Abstract
Background:
Increased passive deltoid tension after reverse total shoulder arthroplasty (RTSA) potentially leads to displacement or tilting of a preexisting os acromiale.
Purpose:
To analyze patients with an os acromiale who underwent RTSA and compare their outcomes and complications with a matched control group without an os acromiale.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
In this study, 45 shoulders in 42 patients with an os acromiale (cases) were matched to 133 patients without os acromiale (controls) who underwent RTSA between 2005 and 2016. The mean follow-up was 52 ± 32 months. Matching criteria included sex, type of surgery, duration of follow-up, and age. The Constant score (CS), Subjective Shoulder Value (SSV), and radiological outcomes were assessed postoperatively at 1-year, 2-year, and final follow-up visits.
Results:
The mean CS, SSV, and range of motion improved from preoperative levels to the final follow-up in both groups (P < .01). Patients with an os acromiale had a relative CS of 70 ± 23 versus 76 ± 21 points (P = .15) and an SSV of 70 ± 30 versus 73 ± 24 (P = .52) compared with controls at the final follow-up visit. Patients with an os acromiale had significantly decreased active flexion of 104° ± 33° versus 114° ± 33° (P = .03) at 1 year and active abduction of 103° ± 37° versus 121° ± 38° at 2 years postoperatively (P = .02). A postoperatively painful os acromiale was found in 12 cases (27%) and spontaneously resolved in 8 cases after a mean of 33 months (range, 12-47 months; P = .04).
Conclusion:
RTSA reliably restores patient satisfaction despite the presence of an os acromiale, with a slightly impaired range of motion. Postoperative local tenderness at the os acromiale can be expected in 1 out of 4 patients, but this resolves spontaneously over time in the majority of patients.
Keywords: RTSA, reverse total shoulder arthroplasty, os acromiale, shoulder, acromion
Lack of fusion between the acromial ossification centers results in an os acromiale.11,12 It is often an incidental radiological finding, but it has been associated with subacromial impingement and rotator cuff tears.13,14 The indications for reverse total shoulder arthroplasty (RTSA) are increasing, and this procedure yields good functional outcomes for otherwise irreparable chronic rotator cuff tears, primary osteoarthritis, and fractures, and as a salvage therapy after fractures of the proximal humerus or revision arthroplasty.5,6,9,10
Ossification of the acromion normally occurs between adolescence and early adulthood, and os acromiale is estimated to occur in up to 15% of the population.17 Of these, a significant number will develop a condition, such as an irreparable rotator cuff tear, that will make them likely candidates for RTSA in the future.1
RTSA leads to a medialization of the center of rotation and distalization of the humerus and therefore increases passive deltoid tension and its lever arm. While this reliably restores shoulder function because of an increase of deltoid muscle fiber recruitment for abduction and flexion, it simultaneously raises the strain on the acromion and the scapular spine.2 This potentially leads to displacement or tilting of a preexisting os acromiale with associated pain. However, the effect of an os acromiale on postoperative outcome after RTSA has been reported infrequently.1
The aim of this study was to analyze patients with an os acromiale who underwent RTSA and compare their outcomes and complications with a matched control group without an os acromiale. We hypothesized that the presence of an os acromiale would be associated with reduced shoulder function and lower patient satisfaction.
Methods
Patients
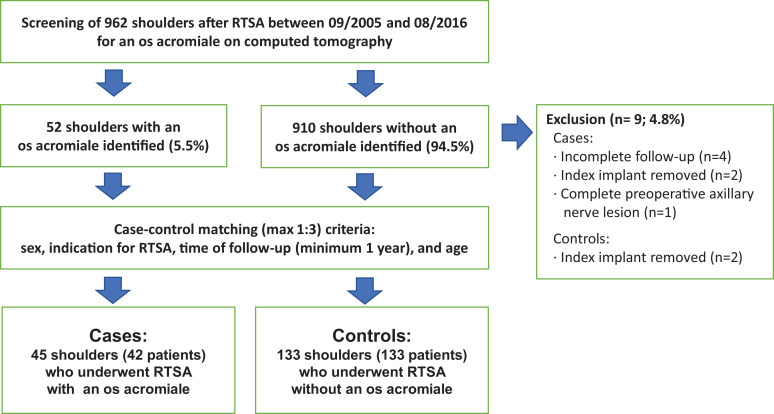
The research protocol was approved by the regional ethics committee, and written informed consent was obtained from all patients. All patients treated with an RTSA at our institute between September 2005 and August 2016 (N = 962) were screened for the presence of an os acromiale by reviewing their preoperative computed tomography images and patient charts. An os acromiale occurred in 52 shoulders (5.4%). In total, 9 patients (4.8%) had to be excluded from analysis. One of these patients declined follow-up after 4 months while living in a nursing home, and 3 patients had incomplete functional or radiological follow-up. One patient had a complete traumatic axillary nerve lesion before undergoing RTSA with persistent deltoid paralysis (n = 1), and in 4 patients the index implant had to be removed because of either periprosthetic joint infection (n = 3) or conversion to a hemiprosthesis owing to massive glenoid destruction (n = 1) (Figure 1).
Figure 1.
Flowchart and eligibility. RTSA, reverse total shoulder arthroplasty.
After exertion of the exclusion criteria, 45 shoulders in 42 patients with an os acromiale (cases) were matched to 133 shoulders in 133 patients who underwent RTSA during the same period without an os acromiale (controls). The matching criteria included sex, type of surgery, and, in decreasing order of importance, minimum deviation in time of follow-up and age (Figure 1).
Surgical Technique
All procedures were performed through a deltopectoral approach using the Zimmer Reverse Anatomical Shoulder System. The subscapularis muscle was mobilized, detached, and grasped with No. 2 FiberWire (Arthrex) sutures and transosseously reconstructed at the end of the procedure, if possible. The long head of the biceps was tenotomized at the level of the bicipital groove, if present. The humeral head was then resected and the glenoid was reamed. In cases of an os acromiale, we avoided placing a retractor on the acromion. The glenoid baseplate was positioned flush with the inferior border of the native glenoid in neutral version and angulation. Glenoid defects or severe dysplastic glenoids were augmented with humeral head autograft using a long peg baseplate, avoiding extensive lateralization. We did not, however, perform grafting in nondeficient native glenoids.
An additional latissimus dorsi transfer was conducted if a pseudoparalysis for combined abduction and external rotation was present.7 Postoperative care included use of a sling for a maximum of 6 weeks. Passive external and internal rotation and active-assisted elevation exercises were started immediately postoperatively with the help of a physical therapist.
Clinical and Radiological Assessment
The Constant score (CS),3 Subjective Shoulder Value (SSV; reported as a percentage),8 pain (assessed based on CS: 0 points for the most severe to 15 points for no pain), and range of motion were used to assess outcomes at 1 and 2 years postoperatively as well as at the final follow-up. The charts were reviewed for reports of local tenderness over the os acromiale. Additionally, complications and revision surgeries were analyzed.
Radiographic assessment included the type of os acromiale14 and scapular notching according to Sirveaux et al15 occurring at the final follow-up visit. Postoperative displacement was defined if a displacement >2 mm or tilting >5° was observed in the anteroposterior view of the radiograph. Postoperative tilting was assessed as described by Aibinder et al.1
Statistical Analysis
Differences between groups regarding patient characteristics and postoperative complications were assessed using the Student t test for normally distributed data. Categorical data were compared using the chi-square test and Fisher exact test. A mixed linear model including postoperative follow-up at 1 and 2 years and a final follow-up was used to test for an effect between the groups (cases vs controls), as well as an effect over time of each outcome variable. Additionally, outcome variables were compared at each time point using t tests. Subgroup analysis between the type of os acromiale and displaced and nondisplaced os acromiales was performed using t tests at each time point. P values were Bonferroni-corrected for multiple tests.
To assess the isolated impairment originating from an os acromiale, a subgroup analysis of patients without any postoperative complication or revision surgery was performed analog to the above-mentioned proceeding (mixed linear model for effect of group and t tests at each time point). All statistical analyses were performed using Stata (release 14; StataCorp LP).
Results
Patients
A total of 45 shoulders with an os acromiale (cases) and 133 shoulders without an os acromiale (controls) were available after a mean follow-up of 52 months (range, 12-121 months) (with data from 45 cases and 133 controls available at 1 year, and 30 cases and 109 controls at 2 years as well as final follow-up). No significant differences in patient characteristics, indications for RTSA, additional surgical procedures, or postoperative notching were found between the groups except for a significant difference in follow-up time of 44 months (range, 12-120 months) for the cases versus 55 months (range, 12-121 months) for the controls (P < .01) (Table 1). The type of os acromiale included 14 preacromions (31.1%), 30 mesoacromions (66.7%), and 1 meta-acromion (2.2%). Patients with a mesoacromion had significantly worse pain levels of 11 ± 4 points versus 14 ± 1 points 2 years postoperatively compared with patients with a pre-acromion (P = .04). The remaining outcome measures yielded no significant differences among the different types of os acromiale at any time point.
Table 1.
Patient Characteristics, Indication for RTSA, and Additional Surgical Proceduresa
| Cases (n = 45) |
Controls (n = 133) | P Value | |
|---|---|---|---|
| Mean follow-up, mo (range) | 44 (12-120) | 55 (12-121) | <.01 b |
| Radiographic notching
grade 0 1 2 3 4 |
14 (31) 12 (27) 4 (9) 5 (11) 10 (22) |
35 (26) 63 (47) 10 (8) 16 (12) 9 (7) |
.07c |
| Mean age at RTSA, y, ±SD | 74 ± 9 | 72 ± 8 | .16b |
| Additional procedures Tendon transfer Greater tuberosity refixation |
6 (13) 1 (2) |
15 (8) 8 (6) |
.44c |
| Indication for RTSA Primary RTSA for irreparable RCT or osteoarthritis Previous rotator cuff surgery Fracture Conversion from anatomical prosthesis Conversion from hemiprosthesis |
27 (60) 11 (24.5) 1 (2) 3 (7) 3 (7) |
80 (60) 37 (28) 3 (2) 7 (5) 6 (5) |
.96c |
| Sex | .98c | ||
| Male Female |
17 (38) 28 (62) |
51 (38) 82 (62) |
aValues are listed as number (percentage) unless otherwise indicated. Boldface type indicates statistical significance. RCT, rotator cuff tear; RTSA, reverse total shoulder arthroplasty.
b Student t test.
c Chi-square test.
Clinical and Radiological Assessment
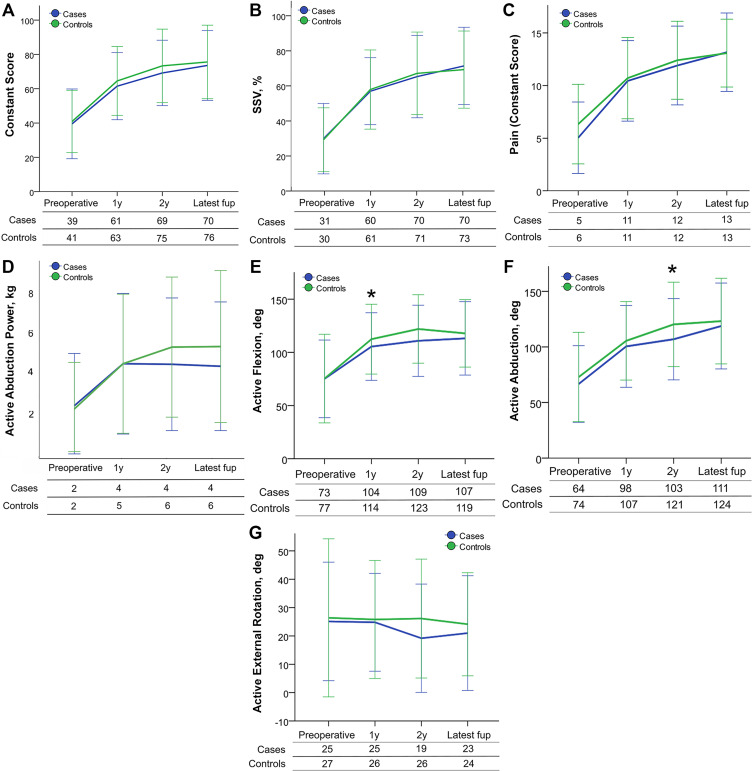
Overall, all mean outcome measures, except active external rotation, improved between the preoperative period and the final follow-up: relative CS from 40 ± 19 to 74 ± 21 (P < .01), SSV from 30% ± 20% to 72% ± 25% (P < .01), pain from 6 ± 4 to 13 ± 3 (P < .01), active flexion from 76° ± 40° to 116° ± 39° (P < .01), and active abduction from 71° ± 39° to 121° ± 39° (P < .01) (Figure 2, C and D).
Figure 2.
Mean relative outcome measures over time. At the 1-year follow-up: 45 cases, 133 controls; at the 2-year and final follow-ups (fup): 30 cases, 109 controls. Only significant P values (t tests) at each time point after Bonferroni correction are depicted (asterisks). (A) Constant score. Mixed linear model between groups (P = .17) and over time (P < .01). (B) Subjective Shoulder Value (SSV). Mixed linear model between groups (P = .99) and over time (P < .01). (C) Pain assessed using Constant score: 0 = most severe,15 = no pain. Mixed linear model between groups (P = .15) and over time (P < .01). (D) Active abduction power. Mixed linear model between groups (P = .19) and over time (P < .01). (E) Active flexion. Mixed linear model between groups (P = .08) and over time (P < .01); *P = .03. (F) Active abduction. Mixed linear model between groups (P = .04) and over time (P < .01); *P = .02. (G) Active external rotation. Mixed linear model between groups (P = .13) and over time (P = .55).
Some outcome measures for patients with an os acromiale were not significantly different from those of controls: relative CS of 70 ± 23 versus 76 ± 21 points (P = .15) and SSV of 70% ± 30% versus 73% ± 24% (P = .52) at the final follow-up, respectively (see Figure 2, A and B).
Postoperative abduction yielded a significant difference in the mixed linear model between groups (P = .04). Analysis at each time point revealed a significantly decreased active flexion for the patients with os acromiale compared with the controls of 104° ± 33° versus 114° ± 33° (P = .03) 1 year postoperatively and active abduction of 103° ± 37° versus 121° ± 38° (P = .02) 2 years postoperatively, respectively (Figure 2, E and F). Abduction strength was also slightly worse in patients with an os acromiale, but this was not significant at any time point. The remaining outcome measures yielded no significant differences between the groups at any time point (Figure 2).
A postoperative displacement or tilting of the os acromiale occurred in 27 patients, including 8 preacromions (29.6%) and 19 mesoacromions (70.4%). No significant differences of the analyzed outcome measures between displaced and nondisplaced os acromiales were found.
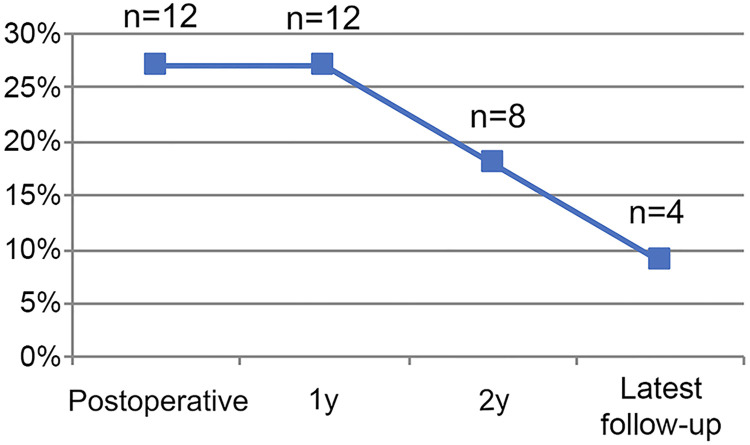
Localized tenderness over the os acromiale was present in 1 patient (2.2%) preoperatively and in 12 (27%) postoperatively. The pain resolved in 8 of these patients after a mean interval of 33 months (range, 12-47 months) after surgery (Figure 3). The only patient with a previously symptomatic os acromiale underwent open reduction and plate fixation for a painful, mobile meta-acromion, 2 years before undergoing RTSA. The fixed os acromiale consolidated uneventfully and remained asymptomatic after RTSA.
Figure 3.
Painful os acromiale over time. Significantly decreased over time, (n = 12; 26.7%) in the immediate postoperative period to (n = 4; 8.9%) after a mean of 33 months (range, 12-71 months) (P = .04).
Patients with a symptomatic os acromiale postoperatively (n = 12) versus those without local tenderness at the os acromiale (n = 33) had a significantly decreased active abduction 2 years postoperatively (P = .04). CS, SSV, active flexion, and abduction power were decreased in patients with a symptomatic os acromiale but yielded no significance between groups at any time point.
Postoperative Complications and Revision Surgery
In addition to the aforementioned excluded patients, another 5 patients with os acromiale had postoperative complications and 3 needed a subsequent revision surgery after a mean of 26 months (range, 17-39 months). In total, 13 of the controls had postoperative complications and 10 (P = .8) of these control patients needed revision surgery after a mean of 27 months (range, 11-56 months). The overall complications (P = .8) and revision surgery (P > .99) did not differ significantly between the groups.
Postoperative complications included (from most to least severe, cases vs controls) aseptic loosening, 2 (4.4%) versus 6 (4.5%) (P > .99); scapular spine fractures, 2 (4.4%) versus 4 (3%) (P > .99); acromial fractures, 0 (0%) versus 1 (0.8%) (P > .99); unclear pain after RTSA after exclusion of aseptic or septic loosening, 0 (0%) versus 2 (1.6%) (P > .99); and postoperative incomplete plexus palsy after locoregional anesthesia with complete sensomotoric remission, 0 (0%) versus 1 (0.8%) (P > .99). A 71-year-old woman with an acromial insufficiency fracture from the control group was treated nonoperatively with abduction bracing for 12 weeks. Despite a moderate fracture displacement and only partial fracture consolidation in computed tomography, she reported high satisfaction, a relative CS of 86 points, and an SSV of 60% 4 years postoperatively.
Subgroup analysis of the patients without postoperative complications or revision surgery (cases: n = 40; controls: n = 120) confirmed the findings of slightly decreased CS, SSV, active flexion, active abduction, and abduction power between groups, but yielded no significance.
Discussion
Our study demonstrated that RSTA in patients with a preexisting os acromiale reliably restores patient satisfaction with only slightly impaired range of motion (active flexion and active abduction) compared with a control group without os acromiale. Postoperative local tenderness at the os acromiale can be expected in 1 out of 4 patients but resolves spontaneously over time in the majority of patients. The presence of an os acromiale did not increase postoperative complications or the need for revision surgery.
These findings support the decision making when considering RTSA for patients with os acromiale. The surgical technique and postoperative rehabilitation were independent of the presence or absence of an os acromiale, with the exception of avoiding placement of a retractor on the acromion in cases of an os acromiale.
The characteristic design of the reverse prosthesis, which increases the lever arm, distalizes the humerus, and increases muscle fiber recruitment of the deltoid, results in increased load on the acromion. A postoperative displacement of the os acromiale is observed in 50% of the cases and more often in mesoacromion. This is in accordance with previous studies that described a tilting or displacement of the os acromiale after RTSA.1 Similarly, a dislocation of scapular spine fractures after RTSA has been attributed to increased deltoid tension.16 From a biomechanical standpoint, it seems logical that a preexisting os acromiale might be adversely affected by increased deltoid strain. The size of the os acromiale and therefore the size of the deltoid origin affected appears to be a relevant factor for postoperative pain, which was significantly higher for patients with a meso-acromion compared with a preacromion 2 years postoperatively. The only surgical fixation of a symptomatic mobile os acromiale was necessary in a patient with a meta-acromion before undergoing RTSA.
Both a biomechanically adversely affected deltoid origin and a painful displacement of the os acromiale may explain the decreased active flexion, abduction, and abduction power after RTSA. However, it remains to be further analyzed to what extent these limitations are a result of a passive restriction of range of motion, a decrease of active muscle contraction due to pain, or a shortened muscle length.
A painful os acromiale after RTSA occurred in 1 out of 4 patients but resolved in the majority over time without interventions. A postoperative painful os acromiale was associated with a significantly decreased active abduction and showed a trend for decreased shoulder function compared with the patients without local tenderness at the os acromiale. However, none of the patients in our cohort underwent revision surgery because of a symptomatic os acromiale. Several treatment options for a symptomatic os acromiale exist, including local injections, open or arthroscopic fragment excision, and internal fixation with or without acromioplasty.4,11 This has also been described after RTSA, but rarely seems to be necessary.1
The proposed sequelae of an os acromiale, including hypothetic subacromial impingement and subsequent cuff tearing, lead to a group of patients who will be considered for RTSA. This group of patients has only been studied scarcely and comprised 5.4% of the patients who underwent RTSA in this cohort.1,13
The limitations of our study include factors that are inherent to its retrospective design. Potential selection bias might be present because of loss to follow-up, different follow-up periods, and varying postoperative complications and revision surgeries. An exclusion rate of 4.8% seems fairly low. The exclusion of patients after removal of the index implant seems negligible, as an impaired function can be expected with or without an os acromiale present in these cases. Potential selection bias might be present as a result of different follow-up periods. However, the range of follow-up was similar in both groups and shoulder function has been reported to be constant up to 15 years.6 Furthermore, the incidence and type of postoperative complications were nearly the same in both groups. The study population included various indications for RTSA and may include an undesired heterogeneity in outcomes, although appropriate matching (including matching for indications and type of additional intervention) between the groups was achieved. To our knowledge, this is the first study to provide a matched control analysis for patients with an os acromiale after RTSA, and therefore it provides level 3 evidence. Still, this study only reports medium-term follow-up and does not allow an extrapolation for long-term function after RTSA in patients with an os acromiale. Nonetheless, as postoperative impairment appears to be temporary and decreasing over time, the main focus of analysis is in the first postoperative year. Local tenderness over the os acromiale could not be assessed with a standardized clinical test and therefore may be underreported.
Conclusion
RTSA reliably restores patient satisfaction despite the presence of an os acromiale, with only slightly impaired active flexion and active abduction. Postoperative local tenderness at the os acromiale can be expected in 1 out of 4 patients but resolves spontaneously over time in the majority of patients.
Acknowledgment
The authors acknowledge Professor Emeritus Christian Gerber and research nurses Sabrina Catanzaro and Sabine Wyss. In memoriam of Dominik Christoph Meyer, Professor of Orthopedics.
Footnotes
Final revision submitted May 12, 2020; accepted June 11, 2020. G.C. and S.H. contributed equally to this article.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the regional ethics committee of Zürich Canton (ref. No. 2017-01648).
References
- 1. Aibinder WR, Schoch BS, Cofield RH, Sperling JW, Sanchez-Sotelo J. Reverse shoulder arthroplasty in patients with os acromiale. J Shoulder Elbow Surg. 2017;26(9):1598–1602. [DOI] [PubMed] [Google Scholar]
- 2. Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–540. [DOI] [PubMed] [Google Scholar]
- 3. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 4. Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br. 1993;75(4):551–555. [DOI] [PubMed] [Google Scholar]
- 5. Ernstbrunner L, Suter A, Catanzaro S, Rahm S, Gerber C. Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am. 2017;99(20):1721–1729. [DOI] [PubMed] [Google Scholar]
- 6. Gerber C, Canonica S, Catanzaro S, Ernstbrunner L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg. 2018;27(5):831–838. [DOI] [PubMed] [Google Scholar]
- 7. Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am. 2006;88(1):113–120. [DOI] [PubMed] [Google Scholar]
- 8. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717–721. [DOI] [PubMed] [Google Scholar]
- 9. Grubhofer F, Wieser K, Meyer DC, et al. Reverse total shoulder arthroplasty for acute head-splitting, 3- and 4-part fractures of the proximal humerus in the elderly. J Shoulder Elbow Surg. 2016;25(10):1690–1698. [DOI] [PubMed] [Google Scholar]
- 10. Grubhofer F, Wieser K, Meyer DC, Catanzaro S, Schurholz K, Gerber C. Reverse total shoulder arthroplasty for failed open reduction and internal fixation of fractures of the proximal humerus. J Shoulder Elbow Surg. 2017;26(1):92–100. [DOI] [PubMed] [Google Scholar]
- 11. Hertel R, Windisch W, Schuster A, Ballmer FT. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg. 1998;7(6):606–609. [DOI] [PubMed] [Google Scholar]
- 12. Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg. 2006;14(1):12–19. [DOI] [PubMed] [Google Scholar]
- 13. Mudge MK, Wood VE, Frykman GK. Rotator cuff tears associated with os acromiale. J Bone Joint Surg Am. 1984;66(3):427–429. [PubMed] [Google Scholar]
- 14. Sammarco VJ. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am. 2000;82(3):394–400. [DOI] [PubMed] [Google Scholar]
- 15. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. J Bone Joint Surg Br. 2004;86(3):388–395. [DOI] [PubMed] [Google Scholar]
- 16. Walch G, Mottier F, Wall B, Boileau P, Mole D, Favard L. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg. 2009;18(3):495–502. [DOI] [PubMed] [Google Scholar]
- 17. Yammine K. The prevalence of os acromiale: a systematic review and meta-analysis. Clin Anat. 2014;27(4):610–621. [DOI] [PubMed] [Google Scholar]