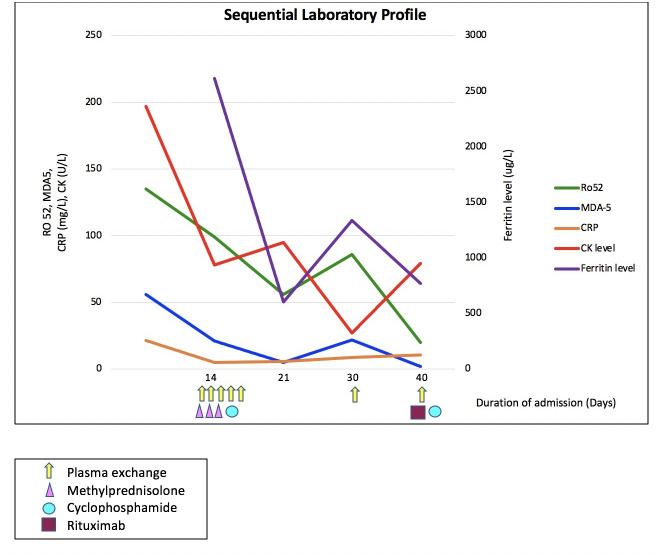
She was commenced on methylprednisolone and mycophenolate. The progressive respiratory failure prompted a transfer to the tertiary referral centre, where she received five cycles of plasma exchange together with further intravenous methylprednisolone 1 g daily for 3 days, cyclophosphamide and rituximab. Serial MDA5 antibody titre and ferritin levels were measured to monitor response to treatment and gauge disease activity. Figure 2 illustrates the decrease in the MDA5 antibody titre and ferritin level with treatment.
Figure 2.
Depiction of levels of MDA5 antibody, Ro52 antibody, creatine kinase (CK), C-reactive protein (CRP) and ferritin with treatments used. MDA5, melanoma differentiation-associatedgene 5.
Outcome and follow-up
She was managed in the intensive care unit for severe respiratory failure for 1 month. Despite intensive therapy, she had ongoing clinical deterioration and developed pneumomediastinum. She died from progressive respiratory failure.
Discussion
Patients with connective tissue disease-related interstitial lung disease are often younger, women and non-smokers as was our patient.7 One study also reported that female gender, anti-CCP and anti-MDA5 positivity are risk factors for connective tissue disease associated with interstitial lung disease.8
Very few cases of MDA5-associated rapidly progressive interstitial lung disease without signs of dermatomyositis have been reported.2 9 In a study of 32 Chinese patients with anti-MDA5 antibody, 11 had no features of dermatomyositis (either cutaneous or muscle), and the interstitial lung disease was classified as interstitial pneumonia with autoimmune features (IPAF).10 IPAF is a terminology based on the combination of clinical, serological and morphological domains used to describe patients with unclassifiable interstitial lung disease who has autoimmune features but not fulfilling the classification criteria of any connective tissue disease diagnosis.11 Indeed the case presented herein would best satisfy this classification, though rapidly progressive interstitial lung disease can precede the development of cutaneous and muscular manifestations.2
Anti-MDA5-associated rapidly progressive interstitial lung disease is known to have a poor prognosis, with mortality up to 54.6%.10 Ro52 antibody has been reported to be more frequently associated with female gender.12 Among patients with anti-synthetase syndrome, those with interstitial lung disease who have concurrent antibodies to Ro52 are known to have more severe disease. Recent evidence suggests that patients with concurrent antibodies to MDA5 and Ro52 also have more severe disease and higher mortality.10 Patients with dual antibodies to MDA5 and Ro52 are at higher risk for pneumomediastinum.10 Patients with anti-MDA5 over 45 years of age are at the highest risk of developing interstitial lung disease.1
The anti-MDA5 antibody is thought to play a pathogenetic role in mediating lung injury,3 and some reports have suggested that anti-MDA5 antibody titre may be a novel tool to monitor disease activity.13 14 However, other reports showed that MDA5 antibody levels did not correlate with disease activity.1 15 Serum ferritin levels exceeding 1600 ng/mL are correlated with poor prognosis,13 as is the number of infiltrated lung fields and worsening lung infiltrates during therapy.
Treatment of MDA5-associated rapidly progressive interstitial lung disease includes intensive immunosuppressive treatment with high-dose glucocorticoids, ciclosporin and cyclophosphamide.9 There are emerging reports for the use of tofacitinib,16 rituximab17 and plasma exchange.13
In summary, we report a case of MDA5 antibody-associated IPAF, without cutaneous features of dermatomyositis, in a Sudanese patient with dual positive antibodies to Ro52 and MDA5. Our case notably had several features associated with poor prognosis, including age, high serum ferritin level, anti-Ro52 antibodies and progressive lung infiltrates during treatment. Clinicians should be aware of anti-MDA5-associated rapidly progressive interstitial lung disease, even in the absence of features of dermatomyositis (in which case the classification is of anti-MDA5-IPAF), as early recognition of this syndrome is essential, to enable prompt and intensive treatment in a condition of known poor prognosis.
Learning points.
Melanoma differentiation-associated gene 5 (MDA5) antibody is characteristically associated with clinically amyopathic dermatomyositis with cutaneous features of tender palmar papules, cutaneous ulceration and the absence of proximal muscle weakness.
In patients with respiratory symptoms and positive MDA5 antibody, consider MDA5 antibody-associated interstitial pneumonia with autoimmune features, without cutaneous features of dermatomyositis.
Early recognition of this syndrome is essential, to enable prompt and intensive treatment in a condition of known poor prognosis.
Acknowledgments
We would like to thank Dr Lawrence Chia Wei Oh (MBBS FRANZCR) for providing us with the CT chest images.
Footnotes
Contributors: LEH, SP and VL were involved in the care of the patient being discussed. LEH performed literature review, prepared and formatted the manuscript of the case report. SP and VL edited, reviewed and formatted the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Moghadam-Kia S, Oddis CV, Aggarwal R. Anti-MDA5 antibody spectrum in Western world. Curr Rheumatol Rep 2018;20:78. 10.1007/s11926-018-0798-1 [DOI] [PubMed] [Google Scholar]
- 2.González-Moreno J, Raya-Cruz M, Losada-Lopez I, et al. Rapidly progressive interstitial lung disease due to anti-MDA5 antibodies without skin involvement: a case report and literature review. Rheumatol Int 2018;38:1293–6. 10.1007/s00296-018-3991-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moghadam-Kia S, Oddis CV, Sato S, et al. Antimelanoma differentiation-associated gene 5 antibody: expanding the clinical spectrum in North American patients with dermatomyositis. J Rheumatol 2017;44:319–25. 10.3899/jrheum.160682 [DOI] [PubMed] [Google Scholar]
- 4.Sontheimer RD, RDJAoTM S. Mda5 autoantibody-another indicator of clinical diversity in dermatomyositis. Ann Transl Med 2017;5:7. 10.21037/atm.2017.03.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaw M, Collins BF, Ho LA, et al. Rheumatoid arthritis-associated lung disease. Eur Respir Rev 2015;24:1–16. 10.1183/09059180.00008014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devaraj A. Imaging: how to recognise idiopathic pulmonary fibrosis. European Respiratory Review 2014;23:215–9. 10.1183/09059180.00001514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jee A, Adelstein S, Bleasel J, et al. Role of autoantibodies in the diagnosis of connective-tissue disease ILD (CTD-ILD) and interstitial pneumonia with autoimmune features (Ipaf). J Clin Med 2017;6:51 10.3390/jcm6050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tian M, Huang W, Ren F, et al. Comparative analysis of connective tissue disease-associated interstitial lung disease and interstitial pneumonia with autoimmune features. Clin Rheumatol 2020;39:575–83. 10.1007/s10067-019-04836-3 [DOI] [PubMed] [Google Scholar]
- 9.Sakamoto N, Ishimoto H, Nakashima S, et al. Clinical features of Anti-MDA5 antibody-positive rapidly progressive interstitial lung disease without signs of dermatomyositis. Intern Med 2019;58:837–41. 10.2169/internalmedicine.1516-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang W, Ren F, Wang Q, et al. Clinical features of thirty-two patients with anti-melanoma differentiation-associated gene 5 antibodies. Clin Exp Rheumatol 2019;37:803–7. [PubMed] [Google Scholar]
- 11.Wilfong EM, Lentz RJ, Guttentag A, et al. Interstitial pneumonia with autoimmune features: an emerging challenge at the intersection of rheumatology and pulmonology. Arthritis Rheumatol 2018;70:1901–13. 10.1002/art.40679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Temmoku J, Sato S, Fujita Y, et al. Clinical significance of myositis-specific autoantibody profiles in Japanese patients with polymyositis/dermatomyositis. Medicine 2019;98:e15578 10.1097/MD.0000000000015578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Endo Y, Koga T, Suzuki T, et al. Successful treatment of plasma exchange for rapidly progressive interstitial lung disease with anti-MDA5 antibody-positive dermatomyositis: a case report. Medicine 2018;97:e0436. 10.1097/MD.0000000000010436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsushita T, Mizumaki K, Kano M, et al. Antimelanoma differentiation-associated protein 5 antibody level is a novel tool for monitoring disease activity in rapidly progressive interstitial lung disease with dermatomyositis. Br J Dermatol 2017;176:395–402. 10.1111/bjd.14882 [DOI] [PubMed] [Google Scholar]
- 15.Abe Y, Matsushita M, Tada K, et al. Clinical characteristics and change in the antibody titres of patients with anti-MDA5 antibody-positive inflammatory myositis. Rheumatology 2017;56:1492–7. 10.1093/rheumatology/kex188 [DOI] [PubMed] [Google Scholar]
- 16.Kurasawa K, Arai S, Namiki Y, et al. Tofacitinib for refractory interstitial lung diseases in anti-melanoma differentiation-associated 5 gene antibody-positive dermatomyositis. Rheumatology 2018;57:2114–9. 10.1093/rheumatology/key188 [DOI] [PubMed] [Google Scholar]
- 17.So H, Wong VTL, Lao VWN, et al. Rituximab for refractory rapidly progressive interstitial lung disease related to anti-MDA5 antibody-positive amyopathic dermatomyositis. Clin Rheumatol 2018;37:1983–9. 10.1007/s10067-018-4122-2 [DOI] [PubMed] [Google Scholar]