Abstract
We present the case of a young obese patient with recent COVID-19 (coronavirus disease 2019) who developed multisystem inflammatory syndrome (MIS) 1 month after spontaneous resolution. A 23-year-old African American man was admitted with a 1-week history of worsening fatigue, myalgias, headache, and dyspnea. Nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was negative by polymerase chain reaction; however, the patient was febrile and had leukocytosis, elevated troponin I, transaminitis, and acute kidney injury. Bedside echocardiogram showed decreased left ventricular ejection fraction (40% to 45%) and global hypokinesis in the setting of a type II non-ST segment myocardial infarction. Despite being on broad spectrum antibiotic therapy, the patient’s clinical condition continued to worsen. The patient was then empirically treated for MIS with intravenous immunoglobulin and methylprednisolone, which led to a rapid resolution of fever and laboratory abnormalities. This case highlights that MIS associated with COVID-19 may present in patients above the age of 21 years and can occur with a delayed onset after mild illness in those with no previous oxygen requirement or hospitalization during SARS-CoV-2 infection.
Keywords: severe acute respiratory coronavirus 2, coronavirus 2019, multisystem inflammatory syndrome, obesity, youth
Background
At least 5.21 million cases of coronavirus disease 2019 (COVID-19) have been documented worldwide.1 Among youth, the proportion of cases has increased by more than 3-fold since February 2020.2 Though individuals aged between 0 and 24 years were originally believed to be largely removed from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) complications, recent data suggest the presence of multisystem inflammatory syndrome (MIS) among a subset of youth who contract the virus.3 We present this unique case to underscore the extensive subacute cardiovascular, renal, and hematologic involvement that can occur after SARS-CoV-2 infection, even after an asymptomatic to mild clinical course among those above 21 years of age. Our case illustrates a need to evolve current age criteria for MIS case definitions, and that mild COVID-19 illness in youth may have implications for future chronic disease prevention.
Case Report
A 23-year-old obese (body mass index = 35.4 kg/m2) African American man with a history of mild COVID-19 presented to the hospital with worsening dyspnea, fatigue, and myalgias over 1 week. One month prior to admission, he contracted COVID-19 and had a spontaneous recovery that did not require hospitalization or supplemental oxygen. His fatigue and myalgias had worsened over the week prior to his presentation and included difficulty sleeping at night due to orthopnea and paroxysmal nocturnal dyspnea. He also reported a fever, self-resolving watery diarrhea, and temporal headaches 3 to 5 days prior to admission. He denied chest pain, cough, and cigarette smoking.
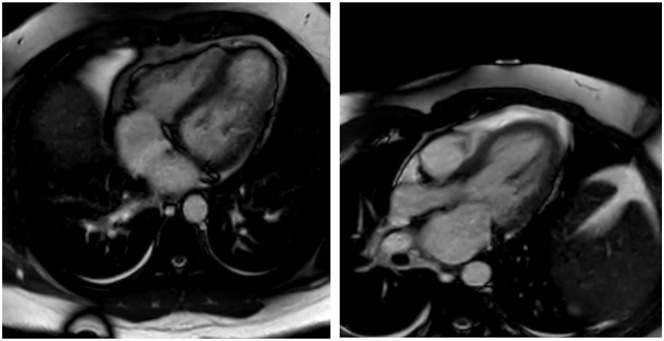
On presentation, the patient was febrile, tachycardic, tachypneic, hypotensive, and had an oxygen saturation of 96% (Table 1). Clinical examination showed a moderately fatigued young man speaking in full sentences. He was noted to have bilateral conjunctival and scleral injection. The oropharynx was clear, and there was no cervical lymphadenopathy. Heart sounds were distant with no obvious murmur, and there was trace lower extremity pitting edema bilaterally. Pulmonary auscultation revealed clear lungs and appropriate airway movement. The abdomen was soft and nontender with normal bowel sounds. Bedside echocardiogram showed decreased left ventricular ejection fraction (40% to 45%) and global hypokinesis. No focal consolidation was appreciated on chest X-ray (Figure 1). He was treated with intravenous fluids and empiric broad spectrum antibiotic therapy for potential sepsis after a negative SARS-CoV-2 nasopharyngeal swab in the emergency department.
Table 1.
Results on Initial Presentation.
| Markers | Concentrations |
|---|---|
| Vital signs | |
| Temperature, °F | 101.8 |
| Heart rate, beats per minute | 154 |
| Systolic/diastolic blood pressure, mm Hg | 97/62 |
| Respiratory rate, breaths per minute | 20 |
| Oxygen saturation, % | 96 |
| Hematologic | |
| White blood cells, per 103/µL | 12.8 |
| Lymphocytes, per 103/µL | 0.50 |
| Hemoglobin, mg/dL | 17.1 |
| Hematocrit, % | 49.0 |
| Platelet count, per 103/µL | 123 |
| Chemistry | |
| Sodium, mmol/L | 137 |
| Potassium, mmol/L | 4.1 |
| Chloride, mmol/L | 101 |
| CO2, mmol/L | 20 |
| Glucose, mg/dL | 122 |
| Calcium, mg/dL | 9.5 |
| Blood urea nitrogen, mg/dL | 18.0 |
| Creatinine, mg/dL | 1.61 |
| Total protein, g/dL | 7.6 |
| Albumin, g/dL | 4.1 |
| Aspartate aminotransferase, U/L | 62 |
| Alanine aminotransferase, U/L | 96 |
| Alkaline phosphatase, U/L | 154 |
| Total bilirubin, mg/dL | 1.7 |
| Inflammatory | |
| D-dimer, ng/mL | 588 |
| Fibrinogen, mg/dL | >700 |
| Ferritin, ng/mL | 1507.7 |
| C-reactive protein, mg/dL | 28.1 |
| Cardiovascular | |
| Troponin I, ng/mL | 0.53 |
| Brain natriuretic peptide, pg/mL | 262 |
| Total cholesterol, mg/dL | 107 |
| High-density lipoprotein cholesterol, mg/dL | 14 |
| Low-density lipoprotein cholesterol, mg/dL | 59 |
| Triglycerides, mg/dL | 171 |
Figure 1.
Chest x-ray on initial presentation.
Initial laboratory tests were notable for leukocytosis with lymphocytopenia, transaminitis, and acute kidney injury with an initial creatinine of 1.61 mg/dL (Table 1). Cardiac workup showed high brain-natriuretic peptide (262 pg/mL) and non-ST segment myocardial infarction with an elevated troponin I of 0.53 ng/mL that peaked on day 3 at 1.43 ng/mL. Inflammatory markers, including C-reactive protein, ferritin, D-dimer, and fibrinogen, were all also markedly elevated. Blood and urine cultures demonstrated no bacterial or fungal growth at 5 days. While the influenza A/B and mononucleosis screen were negative, SARS-CoV-2-specific IgG (immunoglobulin G) was reactive and indicative of a previous SAR-CoV-2 infection. Contrast computed tomography chest angiogram was unremarkable and did not show evidence of pulmonary embolism, acute airspace disease, or coronary artery aneurysm.
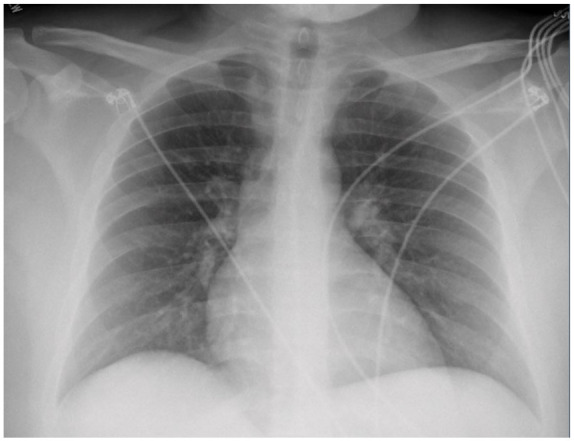
Atherosclerotic cardiovascular disease risk markers were overall notable for markedly reduced high-density lipoprotein cholesterol, hypertriglyceridemia, and obesity (Table 1). Nonischemic cardiomyopathy workup was unrevealing, including normal thyroid-stimulating hormone as well as negative hepatitis B and C, human immunodeficiency virus, anti-nuclear antibody panel, and serum-free light chains. On day 5, cardiac magnetic resonance imaging revealed a borderline normal ejection fraction (54%) and pericardial effusion (Figure 2).
Figure 2.
Key images from cardiac magnetic resonance imaging on day five.
The presence of tachycardia and hypotension in the setting of a fever on initial presentation in this patient prompted workup for sepsis and pulmonary embolism. The latter diagnoses were ruled out by negative microbial cultures and benign chest imaging. Reduced ejection fraction on bedside echo combined with elevated cardiac biomarkers were concerning for acute myocarditis or new-onset heart failure, necessitating evaluation of both ischemic and nonischemic cardiomyopathies. These investigations were largely unremarkable. Ultimately, the patient’s history of COVID-19 infection, persistent fever, lymphopenia, elevated inflammatory markers, and multiorgan involvement, were concerning for MIS.
On clinical recognition of MIS, the patient was taken off initial broad-spectrum antibiotic therapy and transitioned to a local MIS treatment protocol4 on day 3 of his hospitalization. He received a methylprednisolone bolus of 10 mg/kg followed by 2 mg/kg/day divided into 2 doses per day until he was afebrile for >48 hours. He also received 2 g/kg of intravenous immunoglobulin, aspirin 325 mg, and enoxaparin 60 mg daily. The patient’s dyspnea, fatigue, myalgias, and fever improved rapidly with completion of immune-modifying therapy. Multiorgan dysfunction also began to resolve with normalization of troponin I, liver enzymes, and creatinine. Similarly, inflammatory markers including C-reactive protein, D-dimer, and ferritin trended downward. The patient was discharged home on day 6 of hospitalization, with outpatient cardiology follow-up.
Discussion
Here, we show that mild COVID-19 cases may transform into MIS in the postinfectious period even among adults. Our findings, thus, challenge the notion that MIS is a COVID-19 complication limited to the pediatric population. Though the pathophysiology of MIS remains incompletely understood, the condition is thought to arise from a dysregulated immune response that closely resembles Kawasaki disease and cytokine release syndrome.3,5 This theory is supported by the fact that the majority of MIS cases present in the postinfectious period rather than during the acute infection itself. Feldstein and colleagues3 documented 186 cases of MIS that had a median time of 25 days between COVID-19 infection and development of MIS. Our patient presented with MIS 29 days after initial COVID-19 infection; however, he was several years older than the average age documented in this case series (23 vs 8.3). Overall, MIS appears to be an exceedingly rare complication in adults.
With regard to other laboratory markers, the patient’s lipid panel was significant for very low high-density lipoprotein-cholesterol and hypertriglyceridemia, laboratory values that have been documented,6 but somewhat overlooked in the setting of MIS in children and COVID-19.6,7 We speculate that the extent of lipid abnormalities may correlate with the severity of illness among youth who develop post-COVID-19 MIS. Furthermore, our findings also have implications for cardiovascular disease prevention, as obesity appears to be an important risk factor for the extensive cardiovascular involvement accompanying post-COVID-19 MIS, particularly in African American patients.8 The elevated troponin and BNP in the setting of reduced ejection fraction and pericardial effusion in our patient suggest that close cardiovascular follow-up is warranted among patients recovering from MIS.
Our case demonstrates that the current Centers for Disease Control and Prevention and World Health Organization age case definition criteria9 do not capture young adults who present with MIS. Regardless of age, clinicians should thus have a low threshold of initiating immune-modulating therapy in the setting of post-COVID-19 multiorgan injury. On a public health level, this case has broader implications for devising safe return to school protocols for college students in the United States.
Acknowledgments
The authors thank the staff of University Medical Center New Orleans for their courage, support, and dedication in helping to provide care for COVID-19 patients.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Alexander C. Razavi  https://orcid.org/0000-0002-3213-0876
https://orcid.org/0000-0002-3213-0876
References
- 1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Academy Academy of Pediatrics. Children and COVID-19: state-level data report. Accessed October 30, 2020 https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- 3. Feldstein LR, Rose EB, Horwitz SM, et al. ; Overcoming COVID-19 Investigators; CDC COVID-19 Response Team. Multisystem inflammatory syndrome in US children and adolescents. N Engl J Med. 2020;383:334-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shulman ST. Pediatric coronavirus disease-2019-associated multisystem inflammatory syndrome. J Pediatric Infect Dis Soc. 2020;9:285-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wei X, Zeng W, Su J, et al. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol. 2020;14:297-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferdinand KC. Understanding African American COVID-19 severity and mortality: is obesity the key? Obesity (Silver Spring). 2020;28:1793-1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bamrah SM, Belay E, Levin M, Schneider J, Marconi VC. Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). Published May 19, 2020. Accessed October 30, 2020 https://emergency.cdc.gov/coca/calls/2020/callinfo_051920.asp