Abstract
Oxalate is a metabolite consumed in nuts, beans and leaves, and excreted in urine. Oxalosis can cause nephropathy. We describe a rare case of a high-oxalate diet intended for irritable bowel syndrome (IBS) treatment causing oxalate nephropathy. A 59-year-old woman with a history of controlled hypertension presented with creatinine 1.8 mg/dL, increased from baseline 1.3 mg/dL. She denied recent illness, urinary stones, medication adjustments, herbal supplements and non-steroidal anti-inflammatory drugs use. Diet included six tablespoons of chia seeds and five handfuls of almonds daily to manage IBS symptoms. Her electrolytes, urinalysis and renal ultrasound were unremarkable. Her 24-hour urine output revealed increased oxalate and low citrate. Renal biopsy showed glomerulosclerosis, fibrosis and calcium oxalate deposition. She switched to a low-oxalate diet, with improvement in laboratory markers. An earlier dietary history could have raised concern for oxalosis prior to renal biopsy. Providers should be trained to identify at-risk patients and provide appropriate dietary counselling.
Keywords: diet, acute renal failure, irritable bowel syndrome
Background
Oxalate is an organic acid and end product of ascorbic acid metabolism in humans and plants. In humans, dietary free oxalate is absorbed in the stomach, distal small intestine and colon; oxalate bound to calcium, iron and magnesium is excreted in faeces.1 Serum oxalate is excreted in urine and excessive filtration can cause calcium oxalate stones or nephropathy. Oxalate nephropathy (ON), is a rare form of kidney injury from calcium oxalate crystal deposition in the kidney parenchyma. It can lead to tubular damage, interstitial inflammation and fibrosis that can cause acute or chronic renal failure, and may progress to end-stage renal disease. Oxalosis is most commonly caused by fat malabsorption, but other factors include mineral deficiencies, fasting states, loss of oxalate, degrading microbes, genetic defects in metabolism and diet.2 3 We describe a rare case of a high-oxalate diet, recommended for irritable bowel syndrome (IBS) treatment, causing ON.
Case presentation
A 59-year-old Caucasian woman with chronic kidney disease stage 3bA1 of unknown aetiology, IBS, osteoporosis, controlled hypertension and hyperthyroidism was found to have acute-on-chronic kidney injury during routine follow-up with her nephrologist. She denied recent illnesses, change in urine, lower extremity edema and history of urinary stones. She denied non-steroidal anti-inflammatory drugs, vitamin, antibiotic and herbal supplement use. Medications included amlodipine and methimazole. She was a non-smoker, drank alcohol occasionally and denied illicit drug use.
Investigations
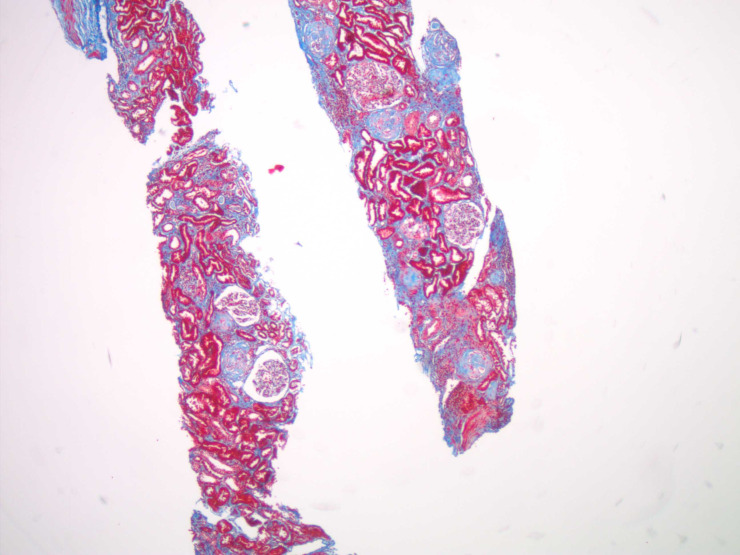
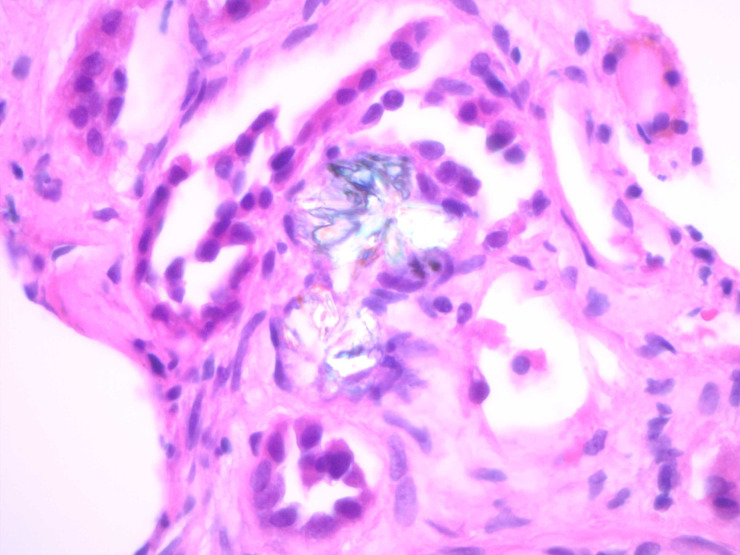
Her laboratory workup was significant for an increase in creatinine to 1.8 mg/dL from 1.34 mg/dL, 6 months earlier. Electrolytes were in normal range. Urinalysis was negative for proteinuria or haematuria. Renal ultrasound showed normal kidneys without stones, masses, hydronephrosis or increased echogenicity. She underwent renal biopsy which showed diffuse global glomerulosclerosis with prominent subcapsular fibrosis, tubular atrophy, severe interstitial fibrosis involving 60% of the cortex (figure 1) and calcium oxalate deposition (figure 2) on light microscopy. Her immunofluorescence and electron microscopy results were unremarkable. She completed a 24-hour urine collection, revealing adequate urine output (3.18 L/day), high oxalate (101 mg/day, normal (nl) 20–40 mg/day), normal calcium level (55 mg/day, nl 51–262 mg/day), low urine pH (5.35, nl 5.8–6.2) and low citrate (496 mg/day, nl >550 mg/day).
Figure 1.
Trichrome taken at 40× magnification showing the background fibrosis and glomerulosclerosis.
Figure 2.
H&E stain taken at 600× magnification with polarisation showing a couple of calcium oxalate deposits within renal tubules.
After the investigation, a diet history was obtained. She reported following the ‘virgin diet’ to treat her IBS symptoms for the past 6 years, which comprised avoiding gluten, dairy, eggs, soy, peanuts, corn and sugar/artificial sweeteners. Finding digestive relief from chia seeds, in the past year, she ingested six tablespoons of chia seeds and five handful of almonds daily, with an estimated intake of 1 g of soluble oxalate daily compared with the normal western diet of <200 mg/day.1
Treatment
Based on the high oxalate content of her urine collection and calcium oxalate deposition on kidney biopsy, she was counselled to switch to a low-oxalate diet with high fluid intake. She started calcium carbonate with meals and worked with a nutritionist.
Outcome and follow-up
Follow-up labs 2 months later showed improved creatinine to 1.57 mg/dL, and it has remained at her baseline 1.3–1.6 mg/dL. Repeat 24-hour urine testing showed normalised oxalate (33 mg/day) and citrate (624 mg/day) excretion, with pH 7.2 (nl 5.8–6.2). Since cutting down on nuts and changing her diet, she has lost weight. She exercises daily and her blood pressures have remained with systolics at 110–120 mm Hg. She also started denosumab injections every 6 months for osteoporosis.
Discussion
This case demonstrates diet-induced oxalosis causing calcium oxalate deposition in the kidneys. It exposes the unintended consequences of consuming large quantities of almonds and seeds for suspected health benefits of improving IBS symptoms and highlights the close relationship between nutrition, the gastrointestinal tract and kidney health.
Oxalosis can be either primary from genetic enzyme deficiencies or secondary from increase in oxalate absorption from the gastrointestinal tract.4 Normally, small amounts of free oxalate are absorbed by the stomach, distal small intestines and colon in humans.2 5 Oxalate also binds calcium, iron and magnesium, and in the gut this gets excreted with faeces. Any host or dietary factor that alters the amount of free oxalate influences absorption.2 The most common cause of secondary oxalosis is from fat malabsorption, responsible for 88% of cases in a systematic review by Lumlertgul et al.6 Conditions that cause fat malabsorption, such as gastric bypass surgery, Crohn’s disease, coeliac sprue, pancreatic deficiency and medications leave more free oxalate available for absorption. This is because fat has a greater affinity for calcium than oxalate. Calcium, iron and magnesium deficiencies as well as fasting states can also increase oxalate absorption. The microbiome, including Oxalobacter formigenes and Lactobacillus acidophilus, plays an important role in degrading oxalate.3 The diversity and extent of these gut bacteria fluctuates in response to dietary oxalate and antibiotics, further influencing oxalosis.3 Diets high in free oxalate also result in increased absorption.5
Dietary oxalate comes primarily from plants. It is found in higher concentrations in the leaves and seeds. Foods known to have high levels of oxalate include nuts, beans, tea, spinach and kale, rhubarb, beets, potato skins, soy and cocoa. Vitamin C is also a potent source of oxalate as it is an end product of metabolism,.2 Absorption rates vary between foods depending on the content of soluble oxalate, which is more bioavailable,2 7 Tea has a significantly higher percentage of oxalate absorption compared with spinach and rhubarb.2 Almonds, Brazil and pine nuts contain nearly twice as much soluble oxalate, compared with peanuts, pistachios and chestnuts.8
Our patient consumed a high-oxalate diet as a result of following a popular diet for digestive health. The virgin diet, promoted to alleviate food intolerances and IBS, advocates elimination of certain foods and consumption of greens, nuts and seeds. In response, our patient consumed an estimated five times the typical quantity of oxalate daily. She ingested approximately 150 g of almonds daily (147–250 mg of gastric soluble oxalate/100 g and 216–305 mg of intestinal insoluble oxalate/100 g) and six tablespoons (1/8 cup) of chia seeds (380 mg oxalate/one-quarter cup), which ultimately caused kidney injury.1 While high-oxalate foods are nutritional, oxalosis can be harmful. Case reports have documented diet-induced ON secondary to spinach, kale, berries, nuts and nut milk, cocoa powder, wheat germ, green smoothies, chagas mushrooms and vitamin C supplements.9–14 The majority followed this diet for presumed health benefits and had partial recovery with restriction of oxalate consumption, increased oral hydration and calcium acetate supplementation to bind gut oxalate.
This case proves the importance of taking a thorough dietary history. In our case, a dietary history could have raised a concern for oxalosis earlier. While hypertension may have also contributed to the development of interstitial fibrosis, the patient’s blood pressure was controlled at the time of biopsy, thus the major intervention after completing the biopsy and urine collection was dietary counselling. At-risk patients with pre-existing gastrointestinal disease, kidney disease or mineral deficiencies should be counselled on the effect of high-oxalate diets on the kidneys. Vegetarians, who may consume greater quantities of foods rich in oxalate may also be vulnerable. Education on cooking techniques, such as soaking and cooking plants to help leach oxalate, fluid hydration, balancing high-oxalate diets with foods rich in free calcium, magnesium and iron, and limiting consumption of tea and nuts is important.2
Given the popularity of fad diets, the curriculum in physician training should include nutrition education. Providers must learn to take a dietary history and be prepared to provide appropriate counselling.
Learning points.
While oxalate nephropathy is a less common cause of kidney disease, it should be considered when patients present with chronic kidney disease or acute-on-chronic kidney injury, particularly in patients with history of pre-existing gastrointestinal, kidney or mineral disease.
A thorough dietary history is extremely important in disease prevention, intervention and management.
Curriculum in physician training should include nutrition education so that providers are comfortable discussing diet and can provide appropriate counselling.
Footnotes
Contributors: VG is the corresponding and first author. She is a third-year Internal Medicine resident (PGY3) at the George Washington University. She performed the literature review, wrote and revised the manuscript under consideration. LH was the pathologist on the case and prepared the slides. The senior author, RR is the patient’s current nephrologist. She gave guidance for the paper, and helped with editing and revising the manuscript. All authors have accountability and responsibility for the work and have approved of the final product.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer-reviewed.
References
- 1.Taylor EN, Curhan GC. Oxalate intake and the risk for nephrolithiasis. J Am Soc Nephrol 2007;18:2198–204. 10.1681/ASN.2007020219 [DOI] [PubMed] [Google Scholar]
- 2.Noonan SC, Savage GP. Oxalate content of foods and its effect on humans. Asia Pac J Clin Nutr 1999;8:64–74. [PubMed] [Google Scholar]
- 3.Miller AW, Oakeson KF, Dale C, et al. Effect of dietary oxalate on the gut microbiota of the mammalian herbivore Neotoma albigula. Appl Environ Microbiol 2016;82:2669–75. 10.1128/AEM.00216-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glew RH, Sun Y, Horowitz BL, et al. Nephropathy in dietary hyperoxaluria: a potentially preventable acute or chronic kidney disease. World J Nephrol 2014;3:122–42. 10.5527/wjn.v3.i4.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaeger P, Robertson WG. Role of dietary intake and intestinal absorption of oxalate in calcium stone formation. Nephron Physiol 2004;98:p64–71. 10.1159/000080266 [DOI] [PubMed] [Google Scholar]
- 6.Lumlertgul N, Siribamrungwong M, Jaber BL, et al. Secondary Oxalate Nephropathy: A Systematic Review. Kidney Int Rep 2018;3:1363–72. 10.1016/j.ekir.2018.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimmermann DJ, Hesse A, von Unruh GE. Influence of a high-oxalate diet on intestinal oxalate absorption. World J Urol 2005;23:324–9. 10.1007/s00345-005-0028-0 [DOI] [PubMed] [Google Scholar]
- 8.Ritter MMC, Savage GP. Soluble and insoluble oxalate content of nuts. Journal of Food Composition and Analysis 2007;20:169–74. 10.1016/j.jfca.2006.12.001 [DOI] [Google Scholar]
- 9.Clark B, Baqdunes MW, Kunkel GM. Diet-Induced oxalate nephropathy. BMJ Case Rep 2019;12:e231284. 10.1136/bcr-2019-231284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khneizer G, Al-Taee A, Mallick MS, et al. Chronic dietary oxalate nephropathy after intensive dietary weight loss regimen. J Nephropathol 2017;6:126–9. 10.15171/jnp.2017.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun Y, Horowitz BL, Servilla KS, et al. Chronic nephropathy from dietary hyperoxaluria: sustained improvement of renal function after dietary intervention. Cureus 2017;9:e1105. 10.7759/cureus.1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Syed F, Mena-Gutierrez A, Ghaffar U. A case of iced-tea nephropathy. N Engl J Med 2015;372:1377–8. 10.1056/NEJMc1414481 [DOI] [PubMed] [Google Scholar]
- 13.Makkapati S, D'Agati VD, Balsam L, et al. "Green Smoothie Cleanse" Causing Acute Oxalate Nephropathy. Am J Kidney Dis 2018;71:281–6. 10.1053/j.ajkd.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 14.Kikuchi Y, Seta K, Ogawa Y, et al. Chaga mushroom-induced oxalate nephropathy. Clin Nephrol 2014;81:440–4. 10.5414/CN107655 [DOI] [PubMed] [Google Scholar]