Abstract
Background:
Both an elevated posterior tibial slope (PTS) and high-grade anterior knee laxity are often present in patients who undergo revision anterior cruciate ligament (ACL) surgery, and these conditions are independent risk factors for ACL graft failure. Clinical data on slope-correction osteotomy combined with lateral extra-articular tenodesis (LET) do not yet exist.
Purpose:
To evaluate the outcomes of patients undergoing revision ACL reconstruction (ACLR) and slope-correction osteotomy combined with LET.
Study Design:
Case series; Level of evidence, 4.
Methods:
Between 2016 and 2018, we performed a 2-stage procedure: slope-correction osteotomy was performed first, and then revision ACLR in combination with LET was performed in 22 patients with ACLR failure and high-grade anterior knee laxity. Twenty patients (6 women and 14 men; mean age, 27.8 ± 8.6 years; range, 18-49 years) were evaluated, with a mean follow-up of 30.5 ± 9.3 months (range, 24-56 months), in this retrospective case series. Postoperative failure was defined as a side-to-side difference of ≥5 mm in the Rolimeter test and a pivot-shift grade of 2 or 3.
Results:
The PTS decreased from 15.3° to 8.9°, the side-to-side difference decreased from 7.2 to 1.1 mm, and the pivot shift was no longer evident in any of the patients. No patients exhibited revision ACLR failure and all patients showed good to excellent postoperative functional scores (mean ± SD: visual analog scale, 0.5 ± 0.6; Tegner, 6.1 ± 0.9; Lysholm, 90.9 ± 6.4; Knee injury and Osteoarthritis Outcome Score [KOOS] Symptoms, 95.2 ± 8.4; KOOS Pain, 94.7 ± 5.2; KOOS Activities of Daily Living, 98.5 ± 3.2; KOOS Function in Sport and Recreation, 86.8 ± 12.4; and KOOS Quality of Life, 65.4 ± 14.9).
Conclusion:
Slope-correction osteotomy in combination with LET is a safe and reliable procedure in patients with high-grade anterior knee laxity and a PTS of ≥12°. Normal knee joint stability was restored and good to excellent functional scores were achieved after a follow-up of at least 2 years.
Keywords: high-grade anterior knee instability, increased posterior tibial slope, revision anterior cruciate ligament reconstruction, slope-correction osteotomy
Significantly higher failure rates have been observed after revision anterior cruciate ligament (ACL) surgery than after primary ACL reconstruction (ACLR).14,37 In recent years, technical errors in ACLR have often been the focus of failure analysis and revision strategies. Moreover, peripheral structures and bony alignment of the knee, such as lesions of the anterolateral structures or an elevated posterior tibial slope (PTS), have been identified as risk factors for ACLR failure.31
A number of biomechanical studies have shown that insufficiency of the anterolateral structures increases anterior knee translation, pivot shift, and internal rotation and results in high-grade anterior knee laxity.10 While studies have demonstrated that high-grade anterior knee laxity is a risk factor for ACLR failure, additionally performing lateral extra-articular tenodesis (LET) reduces the risk of ACLR and revision ACLR failure.12,23
An elevated PTS also increases the magnitude of anterior tibial translation (ATT). Biomechanical studies have demonstrated that a high force on the ACL may contribute to ACLR failure.17,38 There are a number of recommendations for surgically treating an elevated PTS in patients undergoing revision ACLR,4,27,34 but a large case series has not been published to date.
To the best of our knowledge, slope-correction osteotomy combined with LET to restore knee stability has not been examined before.
The aim of this study was to present the clinical results of a 2-stage slope-correction osteotomy (proximal tibial anterior closed-wedge osteotomy) in combination with revision ACLR and LET. We hypothesized that slope-correction osteotomy with revision ACLR and LET in patients with an increased PTS and high-grade anterior knee laxity is a safe procedure and can effectively restore normal knee stability.
Methods
Study Population
Between 2016 and 2018, we consecutively performed a 2-stage procedure: slope-correction osteotomy (proximal tibia anterior closed-wedge osteotomy) was performed first, and then autograft revision ACLR in combination with LET was performed in 22 patients with ACLR failure and high-grade anterior knee laxity. All surgical procedures were performed by 2 experienced surgeons (K.-H.F. and R.A.) and the data were retrospectively retrieved by searching the records of all surgical procedures for the terms “slope-correction osteotomy” and “revision ACLR.” Patients with ACLR failure, high-grade anterior knee laxity (a side-to-side difference of ≥6 mm), and a PTS of ≥12° were included in the retrospective case series.
The exclusion criteria were posterior knee laxity, a PTS of ≤11°, and hyperlaxity with hyperextension of the knee by >5°. Two patients were lost to follow-up and thus were not included in the study. Subsequently, 20 patients were clinically examined with a mean follow-up of 30.5 ± 9.3 months (range, 24-56 months). The patients were contacted by telephone 2 years after revision ACLR, and after they provided consent to participate in the study, they were invited for an examination. At the time of follow-up, the Lysholm, Tegner, subjective International Knee Documentation Committee (IKDC), and Knee injury and Osteoarthritis Outcome Score (KOOS) scores were recorded, and subjective pain was quantified by visual analog scale (VAS).2,18,21,32 The pivot-shift test was administered pre- and postoperatively, and the grades were as follows: grade 1, glide; grade 2, clunk; and grade 3, gross. Postoperative failure was defined as a side-to-side difference of ≥5 mm in the Rolimeter test and a pivot-shift grade of 2 or 3. All clinical examinations were performed by an experienced examiner (L.A.). Full-leg standing radiographs were taken to determine malalignment of the leg. The range of motion (ROM), in particular the extension of the knee, was assessed in comparison with that of the contralateral side. An extension ROM of 0° to 5° on the ipsilateral side was defined as normal. Deviation from this range was defined as an extension deficit (<0°) or hyperextension (>5°). Symptomatic hyperextension was defined as painful dorsal penetration of the knee joint when walking or standing, pain in the popliteal fossa, or similar symptoms due to hyperextension. The study design was approved by the local ethics committee (No. 3293).
Measurement and Definition of PTS
The PTS was measured as previously described.3,26 The angle between the anatomic axis of the lateral tibia and the medial tibial plateau was determined. The middiaphysis of the tibia was marked at 90 mm and 150 mm below the joint line using the circle 3-point method. The circles were digitally drawn in the center of the diaphysis, reaching the anterior and posterior border of the tibial shaft (Figure 1). In this manner, the normal PTS was defined as 8.01°± 2.93°.20
Figure 1.
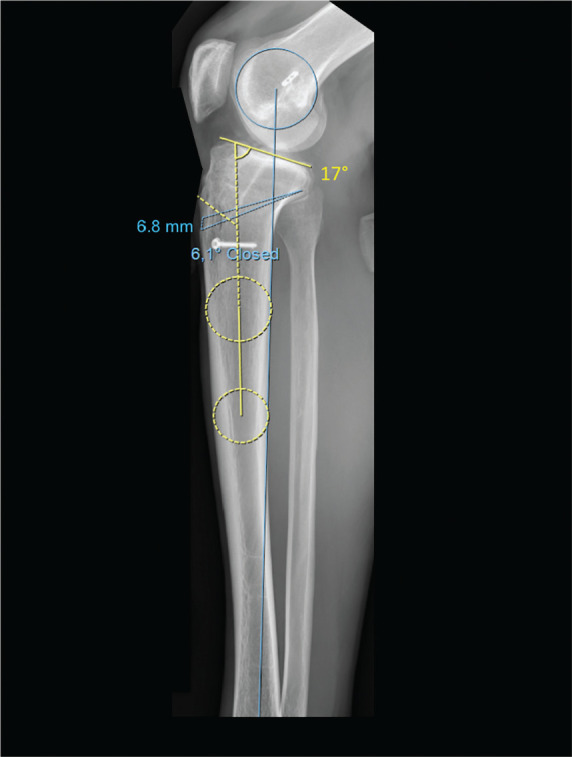
Measurement of the posterior tibial slope in the lateral radiograph of the tibia using the circle 3-point method and planning of the osteotomy. The angle between the middiaphysis at 90-150 mm below the joint line (center of the dotted circles) and the joint line minus 90° gives the PTS, (17°, yellow angle). The correction angle was 6.1° (blue angle) and the height of the osteotomy gap was 6.8 mm.
Surgical Technique
All slope-correction osteotomies were performed with 2-stage revision ACLR. The osteotomy was performed in the first session; the remaining graft was resected and the bone tunnel was filled with allogenic cancellous bone. After the osteotomy healed and the allogenic bone integrated with the bone tunnels, revision ACLR was performed no earlier than 4 months after the previous surgery.
Preoperative osteotomy planning was performed with Sectra 2-dimensional planning system software (Sectra) and the target PTS was 8° to 10°. The upper part of the osteotomy angle was placed to be 2 to 3 cm distal to the proximal edge of the tibial tuberosity, and the hinge point of the osteotomy was placed in the center of the tibial bony insertion of the posterior cruciate ligament (Figure 2).
Figure 2.
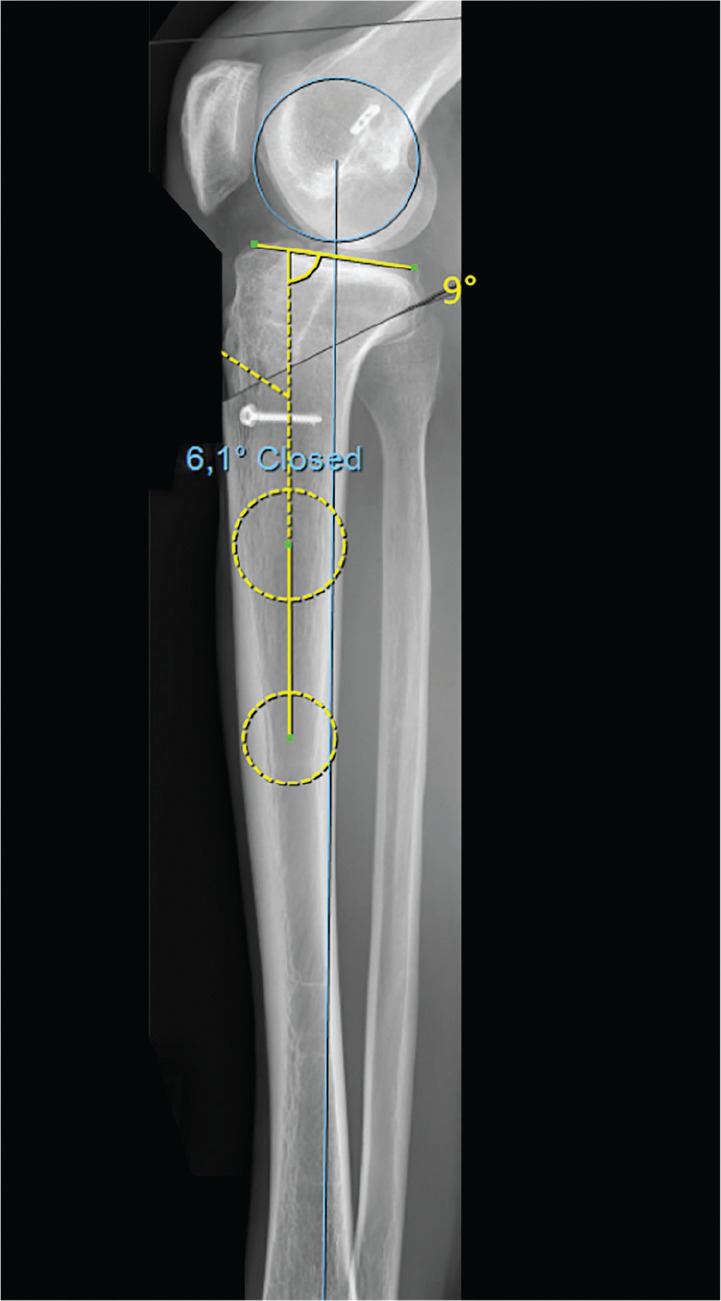
Preoperative planning and simulation of the osteotomy. A correction angle of 6.1° reduces the PTS (yellow angle) to 9°. Middiaphysis 90-150 mm below the joint line is marked by the dotted circles.
A longitudinal incision of 4 to 6 cm was made medial to the tuberosity of the tibia. A tuberosity osteotomy was performed with an oscillating saw under constant cooling, and a tuberosity fragment that was approximately 7 to 10 cm long and approximately 1.5 to 2 cm wide was attached to the patellar tendon (Figure 3). The tuberosity fragment was looped upward at the patellar tendon and an oscillating saw was used to make the ventrally wedge-shaped osteotomy (Figure 4).
Figure 3.

Tuberosity osteotomy with the oscillating saw via a medial skin incision of approximately 4 to 6 cm.
Figure 4.

The tuberosity was looped upward at the patellar tendon and the anterior closed-wedge osteotomy was performed.
The bone wedge was used to additionally fill the ACL bone tunnels. The osteotomy was extended medially and laterally with a chisel or an osteotome until it could be ventrally closed. The tuberosity was then placed back on the osteotomy and fixed with at least three 3.5-mm lag screws proximally and distally to the osteotomy (Figure 5). The tuberosity was used as a “bioplate” to stabilize the osteotomy, and additional screws were used.
Figure 5.
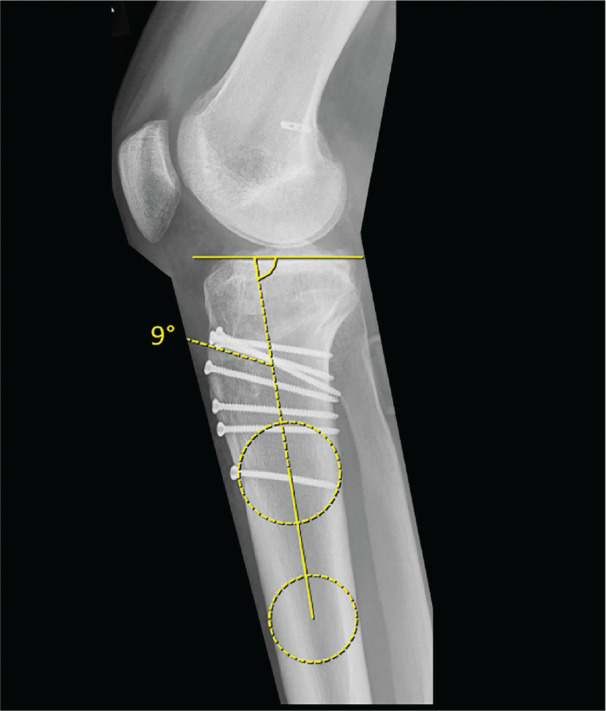
The slope-correction osteotomy was stabilized with the tuberosity, which was used as a “bioplate.” According to the preoperative planning, the postoperative PTS was 9° (angle). Middiaphysis 90-150 mm below the joint line is marked by the dotted circles.
All revision ACLR procedures were single-bundle ACLR procedures with autografts, the type of which depended on the previously harvested grafts. Our first choice was hamstring tendons, followed by bone–patellar tendon–bone or quadriceps grafts. During revision ACLR, the femoral and tibial tunnels were placed with the anteromedial portal technique under fluoroscopic control.
In all cases, lateral extra-articular tenodesis was additionally performed. Via a 4-cm skin incision made over the lateral epicondyle, a wide strip of the distal iliotibial band (6-8 cm long and 6-8 mm wide) was prepared, and the connection to the Gerdy tubercle was preserved. The free end was secured with a Vicryl suture and a 2.4-mm K-wire was inserted into the lateral femur approximately 1 cm proximal and posterior to the lateral epicondyle. If the graft showed slight tension in extension, a 5- to 6-mm drill channel was made over the 2.4-mm K-wire, and tenodesis was performed at 45° of knee flexion and a neutral rotation angle, with fixation using an interference screw. LET was performed superficially over the lateral collateral ligament.
Postoperative Rehabilitation
Slope-Correction Osteotomy and Bone Filling with Allogenic Cancellous Bone
On the first postoperative day, physical therapy was started; it included movement exercises, training and walking with crutches on the floor and stairs, and decongestant measures, including lymph drainage if necessary. Partial weightbearing (20 kg) was recommended for 6 weeks, and full ROM was allowed. Oral vitamin D supplementation for 3 to 6 months was recommended for nonunion prophylaxis. Outpatient physical therapy for the restoration of normal muscle function was recommended for 6 to 12 weeks.
Postoperative Protocol After Revision ACLR and LET
Postoperative treatment was administered according to our standard protocol after revision ACL reconstruction. All patients were treated with a dynamic knee brace immediately after surgery for 6 weeks with ROM limitations for 6 weeks (weeks 1-2: 30° of knee flexion, weeks 3-4: 60° of knee flexion, weeks 5-6: 90° of knee flexion). Physical therapy was started on the first postoperative day, and full extension, quadriceps stimulation, and decongestant therapy were started as soon as possible. After the sixth week, the goals were to regain full ROM and muscle function. Another goal was for patients to return to nonpivoting sports (jogging, cycling, etc) at 6 months.
Statistical Analysis
The descriptive statistics are expressed as means and standard deviations. The mean differences between the pre- and postoperative scores were calculated with the unpaired Student t test for normally distributed parameters and the Kruskal-Wallis test for nonnormally distributed parameters.
Statistical analysis was performed using IBM SPSS Statistics, Version 22. P < .05 was considered significant.
Results
Patient characteristics are displayed in Table 1. There were 20 patients (6 women and 14 men; mean age, 27.8 ± 8.6 years; range, 18-49 years) who were clinically evaluated after revision ACLR and slope-correction osteotomy. All patients reported having symptomatic laxity without the recurrence of trauma after the previous ACLR (Table 1). In 2 patients, there were preoperative extension deficits, which were resolved by the time of the follow-up. No patients exhibited revision ACLR failure.
Table 1.
Patient Characteristics (N = 20) a
| No. (%) | |
|---|---|
| Female sex | 6 (30) |
| Left knee | 11 (55) |
| BMI >30 kg/m2 | 2 (10) |
| Atraumatic mechanism of graft failure preoperatively | 20 (100) |
| Failed revision ACLR | 0 |
| Choice of revision ACLR graft | |
| Bone–patellar tendon–bone | 1 (5) |
| Hamstring tendon | 7 (35) |
| Quadriceps tendon | 12 (60) |
| Additional lateral extra-articular tenodesis | 20 (100) |
| Complications | 1 (5) |
| Preoperative femoral tunnel malposition | 5 (25) |
| Osteoarthritis | 7 (35) |
| Return to sports | 13 (65) |
ACLR, anterior cruciate ligament reconstruction; BMI, body mass index.
Three patients had hyperextension at the time of the follow-up; all cases were asymptomatic (Table 2).
Table 2.
Clinical and Radiological Findings in All Patients Pre- and Postoperatively a
| No. of Revision | Side-to-side Difference (Rolimeter), mm | Pivot-Shift Grade | Extension of the Knee, deg | PTS, deg | Coronal Alignment | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | ACL Procedures | Preop | FU | Preop | FU | Preop | FU | Preop | FU | Preop |
| 1 | 2 | 10 | 0 | 3 | 0 | N | N | 14 | 10 | N |
| 2 | 2 | 6 | 0 | 3 | 0 | N | N | 14 | 6 | N |
| 3 | 1 | 6 | 3 | 3 | 0 | N | N | 16 | 9 | N |
| 4 | 2 | 9 | 2 | 3 | 0 | N | +3 (a) | 17 | 9 | N |
| 5 | 1 | 7 | 2 | 3 | 0 | N | N | 16 | 10 | N |
| 6 | 1 | 8 | 2 | 3 | 0 | N | N | 15 | 10 | N |
| 7 | 1 | 6 | 3 | 3 | 0 | N | N | 15 | 9 | N |
| 8 | 1 | 9 | 0 | 3 | 0 | −10 | N | 15 | 8 | N |
| 9 | 2 | 6 | 1 | 3 | 0 | N | N | 13 | 7 | 4° varus |
| 10 | 3 | 7 | 0 | 3 | 0 | N | N | 15 | 10 | N |
| 11 | 1 | 6 | 1 | 3 | 0 | −5 | N | 16 | 10 | N |
| 12 | 1 | 6 | 0 | 3 | 0 | N | N | 13 | 9 | N |
| 13 | 1 | 8 | 0 | 3 | 0 | N | N | 17 | 10 | N |
| 14 | 1 | 6 | 2 | 3 | 0 | N | N | 14 | 8 | N |
| 15 | 1 | 9 | 1 | 3 | 0 | N | +3 (a) | 20 | 10 | N |
| 16 | 1 | 6 | 1 | 3 | 0 | N | 0 | 15 | 8 | N |
| 17 | 1 | 7 | 0 | 3 | 0 | N | +8 (a) | 15 | 8 | N |
| 18 | 1 | 7 | 0 | 3 | 0 | N | N | 14 | 9 | N |
| 19 | 2 | 8 | 2 | 3 | 0 | N | N | 16 | 8 | N |
| 20 | 1 | 7 | 1 | 3 | 0 | N | N | 15 | 9 | N |
| Mean ± SD | 1.3 ± 0.6 | 7.2 ± 1.3 | 1.1 ± 1.1 | 3 | 0 | 15.3 ± 11.6 | 8.9 ± 11.1 | |||
| P value | <.001 | <.001 | <.001 | |||||||
Bold indicates statistical significance. a, asymptomatic; ACL, anterior cruciate ligament; FU, follow-up; N, normal (normal extension was defined as 0-5°, normal coronal alignment means <3°); preop, preoperative; PTS, posterior tibial slope; –, extensions deficit; +, hyperextension.
The side-to-side differences in the Rolimeter test results and PTS significantly decreased from pre- to postoperatively (Table 2). All patients improved from a pivot-shift grade of 3 preoperatively to a pivot-shift grade of 0 postoperatively (P < .001) and stated that they would have undergone the operation again. In 1 case, an additional surgery was performed on the fourth day after surgery because of a postoperative hematoma. No additional intra- or postoperative complications were observed.
The preoperative ligamentous laxity grades and meniscal statuses at the time of revision surgery are demonstrated in Tables 3 and 4.
Table 3.
Meniscal Status at the Time of Revision ACLR (N = 20) a
| No. (%) | |
|---|---|
| Medial meniscal lesion in total | 12 (60) |
| Medial meniscal repair | 8 (40) |
| Partial medial meniscal resection | 3 (15) |
| Total medial meniscal resection | 1 (5) |
| Medial meniscal transplantation | 0 |
| Lateral meniscal lesion in total | 0 |
ACLR, anterior cruciate ligament reconstruction.
Table 4.
Preoperative Ligamentous Laxity a
| Preoperative | Postoperative | |
|---|---|---|
| Lachman test | 20 (100) | 1 (5) |
| Grade 1 (2-5 mm) | 0 | 1 (5) |
| Grade 2 (5-10 mm) | 11 (55) | 0 |
| Grade 3 (>10 mm) | 9 (45) | 0 |
| Lateral knee laxity | 8 (40) | 1 (5) |
| Grade 1 | 7 (35) | 1 (5) |
| Grade 2 | 1 (5) | 0 |
| Grade 3 | 0 | 0 |
| Medial knee laxity | 5 (25) | 3 (15) |
| Grade 1 | 3 (15) | 3 (15) |
| Grade 2 | 2 (10) | 0 |
| Grade 3 | 0 | 0 |
Data are reported as n (%).
Postoperative functional scores are shown in Table 5. The patients showed good to excellent postoperative functional scores–except for the KOOS Quality of Life score– and the postoperative VAS, Lysholm, and Tegner scores significantly improved from the preoperative scores.
Table 5.
Comparison of Preoperative and Postoperative Functional Scores for Slope-Correction Osteotomy Plus Revision ACLR (N = 20) a
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| VAS, points | 3.6 ± 1.5 (1-6) | 0.5 ± 0.6 (0-2) | <.001 |
| Postoperative subjective IKDC score, points | 87.4 ± 5.9 (75.9-100) | ||
| Tegner rating system, points | 2.9 ± 1.5 (0-5) | 6.1 ± 0.9 (5-8) | <.001 |
| Lysholm score, points | 49.9 ± 21 (0-70) | 90.9 ± 6.4 (76-100) | <.001 |
| KOOS postoperative, points | |||
| Symptoms | 95.2 ± 8.4 (71.43-100) | ||
| Pain | 94.7 ± 5.2 (80.56-100) | ||
| Activities of Daily Living | 98.5 ± 3.2 (87-100) | ||
| Function, Sport and Recreation | 86.8 ± 12.4 (55-100) | ||
| Quality of Life | 65.4 ± 14.9 (31.25-81.25) | ||
Data are reported as mean ± SD (range). ACLR, anterior cruciate ligament reconstruction; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; VAS, visual analog scale.
Discussion
The most important finding of this study was that slope-correction osteotomy in combination with LET in patients with revision ACLR and high-grade anterior knee laxity is a safe procedure that leads to excellent postoperative results. In a case series of 20 patients, all patients showed restored knee joint stability and good to excellent postoperative functional scores.
Biomechanical studies have demonstrated that LET decreases the force acting on the ACL and is thus able to reduce the risk of failure.7,8,11 In a case series, Trojani et al33 observed a 15% failure rate when ACLR only was performed and a 7% failure rate when ACLR in combination with LET was performed. In a systematic review, Grassi et al15 also showed that revision ACLR in combination with LET leads to good clinical results. In particular, the magnitude of pivot shift was reduced considerably by the combination of revision ACLR and LET, and in 83% of the patients, it was completely resolved at the follow-up. However, 35% of the patients had a persistent side-to-side difference of 3 to 5 mm, and 17% showed a side-to-side difference of 5 mm. The large proportion of cases in which persistent ATT could not be completely resolved indicates that even a combination of ACLR and LET cannot restore normal knee joint stability in all patients. The PTS was not considered in these 2 studies.
Previous studies have demonstrated that a PTS of ≥12° is associated with increased shear forces on the ACL and extended ATT.3,13,24,29 Salmon et al27 described an 11 times higher rate of ACL graft failure for patients with a PTS of ≥12°. An increased PTS is associated with an elevated failure rate and the development of high-grade anterior knee laxity, which is another risk factor for ACLR failure.22,23 These data indicate that patients with an increased PTS in combination with high-grade anterior laxity have a high risk of graft failure. Biomechanical studies have demonstrated that slope-correction osteotomy reduces the force on the ACL graft and decreases the ATT in the ACL-deficient knee.1,17,38 The aforementioned literature suggests that the combination of ACLR and LET as well as slope-correction osteotomy can restore knee stability and reduce the forces on the ACL graft and LET in patients with high-grade anterior knee laxity and a PTS of ≥12°.
When ACLR and LET are performed without slope-correction osteotomy in patients with high-grade anterior knee laxity with a PTS of ≥12°, the reconstructed ligament is still exposed to a high force and is therefore at risk of failing again.1 Slope-correction osteotomy can reduce the load on reconstructed ligaments.1,17,38
There are some technical notes and case reports on slope-correction osteotomy and revision ACLR, but the only case series available were published by Dejour et al,5 who studied 9 cases, and Sonnery-Cottet et al,30 who studied 5 cases.4,6,16,30,35 In line with the studies by Dejour et al and Sonnery-Cottet et al, our study showed very good clinical results and few complications.
In the biomechanical study by Imhoff et al,17 a significant reduction in the ATT was achieved by a PTS reduction of 10°, which likely resulted in a PTS of 0 to 5°. Yamaguchi et al38 observed a significant reduction in the force on the ACL after a PTS reduction of 10°. However, both studies were performed on specimens with normal PTS (mean PTS: Imhoff et al, 10°; Yamaguchi et al, 7.3°). Bernhardson et al1 recommended that the PTS be reduced to <6° based on their biomechanical data. If a PTS of 8° to 10° is assumed to be normal, Imhoff et al, Yamaguchi et al, and Bernhardson et al suggested that the PTS be reduced to a value below the physiological norm.13,20,28
Symptoms such as chronic knee pain and painful hyperextension of the knee when walking and standing, which are observed in patients with symptomatic genu recurvatum, can occur in patients with PTS deformities after, for example, epiphyseal injuries or posttraumatic deformities.19
A surgeon must be aware that a slope-correction osteotomy also entails the risk of creating symptomatic genu recurvatum. In this study, the slope-correction osteotomy led to a physiological PTS in all cases (mean PTS at follow-up, 8.9°), although an increase in knee extension was observed. Dejour et al5 observed a nonsymptomatic hyperextension angle of 5° in 2 patients, in whom the PTS decreased from an average of 13° to 4°.
This study also observed 3 patients with a nonsymptomatic hyperextension.
In line with Sonnery-Cottet et al,30 we aimed to achieve a PTS of 8° to 10°, whereas Dejour et al5 performed a slope-correction osteotomy to a mean PTS of 4° in their study. The potentially smaller reduction of the shear forces acting on the ACL by a PTS reduction <10°, to the physiological norm, might be compensated by the additional LET. Sonnery-Cottet et al also performed an additional lateral extra-articular procedure in 2 of the 5 cases.
Furthermore, the postoperative functional scores improved in the study by Sonnery-Cottet et al30 and in our study more than those of Dejour et al,5 which may be associated with the PTS being corrected to a physiological PTS (Dejour et al5: mean postoperative PTS, 4.4°; IKDC, 72; Lysholm, 74; Sonnery-Cottet et al: mean postoperative PTS, 9.2°; postoperative IKDC, 79; Lysholm, 88; and this study: mean postoperative PTS, 8.9°; IKDC, 94; Lysholm, 91).
In contrast to Dejour et al5 and Sonnery-Cottet et al,30 we performed a slope-correction osteotomy not only after multiple previous ACLR procedures but also in primary revision surgery in patients with a PTS of ≥12°. In our opinion, the indication for a slope-correction osteotomy is not the number of previous ACLR failures but the combination of a PTS of ≥12° and high-grade anterior knee laxity at the time of revision surgery.
This study has some limitations. The measurements of the PTS in the radiographs are prone to errors and the measurement method is not well validated. Many different methods of measuring the PTS have been described in the literature.3,9 A PTS of ≥12° is usually considered to be the threshold value for a PTS correction. However, standard PTS values depend on the measurement method. In the largest cohort study published to date, which was published by Weinberg et al,36 a medial PTS of 6.9 ± 3.7 and lateral PTS of 4.7 ± 3.6 were measured on 1090 cadavers. Furthermore, the authors showed that an axial rotation of the tibia by 10° leads to a PTS change of 1° to 2° on radiographs. The strict lateral adjustments of the radiographic settings reported by Weinberg et al are not possible in clinical practice. For this reason, a method of measuring PTS that was validated on the basis of the above-mentioned measurement procedure was used.20 Napier et al25 evaluated this method and the intraobserver correlation coefficient, and the results showed excellent intraobserver reliability. Another limitation of the study may be that the study population is relatively small, but it is the largest published case series on slope-correction osteotomies in combination with revision ACLR. There was no control group that received LET or osteotomy alone, so it is not possible to determine the relative contributions of each procedure to the success of the operation or to be certain that both components were necessary. The pivot shift was evaluated subjectively and this was susceptible to assessment bias.
Conclusion
Slope-correction osteotomy in combination with LET is a safe and reliable procedure during revision ACLR in patients with high-grade anterior knee laxity and a PTS of ≥12°. After a follow-up period of at least 2 years, knee joint stability was restored and good to excellent postoperative functional scores were achieved. We recommend performing an osteotomy to correct the PTS to a physiological PTS between 8° and 10°.
Footnotes
Submitted April 16, 2020; accepted July 23, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.-H.F. received royalties and payment for educational support from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296-302. [DOI] [PubMed] [Google Scholar]
- 2. Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM. Knee injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317-1329. [DOI] [PubMed] [Google Scholar]
- 3. Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745-749. [PubMed] [Google Scholar]
- 4. Dejour D, La Barbera G, Pasqualotto S, et al. Sagittal plane corrections around the knee. J Knee Surg. 2017;30(8):736-745. [DOI] [PubMed] [Google Scholar]
- 5. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846-2852. [DOI] [PubMed] [Google Scholar]
- 6. DePhillipo NN, Kennedy MI, Dekker TJ, Aman ZS, Grantham WJ, LaPrade RF. Anterior closing wedge proximal tibial osteotomy for slope correction in failed ACL reconstructions. Arthrosc Tech. 2019;8(5):e451-e457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Draganich LF, Reider B, Ling M, Samuelson M. An in vitro study of an intraarticular and extraarticular reconstruction in the anterior cruciate ligament deficient knee. Am J Sports Med. 1990;18(3):262-266. [DOI] [PubMed] [Google Scholar]
- 8. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169-176. [DOI] [PubMed] [Google Scholar]
- 9. Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):134-145. [DOI] [PubMed] [Google Scholar]
- 10. Getgood A, Brown C, Lording T, et al. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):166-176. [DOI] [PubMed] [Google Scholar]
- 11. Getgood A, Moatshe G. Lateral extra-articular tenodesis in anterior cruciate ligament reconstruction. Sports Med Arthrosc Rev. 2020;28(2):71-78. [DOI] [PubMed] [Google Scholar]
- 12. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020;48(2):285-297. [DOI] [PubMed] [Google Scholar]
- 13. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376-382. [DOI] [PubMed] [Google Scholar]
- 14. Gifstad T, Drogset JO, Viset A, Grontvedt T, Hortemo GS. Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2011-2018. [DOI] [PubMed] [Google Scholar]
- 15. Grassi A, Zicaro JP, Costa-Paz M, et al. Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg Sports Traumatol Arthrosc. 2020;28(2):418-431. [DOI] [PubMed] [Google Scholar]
- 16. Hees T, Petersen W. Anterior closing-wedge osteotomy for posterior slope correction. Arthrosc Techn. 2018;7(11):e1079-e1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imhoff FB, Mehl J, Comer BJ, et al. Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3381-3389. [DOI] [PubMed] [Google Scholar]
- 18. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600-613. [DOI] [PubMed] [Google Scholar]
- 19. Kim TW, Lee S, Yoon JR, Han HS, Lee MC. Proximal tibial anterior open-wedge oblique osteotomy: a novel technique to correct genu recurvatum. Knee. 2017;24(2):345-353. [DOI] [PubMed] [Google Scholar]
- 20. Krause M, Drenck TC, Korthaus A, Preiss A, Frosch KH, Akoto R. Patella height is not altered by descending medial open-wedge high tibial osteotomy (HTO) compared to ascending HTO. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1859-1866. [DOI] [PubMed] [Google Scholar]
- 21. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150-154. [DOI] [PubMed] [Google Scholar]
- 22. Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP. Factors associated with high-grade Lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(6):1080-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Magnussen RA, Reinke EK, Huston LJ, et al. Effect of high-grade preoperative knee laxity on 6-year anterior cruciate ligament reconstruction outcomes. Am J Sports Med. 2018;46(12):2865-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marouane H, Shirazi-Adl A, Hashemi J. Quantification of the role of tibial posterior slope in knee joint mechanics and ACL force in simulated gait. J Biomech. 2015;48(10):1899-1905. [DOI] [PubMed] [Google Scholar]
- 25. Napier RJ, Garcia E, Devitt BM, Feller JA, Webster KE. Increased radiographic posterior tibial slope is associated with subsequent injury following revision anterior cruciate ligament reconstruction. Orthop J Sports Med. 2019;7(11):2325967119879373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nerhus TK, Ekeland A, Solberg G, Sivertsen EA, Madsen JE, Heir S. Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):910-917. [DOI] [PubMed] [Google Scholar]
- 27. Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531-543. [DOI] [PubMed] [Google Scholar]
- 28. Schatka I, Weiler A, Jung TM, Walter TC, Gwinner C. High tibial slope correlates with increased posterior tibial translation in healthy knees. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2697-2703. [DOI] [PubMed] [Google Scholar]
- 29. Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223-231. [DOI] [PubMed] [Google Scholar]
- 30. Sonnery-Cottet B, Mogos S, Thaunat M, et al. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(8):1873-1880. [DOI] [PubMed] [Google Scholar]
- 31. Southam BR, Colosimo AJ, Grawe B. Underappreciated factors to consider in revision anterior cruciate ligament reconstruction: a current concepts review. Orthop J Sports Med. 2018;6(1):2325967117751689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49. [PubMed] [Google Scholar]
- 33. Trojani C, Beaufils P, Burdin G, et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1565-1570. [DOI] [PubMed] [Google Scholar]
- 34. Utzschneider S, Goettinger M, Weber P, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1643-1648. [DOI] [PubMed] [Google Scholar]
- 35. Walker J, Hartigan D, Stuart M, Krych A. Anterior closing wedge tibial osteotomy for failed anterior cruciate ligament reconstruction. J Knee Surg Rep. 2015;1(1):51-56. [Google Scholar]
- 36. Weinberg DS, Williamson DFK, Gebhart JJ, Knapik DM, Voos JE. Differences in medial and lateral posterior tibial slope: an osteological review of 1090 tibiae comparing age, sex, and race. Am J Sports Med. 2016;45(1):106-113. [DOI] [PubMed] [Google Scholar]
- 37. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yamaguchi KT, Cheung EC, Markolf KL, et al. Effects of anterior closing wedge tibial osteotomy on anterior cruciate ligament force and knee kinematics. Am J Sports Med. 2018;46(2):370-377. [DOI] [PubMed] [Google Scholar]


