The aryl hydrocarbon receptor (AHR) is activated by multiple viruses to evade the host immune response, a strategy exploited in pre-clinical models to limit the replication of Zika and Influenza A. In a recent study, Liu et al. report that AHR drives the hypersecretion of lung mucins after SARS-CoV-2 infection, suggesting a role for AHR in respiratory failure and highlighting its potential therapeutic value.
COVID-19 shows a wide spectrum of clinical severity, ranging from asymptomatic or mild infection (~80% of cases) to severe and critical life-threatening forms of the disease (~5%–15%). The primary cause of death in severe COVID-19 patients is progressive respiratory failure. Since respiratory symptoms in these patients usually worsen a week after disease onset, it has been suggested that they result from a dysregulated pro-inflammatory response, which eventually damages lung epithelial and endothelial cells, impairing the exchange of O2 and CO2.1 An imbalanced inflammatory response, however, does not explain hypoxia in all COVID-19 patients. Indeed, severe hypoxia has also been reported at early stages of COVID-19, before an excessive inflammatory response is established. Intriguingly, despite presenting low blood O2 levels, some of these patients show minimal symptoms and apparent distress, a condition referred to as ‘silent hypoxia’.2 The mechanism responsible for the development of silent hypoxia is still lacking. In a recent work published in Cell Research, Liu et al. report that SARS-CoV-2-triggered IFN signaling induces mucin overproduction by lung epithelial cells, thickening the blood–air barrier and hindering O2 diffusion, leading to hypoxia.3 Moreover, they show that mucin expression is driven by the transcription factor aryl hydrocarbon receptor (AHR), identifying AHR as a potential target for the treatment of hypoxia in COVID-19 patients.
Liu et al. first detected increased expression of mucins in bronchoalveolar lavage (BALF) samples taken from COVID-19 patients and macaques infected with SARS-CoV-2, in agreement with independent scRNA-Seq studies4 and the detection of increased mucin expression and mucus production in COVID-19 autopsy samples.5 Mucus hypersecretion in COVID-19 patients has been associated with airflow obstruction and respiratory distress, hence the mechanisms that control it are considered therapeutic targets of interest. Through a combination of in vitro and in vivo experiments, Liu et al. found that IFN-β and IFN-γ upregulate mucin production in lung epithelial cells. IFNs are known to activate AHR signaling, e.g., by inducing the expression of the enzymes IDO1/TDO2 which catalyze the generation of the AHR agonist Kynurenine (Kyn).6,7 Indeed, the authors found that an IFN-IDO-Kyn-AHR axis drives mucin expression in lung epithelial cells. Finally, the authors used a murine model to evaluate the translational implications of their work. Using human ACE2 transgenic mice, they found that SARS-CoV-2 induced the upregulation of lung mucin expression and decrease in O2 levels in peripheral blood, which was reverted by the administration of an AHR antagonist, identifying AHR as a candidate target to treat SARS-CoV-2-induced lung pathology.
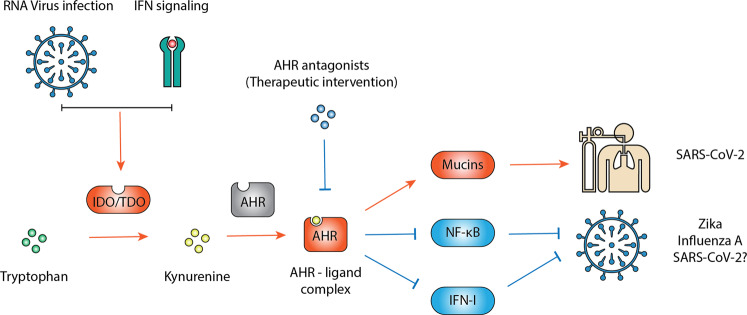
AHR signaling has been shown to play a physiological role in the regulation of the host anti-viral response.8–10 Type I IFN (IFN-I), the central regulator of the anti-viral response, induces AHR expression, but AHR can suppress the expression of IFN-I, most likely as part of a negative feedback loop.6–9 Moreover, AHR has also been shown to inhibit NF-κB, an additional key effector molecule in the host anti-viral and inflammatory response.6,7,9 Previous studies using AHR antagonists and gene knockdown have shown that AHR inactivation reduces Influenza A, Zika and Dengue virus replication.8,9 These findings led to the hypothesis that AHR is a pro-viral host factor targeted by multiple viruses to limit IFN-I/NF-κB-driven host anti-viral immunity and promote virus replication (Fig. 1). The identification of AHR as a pro-viral host factor also has important therapeutic implications. Indeed, in mice infected with Influenza A virus, AHR antagonism increased IFN-β levels, reduced BALF viral titers and increased survival.8 AHR antagonism also reduced Zika virus replication in fetuses and ameliorated congenital Zika virus syndrome in a pre-clinical mouse model.9
Fig. 1. AHR is a candidate therapeutic target for viral infection.
AHR activation during viral infection results in the upregulation of IDO/TDO, which convert tryptophan to Kynurenine (Kyn). Kyn activates AHR, leading to formation of an AHR–ligand complex that limits host anti-viral responses mediated by IFN-I and NF-κB, thus promoting viral replication. AHR signaling also induces mucin expression in lung epithelial cells, thickening the blood–air barrier, impairing O2 diffusion and causing hypoxia. AHR antagonists limit AHR activation, boosting the host anti-viral response and consequently reducing viral replication. AHR antagonism also reduces the expression of mucins, limiting lung pathology during SARS-CoV-2 infection.
It was recently reported that infection with human coronaviruses, including SARS-CoV-2, activated AHR signaling, as determined by the RNA-seq analysis of lung epithelial cells.10 This finding triggered the question of whether AHR also plays a role as a pro-viral host factor in the replication of coronaviruses and, consequently, can be a candidate therapeutic target against SARS-CoV-2. The work by Liu et al. uncovers an additional benefit of targeting AHR during SARS-CoV-2 infection; pharmacologic inhibition of AHR may not only boost anti-viral immunity, but also directly suppress mechanisms of lung pathology (Fig. 1). However, since the effects of AHR inhibition on lung SARS-CoV-2 replication were not assessed, Liu et al. cannot rule out the possibility that the reduction in virus-induced lung pathology results from the suppression of SARS-CoV-2 replication. AHR antagonists likely ameliorate lung pathology by both boosting anti-viral immunity and limiting virus replication, and also by suppressing excessive mucus production.
Independently of the specific mechanisms involved in the therapeutic effects of AHR antagonists on SARS-CoV-2 infection, the last few years have seen an increasing number of reports identifying AHR as a candidate target for novel anti-viral therapies. The work by Liu et al. highlights the need to characterize the role of AHR in virus-induced pathology and the mechanisms involved, to guide the development of AHR-targeted therapies for virus-induced diseases.
Competing interests
F.J.Q. is a member of the Scientific Advisory Board of Kyn Therapeutics.
References
- 1.Huang C, et al. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tobin MJ, et al. Am. J. Respir. Crit. Care Med. 2020;202:356–360. doi: 10.1164/rccm.202006-2157CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y, et al. Cell Res. 2020 doi: 10.1038/s41422-020-00435-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He J, et al. Protein Cell. 2020;11:680–687. doi: 10.1007/s13238-020-00752-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bian XW, et al. Natl. Sci. Rev. 2020;7:1414–1418. doi: 10.1093/nsr/nwaa123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gutierrez-Vazquez C, et al. Immunity. 2018;48:19–33. doi: 10.1016/j.immuni.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rothhammer V, et al. Nat. Med. 2016;22:586–597. doi: 10.1038/nm.4106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamada T, et al. Nat. Immunol. 2016;17:687–694. doi: 10.1038/ni.3422. [DOI] [PubMed] [Google Scholar]
- 9.Giovannoni F, et al. Nat. Neurosci. 2020;23:939–951. doi: 10.1038/s41593-020-0664-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giovannoni F, et al. Res. Sq. 2020 doi: 10.21203/rs.3.rs-25639/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]