Abstract
The high mortality rate of breast cancer is mainly caused by the metastatic ability of cancer cells, resistance to chemotherapy and radiotherapy, and tumor regression capacity. In recent years, it has been shown that the presence of breast cancer stem cells is closely associated with the migration and metastatic ability of cancer cells, as well as with their resistance to chemotherapy and radiotherapy. The tumor microenvironment is one of the main molecular factors involved in cancer and metastatic processes development, in this sense it is interesting to study the role of platelets, one of the main communicator cells in the human body which are activated by the signals they receive from the microenvironment and can generate more than one response. Platelets can ingest and release RNA, proteins, cytokines and growth factors. After the platelets interact with the tumor microenvironment, they are called "tumor-educated platelets." Tumor-educated platelets transport material from the tumor microenvironment to sites adjacent to the tumor, thus helping to create microenvironments conducive for the development of primary and metastatic tumors. It has been observed that the clone capable of carrying out the metastatic process is a cancer cell with stem cell characteristics. Cancer stem cells go through a series of processes, including epithelial-mesenchymal transition, intravasation into blood vessels, movement through blood vessels, extravasation at the site of the establishment of a metastatic focus, and site colonization. Tumor-educated platelets support all these processes.
Keywords: Breast cancer stem cells, Platelets, Metastasis, Tumor microenvironment, Epithelial-mesenchymal transition
Core Tip: Cancer is a complex disease with several unknown mechanisms. The main aim of this work is to highlight the key role of platelets as communicator cells and their crucial role in cancer progression and second metastatic foci. This review focuses on the role of platelets in the tumor microenvironment as well as the interaction of molecules from platelets and breast cancer stem cells involved in cancer.
INTRODUCTION
Cancer is a multifactorial disease associated with a broad spectrum of molecular alterations inside the cells and the cellular microenvironment[1]. Cancer progresses mainly due to (1) uncontrolled cellular division; (2) alterations in the mechanisms that regulate cell death; (3) epithelial-mesenchymal-transition; (4) intravasation of tumor cells into the circulatory system; (5) cell migration to distant sites; (6) extravasation of tumor cells to initiate new foci; and (7) metastatic tumor development[2].
Breast cancer (BC) is a complex disease characterized by high cellular heterogeneity that comprises[3] a tumor microenvironment[4] and a stem cell niche[3]. BC is the leading cause of cancer death in women worldwide[5]. The lymphatic system is the main system involved in breast tissue drainage[6]. In BC, this is of high relevance due to its role in tumor cell dissemination and subsequent metastatic tumor development. The flow rate through the lymphatic system is 100 to 500 times greater than through blood vessels, and its shear force is lower due to the higher dilation capacity of lymphatic vessels; this means that metastatic cells traveling through the lymphatic system are much more likely to succeed in colonizing a second microenvironment[7].
BC is one of the most studied cancers; however, several molecular processes associated with BC are still unknown. There are various risk factors associated with BC development, such as estrogen production by menopause, or by nulliparity, a sedentary lifestyle, alcoholism, obesity, ionizing radiation, hormonal therapy, age, sex, family history, among others[8,9]. According to a report by The Global Cancer Observatory (a division of the World Health Organization), in 2018, there were 2088849 incident cases of BC and 626679 deaths worldwide[5].
Despite the tremendous histological diversity of breast tumors, a molecular classification system has been developed based on the expression of progesterone receptors (PR), estrogen receptors (ER), and the epidermal growth factor-2 (HER2)[10]. This classification system divides BC tumors into luminal-A, positive for ER and positive for PR, but negative for HER2; Luminal B, ER-positive, PR-negative, and HER2-positive; HER2, ER-negative, PR-negative, but HER2-positive. Triple-negative (TNBC) or basal-like, ER-negative, PR-negative, and HER2-negative[10].
PR and ER are expressed in the membrane of tumor cells and depend on their ligands to proliferate[11]. HER2+ tumor cells have many copies of the HER2 gene and high levels of the HER2 protein, which probably play a role in the accelerated growth of tumors[12]. Breast tumors classified as triple-negative are common in Black and Latino ethnic groups and are found more frequently in younger women[13].
The treatment and prognosis of a patient are closely related to the molecular subtype of BC present[10]. It has been reported that the subtype with the best prognosis is luminal A, while the one with the worst prognosis is triple-negative[14].
Breast cancer has a highly complex biological and molecular behavior as each cell subtype sends different signals to the tumor microenvironment, in this sense, each signal contributes in a different way to cancer cell differentiation, tumor growth rate and metastasis development. Also, BC stem cells and platelets are two crucial players that participate in BC malignancy and metastasis development, transferring signals and regulation factors through the whole process.
BREAST CANCER STEM CELLS
Breast cancer stem cells (BCSCs), also called breast cancer-initiating cells, are a subpopulation of cells within the tumor that can self-renew and produce different tumor cell lines by asymmetric division. The BCSC population is responsible for developing and maintaining the tumor mass through the expression of survival factors, proliferation and migration[3,10]. BCSCs are regulated through interactions with growth factors and cytokines produced by mesenchymal stem cells (MSCs), cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs) and the extracellular matrix (ECM)[15]. These interactions help stimulate CSC self-renewal, induce angiogenesis and promote invasion by tumor cells and their migration towards new tumor foci.
BCSCs have unique characteristics, including an unlimited capacity for self-renewal, resistance to chemotherapy, the ability to induce the formation of new blood vessels to feed the tumor[3,15] and due to their plasticity, the ability to transition between two states reversibly (epithelial-mesenchymal transition, EMT), which allows them to migrate through the lymphatic and blood systems and establish metastatic foci in distant tissues with the help of platelets[3,16].
Two main models explaining tumor origin have been described: (1) The stochastic or clonal evolution classic model does not contemplate CSCs existence; in this model, each cell can induce tumor development throughout mutations. The model assumes that cancer cell clones produced by genomic abnormalities randomly accumulated could explain heterogeneity[3,17]; and (2) The tumorigenesis model considers CSC existence and postulates that cancer arises from stem cells with unlimited self-renewal capacity. According to this model, cancer originates from poorly differentiated cells with epigenetic mutations and unlimited replication capacity[3,18].
BCSCs can be distinguished from other tumor cells by the presence of cell surface markers EpCAM+, CD24-/Low, and CD44+[16,19]. EpCAM, or epithelial cell adhesion molecule, is a transmembrane glycoprotein that participates in intracellular signaling, proliferation, differentiation, and tumorigenic and metastatic processes[20]. CD44 regulates cell-cell and cell-ECM interactions through hyaluronic acid. It participates in cell adhesion, proliferation, survival, and differentiation[21]. CD44 plays an essential role in cancer development as it is responsible for maintaining the multipotentiality of BCSCs[21]. CD24 is a sialoprotein that participates in adhesion, proliferation, and metastasis; its upregulation inhibits the activity of BCSCs[22].
CD49f and ALDH1 are other cell surface markers found in BCSCs that are associated with chemoresistance; therefore, their presence is associated with a poor prognosis and reduced patient survival. CD49f, also known as α6-integrin, binds to laminin and facilitates the adhesion of epithelial cells to the ECM. ALDH1 is a cytosolic isoenzyme that catalyzes the oxidation of retinol to retinoic acid[23].
Li et al[3] indicated that all mammary tumor subtypes are produced by luminal stem cells. According to these authors, the different mammary tumor subtypes have a single origin that, due to different epigenetic and oncogenic events, are dispersed into the different known BC subtypes.
Different cell surface markers have been observed in BCSCs depending on the cells' EMT state[16,24]. EMT is a process characterized by the loss of apicobasal polarity, loss of intracellular junctions and ECM junctions, and changes in the cytoskeleton[16,25] that make BCSCs, which have epithelial morphology, acquire a mesenchymal phenotype that allows travel through the blood or lymphatic vessels to reach distant sites and create metastatic foci. The phenotype of BCSCs in the EMT state is CD24-CD44+ E-cadherin- EpCAM- Vimentin+ ALDH+. BCSCs that are in the mesenchymal-epithelial transition (MET) state have a phenotype E-cadherin+ EpCAM+and Vimentin-[19,24,26]. The transition between these states is induced by several factors contained in the tumor microenvironment[16,24]. The inflammatory immune response and hypoxia[27], for example, are EMT inducers in BCSCs. Transforming growth factor β (TGF-β) induces EMT by downregulating epithelial proteins such as E-cadherin and upregulating factors like Twist and Snail, which induce the mesenchymal state[28-31]. TGF-β also supports BCSC functions via Wnt[32] and FAK[33] and promotes the expression of vimentin[26].
Labelle et al[25] reported that BC cells exposed to platelets treatment developed a mesenchymal phenotype; additionally, when these cells were also subjected to treatment with TGFβ, their invasive and metastatic capacity increased. These results indicate that platelets and TGFβ act synergistically and can produce cells with characteristics of BCSCs[25].
In 2014, Asiedu et al[34] showed that AXL upregulation by a member of the TAM family (Tyro3, Axl, Mer; tyrosine kinase receptors) increases the tumorigenic capacity, invasion, and metastasis of BC cells, while AXL downregulation reverses EMT in BCSCs and restores chemosensitivity. AXL regulates several signal transduction pathways, including NF-k β, STAT, Akt, and MAPK. Asideu et al[34] demonstrated that AXL is constitutively activated in BCSCs and that it induces EMT by regulating E-cadherin, N-cadherin, Snail, and Slug expression.
It has been shown that BCSC activity is also regulated by signals from the Notch, Hedgehog, Wnt/ β-catenin, p53, and TGF-β pathways[16,32], helping to maintain cell survival and proliferation and, in this way, contributing to the growth of breast tumors.
TUMOR MICROENVIRONMENT
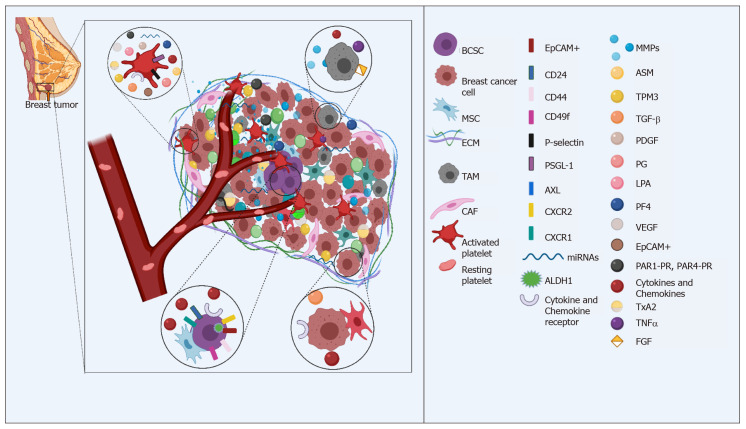
The tumor microenvironment (TME) is constituted by the ECM, CAFs, MSC, TAMs, and inflammatory cells (ICs)[35]. The TME is also constituted by soluble active biomolecules such as cytokines, growth factors, ligands, membrane-anchored molecules, secretion proteins and RNAs (miRNAs, lncRNAs)[28,36] (Figure 1).
Figure 1.
Tumor microenvironment in breast cancer. The figure describes the microenvironment present in cancer development. The tumor grows in an allowable microenvironment delimited by an extracellular matrix and inside there is a series of biomolecules such as cytokines, chemokines, miRNAs, growth factors. Furthermore, different cell types, such as breast cancer stem cells, platelets, tumor-associated macrophages, mesenchymal stem cells, and cancer-associated fibroblasts, contribute to the optimal conditions for cancer development. Biomolecules and cells, all orchestrate to promote tumor growth, angiogenesis, epithelial-mesenchymal transition, and metastasis. Created by Biorender.com. BCSC: Breast cancer stem cells; MSC: Mesenchymal stem cell; ECM: Extracellular matrix; TAM: Tumor-associated macrophage; CAF: Cancer-associated fibroblast. Created with Biorender.com
All the interactions that dictate the behavior of the tumor take place in the TME. This behavior can include a reversion to healthy tissue states or progression to the most advanced and deadly stages of the disease. Some of the interactions in the TME that promote cancer development, such as angiogenesis and metastasis, are discussed below.
The ECM provides attachment sites to normal and tumor stem cells, allowing them to interact with signals from other cells or from the TME that plays a role in their maintenance and regulation. It is through the ECM that CSCs that have experienced EMT can exit to points distant from the primary tumor[24]. It has been reported that in BC, the ECM increases its rigidity, which promotes TAZ protein activation[36], one of the main effectors of the Hippo pathway, responsible for controlling organ size by regulating cell proliferation, apoptosis and stem cell renewal[37].
MSCs regulate BCSCs through the loops of cytokines IL-6 and CXCL7; IL-6 is produced by MSCs and other immune cells present in the TME[38]. The interaction between IL-6 and the ILR 6/gp130 receptor present in BC cells induces CXCL7 production. In turn, CXCL7 induces IL-6, IL-8, CXCL6 and CXCL5 secretion, all of them with the ability to stimulate the self-renewal of BCSCs, which leads to tumor growth, metastasis and chemotherapy resistance[39].
TAMs are also part of the TME; they accumulate in hypoxic microenvironments and are the main orchestrators of an inflammatory TME. They promote cancer cell proliferation, invasion, and metastasis, stimulating angiogenesis and inhibiting the T-cell-mediated antitumor immune response. Furthermore, they play a crucial role in the regulation of EMT[40].
TAMs secrete TNF-alpha[41], which induces EMT through the NF-κβ pathway[42], and also induce an increased expression of Slug, Snail, and Twist[40]. Furthermore, TAMs indirectly increase the self-renewal capacity of BCSCs by maintaining constant communication with TGF-β[40].
To support tumor angiogenesis, TAMs produce angiogenesis-modulating enzymes[43] such as the metalloproteinases MMP-2, MMP-7, MMP-9, MMP12, and cyclooxygenase 2[43,44]. They also release cytokines (CXCL12, CCL2, CXCL8, CXCL1, CXCL3, and CCL5) that play a crucial role in different processes associated with cancer development[45].
Micro-RNAs (miRNAs) are also associated with the TME. These molecules are small non-coding RNAs that participate in various cellular functions, are found in large numbers in the TME, and are essential for the maintenance, development, and progression of cancer[36]. They are also critical regulators of the signaling pathways associated with cell stemness. The presence of oncogenic miRNAs in the TME is partly explained by their increase during specific transcription and by their release by tumor-educated platelets[46,47].
Several miRNA clusters, such as miR-183, miR-221–222, let-7, miR-142, and miR-214, play a role in the maintenance of BCSCs[47]. Others, such as let-7, miR-7, miR-10, and miR-15a, have been associated with BCSC chemoresistance ability[48]. EMT and MET transitions are also regulated by miRNAs clusters, including mir-9, mir-100, mir-221, and mir-155 as EMT inducers, while mir-200, mir-205, and mir-93 induce MET[49]. MiR-939 induces the EMT process by reducing E-cadherin and Claudin expression[50].
The p53 protein depletion in tumor cells reduces miR-200c expression[51], induces EMT development, and provides stem cell-like properties. The p53 activation reduces the expression of Snail and other EMT-inducing transcription factors through the upregulation of the miR-34 family[52].
The miRNAs found in the TME can come from platelets or platelet microparticles (PMPs). PMPs are the most abundant microparticles in the blood and contain, in addition to miRNAs[53], several EMT-promoting factors, including basic fibroblast growth factor (bFGF), fibroblast growth factor (FGF)[54], platelet-derived growth factor (PDGF)[55], hepatocyte growth factor (HGF)[56], TGF-β[57], vascular endothelial growth factor (VEGF)[58] and brain-derived neurotrophic factor/tropomyosin-related kinase (BDNF/TRK)[59].
TGF-β secreted by PMPs allows the overexpression of miR-183, which decreases the expression of DAP12, a receptor of natural killer cells (NKs) that plays a crucial role in membrane potential stabilization and signal transduction in these cells. The result is an increase in the survival of migratory cancer cells within blood vessels[60].
The transcription factor NF-kB participates in the regulation of metastasis and the induction of EMT. The activation of NF-κB is associated with a change of the TGFβ factor from a tumor-inhibiting role to a prometastatic role. The direct contact of platelet-derived TGFβ with tumor cells activates the TGFβ/Smad and NF-κB pathways in cancer cells, promoting EMT, and increasing metastasis in vivo[25,57].
It has been widely reported that a chronic inflammatory microenvironment promotes tumor development[4]. These inflammatory microenvironments are usually enriched with several lipid mediators such as platelet-activating factor (PAF)[61], prostaglandin (PG)[62] and lysophosphatidic acid (LPA)[63], all of which are secreted by platelets, by different types of immune cells during inflammation and by BC cells after stimulation with growth factors. These lipid mediators play an essential role in platelet aggregation and neo-angiogenesis[61-63]. The PAF has been shown to play an essential role in the onset and progression of BC and plays a predominant role in neo-angiogenesis[61]. Ward et al[64] reported that LPA release by the GPCR CD97 complex activates platelets and improves the permeability of tumor cells within blood vessels, which results in a higher capacity for invasiveness[64].
ROLE OF PLATELETS IN CANCER PROGRESSION AND METASTASIS
Platelets were discovered by the Italian physician Giulio Bizzozero in 1882. In 1906, JH Wright described them as anuclear cell fragments derived from megakaryocytes[65].
Platelets are widely known as the most critical first response factor in (1) coagulation, vasoconstriction, and inflammation, facilitating sterilization, tissue repair, and resolution; (2) they are the first to detect, phagocytize and react to pathogens in the circulation; (3) they maintain vascular integrity by hemostasis; (4) heal wounds; and (5) initiate and coordinate intravascular immune responses during infections and cancer[66,67].
The secretome of platelets is made up of more than 300 biomolecules, mainly in dense granules, alpha granules, and lysosomes. The presence of these biomolecules in the granules may be explained by the endocytosis and biosynthesis processes that take place in the megakaryocyte from which platelets originate[68].
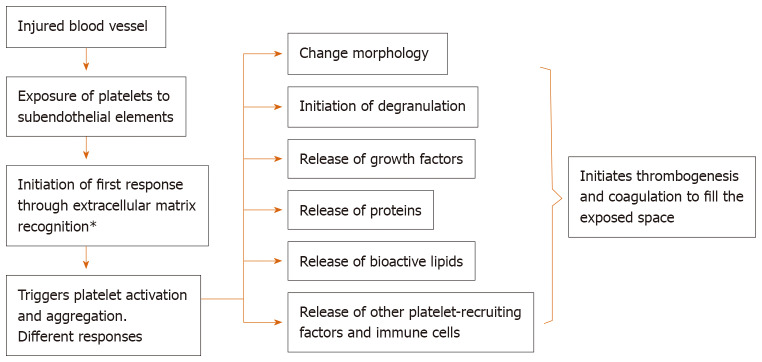
One of the properties of platelets as first responder cells is the ability to actively migrate through any inflamed or leaking vessel wall, in response to a variety of stimuli, in order to aid in wound sterilization and tissue regeneration[66] (Figure 2).
Figure 2.
The role of platelets in wound biology. The response by platelets depends on the recognition of extracellular matrix receptors[1]. These receptors can be proteoglycans, laminin, vitronectin, and various collagen isoforms.
Platelet morphology changes according to the state they are in. When they are in a resting state, platelets assume a discoid shape that maximizes interactions with flat surfaces[69,70]. In this state, platelets travel out of blood vessels and, after coming into contact with external microenvironmental factors, become activated, and their cytoskeleton undergoes a series of changes that result in the development of filopodia, which enlarge the cell contact surface and allows platelets to provide a highly rapid response to tissue injuries[70].
There are two ways by which platelets manage to disseminate the information they collect from the various microenvironments in which they are present. The first is by shedding membrane-enclosed cell fragments or microvesicles such as PMPs. These are also known as platelet-derived microvesicles (PMVs), which range in size from 100 to 1000 nm or others such as exosome-like microvesicular bodies range in size from 40–100 nm, that carry a wide variety of biomolecules such as miRNAs, growth factors and cytokines, among others. The second way by which platelets disseminate information is membrane fusion[71].
The platelet content is enriched by the various microenvironments through which they circulate. When circulating through the TME, platelets incorporate tumor-associated molecules, including molecules from TMAs or CSC niches that can support the growth of the original tumor or help establish secondary metastatic foci. These platelets are called "tumor-educated platelets" (TEPs)[72].
The molecules secreted by platelets include nitric oxide (NO), a bioactive compound that modulates angiogenesis, the immune response and neural regulation[73]. It is synthesized by nitric oxide synthase (NOS2) during the oxidation of L-arginine and has been shown to decrease the apoptosis of human lung carcinoma cells. In BC, NOS2 is a biomarker of disease progression and prognosis. NOS2 also mediates angiogenesis and the immune response in the TME, which are critical factors in cancer development[73,74].
In 2016, Banskota et al[75] demonstrated that serotonin is also released by platelets, inducing the production of reactive oxygen species (ROS) derived from NADPH oxidase (NOX) in tumor cells[75]. ROS production occurs as a result of alterations in the functions of mitochondria, associated with the development and progression of various diseases, including cancer[76]. In cancer, ROS production promotes the activation of the epidermal growth factor receptor (EGFR), which has been identified as a tumorigenesis driver and tumor resistance biomarker[77]. EGFR is capable of inhibiting anoikis, a form of programmed cell death caused by the detachment of cells from the ECM through activation of the extracellular signal-related kinases (ERK) pathway[78], which is associated with cell proliferation, migration, apoptosis, differentiation and senescence.
Along with ATP[67,79], platelets release other metabolites, such as thromboxane A2 (TxA2), 12-HETE[80] and serotonin[65], which, by regulating the permeability of blood vessels, allow TEPs and other cells with a migratory phenotype to move through blood vessels and colonize secondary metastatic foci[72,79]. In 2013, Schumacher et al[81] demonstrated that TEPs release adenine nucleotides (ATP) from their dense granules, which act on the P2Y2 receptors of endothelial cells, disrupting the adhesive junctions of endothelial cells and opening the endothelial barrier of blood vessels, which allows tumor cells to exit the bloodstream and travel to new metastatic foci[81].
The platelet's role in coagulation has been widely studied. Tissue Factor (TF), also called platelet tissue factor, is a transmembrane glycoprotein that binds to the coagulation serine protease factor VII/VIIa (FVII/VIIa) and is activated when a blood vessel is injured, triggering the coagulation cascade (extrinsic pathway). Fibroblasts typically express TF on blood vessel walls[82]. Its presence promotes thrombin production and platelet activation, which has been associated with cancer, contributing to the survival of cancer cells and metastasis[83]. In 2015, Orellana et al[84] showed that exposure to platelets increases TF expression in cancer cells[83]. As cancer cells can also express TF on their cell membrane, they can activate the coagulation cascade, which leads to the production of thrombin and the activation of platelets[83,84]. Thrombin is a crucial mediator of the metastatic process participating in both angiogenesis and cell migration and is capable of inhibiting apoptosis and inducing the proliferation and differentiation of vascular progenitor cells[85].
It has been reported that endothelial cells stimulated by thrombin induce morphology changes related to an EMT phenotype, which, as discussed, is associated with the loss of adhesive cell-cell junctions and migration to blood vessels[86].
Platelets also express multiple receptors on their surface that are activated according to signals they receive from the microenvironment. These receptors can generate different responses, including hemostasis, thrombosis, inflammation and tissue remodeling, but also the promotion of cancer cell survival and metastasis[67,72]. Mice that have been depleted of platelets or have a deficiency in granule content do not develop metastasis[87]. Other studies have shown that the proteins released by platelets influence the degree of malignancy of breast tumor cells, contributing to the generation of a more aggressive and metastatic phenotype[88].
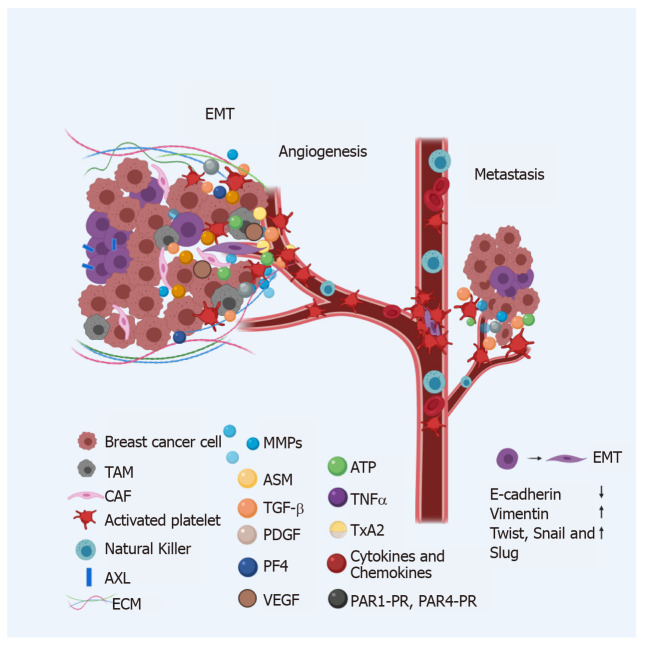
Once CSCs acquire the migratory phenotype through EMT and are ready to start moving to sites distant from the primary tumor, they must be protected by platelets from shear forces and the first line of defense of the immune system in blood, NK cells[89,90] (Figure 3). Migratory cells activate platelets through different mechanisms, in an exacerbated manner, which explains hypercoagulation and the increased risk of thrombosis in cancer patients[66,68].
Figure 3.
Breast cancer metastasis. Metastatic foci are the product of a series of events and in all these steps, they are accompanied by platelets. Breast cancer stem cell (BCSC) receives stimuli from the tumor microenvironment, including platelets, to allow the cellular transition epithelial-mesenchymal transition. Once the BCSC has achieved cell transformation and has broken the intercellular junctions and the extracellular matrix, it passes through the bloodstream or lymphatic system, always accompanied by platelets to avoid anoikis, shear forces and natural killer cells. The tumor educated platelets prepare the second metastatic niche. Created by Biorender.com. EMT: Epithelial-mesenchymal transition; TAM: Tumor-associated macrophage; CAF: Cancer-associated fibroblast; ECM: Extracellular matrix. Created with Biorender.com
The chemokines and cytokines that stimulate cell migration, CXCL1, CXCL4, CXCL5, CXCL7, CXCL8 and CXCL12, play an essential role in the platelet response to tissue injury, but also play a key role in angiogenesis and the metastatic process of BC[91]. CXCL4, also known as platelet factor 4 (PF4), is produced by megakaryocytes and stored in platelet α granules during platelet formation. The primary function of this chemokine is to contribute to coagulation but, being an angiostatic factor, it also plays a decisive role in the development of cancer by inhibiting cell migration[91,92].
Johnson et al[93] looked for a relationship between the biomolecules secreted by platelets and some type of secretome in BC cells that could make them prometastatic. They found that platelet-secreted biomolecules in the TME induced the release of CCL2, angiogenin, interferon-gamma, IL-6, granulocyte-macrophage colony-stimulating factor and CXCL1 in BC cells. They also found that IL-8 or CXCL8, the most studied proinflammatory chemokine secreted by metastasis-promoting tumor cells, increases its expression 50-fold in BC cell lines[93]. This cytokine is known to be released in response to platelet activation and aggregation[43]. IL-8 interacts with the CXCR1 and CXCR2 membrane receptors, which are highly expressed in BC cells; in fact, their expression is associated with angiogenic and metastatic processes, as well as with the regulation of BCSC expansion. Blocking CXCR1 and CXCR2 receptors have an antitumor effect[94].
Platelet inactivation in the TME has been shown to inhibit the Akt pathway, which usually induces IL8 production. When the production of IL-8 decreases, the metastatic capacity of BC cells decreases[67]. IL-8 positively regulates the AKT pathway, generating a much more metastatic and aggressive BC phenotype[67]. Consecutively, AKT induces SOX2 overexpression in CSCs, one of the main transcription factors involved in stem cell self-renewal[95].
It has been reported that aspirin can induce platelet inhibition[64,67]. A study by Johnson et al[93] showed that administering aspirin to BC patients significantly decreased IL8 levels and the platelet count. Aspirin intake was also associated with a decrease in tumor invasion compared to patients who did not receive aspirin[67]. Rothwell et al[96] concluded that people who consume aspirin daily are less likely to be diagnosed with cancer and show a higher probability of survival if they develop malignancy[96].
CCL5, also known as RANTES, is another chemokine associated with the progression and metastasis of BC promoted by platelets. Several authors have shown that platelets store and release large amounts of this chemokine, which is associated with disease progression and metastatic processes in patients with BC[44].
CXCR2 and its ligands are also involved in cancer development by promoting tumor angiogenesis and chemoresistance[95]. It has been reported that the expression of CXCR2 ligands increases in the supernatants of BC cells treated with chemotherapy and that BCSCs are enriched during doxorubicin and paclitaxel chemotherapy, showing more significant metastatic potential than primary tumor cells[97].
Cells from metastatic BC are rich in CXCR4 and CCR7 receptors and it has been observed that the sites where secondary metastatic foci are more likely to develop are those sites rich in ligands for CXCR4 and CCR7[98].
CXCR4 also interacts with CXCL12, a chemokine produced by stromal cells whose leading role is to trigger platelet migration into extravascular spaces, which promotes the polymerization of actin in the cytoskeleton of cancer cells, thereby causing a rearrangement of the pseudopodia of BC cells, which in turn induces chemotactic and invasive responses[99].
PAR1-PR and PAR4-PR (molecules found inside platelets) are other platelet-secreted molecules that play a crucial role in the TME and the development of cancer, angiogenesis and metastasis[66,78]. Their expression increases BC cell proliferation in vitro and, together, in vivo, promote MDA-MB-231 growth implanted in mice[66]. PAR1-PR is a proangiogenic factor that stimulates platelet activation and induces the release of SDF-1 and VEGF by promoting the growth of BC cells, more efficiently[78] than PAR4-PR, an antiangiogenic factor that promotes the release of PF4 and endostatin but limits the release of SDF-1 and VEGF[78].
VEGF, another factor released by platelets[100], promotes cancer cell proliferation mainly through the cooperative signaling of VEGFR2 and integrin activation by VEGF, via the PI3K/PKC signaling pathway[101]. Breast cancer patients submitted to several treatments showed platelet phenotype changes. Platelets were activated by ADP receptors, thrombin and collagen from patients with BC, which led to a significant increase in the secretion of VEGF, TSP1 and TGF-β1, compared to resting platelets. The response, however, differed depending on the platelet agonist. For example, the ADP agonist was a much weaker inducer of protein release than agonists attacking collagen and thrombin receptors. The study demonstrated the effects of specific stimulation of platelet receptor pathways on the release of VEGF, TSP1 and TGF-β1 in BC patients[102].
In 2015, Orellana et al[83] studied the association between platelets and ovarian cancer stem cells. They showed that platelets promoted the formation of ovarian cancer spheres that express cancer stem cell surface markers, such as CD44. In addition, the authors showed, through an experiment with a Boyden camera, where cancer cells were placed on top and platelets on the bottom, that microparticles from platelets and exosomes in the proximity of tumor cells promoted the migration of these cells, probably because the molecules inside platelets, such as PDGF and TGFβ, can serve as chemoattractants[83].
Platelets have been reported to induce activation by dephosphorylation and subsequent entry into cell nuclei, of RhoA-(myosin phosphatase targeting subunit 1), MYPT1-protein phosphatase (PP1)-mediated and the Yes-associated protein 1 (YAP1), which confer resistance to anoikis[103]. It has also been shown that platelets with a low expression level of apoptosis signal-regulating kinase 1 (Ask1), which activates the phosphorylation of AKT, JNK and p38, are associated with a decrease in metastasis[104].
Another protein secreted by platelets that plays an essential role in the metastatic process of BC is acid sphingomyelinase (Asm), which induces ceramide production, which activates integrin 51, which in turn promotes metastasis[105]. Ferroni et al[106] demonstrated that cancer-associated oxidative stress contributes to persistent platelet activation.
In TNBC, the most aggressive form of BC with the poorest outcome, there are molecules related to self-renewal signaling pathways that are highly activated in TNBC relative to non-TNBC, these include SRC, PTK7, CX26, USP2, and PLK1[107].
On the other hand, Jansson et al[108] reported that the platelet-derived growth factor (PDGF) has higher expression in the TNBC subtype and the prognosis of these patients is even worse. Also Camorani et al[109] considered PDGFRß as "a reliable biomarker of TNBCs subgroup with invasive and stem-like phenotype[109]." In this sense, several PDGF receptor kinase inhibitors have been developed, including Imatinib, Sunitinib, Sorafenib, Pazopanib, and Nilotinib. In addition, monoclonal antibodies directed against PDGF or PDGFR have been developed, such as MC-3G3 specific to PDGFRα, and IMC-2C5 directed against PDGFRβ to delay tumoral growth[110].
Experimental evidence indicates that platelets can exacerbate the cancer metastasis process in several ways; (1) promoting extravasation; (2) improving tumor cell survival in the circulatory system; (3), increasing tumor cell arrest in the vasculature system; and (4) stimulating tumor proliferation and angiogenesis at secondary sites[111].
ROLE OF PLATELETS IN CANCER CELL PROTECTION
When cells metastasize, only a small group of them manage to survive and initiate metastatic foci. Platelets play an essential role in cancer cell survival, by protecting anoikis. When cancer cells travel throughout the bloodstream, platelets induce thrombus formation to protect them from dangerous shear forces and NK cells[71,91,111,112]. Anoikis is an apoptotic process induced by cell detachment from the ECM that constitutes the main barrier against the metastatic process[112]. As discussed above, one of the main characteristics of cells with a migratory EMT phenotype is the loss of cell-cell and cell-ECM junctions, which allows them to enter the blood or lymphatic vessels and colonize distant sites as part of the metastatic process[16,24]. A characteristic of cancer cells that has been fully identified is their ability to survive without anchorage, travel to distant sites through the blood system and initiate secondary tumors[16]. Several studies have analyzed the role of signaling pathways in anoikis. For example, PI3K-AKT is one of the main pathways involved in promoting resistance to anoikis via the growth factor IGF-1, which is found in the TME and plays an essential role in tumor development and growth, as well as in the prevention of apoptosis through its ligand IGFR1[113].
In 2002, Zeng et al[77] showed that the cytokine HGF, which promotes cell proliferation, migration and invasion, can inhibit anoikis and improve the survival of head and neck tumor cells through activation of the ERK pathway[77].
In 2004, Douma et al[114] demonstrated the role of the neurotrophic tyrosine kinase receptor TrkB as a direct suppressor of caspases in anoikis. TrkB prevents cell death, allowing them to survive and proliferate as suspended spheroid cell aggregates[114].
A large number of adhesion molecules embedded in the cell membrane of platelets and platelet-derived microparticles promote adhesion between different cells; platelet/platelet, platelet/blood vessel endothelium and platelet/cancer cell. The cellular adhesion aids the formation of a thrombus around cancer cells that have entered blood vessels and thereby helping them evade both anoikis and the immune response[115]. The adhesion molecules of platelets include integrins (αIIbβ3, α2β1, α5β1, α6β1, αLβ2, αvβ3, P-selectin), membrane glycoproteins (GPIb/V/IX and PSGL-1) and immunoglobulin superfamily proteins (platelet-endothelial cell adhesion molecule-1, PECAM-1)[115,116].
Both platelets and endothelial cells have been shown to express P-selectin, which aids the dissemination of tumor cells. P-selectin can be found in the alpha granules of platelets. When platelets are activated, P-selectin is translocated to the surface and regulates the binding between platelets and endothelial cells through the formation of glucan structures[117]. It has been shown that a decrease in P-selectin, which weakens the junctions between platelets and tumor cells, is associated with a reduction in tumor size, a reduction of metastatic foci and an increased survival rate in mice with BC[118]. P-selectin is known to play an essential role in the evasion of NK cells by BCSCs in blood vessels. Platelets aggregate around a tumor cell when the PSGL-1 ligands on platelets recognize P-selectin, allowing tumor cells to evade the immune response[119].
ROLE OF PLATELETS IN ANGIOGENESIS DEVELOPMENT
As neo-angiogenesis produces leaky blood vessels during the early progression of cancer, it is no surprise that platelets are among the first cells to be involved in this process. Their ability to extravasate, activate and release proangiogenic, chemoattractant and immunomodulatory compounds can potentially promote cancer progression and metastasis.
Neo-angiogenesis is regulated by several pro- and antiangiogenic factors, mainly VEGF[120], FGF[103], EGF[121], HIF-1[122] and TGF[123], but many other angiogenic cytokines such as factors PDGF[103,120], NGF[124] and SCF[125] participate in this process.
In cancer, the angiogenesis process is promoted and regulated by the TME, including BCSCs. Two mechanisms explain the formation of new blood vessels in tumors. The first involves the transdifferentiation of cancer cells in a process called vasculogenic mimicry[126]. The second one involves the binding of neoplastic cells to the vessel wall through a process called mosaic vessel formation[127]. Both mechanisms depend on stimulating factors that promote the formation of new vessels. Feng et al[128] reported that the vesicle-associated membrane protein 8 (VAMP8), which can be found in platelet α-granules, is capable of attracting and recruiting bone marrow cells to hypoxic stress points in the tumor tissue, thus contributing to the formation of blood vessels within the tumor[128].
PLATELETS AND STEM CELLS INTERACTION
In mice, platelets help stem cells promote the proliferation of cells in injured tissues. They also help differentiate them through platelet-derived factors such as SDF-1, which not only regulates stem cell adhesion but also promotes the differentiation of CD34+ cells into the EPC under strong shear forces[129]. Healthy stem cells travel through the bloodstream, leaving it to reach injured tissue and initiating replication, differentiation and repair. Cancer stem cells, originating in the core of the tumor and having undergone a process of cell detachment and MET, allow them to invade distant tissues and go through the same type of processes as healthy stem cells. In both cases, platelets help stem cells survive and reach their target site, in one case, to repair injured tissue and in the other to colonize and form metastatic foci. Healthy stem cells have not been reported to activate the platelets that protect them, but several studies have shown that cancer stem cells continuously activate platelets through various pathways.
Interestingly, bone marrow-derived mesenchymal stem cells (BM-MSCs) produce cytokines and exosomes, promoting tumor growth and metastasis of cancer cells. Recently, researchers reported that BM-MSCs presented transdifferentiation TGFß dependent into CAFs and perivascular-like cells after co-incubation with platelets which was associated with an overexpression of vimentin, fibroblast activation protein and a-smooth muscle actin. Transdifferentiated-BM-MSCs cell medium had an interesting effect on gastric cancer cells: they were able to metastasize to lung and increased their proliferation and migration toward cancer cells[130-132].
Recently, efforts to create new therapies have been focused on targets related to pathways involved in stemness of BC cells, many of which have already been reviewed in this work. These factors can be transported into platelets or they can be regulated by the platelet content released into the microenvironment. Some of the developed therapies are shown in Table 1.
Table 1.
Therapeutic targets related to breast cancer stem cell pathways and platelet content
|
Breast cancer
|
Target/Pathway
|
Treatment Phase
|
Drug name
|
Ref.
|
| BC | CXCR4 | - | Plerixafor | [136] |
| BC | TGFß | - | Trabedersen | [137] |
| BC | DDL4/Notch | I | Demcizumab | [138] |
| BC, TNBC | Notch3 | I | AntiNotch3-ADC | [139] |
| BC | Wnt | I | Ipafricept | [140] |
| BC | PI3K | I | Alpelisib | [141] |
| TNBC | PI3K | I | Buparlisib | [142] |
| MBC | CXCR1 | Ib | Reparixin | [143] |
| BC | EpCAM | II | Adecatumumab | [144] |
| TNBC | Notch | II | Nirogacestat | [145] |
| MTNBC | JAK | II | Ruxolitinib | [146] |
| MBC | VEGF | III | Bevacizumab | [147] |
BC: Breast Cancer; TNBC: Triple-negative breast cancer; MBC: Metastatic breast cancer; MTNBC: Metastatic triple-negative breast cancer.
On the other hand, several clinical studies have suggested that treatment with anticoagulants (AC) or antiplatelets (AP) helps treat cancer by directly influencing platelet behavior and indirectly affecting tumor cell behavior. A large cohort study of patients showed that daily use of aspirin, the most commonly used antiplatelet agent was associated with a reduced incidence of malignancy[133], and this effect was evident in colorectal, prostate and breast cancer[134,135] and for others types of cancer there is still controversy.
Other antiplatelets in addition to aspirin have been studied, such as Dipyridamole and RA-233 in pancreatic cancer; Prasugrel in gastrointestinal cancer, Clopidogrel in the pancreatic cancer mouse model and hepatoma carcinoma, melanoma and breast cancer with promising results. It is clear that more studies are needed in order that personalized platelet-targeted therapies in cancer may be administered.
CONCLUSION
TEPs can be considered the perfect weapon of CSCs for tumor development and metastatic foci formation.
TEPs contribute to various levels of cancer progression when platelets have been activated by stimuli from TME or cancer cells, they secrete factors that strengthen the TME by promoting (1) the mobilization of tumor cells into blood vessels, to produce metastatic foci; (2) tumor growth; and (3) neo-angiogenesis to feed the tumor.
In order to be able to contribute to cancer mortality reduction, it is necessary to understand the interactions between platelets and BCSCs in the TME, and how they control cancer progression and metastatic secondary tumor development. This information could be useful in identifying new therapeutic targets or in the development of an accurate and straightforward diagnosis.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest. No financial support.
Manuscript source: Invited manuscript
Peer-review started: July 1, 2020
First decision: August 9, 2020
Article in press: September 22, 2020
Specialty type: Oncology
Country/Territory of origin: Mexico
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ding MX, Sulkowski S S-Editor: Ma YJ L-Editor: Webster JR P-Editor: Wang LYT
Contributor Information
Gretel Mendoza-Almanza, CONACYT, Universidad Autónoma de Zacatecas., Zacatecas 98060, Mexico.
Luis Burciaga-Hernández, Maestría en Ciencias Biomédicas, Universidad Autónoma de Zacatecas, Zacatecas 98160, Mexico.
Vilma Maldonado, Laboratorio de Epigenética, Instituto Nacional de Medicina Genómica, Ciudad de México 14610, Mexico.
Jorge Melendez-Zajgla, Génómica funcional del cáncer, Instituto Nacional de Medicina Genómica, Ciudad de México 14610, Mexico.
Jorge Olmos, Biotecnología Marina, Centro de Investigación Científica y de Estudios Superiores de Ensenada, Ensenada 22860, Mexico. jolmos@cicese.mx.
References
- 1.Mendoza-Almanza G, Ortíz-Sánchez E, Rocha-Zavaleta L, Rivas-Santiago C, Esparza-Ibarra E, Olmos J. Cervical cancer stem cells and other leading factors associated with cervical cancer development. Oncol Lett. 2019;18:3423–3432. doi: 10.3892/ol.2019.10718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin TA, Lin Y, Sanders AJ, Lane J, Jiang WG. Cancer invasion and metastasis molecular and cellular perspective. Austin (TX): Landers Bioscience; 2013. [Google Scholar]
- 3.Luo M, Clouthier SG, Deol Y, Liu S, Nagrath S, Azizi E, Wicha MS. Breast cancer stem cells: current advances and clinical implications. Methods Mol Biol. 2015;1293:1–49. doi: 10.1007/978-1-4939-2519-3_1. [DOI] [PubMed] [Google Scholar]
- 4.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Global Cancer Observatory. International Agency for research on cancer. Available from: https://gco.iarc.fr .
- 6.Estourgie SH, Nieweg OE, Olmos RA, Rutgers EJ, Kroon BB. Lymphatic drainage patterns from the breast. Ann Surg. 2004;239:232–237. doi: 10.1097/01.sla.0000109156.26378.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paduch R. The role of lymphangiogenesis and angiogenesis in tumor metastasis. Cell Oncol (Dordr) 2016;39:397–410. doi: 10.1007/s13402-016-0281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun YS, Zhao Z, Yang ZN, Xu F, Lu HJ, Zhu ZY, Shi W, Jiang J, Yao PP, Zhu HP. Risk Factors and Preventions of Breast Cancer. Int J Biol Sci. 2017;13:1387–1397. doi: 10.7150/ijbs.21635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Majeed W, Aslam B, Javed I, Khaliq T, Muhammad F, Ali A, Raza A. Breast cancer: major risk factors and recent developments in treatment. Asian Pac J Cancer Prev. 2014;15:3353–3358. doi: 10.7314/apjcp.2014.15.8.3353. [DOI] [PubMed] [Google Scholar]
- 10.Zhang X, Claerhout S, Prat A, Dobrolecki LE, Petrovic I, Lai Q, Landis MD, Wiechmann L, Schiff R, Giuliano M, Wong H, Fuqua SW, Contreras A, Gutierrez C, Huang J, Mao S, Pavlick AC, Froehlich AM, Wu MF, Tsimelzon A, Hilsenbeck SG, Chen ES, Zuloaga P, Shaw CA, Rimawi MF, Perou CM, Mills GB, Chang JC, Lewis MT. A renewable tissue resource of phenotypically stable, biologically and ethnically diverse, patient-derived human breast cancer xenograft models. Cancer Res. 2013;73:4885–4897. doi: 10.1158/0008-5472.CAN-12-4081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniel AR, Hagan CR, Lange CA. Progesterone receptor action: defining a role in breast cancer. Expert Rev Endocrinol Metab. 2011;6:359–369. doi: 10.1586/eem.11.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freudenberg JA, Wang Q, Katsumata M, Drebin J, Nagatomo I, Greene MI. The role of HER2 in early breast cancer metastasis and the origins of resistance to HER2-targeted therapies. Exp Mol Pathol. 2009;87:1–11. doi: 10.1016/j.yexmp.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Y, Sarkissyan M, Elshimali Y, Vadgama JV. Triple negative breast tumors in African-American and Hispanic/Latina women are high in CD44+, low in CD24+, and have loss of PTEN. PLoS One. 2013;8:e78259. doi: 10.1371/journal.pone.0078259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in Breast Cancer Survival by Molecular Subtypes in the United States. Cancer Epidemiol Biomarkers Prev. 2018;27:619–626. doi: 10.1158/1055-9965.EPI-17-0627. [DOI] [PubMed] [Google Scholar]
- 15.Guo W. Concise review: breast cancer stem cells: regulatory networks, stem cell niches, and disease relevance. Stem Cells Transl Med. 2014;3:942–948. doi: 10.5966/sctm.2014-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu S, Cong Y, Wang D, Sun Y, Deng L, Liu Y, Martin-Trevino R, Shang L, McDermott SP, Landis MD, Hong S, Adams A, D'Angelo R, Ginestier C, Charafe-Jauffret E, Clouthier SG, Birnbaum D, Wong ST, Zhan M, Chang JC, Wicha MS. Breast cancer stem cells transition between epithelial and mesenchymal states reflective of their normal counterparts. Stem Cell Reports. 2014;2:78–91. doi: 10.1016/j.stemcr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kreso A, Dick JE. Evolution of the cancer stem cell model. Cell Stem Cell. 2014;14:275–291. doi: 10.1016/j.stem.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Koren S, Bentires-Alj M. Breast Tumor Heterogeneity: Source of Fitness, Hurdle for Therapy. Mol Cell. 2015;60:537–546. doi: 10.1016/j.molcel.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 19.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hyun KA, Koo GB, Han H, Sohn J, Choi W, Kim SI, Jung HI, Kim YS. Epithelial-to-mesenchymal transition leads to loss of EpCAM and different physical properties in circulating tumor cells from metastatic breast cancer. Oncotarget. 2016;7:24677–24687. doi: 10.18632/oncotarget.8250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Draffin JE, McFarlane S, Hill A, Johnston PG, Waugh DJ. CD44 potentiates the adherence of metastatic prostate and breast cancer cells to bone marrow endothelial cells. Cancer Res. 2004;64:5702–5711. doi: 10.1158/0008-5472.CAN-04-0389. [DOI] [PubMed] [Google Scholar]
- 22.Crabtree JS, Miele L. Breast Cancer Stem Cells. Biomedicines. 2018;6 doi: 10.3390/biomedicines6030077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ginestier C, Hur MH, Charafe-Jauffret E, Monville F, Dutcher J, Brown M, Jacquemier J, Viens P, Kleer CG, Liu S, Schott A, Hayes D, Birnbaum D, Wicha MS, Dontu G. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1:555–567. doi: 10.1016/j.stem.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luo M, Brooks M, Wicha MS. Epithelial-mesenchymal plasticity of breast cancer stem cells: implications for metastasis and therapeutic resistance. Curr Pharm Des. 2015;21:1301–1310. doi: 10.2174/1381612821666141211120604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Labelle M, Begum S, Hynes RO. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell. 2011;20:576–590. doi: 10.1016/j.ccr.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bollong MJ, Pietilä M, Pearson AD, Sarkar TR, Ahmad I, Soundararajan R, Lyssiotis CA, Mani SA, Schultz PG, Lairson LL. A vimentin binding small molecule leads to mitotic disruption in mesenchymal cancers. Proc Natl Acad Sci . 114:E9903–E9912. doi: 10.1073/pnas.1716009114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie J, Xiao Y, Zhu XY, Ning ZY, Xu HF, Wu HM. Hypoxia regulates stemness of breast cancer MDA-MB-231 cells. Med Oncol. 2016;33:42. doi: 10.1007/s12032-016-0755-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S, Li Z, Xu R. Human Cancer and Platelet Interaction, a Potential Therapeutic Target. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19041246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 30.Stankic M, Pavlovic S, Chin Y, Brogi E, Padua D, Norton L, Massagué J, Benezra R. TGF-β-Id1 signaling opposes Twist1 and promotes metastatic colonization via a mesenchymal-to-epithelial transition. Cell Rep. 2013;5:1228–1242. doi: 10.1016/j.celrep.2013.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liang Y, Hu J, Li J, Liu Y, Yu J, Zhuang X, Mu L, Kong X, Hong D, Yang Q, Hu G. Epigenetic Activation of TWIST1 by MTDH Promotes Cancer Stem-like Cell Traits in Breast Cancer. Cancer Res. 2015;75:3672–3680. doi: 10.1158/0008-5472.CAN-15-0930. [DOI] [PubMed] [Google Scholar]
- 32.Thiery JP, Sleeman JP. Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 33.Schober M, Fuchs E. Tumor-initiating stem cells of squamous cell carcinomas and their control by TGF-β and integrin/focal adhesion kinase (FAK) signaling. Proc Natl Acad Sci USA. 2011;108:10544–10549. doi: 10.1073/pnas.1107807108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asiedu MK, Beauchamp-Perez FD, Ingle JN, Behrens MD, Radisky DC, Knutson KL. AXL induces epithelial-to-mesenchymal transition and regulates the function of breast cancer stem cells. Oncogene. 2014;33:1316–1324. doi: 10.1038/onc.2013.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kise K, Kinugasa-Katayama Y, Takakura N. Tumor microenvironment for cancer stem cells. Adv Drug Deliv Rev. 2016;99:197–205. doi: 10.1016/j.addr.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Rupaimoole R, Calin GA, Lopez-Berestein G, Sood AK. miRNA Deregulation in Cancer Cells and the Tumor Microenvironment. Cancer Discov. 2016;6:235–246. doi: 10.1158/2159-8290.CD-15-0893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Xu X, Maglic D, Dill MT, Mojumdar K, Ng PK, Jeong KJ, Tsang YH, Moreno D, Bhavana VH, Peng X, Ge Z, Chen H, Li J, Chen Z, Zhang H, Han L, Du D, Creighton CJ, Mills GB Cancer Genome Atlas Research Network; Camargo F; Liang H. Comprehensive Molecular Characterization of the Hippo Signaling Pathway in Cancer. Cell Rep 2018; 25: 1304-1317. :e5. doi: 10.1016/j.celrep.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu S, Ginestier C, Ou SJ, Clouthier SG, Patel SH, Monville F, Korkaya H, Heath A, Dutcher J, Kleer CG, Jung Y, Dontu G, Taichman R, Wicha MS. Breast cancer stem cells are regulated by mesenchymal stem cells through cytokine networks. Cancer Res. 2011;71:614–624. doi: 10.1158/0008-5472.CAN-10-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao M, Liu Y, Liu R, Qi J, Hou Y, Chang J, Ren L. Upregulation of IL-11, an IL-6 Family Cytokine, Promotes Tumor Progression and Correlates with Poor Prognosis in Non-Small Cell Lung Cancer. Cell Physiol Biochem. 2018;45:2213–2224. doi: 10.1159/000488166. [DOI] [PubMed] [Google Scholar]
- 40.Allavena P, Sica A, Solinas G, Porta C, Mantovani A. The inflammatory micro-environment in tumor progression: the role of tumor-associated macrophages. Crit Rev Oncol Hematol. 2008;66:1–9. doi: 10.1016/j.critrevonc.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 41.Leek RD, Landers R, Fox SB, Ng F, Harris AL, Lewis CE. Association of tumour necrosis factor alpha and its receptors with thymidine phosphorylase expression in invasive breast carcinoma. Br J Cancer. 1998;77:2246–2251. doi: 10.1038/bjc.1998.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mancino A, Lawrence T. Nuclear factor-kappaB and tumor-associated macrophages. Clin Cancer Res. 2010;16:784–789. doi: 10.1158/1078-0432.CCR-09-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alonso-Escolano D, Strongin AY, Chung AW, Deryugina EI, Radomski MW. Membrane type-1 matrix metalloproteinase stimulates tumour cell-induced platelet aggregation: role of receptor glycoproteins. Br J Pharmacol. 2004;141:241–252. doi: 10.1038/sj.bjp.0705606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hagemann T, Robinson SC, Schulz M, Trümper L, Balkwill FR, Binder C. Enhanced invasiveness of breast cancer cell lines upon co-cultivation with macrophages is due to TNF-alpha dependent up-regulation of matrix metalloproteases. Carcinogenesis. 2004;25:1543–1549. doi: 10.1093/carcin/bgh146. [DOI] [PubMed] [Google Scholar]
- 45.Läubli H, Spanaus KS, Borsig L. Selectin-mediated activation of endothelial cells induces expression of CCL5 and promotes metastasis through recruitment of monocytes. Blood. 2009;114:4583–4591. doi: 10.1182/blood-2008-10-186585. [DOI] [PubMed] [Google Scholar]
- 46.Michael JV, Wurtzel JGT, Mao GF, Rao AK, Kolpakov MA, Sabri A, Hoffman NE, Rajan S, Tomar D, Madesh M, Nieman MT, Yu J, Edelstein LC, Rowley JW, Weyrich AS, Goldfinger LE. Platelet microparticles infiltrating solid tumors transfer miRNAs that suppress tumor growth. Blood. 2017;130:567–580. doi: 10.1182/blood-2016-11-751099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shimono Y, Mukohyama J, Nakamura S, Minami H. MicroRNA Regulation of Human Breast Cancer Stem Cells. J Clin Med. 2015;5 doi: 10.3390/jcm5010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shah NR, Chen H. MicroRNAs in pathogenesis of breast cancer: Implications in diagnosis and treatment. World J Clin Oncol. 2014;5:48–60. doi: 10.5306/wjco.v5.i2.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu S, Clouthier SG, Wicha MS. Role of microRNAs in the regulation of breast cancer stem cells. J Mammary Gland Biol Neoplasia. 2012;17:15–21. doi: 10.1007/s10911-012-9242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tang M, Jiang L, Lin Y, Wu X, Wang K, He Q, Wang X, Li W. Platelet microparticle-mediated transfer of miR-939 to epithelial ovarian cancer cells promotes epithelial to mesenchymal transition. Oncotarget. 2017;8:97464–97475. doi: 10.18632/oncotarget.22136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Korpal M, Ell BJ, Buffa FM, Ibrahim T, Blanco MA, Celià-Terrassa T, Mercatali L, Khan Z, Goodarzi H, Hua Y, Wei Y, Hu G, Garcia BA, Ragoussis J, Amadori D, Harris AL, Kang Y. Direct targeting of Sec23a by miR-200s influences cancer cell secretome and promotes metastatic colonization. Nat Med. 2011;17:1101–1108. doi: 10.1038/nm.2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brabletz T. MiR-34 and SNAIL: another double-negative feedback loop controlling cellular plasticity/EMT governed by p53. Cell Cycle. 2012;11:215–216. doi: 10.4161/cc.11.2.18900. [DOI] [PubMed] [Google Scholar]
- 53.Lazar S, Goldfinger LE. Platelet Microparticles and miRNA Transfer in Cancer Progression: Many Targets, Modes of Action, and Effects Across Cancer Stages. Front Cardiovasc Med. 2018;5:13. doi: 10.3389/fcvm.2018.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Strutz F, Zeisberg M, Ziyadeh FN, Yang CQ, Kalluri R, Müller GA, Neilson EG. Role of basic fibroblast growth factor-2 in epithelial-mesenchymal transformation. Kidney Int. 2002;61:1714–1728. doi: 10.1046/j.1523-1755.2002.00333.x. [DOI] [PubMed] [Google Scholar]
- 55.Wu Q, Hou X, Xia J, Qian X, Miele L, Sarkar FH, Wang Z. Emerging roles of PDGF-D in EMT progression during tumorigenesis. Cancer Treat Rev. 2013;39:640–646. doi: 10.1016/j.ctrv.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Farrell J, Kelly C, Rauch J, Kida K, García-Muñoz A, Monsefi N, Turriziani B, Doherty C, Mehta JP, Matallanas D, Simpson JC, Kolch W, von Kriegsheim A. HGF induces epithelial-to-mesenchymal transition by modulating the mammalian hippo/MST2 and ISG15 pathways. J Proteome Res. 2014;13:2874–2886. doi: 10.1021/pr5000285. [DOI] [PubMed] [Google Scholar]
- 57.Assoian RK, Sporn MB. Type beta transforming growth factor in human platelets: release during platelet degranulation and action on vascular smooth muscle cells. J Cell Biol. 1986;102:1217–1223. doi: 10.1083/jcb.102.4.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meng D, Meng M, Luo A, Jing X, Wang G, Huang S, Luo M, Shao S, Zhao X, Liu R. Effects of VEGFR1+ hematopoietic progenitor cells on pre-metastatic niche formation and in vivo metastasis of breast cancer cells. J Cancer Res Clin Oncol. 2019;145:411–427. doi: 10.1007/s00432-018-2802-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cherubini E, Mariotta S, Scozzi D, Mancini R, Osman G, D'Ascanio M, Bruno P, Cardillo G, Ricci A. BDNF/TrkB axis activation promotes epithelial-mesenchymal transition in idiopathic pulmonary fibrosis. J Transl Med. 2017;15:196. doi: 10.1186/s12967-017-1298-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Donatelli SS, Zhou JM, Gilvary DL, Eksioglu EA, Chen X, Cress WD, Haura EB, Schabath MB, Coppola D, Wei S, Djeu JY. TGF-β-inducible microRNA-183 silences tumor-associated natural killer cells. Proc Natl Acad Sci USA. 2014;111:4203–4208. doi: 10.1073/pnas.1319269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anandi VL, Ashiq KA, Nitheesh K, Lahiri M. Platelet-activating factor promotes motility in breast cancer cells and disrupts non-transformed breast acinar structures. Oncol Rep. 2016;35:179–188. doi: 10.3892/or.2015.4387. [DOI] [PubMed] [Google Scholar]
- 62.Umar A, Steele VE, Menter DG, Hawk ET. Mechanisms of nonsteroidal anti-inflammatory drugs in cancer prevention. Semin Oncol. 2016;43:65–77. doi: 10.1053/j.seminoncol.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 63.Prescott SM, Zimmerman GA, Stafforini DM, McIntyre TM. Platelet-activating factor and related lipid mediators. Annu Rev Biochem. 2000;69:419–445. doi: 10.1146/annurev.biochem.69.1.419. [DOI] [PubMed] [Google Scholar]
- 64.Ward Y, Lake R, Faraji F, Sperger J, Martin P, Gilliard C, Ku KP, Rodems T, Niles D, Tillman H, Yin J, Hunter K, Sowalsky AG, Lang J, Kelly K. Platelets Promote Metastasis via Binding Tumor CD97 Leading to Bidirectional Signaling that Coordinates Transendothelial Migration. Cell Rep. 2018;23:808–822. doi: 10.1016/j.celrep.2018.03.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Catani MV, Savini I, Tullio V, Gasperi V. The "Janus Face" of Platelets in Cancer. Int J Mol Sci. 2020;21 doi: 10.3390/ijms21030788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Menter DG, Kopetz S, Hawk E, Sood AK, Loree JM, Gresele P, Honn KV. Platelet "first responders" in wound response, cancer, and metastasis. Cancer Metastasis Rev. 2017;36:199–213. doi: 10.1007/s10555-017-9682-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jiang L, Luan Y, Miao X, Sun C, Li K, Huang Z, Xu D, Zhang M, Kong F, Li N. Platelet releasate promotes breast cancer growth and angiogenesis via VEGF-integrin cooperative signalling. Br J Cancer. 2017;117:695–703. doi: 10.1038/bjc.2017.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Palacios-Acedo AL, Mège D, Crescence L, Dignat-George F, Dubois C, Panicot-Dubois L. Platelets, Thrombo-Inflammation, and Cancer: Collaborating With the Enemy. Front Immunol. 2019;10:1805. doi: 10.3389/fimmu.2019.01805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jen CJ, Tai YW. Morphological study of platelet adhesion dynamics under whole blood flow conditions. Platelets. 1992;3:145–153. doi: 10.3109/09537109209013175. [DOI] [PubMed] [Google Scholar]
- 70.Italiano JE Jr, Bergmeier W, Tiwari S, Falet H, Hartwig JH, Hoffmeister KM, André P, Wagner DD, Shivdasani RA. Mechanisms and implications of platelet discoid shape. Blood. 2003;101:4789–4796. doi: 10.1182/blood-2002-11-3491. [DOI] [PubMed] [Google Scholar]
- 71.Flaumenhaft R. Molecular basis of platelet granule secretion. Arterioscler Thromb Vasc Biol. 2003;23:1152–1160. doi: 10.1161/01.ATV.0000075965.88456.48. [DOI] [PubMed] [Google Scholar]
- 72.Schlesinger M. Role of platelets and platelet receptors in cancer metastasis. J Hematol Oncol. 2018;11:125. doi: 10.1186/s13045-018-0669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Freedman JE, Loscalzo J, Barnard MR, Alpert C, Keaney JF, Michelson AD. Nitric oxide released from activated platelets inhibits platelet recruitment. J Clin Invest. 1997;100:350–356. doi: 10.1172/JCI119540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Basudhar D, Somasundaram V, de Oliveira GA, Kesarwala A, Heinecke JL, Cheng RY, Glynn SA, Ambs S, Wink DA, Ridnour LA. Nitric Oxide Synthase-2-Derived Nitric Oxide Drives Multiple Pathways of Breast Cancer Progression. Antioxid Redox Signal. 2017;26:1044–1058. doi: 10.1089/ars.2016.6813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Banskota S, Gautam J, Regmi SC, Gurung P, Park MH, Kim SJ, Nam TG, Jeong BS, Kim JA. BJ-1108, a 6-Amino-2,4,5-Trimethylpyridin-3-ol Analog, Inhibits Serotonin-Induced Angiogenesis and Tumor Growth through PI3K/NOX Pathway. PLoS One. 2016;11:e0148133. doi: 10.1371/journal.pone.0148133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sarmiento-Salinas FL, Delgado-Magallón A, Montes-Alvarado JB, Ramírez-Ramírez D, Flores-Alonso JC, Cortés-Hernández P, Reyes-Leyva J, Herrera-Camacho I, Anaya-Ruiz M, Pelayo R, Millán-Pérez-Peña L, Maycotte P. Breast Cancer Subtypes Present a Differential Production of Reactive Oxygen Species (ROS) and Susceptibility to Antioxidant Treatment. Front Oncol. 2019;9:480. doi: 10.3389/fonc.2019.00480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Reginato MJ, Mills KR, Paulus JK, Lynch DK, Sgroi DC, Debnath J, Muthuswamy SK, Brugge JS. Integrins and EGFR coordinately regulate the pro-apoptotic protein Bim to prevent anoikis. Nat Cell Biol. 2003;5:733–740. doi: 10.1038/ncb1026. [DOI] [PubMed] [Google Scholar]
- 78.Zeng Q, McCauley LK, Wang CY. Hepatocyte growth factor inhibits anoikis by induction of activator protein 1-dependent cyclooxygenase-2. Implication in head and neck squamous cell carcinoma progression. J Biol Chem. 2002;277:50137–50142. doi: 10.1074/jbc.M208952200. [DOI] [PubMed] [Google Scholar]
- 79.Chatterjee M, Huang Z, Zhang W, Jiang L, Hultenby K, Zhu L, Hu H, Nilsson GP, Li N. Distinct platelet packaging, release, and surface expression of proangiogenic and antiangiogenic factors on different platelet stimuli. Blood. 2011;117:3907–3911. doi: 10.1182/blood-2010-12-327007. [DOI] [PubMed] [Google Scholar]
- 80.Maskrey BH, Rushworth GF, Law MH, Treweeke AT, Wei J, Leslie SJ, Megson IL, Whitfield PD. 12-hydroxyeicosatetraenoic acid is associated with variability in aspirin-induced platelet inhibition. J Inflamm (Lond) 2014;11:33. doi: 10.1186/s12950-014-0033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schumacher D, Strilic B, Sivaraj KK, Wettschureck N, Offermanns S. Platelet-derived nucleotides promote tumor-cell transendothelial migration and metastasis via P2Y2 receptor. Cancer Cell. 2013;24:130–137. doi: 10.1016/j.ccr.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 82.Bogdanov VY, Balasubramanian V, Hathcock J, Vele O, Lieb M, Nemerson Y. Alternatively spliced human tissue factor: a circulating, soluble, thrombogenic protein. Nat Med. 2003;9:458–462. doi: 10.1038/nm841. [DOI] [PubMed] [Google Scholar]
- 83.Cole M, Bromberg M. Tissue factor as a novel target for treatment of breast cancer. Oncologist. 2013;18:14–18. doi: 10.1634/theoncologist.2012-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Orellana R, Kato S, Erices R, Bravo ML, Gonzalez P, Oliva B, Cubillos S, Valdivia A, Ibañez C, Brañes J, Barriga MI, Bravo E, Alonso C, Bustamente E, Castellon E, Hidalgo P, Trigo C, Panes O, Pereira J, Mezzano D, Cuello MA, Owen GI. Platelets enhance tissue factor protein and metastasis initiating cell markers, and act as chemoattractants increasing the migration of ovarian cancer cells. BMC Cancer. 2015;15:290. doi: 10.1186/s12885-015-1304-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Reddel CJ, Tan CW, Chen VM. Thrombin Generation and Cancer: Contributors and Consequences. Cancers (Basel) 2019;11 doi: 10.3390/cancers11010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mezouar S, Frère C, Darbousset R, Mege D, Crescence L, Dignat-George F, Panicot-Dubois L, Dubois C. Role of platelets in cancer and cancer-associated thrombosis: Experimental and clinical evidences. Thromb Res. 2016;139:65–76. doi: 10.1016/j.thromres.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 87.Guerrero JA, Bennett C, van der Weyden L, McKinney H, Chin M, Nurden P, McIntyre Z, Cambridge EL, Estabel J, Wardle-Jones H, Speak AO, Erber WN, Rendon A, Ouwehand WH, Ghevaert C. Gray platelet syndrome: proinflammatory megakaryocytes and α-granule loss cause myelofibrosis and confer metastasis resistance in mice. Blood. 2014;124:3624–3635. doi: 10.1182/blood-2014-04-566760. [DOI] [PubMed] [Google Scholar]
- 88.Bambace NM, Holmes CE. The platelet contribution to cancer progression. J Thromb Haemost. 2011;9:237–249. doi: 10.1111/j.1538-7836.2010.04131.x. [DOI] [PubMed] [Google Scholar]
- 89.Clar KL, Hinterleitner C, Schneider P, Salih HR, Maurer S. Inhibition of NK Reactivity Against Solid Tumors by Platelet-Derived RANKL. Cancers (Basel) 2019;11 doi: 10.3390/cancers11030277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang S, Zhang Y, Cong W, Liu J, Zhang Y, Fan H, Xu Y, Lin H. Breast cancer stem-like cells can promote metastasis by activating platelets and down-regulating antitumor activity of natural killer cells. J Tradit Chin Med. 2016;36:530–537. doi: 10.1016/s0254-6272(16)30071-1. [DOI] [PubMed] [Google Scholar]
- 91.Santoni M, Bracarda S, Nabissi M, Massari F, Conti A, Bria E, Tortora G, Santoni G, Cascinu S. CXC and CC chemokines as angiogenic modulators in nonhaematological tumors. Biomed Res Int. 2014;2014:768758. doi: 10.1155/2014/768758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yamaguchi K, Ogawa K, Katsube T, Shimao K, Konno S, Shimakawa T, Yoshimatsu K, Naritaka Y, Yagawa H, Hirose K. Platelet factor 4 gene transfection into tumor cells inhibits angiogenesis, tumor growth and metastasis. Anticancer Res. 2005;25:847–851. [PubMed] [Google Scholar]
- 93.Johnson KE, Ceglowski JR, Roweth HG, Forward JA, Tippy MD, El-Husayni S, Kulenthirarajan R, Malloy MW, Machlus KR, Chen WY, Italiano JE Jr, Battinelli EM. Aspirin inhibits platelets from reprogramming breast tumor cells and promoting metastasis. Blood Adv. 2019;3:198–211. doi: 10.1182/bloodadvances.2018026161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Singh JK, Farnie G, Bundred NJ, Simões BM, Shergill A, Landberg G, Howell SJ, Clarke RB. Targeting CXCR1/2 significantly reduces breast cancer stem cell activity and increases the efficacy of inhibiting HER2 via HER2-dependent and -independent mechanisms. Clin Cancer Res. 2013;19:643–656. doi: 10.1158/1078-0432.CCR-12-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang Z, Kang L, Zhang H, Huang Y, Fang L, Li M, Brown PJ, Arrowsmith CH, Li J, Wong J. AKT drives SOX2 overexpression and cancer cell stemness in esophageal cancer by protecting SOX2 from UBR5-mediated degradation. Oncogene. 2019;38:5250–5264. doi: 10.1038/s41388-019-0790-x. [DOI] [PubMed] [Google Scholar]
- 96.Rothwell PM, Price JF, Fowkes FG, Zanchetti A, Roncaglioni MC, Tognoni G, Lee R, Belch JF, Wilson M, Mehta Z, Meade TW. Short-term effects of daily aspirin on cancer incidence, mortality, and non-vascular death: analysis of the time course of risks and benefits in 51 randomised controlled trials. Lancet. 2012;379:1602–1612. doi: 10.1016/S0140-6736(11)61720-0. [DOI] [PubMed] [Google Scholar]
- 97.Sharma B, Nawandar DM, Nannuru KC, Varney ML, Singh RK. Targeting CXCR2 enhances chemotherapeutic response, inhibits mammary tumor growth, angiogenesis, and lung metastasis. Mol Cancer Ther. 2013;12:799–808. doi: 10.1158/1535-7163.MCT-12-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Müller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, Barrera JL, Mohar A, Verástegui E, Zlotnik A. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 99.Sun X, Cheng G, Hao M, Zheng J, Zhou X, Zhang J, Taichman RS, Pienta KJ, Wang J. CXCL12 / CXCR4 / CXCR7 chemokine axis and cancer progression. Cancer Metastasis Rev. 2010;29:709–722. doi: 10.1007/s10555-010-9256-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Battinelli EM, Markens BA, Italiano JE Jr. Release of angiogenesis regulatory proteins from platelet alpha granules: modulation of physiologic and pathologic angiogenesis. Blood. 2011;118:1359–1369. doi: 10.1182/blood-2011-02-334524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Abhinand CS, Raju R, Soumya SJ, Arya PS, Sudhakaran PR. VEGF-A/VEGFR2 signaling network in endothelial cells relevant to angiogenesis. J Cell Commun Signal. 2016;10:347–354. doi: 10.1007/s12079-016-0352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Holmes CE, Levis JE, Schneider DJ, Bambace NM, Sharma D, Lal I, Wood ME, Muss HB. Platelet phenotype changes associated with breast cancer and its treatment. Platelets. 2016;27:703–711. doi: 10.3109/09537104.2016.1171302. [DOI] [PubMed] [Google Scholar]
- 103.Kano MR, Morishita Y, Iwata C, Iwasaka S, Watabe T, Ouchi Y, Miyazono K, Miyazawa K. VEGF-A and FGF-2 synergistically promote neoangiogenesis through enhancement of endogenous PDGF-B-PDGFRbeta signaling. J Cell Sci. 2005;118:3759–3768. doi: 10.1242/jcs.02483. [DOI] [PubMed] [Google Scholar]
- 104.Kamiyama M, Shirai T, Tamura S, Suzuki-Inoue K, Ehata S, Takahashi K, Miyazono K, Hayakawa Y, Sato T, Takeda K, Naguro I, Ichijo H. ASK1 facilitates tumor metastasis through phosphorylation of an ADP receptor P2Y12 in platelets. Cell Death Differ. 2017;24:2066–2076. doi: 10.1038/cdd.2017.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Carpinteiro A, Beckmann N, Seitz A, Hessler G, Wilker B, Soddemann M, Helfrich I, Edelmann B, Gulbins E, Becker KA. Role of Acid Sphingomyelinase-Induced Signaling in Melanoma Cells for Hematogenous Tumor Metastasis. Cell Physiol Biochem. 2016;38:1–14. doi: 10.1159/000438604. [DOI] [PubMed] [Google Scholar]
- 106.Ferroni P, Santilli F, Cavaliere F, Simeone P, Costarelli L, Liani R, Tripaldi R, Riondino S, Roselli M, Davi G, Guadagni F. Oxidant stress as a major determinant of platelet activation in invasive breast cancer. Int J Cancer. 2017;140:696–704. doi: 10.1002/ijc.30488. [DOI] [PubMed] [Google Scholar]
- 107.Park SY, Choi JH, Nam JS. Targeting Cancer Stem Cells in Triple-Negative Breast Cancer. Cancers (Basel) 2019;11 doi: 10.3390/cancers11070965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jansson S, Aaltonen K, Bendahl PO, Falck AK, Karlsson M, Pietras K, Rydén L. The PDGF pathway in breast cancer is linked to tumour aggressiveness, triple-negative subtype and early recurrence. Breast Cancer Res Treat. 2018;169:231–241. doi: 10.1007/s10549-018-4664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Camorani S, Hill BS, Collina F, Gargiulo S, Napolitano M, Cantile M, Di Bonito M, Botti G, Fedele M, Zannetti A, Cerchia L. Targeted imaging and inhibition of triple-negative breast cancer metastases by a PDGFRβ aptamer. Theranostics. 2018;8:5178–5199. doi: 10.7150/thno.27798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Huang F, Wang D, Yao Y, Wang M. PDGF signaling in cancer progression. Int J Clin Exp Med . 2017;10:9918–9929. [Google Scholar]
- 111.Gkolfinopoulos S, Jones RL, Constantinidou A. The Emerging Role of Platelets in the Formation of the Micrometastatic Niche: Current Evidence and Future Perspectives. Front Oncol. 2020;10:374. doi: 10.3389/fonc.2020.00374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Naderi-Meshkin H, Ahmadiankia N. Cancer metastasis vs stem cell homing: Role of platelets. J Cell Physiol. 2018;233:9167–9178. doi: 10.1002/jcp.26937. [DOI] [PubMed] [Google Scholar]
- 113.Luey BC, May FE. Insulin-like growth factors are essential to prevent anoikis in oestrogen-responsive breast cancer cells: importance of the type I IGF receptor and PI3-kinase/Akt pathway. Mol Cancer. 2016;15:8. doi: 10.1186/s12943-015-0482-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Douma S, Van Laar T, Zevenhoven J, Meuwissen R, Van Garderen E, Peeper DS. Suppression of anoikis and induction of metastasis by the neurotrophic receptor TrkB. Nature. 2004;430:1034–1039. doi: 10.1038/nature02765. [DOI] [PubMed] [Google Scholar]
- 115.Lavergne M, Janus-Bell E, Schaff M, Gachet C, Mangin PH. Platelet Integrins in Tumor Metastasis: Do They Represent a Therapeutic Target? Cancers (Basel) 2017;9 doi: 10.3390/cancers9100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ni H, Freedman J. Platelets in hemostasis and thrombosis: role of integrins and their ligands. Transfus Apher Sci. 2003;28:257–264. doi: 10.1016/S1473-0502(03)00044-2. [DOI] [PubMed] [Google Scholar]
- 117.Geng JG, Chen M, Chou KC. P-selectin cell adhesion molecule in inflammation, thrombosis, cancer growth and metastasis. Curr Med Chem. 2004;11:2153–2160. doi: 10.2174/0929867043364720. [DOI] [PubMed] [Google Scholar]
- 118.Nasti TH, Bullard DC, Yusuf N. P-selectin enhances growth and metastasis of mouse mammary tumors by promoting regulatory T cell infiltration into the tumors. Life Sci. 2015;131:11–18. doi: 10.1016/j.lfs.2015.02.025. [DOI] [PubMed] [Google Scholar]
- 119.Tinoco R, Otero DC, Takahashi AA, Bradley LM. PSGL-1: A New Player in the Immune Checkpoint Landscape. Trends Immunol. 2017;38:323–335. doi: 10.1016/j.it.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gacche RN, Meshram RJ. Targeting tumor micro-environment for design and development of novel anti-angiogenic agents arresting tumor growth. Prog Biophys Mol Biol. 2013;113:333–354. doi: 10.1016/j.pbiomolbio.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 121.van Cruijsen H, Giaccone G, Hoekman K. Epidermal growth factor receptor and angiogenesis: Opportunities for combined anticancer strategies. Int J Cancer. 2005;117:883–888. doi: 10.1002/ijc.21479. [DOI] [PubMed] [Google Scholar]
- 122.Shi YH, Fang WG. Hypoxia-inducible factor-1 in tumour angiogenesis. World J Gastroenterol. 2004;10:1082–1087. doi: 10.3748/wjg.v10.i8.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ferrari G, Cook BD, Terushkin V, Pintucci G, Mignatti P. Transforming growth factor-beta 1 (TGF-beta1) induces angiogenesis through vascular endothelial growth factor (VEGF)-mediated apoptosis. J Cell Physiol. 2009;219:449–458. doi: 10.1002/jcp.21706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lazarovici P, Gazit A, Staniszewska I, Marcinkiewicz C, Lelkes PI. Nerve growth factor (NGF) promotes angiogenesis in the quail chorioallantoic membrane. Endothelium. 2006;13:51–59. doi: 10.1080/10623320600669053. [DOI] [PubMed] [Google Scholar]
- 125.Zhang W, Stoica G, Tasca SI, Kelly KA, Meininger CJ. Modulation of tumor angiogenesis by stem cell factor. Cancer Res. 2000;60:6757–6762. [PubMed] [Google Scholar]
- 126.Scully S, Francescone R, Faibish M, Bentley B, Taylor SL, Oh D, Schapiro R, Moral L, Yan W, Shao R. Transdifferentiation of glioblastoma stem-like cells into mural cells drives vasculogenic mimicry in glioblastomas. J Neurosci. 2012;32:12950–12960. doi: 10.1523/JNEUROSCI.2017-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chang YS, di Tomaso E, McDonald DM, Jones R, Jain RK, Munn LL. Mosaic blood vessels in tumors: frequency of cancer cells in contact with flowing blood. Proc Natl Acad Sci USA. 2000;97:14608–14613. doi: 10.1073/pnas.97.26.14608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Feng W, Madajka M, Kerr BA, Mahabeleshwar GH, Whiteheart SW, Byzova TV. A novel role for platelet secretion in angiogenesis: mediating bone marrow-derived cell mobilization and homing. Blood. 2011;117:3893–3902. doi: 10.1182/blood-2010-08-304808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kraemer BF, Schmidt C, Urban B, Bigalke B, Schwanitz L, Koch M, Seizer P, Schaller M, Gawaz M, Lindemann S. High shear flow induces migration of adherent human platelets. Platelets. 2011;22:415–421. doi: 10.3109/09537104.2011.556277. [DOI] [PubMed] [Google Scholar]
- 130.Au P, Tam J, Fukumura D, Jain RK. Bone marrow-derived mesenchymal stem cells facilitate engineering of long-lasting functional vasculature. Blood. 2008;111:4551–4558. doi: 10.1182/blood-2007-10-118273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bexell D, Gunnarsson S, Tormin A, Darabi A, Gisselsson D, Roybon L, Scheding S, Bengzon J. Bone marrow multipotent mesenchymal stroma cells act as pericyte-like migratory vehicles in experimental gliomas. Mol Ther. 2009;17:183–190. doi: 10.1038/mt.2008.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wang Q, Li Z, Sun L, Chen B, Zhao Y, Shen B, Zhu M, Zhao X, Xu C, Wang M, Xu W, Zhu W. Platelets enhance the ability of bone-marrow mesenchymal stem cells to promote cancer metastasis. Onco Targets Ther. 2018;11:8251–8263. doi: 10.2147/OTT.S181673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cuzick J, Otto F, Baron JA, Brown PH, Burn J, Greenwald P, Jankowski J, La Vecchia C, Meyskens F, Senn HJ, Thun M. Aspirin and non-steroidal anti-inflammatory drugs for cancer prevention: an international consensus statement. Lancet Oncol. 2009;10:501–507. doi: 10.1016/S1470-2045(09)70035-X. [DOI] [PubMed] [Google Scholar]
- 134.Chen WY, Holmes MD. Role of Aspirin in Breast Cancer Survival. Curr Oncol Rep. 2017;19:48. doi: 10.1007/s11912-017-0605-6. [DOI] [PubMed] [Google Scholar]
- 135.Gutiontov SI, Choe KS, Miller JL, Liauw SL. Improved outcomes after radiotherapy for prostate cancer: Anticoagulation, antiplatelet therapy, and platelet count as key factors in disease progression. Cancer Med. 2020;9:4667–4675. doi: 10.1002/cam4.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Eckert F, Schilbach K, Klumpp L, Bardoscia L, Sezgin EC, Schwab M, Zips D, Huber SM. Potential Role of CXCR4 Targeting in the Context of Radiotherapy and Immunotherapy of Cancer. Front Immunol. 2018;9:3018. doi: 10.3389/fimmu.2018.03018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Haque S, Morris JC. Transforming growth factor-β: A therapeutic target for cancer. Hum Vaccin Immunother. 2017;13:1741–1750. doi: 10.1080/21645515.2017.1327107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Smith DC, Eisenberg PD, Manikhas G, Chugh R, Gubens MA, Stagg RJ, Kapoun AM, Xu L, Dupont J, Sikic B. A phase I dose escalation and expansion study of the anticancer stem cell agent demcizumab (anti-DLL4) in patients with previously treated solid tumors. Clin Cancer Res. 2014;20:6295–6303. doi: 10.1158/1078-0432.CCR-14-1373. [DOI] [PubMed] [Google Scholar]
- 139.Massard C, Azaro A, Soria JC, Lassen U, Le Tourneau C, Sarker D, Smith C, Ohnmacht U, Oakley G, Patel BKR, Yuen ESM, Benhadji KA, Rodon J. First-in-human study of LY3039478, an oral Notch signaling inhibitor in advanced or metastatic cancer. Ann Oncol. 2018;29:1911–1917. doi: 10.1093/annonc/mdy244. [DOI] [PubMed] [Google Scholar]
- 140.Jimeno A, Gordon M, Chugh R, Messersmith W, Mendelson D, Dupont J, Stagg R, Kapoun AM, Xu L, Uttamsingh S, Brachmann RK, Smith DC. A First-in-Human Phase I Study of the Anticancer Stem Cell Agent Ipafricept (OMP-54F28), a Decoy Receptor for Wnt Ligands, in Patients with Advanced Solid Tumors. Clin Cancer Res. 2017;23:7490–7497. doi: 10.1158/1078-0432.CCR-17-2157. [DOI] [PubMed] [Google Scholar]
- 141.Ando Y, Iwasa S, Takahashi S, Saka H, Kakizume T, Natsume K, Suenaga N, Quadt C, Yamada Y. Phase I study of alpelisib (BYL719), an α-specific PI3K inhibitor, in Japanese patients with advanced solid tumors. Cancer Sci. 2019;110:1021–1031. doi: 10.1111/cas.13923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hwang SY, Park S, Kwon Y. Recent therapeutic trends and promising targets in triple negative breast cancer. Pharmacol Ther. 2019;199:30–57. doi: 10.1016/j.pharmthera.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 143.Schott AF, Goldstein LJ, Cristofanilli M, Ruffini PA, McCanna S, Reuben JM, Perez RP, Kato G, Wicha M. Phase Ib Pilot Study to Evaluate Reparixin in Combination with Weekly Paclitaxel in Patients with HER-2-Negative Metastatic Breast Cancer. Clin Cancer Res. 2017;23:5358–5365. doi: 10.1158/1078-0432.CCR-16-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kurtz JE, Dufour P. Adecatumumab: an anti-EpCAM monoclonal antibody, from the bench to the bedside. Expert Opin Biol Ther. 2010;10:951–958. doi: 10.1517/14712598.2010.482098. [DOI] [PubMed] [Google Scholar]
- 145.Katoh M, Katoh M. Precision medicine for human cancers with Notch signaling dysregulation (Review) Int J Mol Med. 2020;45:279–297. doi: 10.3892/ijmm.2019.4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stover DG, Gil Del Alcazar CR, Brock J, Guo H, Overmoyer B, Balko J, Xu Q, Bardia A, Tolaney SM, Gelman R, Lloyd M, Wang Y, Xu Y, Michor F, Wang V, Winer EP, Polyak K, Lin NU. Phase II study of ruxolitinib, a selective JAK1/2 inhibitor, in patients with metastatic triple-negative breast cancer. NPJ Breast Cancer. 2018;4:10. doi: 10.1038/s41523-018-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Montero AJ, Escobar M, Lopes G, Glück S, Vogel C. Bevacizumab in the treatment of metastatic breast cancer: friend or foe? Curr Oncol Rep. 2012;14:1–11. doi: 10.1007/s11912-011-0202-z. [DOI] [PMC free article] [PubMed] [Google Scholar]