Abstract
Positive patient experiences are associated with illness recovery and adherence to medication. To evaluate the virtual care experience for patients with COVID-19 symptoms as their chief complaints. We conducted a cross-sectional study of the first cohort of patients with COVID-19 symptoms in a virtual clinic. The main end points of this study were visit volume, wait times, visit duration, patient diagnosis, prescriptions received, and satisfaction. Of the 1139 total virtual visits, 212 (24.6%) patients had COVID-19 symptoms. The average wait time (SD) for all visits was 75.5 (121.6) minutes. The average visit duration for visits was 10.5 (4.9) minutes. The highest volume of virtual visits was on Saturdays (39), and the lowest volume was on Friday (19). Patients experienced shorter wait times (SD) on the weekdays 67.1 (106.8) minutes compared to 90.3 (142.6) minutes on the weekends. The most common diagnoses for patients with COVID-19 symptoms were upper respiratory infection. Patient wait times for a telehealth visit varied depending on the time and day of appointment. Long wait times were a major drawback in the patient experience. Based on patient-reported experience, we proposed a list of general, provider, and patient telehealth best practices.
Keywords: telehealth, virtual visits, patient experience, recommendations
Introduction
Positive patient experiences are associated with illness recovery and adherence to medication (1). On the contrary, suboptimum patient experiences have important implications on patients’ health conditions and on health care costs as patients would require more health care services (2,3). Traditionally, patient experience is defined as patient-reported encounters and events that occur across the continuum of care (4). In the virtual world, patient experience may be defined differently.
Amid the COVID-19 pandemic, virtual care, which is the remote exchange of health information between a patient and provider (5), has become the new norm, temporarily replacing many outpatient services for health care delivery. Virtual visits include telephone and video calls. Social determinants, defined as the conditions with which people are born, grow, live, and work, may play a role in the choice of communication preferred by the patient (6). Young and male patients have a higher chance of choosing a video call over telephone call compared to old or female patients (6).
Differences in workflow between virtual care and in-office visits can impact patient experience. Workflow is a sequence of tasks performed by different professionals or entities within the system (7). In virtual care, patients do not interact with or rely on other professionals to complete certain tasks. For example, virtual care patients are expected to independently complete the patient registration and to request an on-demand appointment without the need to interact with others. Additionally, patients can choose between telephone and video visit, which required the patient to assess their readiness for a video visit. In the hospital setting, patients are assisted to check-in upon arrival at the clinic by trained professionals, and if required, patients are scheduled for follow-up visit based on the availability of appointments. Therefore, the workflow processes are different in both environments.
Observational studies have characterized patient experiences and studied the relationship between patient experiences and satisfaction within the traditional, in-person visits (8 -10). However, there is limited knowledge describing the patient experience within a virtual care setting especially during a pandemic. The shift toward virtual visits creates a need to understand the opportunities and challenges in providing a patient experience that is at least as positive as in-person visits. In this study, we evaluated the virtual experience for patients with COVID-19 symptoms.
Objective
The goal of this study was to evaluate the virtual care experience of patients of all ages with COVID-19 symptoms as their chief complaints.
Methods
We conducted a cross-sectional study of the first cohort of patients with COVID-19 symptoms in a virtual clinic in a Southeastern medical center where the epidemiological curve has been increasing over time (11). The virtual clinic is an on-demand service, running for 24 hours per day and 7 days per week, that has been in operations since its initiation in 2018 by a major Southeastern health care system (12). Prior to the COVID-19 pandemic, the virtual clinic was in operation for nonemergency symptoms, functioning in the same manner as during the pandemic, and the in-person equivalent of the clinic would be any in-person Urgent Care center. The clinic has provided care to over 8000 patients through board-certified physicians.
Virtual Workflow
The service is open to any patient, regardless of geographic location or healthcare system plan. For patients less than 18 years of age, a parent or guardian is required to accompany them during the virtual visit. In order for individuals to request an appointment with a provider, they are required to register through the online portal. The online portal is available to any individual, regardless of their location of health care system affiliation. The online portal is not currently linked to the institutional electronic health record, although efforts to link both platforms are in progress.
Prior to starting a visit, a patient must create an account and complete their medical history. To ensure continuity of care, if a patient is within the associated health care system, all telemedicine visits will be visible in the patient’s electronic medical record. During registration, patients provide demographic information, insurance information, chief complaints, and the pharmacy of choice. Patients have the option to choose from a list of available board-certified physicians who are specialized in the subspecialty related to their chief complaints; otherwise, a random assignment is made based on availability. Physicians were on call for this specific clinic and not assigned to other services.
Once registration is complete and an appointment is requested, patients are either placed in a virtual waiting room or on hold, depending on whether they are registering through the online portal or through a phone call that is operated by a professional staff member. Patients using the phone can hang up and receive a callback.
We extracted the wait time in minutes, which is defined as the time between when an appointment was requested and the start time of the virtual visit. We labeled each appointment as “Completed” if a virtual call was successfully established between the provider and the patient, “Canceled” if the patient requested to cancel an existing appointment, “Missed” if the patient was not present to join the call, and “Patient left wait room” if the patient successfully checked in to the virtual waiting room and then exited the waiting room and did not join the call. Since this is an on-demand service, there is no dedicated slots per hour or per day except if the patient tried to schedule an appointment with a physician who was already booked. In that case, the patient is offered alternative time options for the same physicians or alternative options to other physicians.
During the virtual visit, the patient directly communicated with the physician either via a telephone or video call based on the patient’s choice at registration. The clinic did not use a triage mechanism or scoring system to route patients. During the virtual visit, we recorded the duration of the visit from start to end time. Post visit, we asked patients to rate their interaction with their provider and overall visit on a 5-point, displayed in Table 1. Patients could also provide comments on their visits. Patients were also asked where they would alternatively gone to seek care. Participation was voluntary.
Table 1.
Patient Satisfaction Scale.
| Patient satisfaction | Point scale |
|---|---|
| Excellent | 5 |
| Very good | 4 |
| Good | 3 |
| Fair | 2 |
| Poor | 1 |
Data Collection
We collected data on all virtual visits between March 10, 2020, and April 19, 2020. We stratified COVID-19 data using the chief complaints entered by patients. We included COVID-19 symptoms (fever, cough, shortness of breath) coupled with the recently added “COVID-19 Concern” chief complaint. The term “COVID-19 Concern” was added to the list of existing chief complaints that is presented to patients during the registration process on March 20, 2020. Because this was a secondary analysis of data, patient consent was not obtained for this study; however, institutional review board approval was obtained prior to this study.
Outcomes
Primary outcomes were visit volume, wait times, visit duration, and patient satisfaction. Secondary outcomes were patient diagnosis, and prescriptions received.
Data analysis
We examined the patient experience of individuals with COVID-19 related symptoms by assessing their Virtual Urgent Care visit. Visits were filtered by patient state of residence, and only patients residing in North Carolina were included. Visits where the chief complaint was “COVID-19 Symptoms” were selected for analysis. We conducted descriptive analysis of the patient experiences as well as qualitative analysis of patient satisfaction survey. All statistical analysis was conducted with Python, a general purpose programming language that is comparable to R. The library pandas was used in Python.
To assess patient outcomes, diagnoses for patients with COVID-19 symptoms were first analyzed and grouped based on International Classification of Diseases-10-Clinical Modification codes, and visits with prescriptions were analyzed to examine which prescriptions were given. A demographic analysis was conducted to analyze patient virtual visits. Age groups were defined as: less than 18, 18 to 34, 35 to 49, 50 to 64, and 65 years or older. Patient visits were also grouped by medium (phone/video) and insurance status (insured/uninsured). Subsequent quantitative and qualitative analyses were conducted to understand the patient experience.
Patient wait times were analyzed in hourly groups. Encounter duration grouped in minutes were examined in tandem with wait times. Whether a patient was a new patient or returning patient was also assess to understand the reason for a return visit. Patient surveys were analyzed to understand patient satisfaction, and information on where patients would have gone alternatively to seek care were analyzed. For patient satisfaction, the 5-point scales were assessed quantitatively, and a qualitative analysis of patient comments was done. Patient responses for where they would have gone were organized into 4 categories: urgent care, delay seeking care, primary care physician, and emergency room.
Results
Of the 1139 total virtual visits, 212 (24.6%) patients had COVID-19 symptoms such that 125 (59%) patients marked “COVID-19 Concern” as their chief complaint, and 87 (41%) patients had COVID-19 chief complaints. There were 128 (60.4%) female patients, the average age (SD) of patients was 34.6 (15.7) years, 189 (89.2%) patients were seeking care for themselves, and 23 (10.9%) visits were for a dependent (Table 2). Of COVID-19-related patients, 161 (80%) were between 18 and 49 years of age, and 9 (4.3%) patients in the vulnerable age-group of over 65 years.
Table 2.
Characteristics of Virtual Care Patients With COVID-19 Concerns.
| Telehealth Visit Variable | Visits (%) |
|---|---|
| COVID-19 symptoms | 212 |
| “COVID-19 concern” chief complaint | 125 (59%) |
| COVID-19 chief complaint | 87 (41%) |
| Gender | |
| Male | 84 (39.6%) |
| Female | 128 (60.4%) |
| Age | |
| 0-10 years | 2 (1%) |
| 11-18 years | 15 (7%) |
| 19-99 years | 195 (92%) |
| Seeking care | |
| Primary | 189 (89.2%) |
| Dependent | 23 (10.9%) |
Telehealth Modality
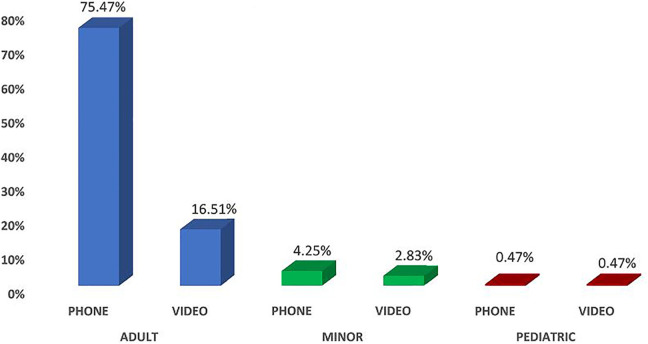
Of 212 patients, 195 (92%) were adults (>18 years), 15 (7%) were minors (<18 years), and 2 (1%) were pediatrics (<10 years). Among adult patients, there was substantial preference toward telephone visits such that 160 (75.5%) of patients preferred telephone visit compared to 35 (16.5%) video visit (Figure 1). In patients under 18 years of age, there was a slight preference for telephone visit such that 9 (60%) patients preferred telephone visit compared to 6 (40%) patients choosing video visit. For pediatric patients, there was an even split of a single (50%) telephone visits and 1 (50%) video visit.
Figure 1.
Patient with COVID-19-related concerns’ choice of communication medium for virtual visit.
Of the COVID-19-related visits, 184 (86.7%) patients were new patients, and 28 (13.2%) were returning patients. Of the new patients, 79 (43%) patients provided medical history information, while for current patients, 11 (39.2%) patients provided medical history information.
Of the 212 scheduled COVID-19 Concern virtual visits, 184 (86.7%) were completed visits, 24 (11.3%) visits were missed because the patient did not answer the clinics call(s), 2 visits were canceled by the patient prior to the visit, and 1 patient left the virtual waiting room.
Call volume, wait times, and duration
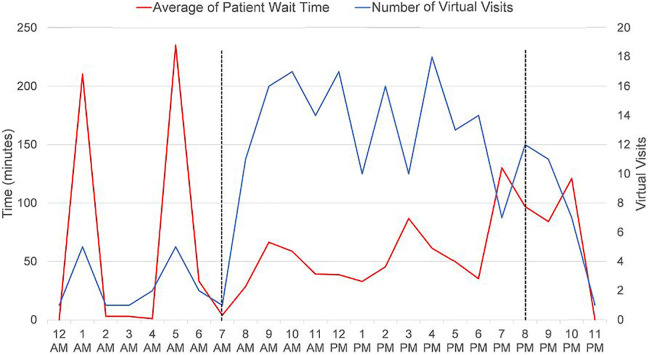
The volume of virtual visits fluctuated across 24 hours. Across all visits, most visits occurred between 7 am and 8 pm with a surge of 18 visits at 4 pm. Between 9 pm and 3 am, patient’s demand for virtual appointment declined, and the lowest number of visits occurred at between 11 pm and 1 am with only 1 visit (Figure 2). Although the number of visits were much higher between 7 am and 8 pm, the wait times were considerably lower than other times with fewer visits.
Figure 2.
Volume of virtual visits and average patient wait times over 24 hours.
The average wait time (SD) for all visits was 75.5 (121.6) minutes. Patients experienced varying wait times based on the time of their appointment. Patients with appointments between 7 pm and 10 pm and 1 am and 5 am experienced the highest wait times with an average of 111.6 minutes and 222.5 minutes, respectively. Patients with appointments between 2 am and 4 am had the shortest average wait time of 1.5 minutes (Figure 2).
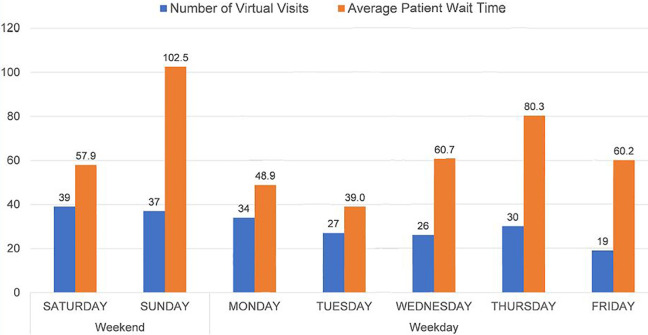
Weekdays vs weekends
The demand from patients for virtual visits varied during the week. The highest volume of virtual visits was on Saturdays (39), and the lowest volume was on Friday (19). Patients experienced shorter wait times (SD) on the weekdays 67.1 (106.8) minutes compared to 90.3 (142.6) minutes on the weekends. The highest average wait times were on Sundays (102.5), and the lowest average wait times were on Tuesday (39; Figure 3).
Figure 3.
Count of virtual visits and average patient wait times by day of the week.
The average visit duration for visits was 10.5 (4.9) minutes. Patients calling on the weekdays experienced a slightly longer visit duration (SD) of 11 (5.2) minutes compared to 9.6 (4.1) minutes on the weekend (Figure 3).
Medical diagnoses and referrals
The most common diagnoses for patients with COVID-19 symptoms were upper respiratory infection (URI) 35 (18.8%), exposure to communicable disease 18 (9.7%), bronchitis 16 (8.6%), cough 14 (7.5%), and viral infection 9 (4.8%; Table 3).
Table 3.
Top 10 Diagnosis of Telehealth Patients With COVID-19 Symptoms.
| Diagnosis | # of Patients (%) | Patients Prescribed Medication (%) |
|---|---|---|
| Upper respiratory infection | 35 (18.8%) | 21 (25.3%) |
| Exposure to communicable diseases | 27 (12.7%) | 7 (8.4%) |
| Bronchitis | 16 (8.6%) | 6 (7.2%) |
| Cough | 14 (7.5%) | 7 (8.4%) |
| Asthma | 8 (4.3%) | 6 (7.2%) |
| Allergic rhinitis | 7 (3.8%) | 3 (3.6%) |
| Influenza | 7 (3.8%) | 2 (2.4%) |
| Sinusitis—acute (sinus infection) | 6 (3.2%) | 6 (7.2%) |
| Shortness of breath | 5 (2.7%) | 3 (3.6%) |
| Other | 87 (41%) | 22 (26.5%) |
| Total | 212 (100%) | 83 (100%) |
Overall, 83 (39.2%) patients received prescription. Of which, 48 (57.8%) patients received 1 prescription medication, and 35 (42.2%) patients received 2 or more prescription medication. Patients diagnosed with URI (25.3%), exposure to communicable diseases (8.4%) and cough, were the highest recipients of prescript medication.
Patients with the same diagnosis experienced different medication prescription outcomes. The range of prescription medication to the eight patients diagnosed with Asthma was 1 to 7 medications per visit. Similarly, the range of prescription for the 16 patients diagnosed with Bronchitis was 0 to 3 per visit.
Patient satisfaction
Overall, 93 (7.8%) patients completed the virtual visit satisfaction survey. Of which, 15 (7.1%) patients were COVID-19 related. Of 15 patients who participated in the satisfaction survey, 7 (46.7%) patients rated their provider as “Excellent”, 2 (13.3%) as “Very Good,” 1 (6.7%) as “Good,” 1 (6.7%) as “Fair,” and 1 (13.3%) as “Poor.” While 9 (60%) patients rated their virtual provider as “Excellent,” 2 (13.3%) as “Good,” 2 (13.3%) as “Fair,” and 1 (6.7%) as “Poor.”
Among the reasons for a positive patient experience were comments related to the convenience of remote consultation without human contact, convenience of out of hour appointments, and avoiding emergency department visit. Factors that lead to a negative experience included long wait time, lack of interpersonal communication, poor telehealth equipment setup, and lack of clarity around ordering COVID-19 testing (Table 4).
Table 4.
Patient Overall Experiences and Physician Experiences Rating and Sample Patient Comments.
| Overall Experience | Physician Experience | Patient Comments |
|---|---|---|
| Excellent | Excellent | “I was able to get a doctor…Get medicine for my bronchitis…Even though my doctors office had no available appointments and not have to go to ER.” (Female, 65) |
| Excellent | Excellent | “Fast, excellent service. Short wait time for call. Live in rural area and walk-in clinics usually have 5-6 hour wait times.” (Female, 32) |
| Excellent | Excellent | “My physicians office was closed and I needed a medical consult without having to leave the house. I did not want to risk exposure to COVID-19.” (Female, 69) |
| Good | Good | “The physician I think appropriately treated my compliant, however I could not make eye contact and only saw the top of his forehead and the ceiling.” (Female, 58) |
| Good | Fair | “Still have to go to another doctor for medication and to get tested for COVID-19.” (Female, 26) |
| Poor | Fair | “While I understand that wait times are long, it was over 5 hours. There was nowhere to check wait times, not to cancel the call. I asked the doctor if she was able to order COVID-19 testing.” (Female, 47) |
| Poor | Poor | “Physician rushed me and did not provide clear guidance and direction.” (Female, 40) |
Discussion
This was the first cross-sectional study evaluating the experience of patients with COVID-19 symptoms in a virtual care environment. We found that all patients who had COVID-19 symptoms were diagnosed differently. Higher utilization of video visits was observed among younger (under 18 years) patients. Patient demand for virtual visits increased on weekend days compared to weekdays. Over 24 hours, the highest volume of visits occurred between 7 am and 8 pm. The longest wait time occurred between midnight and 6 am as well as on Sundays. Lack of staff during off peak times possibly resulted in long wait times especially that the volume of visits between midnight and 6 am was lower than the volume of visits during the day. Approximately, 40% of COVID-19 patients received prescription; however, the prescribing rates varied between COVID-19 concerned patients with similar diagnoses.
Patients with COVID-19 symptoms rated their virtual experience with a provider positively. The convenience of no transportation or physical interaction with others was praised by patients. The extra-long wait times, due to an unprecedented volume of calls since the COVID-19 pandemic, were criticized by patients. While wait times were longer due to increased call volume, COVID-19 cases in the community were also rising, which could have led to more COVID-19-related symptoms. Resolving wait times can be fixed by increased staffing; however, the shortage of medical providers for in-person or virtual environments remains a challenge during this time. The relatively low satisfaction survey response rate can be explained by the overall mood of patients with COVID-19 suspicion who may be in a rush to receive care or testing rather than complete the satisfaction survey.
Like the airline industry, virtual clinics should consider the use of callback options during high-volume call times. Additionally, providing an approximated wait time can be incredibly valuable in improving patient satisfaction. Similar to the aviation industry, a customer calling the airline company is presented with an estimated waiting time to connect with a customer service representative.
Some virtual patients complained about feeling rushed in virtual visits, there being a lack of eye contact with their provider or missing clear guidance. Since the shift to virtual care is novel to everyone, virtual care training is essential for both users—patients and providers. A clear set of expectations and virtual care best practices need to be developed and communicated.
Telehealth Best Practices
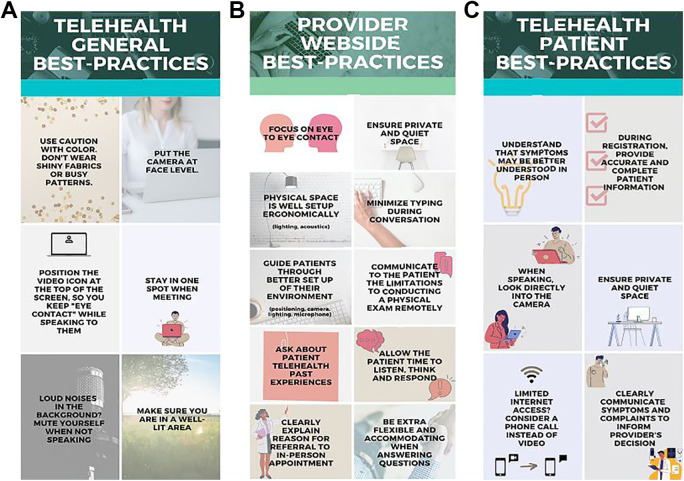
In addition to the briefly suggested best practices (13), we created a set of telehealth best practices based on patient-reported experiences to improve the quality of virtual visits based on the COVID-19 increased workflow, subsequent to data collection. Our recommendations include general, provider, and patient telehealth best-practices.
Generally, in virtual care, there are ways that can improve the telehealth experience regardless of the participant’s role. First, unlike in-person visits, participants are advised to use caution with color because wearing shiny fabrics or busy patterns can be distracting and frustrating to the other party. Second, setting the camera at face-level ease eye contact. Third, to keep eye contact with the person you are speaking to, position their icon at the top of the screen (below the camera). Therefore, when you are looking at them and speaking, it will seem like you are looking at the camera. Forth, it is recommended to stay in one place during the virtual visits and to avoid continuous movement. Lastly, if there are loud noises in the background, mute yourself when you are not speaking (Figure 4A).
Figure 4.
Telehealth best practices by (A) general, (B) provider, (C) patient.
Additionally, our best practice recommendations include “web-side” etiquettes, comparable to bedside etiquette, for providers such as: (a) focus on eye to eye contact when speaking or listening to the patient; (b) ensure you are in a private and quiet space; (c) physical space is well setup ergonomically with adequate lighting and acoustics; (d) when possible, take notes and minimize typing during the conversation which may add noise to the conversation; (e) guide patients through better set up of their environment (positioning, camera, lightning, and microphone); (f) communicate to the patient the limitations to conducting a physical exam remotely; (g) ask the patient of their virtual care history and reason for choosing virtual care to better understand and manage expectations; (h) expect “lag-time” and therefore allow the patient time to listen, think, and respond; (i) if referring a patient to an in-person appointment, clearly explain the reason for referral and the financial implications, if any; and (j) provider is the only point of contact for the patient, so providers should be more flexible and accommodating when answering questions (Figure 4B).
For patients, it is important to manage and set the expectations prior to a virtual visit. To ensure a positive experience, we recommend best practices for patients: (a) Virtual care does not suit all health conditions such as testing for COVID-19; therefore, it is essential for patients to understand the suitable health care options to avoid unnecessary costs and/or referrals; (b) during registration, accurate and complete patient information can expedite the workflow process to find the correct and appropriate provider; (c) set your camera to eye level, and when speaking, look directly into the camera and avoid bright light in the background; (d) make sure you are in a private and quiet space; (e) if you have limited internet access consider a phone call instead of video; and (f) the quality of virtual care relies heavily on effective communication of the patient’s symptoms and complaints to inform the provider’s decision (Figure 4C).
Limitations and Future Work
A limitation to this study is the inability to follow-up with virtual patients on the prognosis of their illness post their virtual visit. We were not able to conduct follow-up visits to assess the clinical outcome of each COVID-19-related visit. The severity of the illness may have been a confounding factor to the varying levels of prescribing among patients with the same diagnosis. Additionally, since COVID-19 testing is not available for patients to self-administer, we were unable to provide any virtual COVID-19 testing to screen for COVID-19 infection, leading to patients being referred for in-person testing. Only 7.1% of patients with COVID-19-related chief complaints completed the survey for patient satisfaction. In the future, we plan to evaluate virtual care outcomes through conducting follow-up surveys asking about the need for hospitalization or in-person appointment post-virtual visit.
Conclusion
This study evaluated the virtual experiences of patients with COVID-19 symptoms. There were different experiences for patients depending on their choice of communication. Long wait times were a major drawback in the patient experience. We have learned from evaluating the experience of our first cohort of COVID-19 Concern patients. This evaluation provided a list of best practices for providers and patients to use during virtual care visits. The future holds great promise for telehealth after the COVID-19 crisis, and thereby, there is a need to optimize telehealth practices in order to make it more sustainable, effective, and meaningful health care delivery medium.
Author Biographies
Saif Khairat is an assistant professor of health informatics with expertise in the application of telehealth/telemedicine to improve health access, disparities, and patient outcomes.
Malvika Pillai is a PhD candidate in Health Informatics at the University of North Carolina at Chapel Hill. Ms Pillai is an NIH National Library of Medicine Doctoral Fellow.
Barbara Edson is the executive director of the Virtual Care Center at UNC Health.
Robert Gianforcaro is the executive medical director of Population Health and Virtual Care at UNC Health.
Footnotes
Authors’ Note: All authors had access to the data and a role in writing the manuscript. IRB approval was obtained from the University of North Carolina at Chapel Hill (18-1628).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by NIH/NLM 1T15LM012500-01.
ORCID iD: Saif Khairat, PhD, MPH, FAMIA  https://orcid.org/0000-0002-8992-2946
https://orcid.org/0000-0002-8992-2946
References
- 1. Fortuna RJ, Nagel AK, Rocco TA, Legette-Sobers S, Quigley DD. Patient experience with care and its association with adherence to hypertension medications. Am J Hypertens. 2018;31:340–345. [DOI] [PubMed] [Google Scholar]
- 2. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care, 2005;43:521–530. [DOI] [PubMed] [Google Scholar]
- 3. Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012;172:1204–1210. [DOI] [PubMed] [Google Scholar]
- 4. Wolf J, Niederhauser V, Lavela S. Defining patient experience. Patient Experi J. 2014;1:7–19. [Google Scholar]
- 5. Hollander JE, Carr BG. Virtually Perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 6. Khairat S, Liu S, Zaman T, Edson B, Gianforcaro R. Factors determining patients’ choice between mobile health and telemedicine: predictive analytics assessment. JMIR Mhealth Uhealth. 2019;7:e13772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vankipuram M, Kahol K, Cohen T. Toward automated workflow analysis and visualization in clinical environments. J Biomed Inf. 2011;44:432–440. [DOI] [PubMed] [Google Scholar]
- 8. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open, 2013;3:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hedges C, Hunt C, Ball P. Quiet time improves the patient experience. J Nurs Care Quality. 2019;34:197–202. [DOI] [PubMed] [Google Scholar]
- 10. Berkowitz B. The patient experience and patient satisfaction: measurement of a complex dynamic. Online J Issues Nurs. 2016;21:1. [DOI] [PubMed] [Google Scholar]
- 11. Khairat S, Meng C, Xu Y, Edson B. Interpreting COVID-19 and virtual care trends: cohort study. JMIR Public Health Surveill. 2020;6:e18811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khairat S, Haithcoat T, Liu S, Zaman T, Edson B, Gianforcaro R, et al. Advancing health equity and access using telemedicine: a geospatial assessment. J Am Med Inform Assoc. 2019;26:796–805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mehrotra A, Ray K, Brockmeyer MD. Rapidly converting to “virtual practices”: outpatient care in the era of COVID-19. Catalyst non-issue content, 2020;1.