Abstract
Objective
This study aimed to explore the prevalence of psychological disorders and associated factors at different stages of the COVID-19 epidemic in China.
Methods
The mental health status of respondents was assessed via the Patient Health Questionnaire-9 (PHQ-9), Insomnia Severity Index (ISI) and the Generalized Anxiety Disorder 7 (GAD-7) scale.
Results
5657 individuals participated in this study. History of chronic disease was a common risk factor for severe present depression (OR 2.2, 95% confidence interval [CI], 1.82–2.66, p < 0.001), anxiety (OR 2.41, 95% CI, 1.97–2.95, p < 0.001), and insomnia (OR 2.33, 95% CI, 1.83–2.95, p < 0.001) in the survey population. Female respondents had a higher risk of depression (OR 1.61, 95% CI, 1.39–1.87, p < 0.001) and anxiety (OR 1.35, 95% CI, 1.15–1.57, p < 0.001) than males. Among the medical workers, confirmed or suspected positive COVID-19 infection as associated with higher scores for depression (confirmed, OR 1.87; suspected, OR 4.13), anxiety (confirmed, OR 3.05; suspected, OR 3.07), and insomnia (confirmed, OR 3.46; suspected, OR 4.71).
Limitation
The cross-sectional design of present study presents inference about causality. The present psychological assessment was based on an online survey and on self-report tools, albeit using established instruments. We cannot estimate the participation rate, since we cannot know how many potential subjects received and opened the link for the survey.
Conclusions
Females, non-medical workers and those with a history of chronic diseases have had higher risks for depression, insomnia, and anxiety. Positive COVID-19 infection status was associated with higher risk of depression, insomnia, and anxiety in medical workers.
Keywords: COVID-19, Prevalence, Psychological disorder, China
1. Introduction
The coronavirus disease 2019 (COVID-19) outbreak emerged in Wuhan, Hubei, China in December 2019, and then spread rapidly to every continent except Antarctica, resulting in a pandemic. WHO reported 55,659,785 cumulative confirmed cases (574,440 newly confirmed cases) and 1338,769 cumulative death cases (November 19, update). In addition to placing a huge burden on cardiopulmonary health, the COVID-19 pandemic places considerable psychological stress on the general public, which can increase the risk of psychological decompensation, especially perhaps among health care workers (HCWs). In a survey conducted during the initial stage of the COVID-19 epidemic in China, about one-third of respondents among the general population had moderate-to-severe anxiety in relation to the disease (Wang et al., 2020). During earlier outbreaks of infectious diseases such as the H1N1 coronavirus or Ebola, common psychological responses included anxiety/fears, depression, anger, guilt, grief and loss, post-traumatic stress disorder, and stigmatization of survivors (Chew QH, 2020). However, no survey had hitherto been conducted to explore the evolution of the psychological responses of individuals at different stages of the COVID-19 epidemic. The extra burden of psychological stressors placed on HCWs during an epidemic are also a matter of concern (Shen et al., 2020; Sheng et al., 2020). During epidemics, HCWs suffering from pre-existing physical symptoms such as headaches are especially apt to experience anxiety, stress, and depression (Chew et al., 2020). Indeed, a body of research indicates that front-line HCWs, especially those working in close contact to infected patients, are susceptible to psychological disorders (Lu et al., 2020). Moreover, quarantined medical workers have had great restrictions placed on their social activities and interactions with family members and friends, which tends to increase the risk of decompensation due to inadequate social support. Arguably, paying excessive attention to media coverage to the crisis can itself be harmful to mental health. For example, one study indicated that people with the highest exposure to news media reported greater acute stress after the Boston Marathon Bombing than did some direct witnesses (Garfin et al., 2020). The present research aimed to assess the psychological responses of the general public at different stages of the COVID-19 epidemic, placing special focus on HCWs in the COVID-19 epicenter in Hubei province. We also attempted to identify risk factors for psychological decompensation in the face of the pandemic.
2. Aims of the study
The coronavirus disease 2019 (COVID-19) pandemic is having a profound effect on mental health as well as physical health of threatened populations around the world. Therefore, this study aimed to explore the prevalence of psychological disorders and associated factors at different stages of the COVID-19 epidemic in China. We conducted a cross sectional study of individuals nationwide in China, the country where the COVID-19 pandemic arose. The study involving 5657 individuals encompasses for the first time all phases of the Chinese COVID-19 epidemic, extending from early in the outbreak to the present remission.
3. Method
3.1. Study design and participants
This cross-sectional observational study ran from January 28 to March 31, 2020. The study began only five days after imposition of the lockdown in Wuhan as a measure to control the COVID-19 outbreak (Shen et al., 2020). The survey period thus corresponds to dynamic stages of the COVID-19 epidemic as experienced in China, namely, outbreak, and remission (Fig. 1 ). The online survey included questions on demographic and clinical variables. Individuals aged more than 15 years who provided informed consent electronically prior to registration were invited to engage in the online survey via the Wenjuanxing platform. Individuals who reported having suffered from baseline psychological problems or who were taking medications for diagnosed mental illnesses such as depression or anxiety disorders were excluded from this study. After submitting the survey, participants received a follow-up telephone call from mental health care workers, and were asked directly if they felt a need for psychological help. The study was approved by the institutional ethics board of Tongji Hospital, Tongji Medical College of Huazhong University of Science and Technology (ID: TJ-IRB20200327).
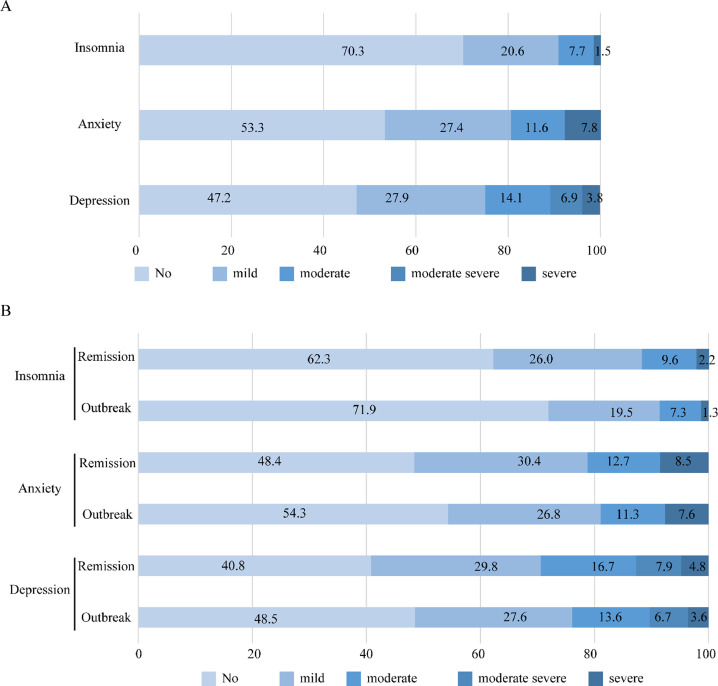
Fig. 1.
Distribution of the mental disorders in the total population and at different stages of the epidemic in China.
3.2. Measurements
Demographic data, i.e. sex, age (15 < age <25 years, 25–45 years old, or >45 years old), marital status (i.e., single or married), living in Wuhan (yes or no), living with families or friends (yes or no), education status (≤12 years, i.e. high school or lower as low education level and > 12 years, college or higher defined as high education level), and history of disease (yes or no) were collected, as well as the information specifically relating to COVID-19, i.e. suspected or confirmed infection, subject to quarantine, or in close contact with infected individuals. Moreover, depression, anxiety, and insomnia were assessed by using the Chinese versions of measurement tools, as described below.
The Patient Health Questionnaire-9 (PHQ-9) is a nine-item scale to detect the presence of depression conditions over the preceding two weeks. Each item is rated as 0 (not at all), 1 (for several days), 2 (at least half the time), and 3 (nearly every day). Severity of depression was ranked from the total scores, i.e. 0–4 (absent), 5–9 (mild), 10–14 (moderate), 15–19 (moderate-severe), and 20–27 (severe).The PHQ-9 has been validated and shows satisfactory reliability (Cronbach's alpha coefficient = 0.869), with excellent sensitivity and specificity (Kroenke et al., 2001).
Generalized Anxiety Disorder 7 (GAD-7) is a seven-item scale to identify anxiety disorders over the preceding two weeks. Each item is rated as 0, 1, 2, and 3, as described above for the PHQ-9. Severity of anxiety was ranked from the total scores, i.e. 0–4 (absent) 5–9 (mild), 10–14 (moderate), and 15–21 (severe). The GAD-7 scale has good reliability (Cronbach's alpha coefficient of 0.89) (Löwe et al., 2008). In addition, the effectiveness of the GAD-7 scale in assessing anxiety disorders has been confirmed in the Chinese population (Wu et al., 2019).
The Insomnia Severity Index (ISI) is a 7-item scale used to detect insomnia, where the severity of insomnia is ranked from the total score as (0–7) absent, 8–14 (mild), 15–21 (moderate), and 22–28 (severe). In testing of the Chinese version of ISI, the Cronbach's alpha coefficient was 0.81 (Morin et al., 2011).
3.3. Statistical analysis
Two researchers entered data into the database using Epidata.3.0 in a double-blind manner to guarantee accuracy. SPSS 22.0 was then used for statistical analysis. Since scores of PHQ-9, ISI, and GAD-7 did not have normal distributions, they were described using median and interquartile range (IQR). Categorical data were described using counts, and proportional and group differences were compared using χ2 tests. Binary logistic regression with stepwise variable selection was used in the multivariate factor analysis. Subgroup analyses were performed separately at the outbreak and remission stages, and contrasting HCWs s versus the general public, and among the three different age groups (15 < age <25 years, 25–45 years, and >45 years old). All hypotheses were tested at a significance threshold of p < 0.05.
4. Results
A total of 5676 participants agreed to participate in this online survey. Among all participants, 4725 (83.2%) were surveyed during the outbreak of COVID-19 epidemic; 951 (16.8%) were surveyed at the remission stage, 3460 (61.0%) were HCWs; 2669 (46.2%) lived in Wuhan during the epidemic, and 4050 (71.4%) were women. Most participants were aged 25 years old (4304[75.8%]), and 537 (9.5%) were in the adolescent-young adult group. A small proportion of participants (984 [17.3%]) lived alone, and most (4853 [85.5%]) had a bachelor's degree or higher degree (Table 1 ).
Table 1.
Demographic, occupational, and temporal characteristics of the surveyed participants.
| Stages, %(n) |
Occupation, %(n) |
Location, %(n) |
||||||
|---|---|---|---|---|---|---|---|---|
| Total, %(n) | Outbreak | Remission | HCWs | NHCWs | Wuhan | Hubeia | Other provinces | |
| Overall | 100(5676) | 83.2(4725) | 16.8(951) | 61.0(3460) | 39.0(2216) | 46.2(2669) | 29.0(1661) | 24.4(1396) |
| Sex, %(n) | ||||||||
| Male | 28.6(1626) | 27.5 (1301) | 34.2 (325) | 23.6(817) | 36.5(809) | 25.1(671) | 28.7(463) | 35.2(492) |
| Female | 71.4(4050) | 72.5 (3424) | 65.8 (626) | 76.4(2643) | 63.5(1407) | 74.9(1998) | 71.3(1148) | 64.8(904) |
| Age, %(n) | ||||||||
| <25 years old | 24.2(1371) | 25.3 (1195) | 18.5 (176) | 21.1(731) | 24.2(640) | 19.1(511) | 26.6(429) | 30.9(431) |
| 25–45 years old | 58.3(3307) | 58.0 (2739) | 59.7 (568) | 64.8(2242) | 48.1(1065) | 60.6(1618) | 58.7(945) | 53.3(744) |
| >45 years old | 17.6(997) | 16.7 (790) | 21.8 (207) | 14.1(486) | 23.1(511) | 20.2(540) | 14.7(237) | 15.8(220) |
| Education, %(n) | ||||||||
| ≤12 years | 14.5(823) | 14.7 (696) | 13.4 (127) | 7.9(272) | 24.9(551) | 13.8(369) | 15.6(251) | 14.5(203) |
| >12 years | 85.5(4853) | 85.3 (4029) | 86.6 (824) | 92.1(3188) | 75.1(1665) | 86.2(2300) | 84.4(1360) | 85.5(1193) |
| Marital status, %(n) | ||||||||
| Single | 31.1(1767) | 30.8 (1455) | 32.8 (312) | 30.8(1064) | 31.7(703) | 24.9(664) | 33.5(540) | 40.3(563) |
| Married | 68.9(3909) | 69.2 (3270) | 67.2 (639) | 69.2(2396) | 68.3(1513) | 75.1(2005) | 66.5(1071) | 59.7(833) |
| Living with others, %(n) | ||||||||
| Yes | 82.7(4692) | 83.3 (3937) | 79.4 (755) | 81.5(2819) | 84.5(1873) | 82.7(2206) | 83.6(1346) | 81.7(1140 |
| No | 17.3(984) | 16.7 (788) | 20.6 (196) | 18.5(641) | 15.5(343) | 17.3(463) | 16.4(265) | 18.3(256) |
| History of diseases, %(n) | ||||||||
| No | 85.0(3579) | 85.3 (2784) | 83.6 (795) | 87.4(1745) | 82.8(1834) | 81.2(1498) | 89.3(1289) | 85.5(792) |
| Yes | 15.0(634) | 14.7 (478) | 16.4 (156) | 12.6(252) | 17.2(382) | 18.8(346) | 10.7(154) | 14.5(134) |
| Living in city with over 1000 confirmed cases, %(n) | ||||||||
| Yes | 46.2(2601) | 44.5 (2082) | 54.6 (519) | 43.5(1484) | 50.4(1117) | 30.4(796) | 59.8(962) | 90.9(1267) |
| No | 53.8(3025) | 55.5 (2593) | 45.4 (432) | 56.5(1926) | 49.6(1099) | 69.6(1826) | 40.2(648) | 9.1(127) |
| Personal infection, %(n) | ||||||||
| Confirmed | 2.9(167) | 3.2 (152) | 1.6 (15) | 2.3(78) | 4.0(89) | 5.7(152) | 0.5(8) | 0.5(7) |
| Suspected | 1.8(101) | 2 (96) | 0.5 (5) | 2.2(76) | 1.1(25) | 2.8(74) | 0.9(15) | 0.9(12) |
| Quarantine | 5.1(290) | 5.5 (258) | 3.4 (32) | 6.8(234) | 2.5(56) | 5.7(152) | 4.0(65) | 5.2(73) |
| Close contacter | 29.2(1655) | 33.9 (1601) | 5.7 (54) | 46.9(1622) | 1.5(33) | 35(935) | 17.1(276) | 31.8(444) |
| No | 61.0(3463) | 55.4 (2618) | 88.9 (845) | 41.9(1450) | 90.8(2013) | 50.8(1365) | 77.4(1611) | 61.6(860) |
Other cities in Hubei province except for Wuhan.
A considerable proportion of participants had symptoms of depression (2998 [52.8%]), anxiety (2652 [46.7%]), or insomnia (1673 [29.7%]). Participants surveyed at the remission stage, females, nonmedical workers, and Wuhan residents reported more severe symptom levels of depression, anxiety, and insomnia than did those surveyed at the outbreak: severe depression among participants surveyed at the remission stage vs outbreak stage: 46 (4.8%) vs 171 (3.6%), p < 0.001; severe anxiety among women vs men: 329 (8.1%) vs 113 (6.9%) (P = 0.001); severe insomnia among NHCWs vs HCWs: 52 (2.3%) vs 31 (0.9%) (P < 0.001); severe insomnia among Wuhan residents: 49 (1.9%) vs Hubei province 22 (1.4%) and other provinces: 12 (0.9%) (both P = 0.01). (Table 2 ). The median (IQR) scores were 5.0 (2.0–9.0) for the PHQ-9 depression scale, 4.0 (1.0–9.0) for the GAD-7 anxiety scale, and 4.0 (1.0–8.0) for the ISI insomnia scale. Participants surveyed at the remission stage had higher scores in PHQ-9 and ISI scores than did those responding at the start of the outbreak, i.e. PHQ-9 scores: 6.0 [2.0–11.0] early vs 5.0 [2.0–9.0] late (P = 0.005); ISI scores: 6.0 [2.0–10.0] early vs 4.0 [1.0–8.0] late (P = 0.005). There were no epidemic-stage differences in scores of anxiety, i.e., GAD-7 scores: 5.0 (1.0–8.0) early vs 4.0 (1.0–7.0) late, (P = 0.149). Similar to findings for severity of symptoms, participants who were women, lived in Wuhan, and were non-HCWs had higher scores in all three instruments than did men, those living outside Wuhan (in Hubei province outside Wuhan or outside Hubei provinces), and HCWs (Table S1).
Table 2.
Severity categories of depression, anxiety, and insomnia complaints in the total population and different subgroups.
| Severity category, n (%) | Stages, n (%) |
Sex, n (%) |
Location, n (%) |
Occupation, n (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | Outbreak | Remission | p | Male | Female | P | Wuhan | Hubeia | Other provinces | p | HCWs | NHCWs | p | |
| PHQ-9, depression symptoms | ||||||||||||||
| Normal | 2678(47.2) | 2290(48.5) | 388(40.8) | <0.001 | 862(53) | 1816(44.8) | <0.001 | 1173(43.9) | 797(49.5) | 708(50.7) | <0.001 | 1730(50) | 948(42.8) | <0.001 |
| Mild | 1586(27.9) | 1303(27.6) | 283(29.8) | 427(26.3) | 1159(28.6) | 829(31.1) | 399(24.8) | 358(25.6) | 994(28.7) | 592(26.7) | ||||
| Moderate | 802(14.1) | 643(13.6) | 159(16.7) | 175(10.8) | 627(15.5) | 378(14.2) | 223(13.8) | 201(14.4) | 462(13.4) | 340(15.3) | ||||
| Moderate-severe | 393(6.9) | 318(6.7) | 75(7.9) | 102(6.3) | 291(7.2) | 190(7.1) | 122(7.6) | 81(5.8) | 198(5.7) | 195(8.8) | ||||
| Severe | 217(3.8) | 171(3.6) | 46(4.8) | 60(3.7) | 157(3.9) | 99(3.7) | 70(4.3) | 48(3.4) | 76(2.2) | 141(6.4) | ||||
| GAD-7, anxiety symptoms | ||||||||||||||
| Normal | 3024(53.3) | 2564(54.3) | 460(48.4) | 0.011 | 933(57.4) | 2091(51.6) | 0.001 | 1318(49.4) | 918(57) | 788(56.4) | <0.001 | 1910(55.2) | 1114(50.3) | <0.001 |
| Mild | 1553(27.4) | 1264(26.8) | 289(30.4) | 409(25.2) | 1144(28.2) | 793(29.7) | 401(24.9) | 359(25.7) | 942(27.2) | 611(27.6) | ||||
| Moderate | 657(11.6) | 536(11.3) | 121(12.7) | 171(10.5) | 486(12) | 318(11.9) | 180(11.2) | 159(11.4) | 383(11.1) | 274(12.4) | ||||
| Severe | 442(7.8) | 361(7.6) | 81(8.5) | 113(6.9) | 329(8.1) | 240(9) | 112(7) | 90(6.4) | 225(6.5) | 217(9.8) | ||||
| ISI, insomnia symptoms | ||||||||||||||
| Normal | 3953(70.3) | 3361(71.9) | 592(62.3) | <0.001 | 1176(72.9) | 2777(69.2) | 0.014 | 1812(69.1) | 1118(69.4) | 1023(73.4) | 0.01 | 2529(74.2) | 1424(64.3) | <0.001 |
| Mild | 1159(20.6) | 912(19.5) | 247(26) | 288(17.9) | 871(21.7) | 548(20.9) | 335(20.8) | 276(19.8) | 644(18.9) | 515(23.2) | ||||
| Moderate | 431(7.7) | 340(7.3) | 91(9.6) | 126(7.8) | 305(7.6) | 213(8.1) | 135(8.4) | 83(6) | 206(6) | 225(10.2) | ||||
| Severe | 83(1.5) | 62(1.3) | 21(2.2) | 23(1.4) | 60(1.5) | 49(1.9) | 22(1.4) | 12(0.9) | 31(0.9) | 52(2.3) | ||||
Other cities in Hubei province except for Wuhan.
The multivariate logistic regression analyses (Table 3 ) showed that younger age (<45 years old), living alone, history of diseases, non-HCW status and personal COVID-19 infection (suspected and quarantine) were common risk factors in the three outcomes (depression, anxiety and insomnia) for the entire population (all p < 0.05). Taking depression as an example, details of the five risk factors are as follows: younger age group (<25 years old, OR 2.09; 95% CI 1.66–2.63; 25–45 years old, OR 1.94, 95% CI 1.59–2.37), living alone (OR 1.56, 95% CI 1.32–1.84), history of diseases (OR 2.2, 95%CI 1.82–2.66), and personal COVID-19 infection (suspected, OR 2.5, 95% CI 1.63–3.83; quarantine, OR 2.02, 95% CI 1.50–2.71). Other risk factors of depression in the entire population were the remission stage of the epidemic (OR 1.22, 95% CI 1.03–1.44), female gender (OR 1.61, 95% CI 1.39–1.87), and single status (OR 1.26, 95% CI 1.08–1.47). Details of risk factors for anxiety and insomnia are shown in Table 3.
Table 3.
Risk factors of depression, anxiety, and insomnia in the cohort identified by the multivariate analysis.
| Characteristic | Depression |
Anxiety |
Insomnia |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Severe cases/ total cases (%) | OR (95% CI) | p | Severe cases/ total cases (%) | OR (95% CI) | p | Severe cases/ total cases (%) | OR (95% CI) | p | |
| Stage of the COVID-19 epidemic in China | |||||||||
| Remission | 1132/4725(24.0) | 1.22(1.03, 1.44) | 0.02 | 897/4725(19.0) | 1.22(1.02, 1.48) | 0.033 | 452/4725(9.6) | ||
| Outbreak | 280/951(29.4) | 1 | 202/951(21.2) | 1 | 112/951(11.8) | ||||
| Gender | |||||||||
| Females | 337/1626(20.7) | 1.61(1.39, 1.87) | <0.001 | 284/1626(17.5) | 1.35(1.15, 1.57) | <0.001 | 172/1626(10.0) | ||
| Males | 1075/4050(26.5) | 1 | 815/4050(20.1) | 1 | 402/4050(9.9) | ||||
| Age groups | |||||||||
| < 25 years old | 407/1371(29.7) | 2.09(1.66, 2.63) | <0.001 | 296/1371(21.6) | 1.86(1.48, 2.34) | <0.001 | 157/1371(11.5) | 1.58(1.17, 2.14) | 0.003 |
| 25–45 years old | 830/3307(25.1) | 1.94(1.59, 2.37) | <0.001 | 646/3307(19.5) | 1.63(1.33, 2.01) | <0.001 | 307/3307(9.3) | 1.49(1.12, 1.96) | 0.006 |
| > 45 years old | 174/997(17.5) | 1 | 156/997(15.6) | 1 | 100/997(10.0) | 1 | |||
| Dwelling state | |||||||||
| Living alone | 331/983(33.6) | 1.56(1.32, 1.84) | <0.001 | 237/984(24.1) | 1.43(1.20, 1.69) | <0.001 | 156/984(15.9) | 1.87(1.50, 2.32) | <0.001 |
| Living together | 1081/4692(23.0) | 1 | 862/4692(18.4) | 1 | 408/4692(8.7) | 1 | |||
| Having organic diseases | |||||||||
| Yes | 234/634(36.9) | 2.20(1.82, 2.66) | <0.001 | 196/634(30.9) | 2.41(1.97, 2.95) | <0.001 | 137/634(21.6) | 2.33(1.83, 2.95) | <0.001 |
| No | 892/3579(24.9) | 1 | 611/3579(17.1) | 1 | 394/3579(11.0) | 1 | |||
| Marital status | |||||||||
| Unmarried | 538/1767(30.4) | 1.26(1.08, 1.47) | 0.003 | 385/1767(21.8) | 196/1767(11.1) | ||||
| Married | 874/3909(22.4) | 1 | 714/3909(18.3) | 368/3909(9.4) | |||||
| Education level | |||||||||
| Senior highschool or lower | 245/823(29.8) | 195/823(23.7) | 126/823(15.3) | 1.60(1.25, 2.06) | <0.001 | ||||
| College or higher | 1167/4853(24.0) | 904/4853(18.6) | 438/4853(9.0) | 1 | |||||
| Occupation | |||||||||
| Nonhealthcare workers | 736/3460(21.3) | 1.88(1.61, 2.20) | <0.001 | 608/3460(17.6) | 1.77(1.49, 2.10) | <0.001 | 287/3460(8.30 | 1.25(1.00, 1.55) | 0.047 |
| Healthcare workers | 676/2216(30.5) | 1 | 491/2216(22.2) | 1 | 277/2216(12.5) | 1 | |||
| Personal infection | |||||||||
| Confirmed | 42/167(25.10 | 1.19(0.82, 1.73) | 0.357 | 41/161(24.60 | 1.65(1.13, 2.41) | 0.009 | 45/167(26.9) | 1.39(0.87, 2.22) | 0.165 |
| Suspected | 40/101(39.6) | 2.50(1.63, 3.83) | <0.001 | 34/101(33.7) | 2.77(1.79, 4.30) | <0.001 | 49/101(48.5) | 3.11(1.70, 5.69) | <0.001 |
| Quarantine | 92/290(31.7) | 2.02(1.50, 2.71) | <0.001 | 100/290(34.5) | 2.81(2.08, 3.79) | <0.001 | 32/290(11.0) | 1.94(1.28, 2.94) | 0.002 |
| Close contactor | 353/1655(21.3) | 1.50(1.19, 1.89) | 0.001 | 306/1655(18.5) | 1.36(1.05, 1.76) | 0.021 | 79/1655(4.8) | 1.41(1.02, 1.96) | 0.038 |
| No | 885/3463(25.6) | 1 | 618/3463(17.8) | 1 | 359/3463(10.4) | 1 | |||
Among the participants surveyed at the epidemic outbreak, living alone, history of diseases, and personal infection (suspected, quarantined, or close contactor) were common risk factors for depression, anxiety, and insomnia. In the depression model, details were as follows: living alone (OR 1.58, 95% CI 1.31–1.90), history of diseases (OR 2.06, 95% CI 1.65–2.57), and personal infection (suspected, OR 2.31, 95% CI 1.48–3.6; quarantined, OR 2.29, 95% CI 1.65–3.16; close contact OR 1.6 95% CI 1.24–2.07). The other four risk factors were female gender (OR 1.57, 95%CI 1.34–1.85), younger age groups (<25 years old, OR 2.07, 95% CI 1.61–2.67; 25–45 years old, OR 1.89, 95% CI 1.51–2.36), single status (OR 1.21, 95% CI 1.03–1.43), and non-HCWs (OR 2, 95% CI 1.68–2.39). As was the case at outbreak, there were six risk factors for depression in participants surveyed at the remission stage, as follows: female gender (OR 1.73, 95% CI 1.24–2.41), younger age groups (<25 years old, OR 1.89, 95% CI 1.01–3.53; 25–45 years old, OR 2.2, 95% CI 1.42–3.4), living alone (OR 1.52, 95% CI 1.05–2.21), history of diseases (OR 2.74, 95% CI 1.85–4.04), single status (OR 1.63, 95% CI 1.07–2.48), and non-HCW status (OR 1.5, 95% CI 1.1–2.05).
In the anxiety model, three risk factors were common in the subgroups of outbreak versus remission of the epidemic, i.e. younger age groups (<45 years old), history of diseases, and non-HCW status. Besides, the risk factors for anxiety were female gender (OR 1.32, 95% CI 1.11–1.58), living alone (OR 1.46, 95% CI 1.21–1.77), living in Wuhan (OR 1.18, 95% CI 1.01–1.38), and personal COVID-19 infection (suspected, OR 2.42, 95% CI 1.52–3.84; in quarantine, OR 3.09, 95%CI 2.22–4.3; close contactor, OR 1.37, 95% CI 1.03–1.82) in those surveyed at the outbreak.
In the insomnia model, risk factors in participants surveyed at the outbreak stage were living alone (OR 2.15, 95% CI 1.69–2.73), history of disease (OR 2.13, 95% CI 1.63–2.79), lower education level (OR 1.66, 95%CI 1.27–2.17), and personal infection (suspected, OR 2.43, 95% CI 1.25–4.72; quarantine, OR 2.04, 95% CI 1.28–3.24; close contact OR 1.51, 95% CI 1.09–2.11) (Table 4 ).
Table 4.
Factors associated with psychological problems in participants surveyed at different stages.
| Characteristic | Depression |
Anxiety |
Insomnia |
|||
|---|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | |
| At the outbreak of COVID-19 epidemic in China | ||||||
| Gender | ||||||
| Female | <0.001 | 1.57(1.34, 1.85) | 0.002 | 1.32(1.11, 1.58) | ||
| Male | 1 | 1 | ||||
| Living state | ||||||
| Living alone | <0.001 | 1.58(1.31, 1.90) | <0.001 | 1.46(1.21, 1.77) | <0.001 | 2.15(1.69, 2.73) |
| Living with partner or family | 1 | 1 | 1 | |||
| Age groups | ||||||
| < 25 years | <0.001 | 2.07(1.61, 2.67) | <0.001 | 1.76(1.37, 2.26) | ||
| 25–45 years | <0.001 | 1.89(1.51, 2.36) | 0.001 | 1.50(1.19, 1.89) | ||
| > 45 years | 1 | 1 | ||||
| Having organic diseases | ||||||
| Yes | <0.001 | 2.06(1.65, 2.57) | <0.001 | 2.28(1.81, 2.88) | <0.001 | 2.13(1.63, 2.79) |
| No | 1 | 1 | 1 | |||
| Marital status | ||||||
| Unmarried | 0.017 | 1.21(1.03, 1.43) | ||||
| Married | 1 | |||||
| Occupation | ||||||
| Nonhealthcare workers | <0.001 | 2.00(1.68, 2.39) | <0.001 | 1.83(1.50, 2.23) | ||
| Healthcare workers | 1 | 1 | ||||
| Living area | ||||||
| In Wuhan | 0.032 | 1.18(1.01, 1.38) | ||||
| Other than Wuhan | 1 | |||||
| Education level | ||||||
| Senior highschool or lower | <0.001 | 1.66(1.27, 2.17) | ||||
| College or higher | 1 | |||||
| Personal infection | ||||||
| Confirmed | 0.251 | 1.26(0.85, 1.86) | 0.119 | 1.39(0.92, 2.10) | 0.303 | 1.30(0.79, 2.12) |
| Suspected | <0.001 | 2.31(1.48, 3.60) | <0.001 | 2.42(1.52, 3.84) | 0.009 | 2.43(1.25, 4.72) |
| Quarantine | <0.001 | 2.29(1.65, 3.16) | <0.001 | 3.09(2.22, 4.30) | 0.003 | 2.04(1.28, 3.24) |
| Close contactor | <0.001 | 1.60(1.24, 2.07) | 0.028 | 1.37(1.03, 1.82) | 0.014 | 1.51(1.09, 2.11) |
| No | 1 | 1 | 1 | |||
| At the remission stage of COVID-19 epidemic in China | No variables entered | |||||
| Gender | ||||||
| Females | 0.001 | 1.73(1.24, 2.41) | ||||
| Males | 1 | |||||
| Age groups | ||||||
| < 25 years | 0.048 | 1.89(1.01, 3.53) | <0.001 | 2.74(1.56, 4.80) | ||
| 25–45 years | <0.001 | 2.20(1.42, 3.40) | <0.001 | 2.51(1.57, 4.00) | ||
| > 45 years | 1 | 1 | ||||
| Living status | ||||||
| Living alone | 0.026 | 1.52(1.05, 2.21) | ||||
| Living together | 1 | |||||
| Having organic diseases | ||||||
| Yes | <0.001 | 2.74(1.85, 4.04) | <0.001 | 2.88(1.92, 4.31) | ||
| No | 1 | 1 | ||||
| Marital status | ||||||
| Unmarried | 0.023 | 1.63(1.07, 2.48) | ||||
| Married | 1 | |||||
| Occupation | ||||||
| Nonhealthcare workers | 0.01 | 1.50(1.10, 2.05) | 0.034 | 1.43(1.03, 1.99) | ||
| Healthcare workers | 1 | 1 | ||||
Three variables were independently associated with insomnia in medical workers; living alone (OR 1.57, 95% CI, 1.15–2.14, p < 0.01), history of diseases (OR 2.81, 95% CI, 1.96–4.03, p < 0.01), and personal infection (confirmed, OR 3.46; suspected, OR 4.71; in quarantine, OR 2.36; close contactor, OR 1.65, p < 0.01). The five factors living alone (OR 2.05), history of disease (OR 2.04), single status (OR 1.42), lower education levels (OR 1.69) and suspected COVID-1 infection (OR 2.84) were significant risk factors for insomnia in non-HVWs (all pvalue < 0.05) (Table S2).
Factors associated with depression in young individuals included female gender (OR 1.92, 95% CI, 1.45–2.55, p < 0.01), history of diseases (OR 3.05, 95% CI, 2.02–4.6, p < 0.01), non-HCW status (OR 2.2, 95% CI, 1.64–2.95, p < 0.01), single status (OR 1.47, 95% CI, 1.12–1.93, p < 0.01), and personal COVID-19 infection status (suspected, OR 7.84; quarantined, OR 2.69; close contactors OR 1.75). Living alone (OR 2.55, 95% CI, 1.59–4.08, p < 0.01), history of diseases (OR 2.36, 95% CI, 1.61–3.45, p < 0.01) and personal infection status (quarantined, OR 2.63, 95% CI, 1.17–5.89, p = 0.02) were risk factors associated with prevalence of depression in individuals aged over 45 (Table S2).
5. Discussion
Our cross-sectional study enrolled 5676 respondents, who reported a high prevalence of psychological symptoms during the COVID-19 epidemic in China during the first half of 2020. Overall, the respondents reported high incidences of depression (53.8%), anxiety (46.7%), and insomnia (29.7%). Participants were divided in two groups interviewed at outbreak or at remission of the epidemic in China. Most respondents were female, aged over 25 years old, married, and were medical workers. We recorded more severe symptoms in all scales among those surveyed at the remission stage, women, those living in Wuhan, and non-HCS. Our study further indicated that the remission of the epidemic was associated with greater prevalence of severe depression and anxiety. Suspicion of being infected with COVID-19 was an independent risk factor for worse mental health in all relevant dimensions. Taken together, our findings raise special concerns about public mental health, especially among non-HCWs involved at the remission stage of the COVID-19 epidemic.
Our study reveals that considerable proportion of surveyed participants reported depression, anxiety, and insomnia. A cross-sectional epidemiological survey conduct by the China Mental Health Survey (CMHS) in 2019 suggested that 5.0% of Chinese adults had experienced anxiety in the preceding years, and 3.6% reported having had depression (Huang et al., 2019). Compared to those findings prior to the epidemic (Fu et al., 2020; Huang and Zhao, 2020), our study identified a much higher incidence of anxiety and depression during the outbreak and the resolution stages of the COVID-19 epidemic in Hubei, thus emphasizing the psychological burden of a major infectious disease presently having global impact. We concede that ourfindings are vulnerable to bias arising from our particular selection of measurement instruments. However, a main strength of our study lies in its encompassing of all phases of the Chinese COVID-19 epidemic, extending from early in the outbreak to the onset of remission.
In our study, the prevalence of psychosomatic complaints of depression, anxiety, and insomnia in the general public were higher at the resolution than at the outbreak stage. Several previous studies have focused on the acute impact of the COVID-19 epidemic on the mental health of ordinary Chinese citizens and HCWs. At the outbreak, over 70% of the general public in China had moderate to severe levels of psycholosomatic symptoms, specifically for traits of obsessive compulsion, interpersonal sensitivity, phobic anxiety, and psychoticism (Tian et al., 2020). Furthermore, over half of respondents rated their psychological impact as moderate or severe at the start of the outbreak (Wang et al., 2020).
The reasons for the greater psychological distress reported in the remission stage of the epidemic might be related to existential factors such as uncertainty about returning to work, loss of income, and the ongoing risk of COVID-19 infection associated with use of public transportation. Moreover, the increase in distress after the fact may be a response to the massive media coverage of the global outbreak. Ongoing lock-down in some regions, news coverage of tragic COVID-19 cases, and the risk of re-introduction of the disease in China, strengthen people's uncertainty about how long the crisis will continue to last. The delay in the development of effective vaccines and treatment intensified the general feeling of powerless against this disease.
Multivariate analysis showed that those living alone, those suffering from organic diseases, and non-HVWs had higher risk of reporting depression, anxiety, and insomnia symptoms. Previous studies revealed that living alone was associated with common psychosomatic disorders such as depression, anxiety, and insomnia (Jacob et al., 2019; Stahl et al., 2017). A population-based study from Finland, showed that participants living alone had a two-fold higher the risk of anxiety or depression than those living with a spouse or partner (Joutsenniemi et al., 2006). People with pre-existing organic diseases (especially cardiopulmonary disease and hypertension) are at heightened risk for succumbing to COVID-19, and are thus unsurprisingly at a higher risk for developing psychological problems in the face of the pandemic (Pfefferbaum and North, 2020). Lock-down policies have delayed hospitalization schedules, such as routine hemodialysis in renal failure patients, and elective surgery. We speculate that the greater psychological vulnerability of non-HCWs may be due to their greater risk of income loss. This epidemic has been especially devastating for travel-related industries that would otherwise have flourished during the traditional spring festival. During the SARS crisis in 2003, Asian countries lost about 12–18 billion dollars from reduced travel, tourism, and retail sales (E, 2010), and China experienced an estimated 1% decline in GDP (Qiu et al., 2018). The final tally of economic consequences of COVID-19 is likely to be much more severe.
In our study, half of all respondents experienced symptoms of anxiety, with a relatively higher incidence among female respondents, which is consistent with previous results showing that women are in general more vulnerable to anxiety disorders than are men (Gao et al., 2020; Guo et al., 2016). A previous study has also reported a greater increase of anxiety, stress and depression among women during the lockdown in India, as well showing that women reported a higher risk of stress and anxiety despite their social support and psychological resilience (Gopal et al., 2020). There are three potential reasons for this phenomenon. First, women could be confronted with an increase in their household responsibilities, leaving less time to care for themselves. Studies in North America showing that male academics have a higher publication rate than female academics gives indirect support for this conjecture (Gopal et al., 2020; Viglione, 2020). Second, the social restrictions led to a decrease in physical activity, especially among the female group. For instance, another internet-based study among pregnant women in Spain has suggested that their restrictions in physical mobility have brought a lessening of physical activity and their health-related quality of life (Bivia-Roig et al., 2020). According to the guidelines of WHO, the minimal requirement of adults aged between 18 and 64 years is 150 min of moderate or 75 of minutes of vigorous exercise per week (Bivia-Roig et al., 2020). A lack of physical activity and consequently lower quality of life could lead to adverse psychological outcomes among women, especially among the maternal group. The third potential reason for the gender difference could be the emergence of latent domestic hostility during the lockdown. Women across the world during the pandemic have been under a heightened risk for domestic violence, including emotional, physical, and sexual abuse (Chandan et al., 2020; Gopal et al., 2020; Mahase, 2020). Although there is no direct evidence of increased domestic violence in China during the lockdown, any such incidents would undoubtedly place great stress on the victimized women's mental health. In contrast, another study has found that pregnant women who delivered during the lockdown have shown reduced risk of depression compared to women who delivered at the same medical center before the COVID-19 pandemic, which reflect the increased availability of social support from family members in the context of a pregnancy, despite relative isolation due to lockdown (Pariente et al., 2020). However, some women who were using short-acting reversible contraception may have discontinued their contraceptive use during the pandemic, and consequently an unplanned pregnancy (Caruso et al., 2020). In this situation, the pregnancy might increase their risk of experiencing psychological disorders during this COVID-19 pandemic era. Our study indicated that medical workers had a considerable incidence of depression (50.0%), anxiety (44.8%), and insomnia (25.8%) symptoms. This concurs with findings in the context of various previous pandemics (Lu et al., 2020; Zhang WR, 2020). Furthmore, there are proposals for mitigating against the heavy psychological burden placed on HCWs by the current pandemic (Huang et al., 2019). Multivariate analysis of the present data suggested that suspicion of COVID-19 infection was associated with higher risk for the triad of psychological symptoms reported by HCWs. A previous study suggested that medical workers with professional contact with COVID-19 patients had higher risk anxiety and insomnia (Zhang, 2020). Furthermore, during the severe acute respiratory syndrome (SARS) epidemic, HCWs at the affected hospitals experienced immediate and long-lasting psychological impact (McAlonan et al., 2007; Wu et al., 2009). The retrospective findings in another cross-sectional survey have shown that records dating from before and during the pandemic did not indicate a significant burden of anxiety and depression among HCWs in general, while subgroups of positive-testing HCWs and HCWs with sleep disturbances had a significantly increased risk for anxiety. Furthermore, the previous report suggested that HCWs with positive test and/or sleep disorders should receive supplementary mental health support interventions (Magnavita et al., 2020).
The present study has several limitations. First, we applied a cross-sectional design, although a longitudinal approach might be better suited to quantify the development of allostatic overload “wear and tear” due to persistent stress among HCWs, and to determine if the self-reported psychosomatic complaints meet the criteria of psychiatric diagnoses such as major depressive disorder of post-traumatic stress disorder (PTSD). Second, the present psychological assessment was based on an online survey and on self-report tools, albeit using established instruments. Third, we cannot estimate the participation rate, since we have no way of knowing how many subjects received and opened the link for the survey.
Funding
This work was suppoted by the Fundamental Research Funds for the Central Universities (grant numbers 2020kfyXGYJ002).
Author contribution
YY, SQZ and MHW conceived and designed the study. YY and SQZ managed the project. MHW, QZ, CHH, YW, JC, SSH, JL, YZH and QML collected the data. MHW, ZLG, LW, LM, SZ, HMW, CLZ, WJL, CSG, CFC, JMY and YC did the statistical analysis. MHW, KX, HXY, YY, LHY, QW, PYZ, GL and YXF wrote the initial draft. All authors subsequently critically edited the report, and all read and approved the final edition.
Date availability statement
All data generated or analysed during this study are included in this published article.
Declaration of Competing Interest
All authors are no conflict of interest exists in carrying out this study and writing this manuscript.
Acknowledgement
We thank Jiahuan Hao and Jia Li (Department of Neurology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China) for providing valuable comments for this manuscript. We thank Professor Paul Cumming for his excellent work on proofreading the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.11.118.
Appendix. Supplementary materials
References
- Bivia-Roig G., La Rosa V.L., Gomez-Tebar M., Serrano-Raya L., Amer-Cuenca J.J., Caruso S., Commodari E., Barrasa-Shaw A., Lison J.F. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an Internet-based cross-sectional survey. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17165933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruso S., Rapisarda A.M.C., Minona P. Sexual activity and contraceptive use during social distancing and self-isolation in the COVID-19 pandemic. Eur. J. Contracept. Reprod. Health Care. 2020;25:445–448. doi: 10.1080/13625187.2020.1830965. [DOI] [PubMed] [Google Scholar]
- Chandan J.S., Taylor J., Bradbury-Jones C., Nirantharakumar K., Kane E., Bandyopadhyay S. COVID-19: a public health approach to manage domestic violence is needed. Lancet Public Health. 2020;5:e309. doi: 10.1016/S2468-2667(20)30112-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Khan Ahmed, F. Napolean Shanmugam, G. Sharma, K. A., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew QH W.K., Vasoo S., Chua H.C., Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Med. J. 2020 doi: 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E W. Dilemmas of securitization and health risk management in the People’s Republic of China: the cases of SARS and avian influenza. Health Policy Plan. 2010;25:454–466. doi: 10.1093/heapol/czq065. [DOI] [PubMed] [Google Scholar]
- Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., Mao J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry. 2020;10:225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao W., Ping S., Liu X. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J. Affect. Disord. 2020;263:292–300. doi: 10.1016/j.jad.2019.11.121. [DOI] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopal A., Sharma A.J., Subramanyam M.A. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0240650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X., Meng Z., Huang G., Fan J., Zhou W., Ling W., Jiang J., Long J., Su L. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015. Sci. Rep. 2016;6:28033. doi: 10.1038/srep28033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wang Y., Wang H., Liu Z., Yu X., Yan J., Yu Y., Kou C., Xu X., Lu J., Wang Z., He S., Xu Y., He Y., Li T., Guo W., Tian H., Xu G., Xu X., Ma Y., Wang L., Wang L., Yan Y., Wang B., Xiao S., Zhou L., Li L., Tan L., Zhang T., Ma C., Li Q., Ding H., Geng H., Jia F., Shi J., Wang S., Zhang N., Du X., Du X., Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group. Psychol. Health Med. 2020:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Jacob L., Haro J.M., Koyanagi A. Relationship between living alone and common mental disorders in the 1993, 2000 and 2007 National Psychiatric Morbidity Surveys. PLoS ONE. 2019;14 doi: 10.1371/journal.pone.0215182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joutsenniemi K., Martelin T., Martikainen P., Pirkola S., Koskinen S. Living arrangements and mental health in Finland. J Epidemiol Community Health. 2006;60:468. doi: 10.1136/jech.2005.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita N., Tripepi G., Di Prinzio R.R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17145218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. Covid-19: EU states report 60% rise in emergency calls about domestic violence. BMJ. 2020;369:m1872. doi: 10.1136/bmj.m1872. [DOI] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariente G., Wissotzky Broder O., Sheiner E., Lanxner Battat T., Mazor E., Yaniv Salem S., Kosef T., Wainstock T. Risk for probable post-partum depression among women during the COVID-19 pandemic. Arch. Womens Ment. Health. 2020 doi: 10.1007/s00737-020-01075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Qiu W., Chu C., Mao A., Wu J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J. Environ. Public Health. 2018 doi: 10.1155/2018/2710185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen X., Zou X., Zhong X., Yan J., Li L. Psychological stress of ICU nurses in the time of COVID-19. Crit. Care. 2020;24:200. doi: 10.1186/s13054-020-02926-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheng X., Liu F., Zhou J., Liao R. [Psychological status and sleep quality of nursing interns during the outbreak of COVID-19] Nan Fang Yi Ke Da Xue Xue Bao. 2020;40:346–350. doi: 10.12122/j.issn.1673-4254.2020.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl S.T., Beach S.R., Musa D., Schulz R. Living alone and depression: the modifying role of the perceived neighborhood environment. Aging Ment. Health. 2017;21:1065–1071. doi: 10.1080/13607863.2016.1191060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viglione G. Are women publishing less during the pandemic? Here’s what the data say. Nature. 2020;581:365–366. doi: 10.1038/d41586-020-01294-9. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P F.Y., Guan Z., et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S.M., Wu B., Liu M., Chen Z.M., Wang W.Z., Anderson C.S., Sandercock P., Wang Y.J., Huang Y.N., Cui L.Y., Pu C.Q., Jia J.P., Zhang T., Liu X.F., Zhang S.M., Xie P., Fan D.S., Ji X.M., Wong K.S.L., Wang L.D., Wei C.C., Wang Y.N., Cheng Y.J., Zhou D., He L., Liu J.F., Zhang S.T., Tao W.D., Hao Z.L., Wang D.R., Zhang S.H., Liu Y.H., Li X., Dong Q., Zeng J.S., Peng B., Xu Y., Yang Y., Wang Y.L., Li Z.X., Zhao G., Wang W., Xu Y.M., Yang Q.W., He Z.Y., Wang S.S., You C., Gao Y., Yang J., Lei C.Y., Zhao Y.H., China Stroke Study, C. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18:394–405. doi: 10.1016/S1474-4422(18)30500-3. [DOI] [PubMed] [Google Scholar]
- Zhang W., Wang K., Yin L., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.