Abstract
Objective:
Definitions of shared decision-making (SDM) have largely neglected to consider goal setting as an explicit component. Applying SDM to people with multiple long-term conditions requires attention to goal setting. We propose an integrated model, which shows how goal setting, at 3 levels, can be integrated into the 3-talk SDM model.
Method:
The model was developed by integrating 2 published models.
Results:
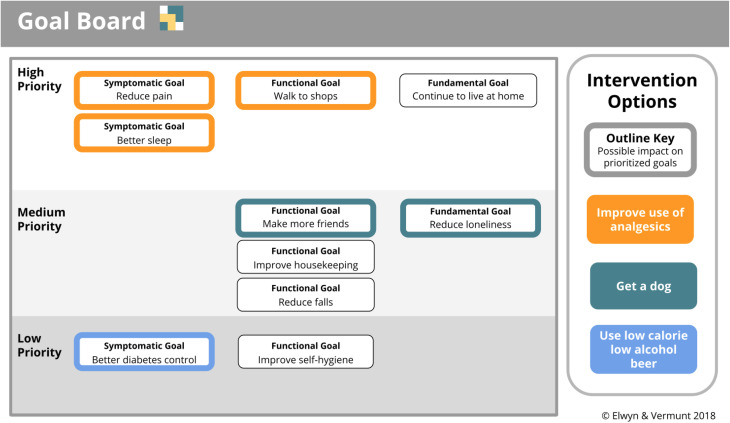
An integrated, goal-based SDM model is proposed and applied to a patient with multiple, complex, long-term clinical conditions to illustrate the use of a visualization tool called a Goal Board. A Goal Board prioritizes collaborative goals and aligns goals with interventional options.
Conclusion:
The model provides an approach to achieve person-centered decision-making by not only eliciting and prioritizing goals but also by aligning prioritized goals and interventions.
Practice Implications:
Further research is required to evaluate the utility of the proposed model.
Keywords: goal setting, goal prioritization, shared decision-making, communication model, comorbidity
Introduction
Expectations, intentions, and goals play a vital part in decision-making, so it seems odd that the early definitions of shared decision-making (SDM) neglected to include these critical aspects of planning future actions (1 –6). This is especially odd given that formulating clear goals are key to long-term planning in patient-centered care. More recently, the role of SDM has expanded to consider long-term conditions (7) and patients with complex multiple health issues (8). Clinical practice guidelines typically only consider single diseases (9 –12). Dealing with each disease separately can lead to polypharmacy and treatment burden (9,13,14), with the risk that inattention to context, or potential interactions, leads to care that is not aligned with individual goals or preferences (15,16). Many argue that paying attention to goals, a high priority for dealing with complex problems, has largely been neglected (17 –22,23).
The absence of goal setting as an explicit step in SDM models has been criticized by clinicians who provide care for elderly patients with complex health conditions (24 –32). Empirical work has led to a proposed 3-level model for goal setting (28). Patients typically seek help to address the first level of goals, that is, to obtain relief from symptoms or answers to direct concerns. Vermunt called this level symptom- or disease-specific goals. Goals can also refer to function, for example, losing the ability to walk upstairs. In addition, goals might draw on a person’s values, hopes, and priorities in life, which are labeled as fundamental goals. It may be easier to elicit goals in relation to symptoms and a loss of function than to address these longer horizon goals, which are often less clearly defined, but these fundamental goals are important as they help guide priorities. The 3-goal model describes the inter-relationships between these goal levels (symptomatic, functional, and fundamental) and how they serve as anchors or markers when decisions are being considered (28).
That SDM has failed to call explicit attention to the central role of goal setting, and that goals are multilayered, led to our realization that there was an opportunity to develop a model that clearly recognizes the relationship between goals and decision-making and to highlight the benefits of addressing goals in more detail. The recent update of the 3-talk SDM model paid attention to goals (33). But we also determined that more could be done to make sure that goals would be considered at 3 levels.
Our aim in this article is to develop an integrated goal-based model for SDM in order to provide both patients and clinicians with an SDM approach suitable for complex health-care problems. We hope that such a model will have high relevance for patients with complex health issues, who have more than 1 health-related condition, and where contextual factors makes decision-making challenging. We illustrate the model using a hypothetical clinical case and also propose a practical tool to support clinicians to adopt a communication process around goal setting.
Methods
To develop the new model, we contacted experts who had made key contributions to existing SDM models and had emphasized the role of goal setting in complex illness. We searched and summarized the literature in this area and held a series of meetings to (1) tabulate the key components of the 3-talk SDM model and the 3-level goal model, (2) agree on terms to use across both models, and (3) develop a provisional model by adopting the perspective of clinicians attempting to manage a complex clinical case.
We describe a hypothetical patient, Peter Smit, seeking help from a primary care clinician about multiple related problems experienced by many elderly individuals (see Box 1). We used an iterative approach, refining the model by considering the case from a clinician and patient perspective. We considered how a multilevel goal setting process would modify the existing 3-talk SDM model by paying attention to the elements listed in Box 1. We outlined the steps required to accomplish a goal-based SDM model, suggested specific questions to be adapted by clinicians, and describe how the model might be used to manage Peter Smit’s case (Box 2).
Box 1.
Elements Considered to Integrate the 3-Talk and 3 level Goal Models.
The relationship between goals and personal context, the problem or need identified
The different nature and levels of goals
Differences in goal priorities
Potential disagreements on goal priority between clinicians and patients
The relationship between the prioritization of goals and the range of possible interventions
Changes in decision-making processes, based on newly generated feedback loops
The cyclical and longitudinal nature of goal setting and goal attainment.
Box 2.
Peter Smit’s Case Description.
Divorced, lonely, drinking, and neglectful. Peter Smit is 70, divorced and retired. He often plays pool at a local bar, but he is lonely. He smokes and drinks roughly 5 units of alcohol most days. He has steep narrow stairs to his bedroom. He has fallen down these stairs on more than 1 occasion. This worries Peter. He neglects his house and his personal hygiene. His sister says that she can’t keep coming to clean up. She has telephoned the medical practice to say he’s not taking good care of himself.
Osteoarthritis of the hips. Peter has osteoarthritis in his left hip, which limits his walking. The pain wakes him up at night. He takes pain relievers.
Adult onset diabetes. His diabetes is poorly controlled with oral medication at the highest dose. His glycosylated hemoglobin level has been too high for at least a year, and during his last visit, his doctor said that insulin injections might have to be considered.
Results
In daily practice, needs are often interdependent and arise from personal, medical, and social problems. Decision-making in these situations is complicated by changes in health states and shifting priorities (9,34). Moreover, patients and clinicians often have different agendas (9,35 –39), which, if not made explicit, remain hidden, albeit influential. In presenting results, we will first describe the integrated conceptual model, followed by a description of the steps, tasks, and clinical questions that arise from the model. Finally, we will apply the new model (see Figure 1) to our hypothetical patient: Peter Smit.
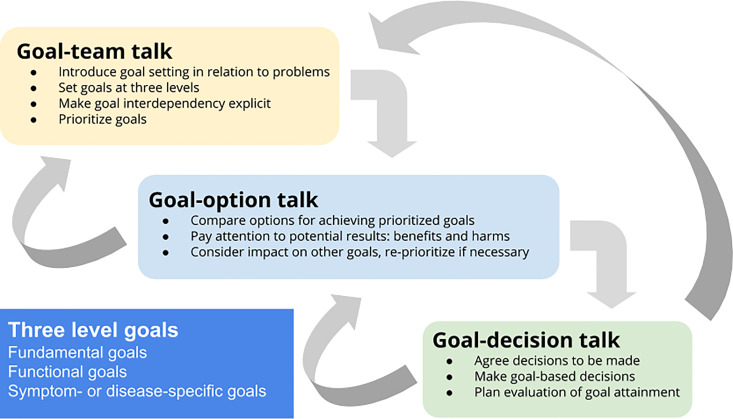
Figure 1.
The goal-based shared decision-making model.
Goal-Based SDM: Describing the New Model
As we built the model, we perceived a significant change in how we thought about Peter Smit’s problems. First, we noticed how decision-making became a secondary concern as our focus shifted to goals, and significantly to the guiding nature of making fundamental goals explicit. We realized that the task of considering goals becomes influential across all phases of the 3-talk SDM process. Goals as well as problems become the focus, because solutions to problems are best evaluated against potential goal achievement. In the integrated model (Figure 1), collaborative goal setting occupies a central place in the 3-talk SDM model. This goal-based SDM process (Figure 1) consists of 3 steps: (1) goal-team talk, (2) goal-option talk, and (3) goal-decision talk. Goal-based SDM represents a shift in perspective: Previous models of SDM assume a relatively fixed range of options. Goal-based SDM by inherently influencing the range, type, and number of relevant options to be considered, also inevitably influences the decision-making process.
Goal-Team Talk
Team talk refers to the work needed to form a partnership between the clinician and the patient to support decision-making (33). Finding agreement on the nature of the problems comes first. By adding a goal setting process, and, where necessary, making the inter-relatedness of goals explicit, the patient is left in no doubt that their goals shape the effort to find good solutions. In goal-team talk, goals are best elicited in a collaborative process by paying attention to 3 levels (symptom-or disease-specific, functional, and fundamental) and to the views of both the clinician and the patient. We suggest starting by discussing fundamental goals, because fundamental goals will also guide discussions about functional and disease- or symptom-specific goals. Where goals are interdependent, attention to their interaction is required. Some goals may be at odds with each other, so the need to prioritize some goals, and to make decisions accordingly, will become evident.
Goal-team talk also enhances the diagnostic process by explicitly considering personal factors and contextual factors, and as with all diagnostic steps, accuracy is key. Eliciting goals at the 3 levels is likely to improve the relevance of interventions, especially where patients have multisystem problems as well as needs that also arise from personal and social contexts, as is the case for Peter Smit, where it becomes clear that resolving his isolation is a goal that he is reluctant to declare and he needs to feel well supported before he might be able to admit to this issue. It is important to say that this task needs not be arduous. Most goals, if accurately elicited, would presumably be relatively stable, and, if well-documented, goal setting at the 3 levels may not need to be completed at every clinical encounter.
Goal-Option Talk
Option talk refers to a process of comparing reasonable intervention options, using risk communication principles (33). Goal-option talk adds to this process because it follows the prioritized goals elicited during goal-team talk. Goals at the multiple levels will ideally guide the selection of interventions that could best achieve the desired outcomes. For example, using pain relief medication could address symptoms of arthritis, as well as help Peter undertake more housekeeping tasks. Prioritizing goals might generate options specifically developed to attain those goals, and to ideas about how to sequence interventions, and to be more explicit about the efforts expected by the patient, the clinician, or the care team. The existence of conflicting goals might require thinking about trade-offs. In Peter’s case for instance, the option to continue living independently may be at odds with his wish to be less lonely.
Goal-Decision Talk
Decision talk describes the task of eliciting patient preferences in order to determine a specific decision. Goal-decision talk is similar and also ensures that desired goals guide the deliberation process. Typically, decisions are made by assessing which options seem best, given the range of benefits and harms. In goal-decision talk, it is possible that more than 1 goal is considered. What might be the impact on symptoms, function, and more fundamental goals be? For Peter, being able to stay at home (a fundamental goal) will require attention to pain (a symptomatic goal) and to his ability to navigate the stairs (a functional goal). This illustrates that the goal-based SDM model has feedback loops. Realizing the difficulty of addressing both symptoms and function may lead Peter to consider whether living independently is even desirable. In other words, goal-based decisions require an iterative process of examining and reexamining how problems, goals, and potential interventions influence each other (Figure 1). Decisions-to-be-made emerge or are refined by this process. An important element of goal-decision talk is planning the evaluation of goal attainment, an explicit feedback loop that becomes a new aspect of SDM.
Goal-Based SDM: Steps, Tasks, and Clinical Questions
The goal-based SDM model proposes a nonlinear iterative process. Goals are likely to evolve, as goal-team talk, goal-option talk, or goal-decision talk takes place. Goal priorities may shift, as potential consequences become clearer or as personal needs and contextual factors become evident. Table 1 illustrates the different steps and tasks to be considered and suggests useful questions at each step of the goal-based SDM process. Table 2 applies the model and illustrates how Peter Smit and his clinician achieve the steps.
Table 1.
A Goal-Based SDM Model: Steps, Tasks, and Clinical Questions.
| Steps | Tasks | Suggested Questions |
|---|---|---|
| Goal-team talk | Introduce goal setting and explain how goals relate to problems and to a personal narrative and context | “Let’s work as a team to explore what bothers you and what matters most to you to elicit the goals we should focus on…” |
| Set collaborative goals at 3 levels, starting from the patient’s perspective. | Fundamental goals “What are you hoping for in your life?” “What are you most afraid of losing in your life?” Functional goals “What activities do you want to be able to carry on doing?” Disease- or symptom-specific goals “What symptoms or aspect of disease do you want to change?” |
|
| Prioritize goals and make the interdependency of goals explicit | “Which of these goals are most important to you, and tell me why…?” “Let’s discuss how these goals relate to each other…” |
|
| Goal-option talk | Compare options for achieving prioritized goals | “Let’s compare the possible options that could help achieve these goals…” |
| Pay attention to expected results, risks, chances of success, and the effort needed to achieve the prioritized goals | “Let’s think about how likely these options are to achieve your goals, and how much effort on your part they might take…” | |
| Consider impact of options on other prioritized goals and reprioritize if necessary | “Do you think we need change which goals are most important to you?” | |
| Goal-decision talk | Agree decisions to be made | “Let’s agree on the decisions we need to make…” |
| Make goal-based decisions | “Given our discussion about goals, what’s your view about next steps…?” | |
| Plan evaluation of goal attainment | “What would attainment of your goals look like to you and how might we evaluate this?” |
Abbreviation: SDM, shared decision-making.
Table 2.
Peter’s Case Using Goal-Based SDM.
| Goal-team talk: Providing support and eliciting goals at multiple levels | Peter visits his clinician often for hip pain and dizziness. She invites Peter to talk about his goals. She summarizes the problems and mentions the risk from falls, from diabetes, and the decline in his ability to live independently. After exploring what bothers him most, she suggests they “work as a team” to set goals and the best interventions. |
| Goal setting | The clinician asks Peter about his hopes and what he is “most afraid of losing.” Peter admits that he really wants to stay living at home, despite his loneliness. Peter’s limited ability to walk is reducing his motivation to get out, and he finds himself watching television and drinking whiskey. Hip pain and insomnia bother him most. He accepts the need to clean his home but lacks motivation. His clinician is afraid he will fall down the stairs. Ideally, his diabetes also needs better control. Peter knows these problems are linked, but he does not know where to start. Peter and his clinician set collaborative goals at 3 levels, summarized below. |
| Goal levels | Fundamental goals
|
| Goal interdependency and conflict | The clinician notes that the goals of living independently and reducing loneliness, given his reduced mobility, are not easy to achieve. Building a wider social group may be difficult for Peter. The clinician offers that living in different accommodation may bring with it more opportunities to meet other people. Peter admits he had not considered that possibility. |
| Prioritizing goals | Peter says his urgent need is to reduce pain levels so that he can walk more and be less concerned about the stairs. However, Peter also says that he puts a high priority on being able to stay at home (a fundamental goal). He understands that improving his mobility (a functional goal) is a key contributor to realize his fundamental goal. Improving the management of Peter’s diabetes, a prominent clinical concern, is acknowledged, but discussions about this problem are postponed. |
| Goal-option talk: Goal-option talk is about considering the synergistic as well as conflicting nature of interventions as a means to goal attainment. | The Goal Board (Figure 2) helps display prioritized goals to both Peter and his clinician. It helps them discuss the potential positive and negative impact of intervention options on more than 1 goal. They notice that the interventions are not all medical and that some depend on Peter changing his behavior (using low-alcohol beer, for instance). Pain relievers may have impact on both sleep and mobility. Lowering alcohol intake and increasing mobility reduce the risk of falls (a functional goal) as well as increases the potential for Peter to stay living at his home (a fundamental goal). Similarly, looking after a dog could improve his mobility (a functional goal) and reduce loneliness (a fundamental goal). Shifting from whiskey to low-alcohol beer has the potential to improve his control of diabetes (a disease-specific goal) and reduce self-neglect (a functional goal). The sequence is relevant. It may be better to improve pain and mobility, before considering a dog. |
| Goal-decision talk: Goal-decision talk has 3 components: (1) clarifying the next steps (decisions that have to be made); (2) agreeing who takes those actions; and (3) agreeing how and when to evaluate the outcomes. | Given Peter’s goal priorities, the clinician’s would wish to address pain as effectively as possible, which may require considering listening to Peter’s preferences as he shares his views about options. Changing to low-alcohol beer seems logical to his clinician but may well be difficult for Peter if alcohol dependence exists. Perhaps, the decision to get a dog would be considered by many as the least urgent and most risky. But it is also possible that this intervention could have the maximum impact: It might also excite Peter. Peter’s sense of loneliness and his motivation to self-care might change; he may walk more, meet others, and take more pride in his home. The outcomes are unknown, so Peter and his clinician decide to focus on pain relief first and to evaluate this decision in 4 weeks. The clinician’s role is supportive, employing the skills of motivational interviewing where behavior change is required, and SDM when comparing options (40). |
Abbreviation: SDM, shared decision-making.
Visualizing the Results: Goal Board
Eliciting goals at the 3 levels, prioritizing them, and considering many possible interventions that could be helpful mean thinking about many things. Using language alone may not be ideal. In applying the model, we found it best to visualize these elements in what we called a Goal Board (see Figure 2). At a basic level, this could be a flat surface where goals could be summarized on pieces of colored paper, then moved up and down to illustrate goal priority. Goals may cluster at priority levels and the possible relationships between goals and the possible effect of interventions could be discussed. For example, improving the use of analgesics is primarily directed at the goal of reducing pain, but this intervention might also address the goal of improving mobility. Using a visualization method would help patients navigate the relationship between goals and interventions. Figure 2 shows an example of a near final version, which required collaboration between Peter and his clinician as they talked about which was the most urgent problem and how it could be solved.
Figure 2.
Goal Board: aligning prioritized goals with intervention options.
Key Insights
To summarize, by eliciting 3 levels of goals, we observed the need to use visualizing techniques to support the work of discussing prioritization and the potential impact of more than one intervention. Eliciting goals at the 3 levels leads to wider and deeper discussions about priorities, beyond resolving symptoms or biomedical abnormalities. Asking about fundamental goals leads to more insight about “what matters most” for individual patients. Talking about goals brings clarity about who is responsible for action: patients, health professionals, or others? And because interventions need to be tested, the process has to become iterative and regularly evaluated.
Discussion and Conclusion
Discussion
Goal-based SDM
Asking patients to think about goals entails adopting a mind shift, and it has significant consequences, especially if goals are conceived as having multiple levels, prioritized, and considered in relation to both their feasibility and the likely effectiveness of possible interventions. Vermunt’s work in specifying a multilevel goal model in health care, specifically for patients with complex illness (28), has brought more depth to recent discussions about the relevance of goals for decision-making. Goals play a central role in guiding health-care decisions, although of course the clinician has to judge when and how often to focus on goals. Taking mutual goals into account changes the nature of decision-making processes, because bringing goals into clearer focus changes how potential interventions are considered and offered. In short, the ends help define the means. A goal-based approach strengthens the likelihood of person-centered care being offered because it is more aligned to personal priorities, while also paying attention to what might be practical and realistic.
By proposing a goal-based SDM model, we made the following observations. Contrary to earlier models of SDM, prioritized goals steer the options presented and decisions that have to be made. Putting goal setting as the guiding principle for conducting clinical interactions has profound impact on relationship building and communication processes, especially when the focus goes to fundamental goals. Asking about an individual’s fundamental goals requires reflection about the future, priorities, values, and relationships, which are of course sensitive personal issues, and likely to require empathetic skilled communication. It is, therefore, inconceivable that dialogues about fundamental, and other related goals, could occur in the absence of a collaborative effort (40).
Strengths and weaknesses of the methods
By applying the integrated goal-based SDM model to a clinical case that represented multiple long-term conditions in the context of many social and psychological problems, we were addressing a common challenge for health systems across the globe (23,41 –44). By imagining how a clinician could apply the goal-based SDM to Peter’s situation, we obtained insights and modified the model. We acknowledge that the utility of this integrated model requires testing in clinical contexts. We also acknowledge that the integration is the result of a collaboration between 2 clinicians who developed these 2 models and who are therefore likely to advocate that goals underpin decision-making processes. Further efforts are required to assess whether this proposed integration has merit.
Results in context
Proposing goal setting as part of SDM for older patients is not novel (35). Attention has recently been drawn to goal setting being a prerequisite to decision-making for individuals with multiple long-term conditions (19,20,24,25,28,29,31,32), and the sharing of treatment goals is at the core of the Ariadne principles, which aim to provide orientation in decision-making in situations where people face the challenges of multiple morbidity (9,36). However, we are not aware of previous efforts to embed goal setting into a model of SDM in order to assess neither the impact on decision-making nor efforts to consider the impact of setting goals at these 3 levels.
Conclusion
In hindsight, it is odd that goal setting has been absent from models of SDM. Although this proposed model is novel, and the application to a clinical case is hypothetical, we hope to have demonstrated the potential impact of this approach, especially for patients with complex problems.
Practice Implications
Further development of this goal-based SDM requires empirical work. Technological applications could assist with goal visualization, but the first task is to examine whether clinicians and patients would find the approach to be of value.
Author Biographies
Glyn Elwyn is a professor in health service research, focused on shared decision-making and coproduction.
Neeltje Petronella Catharina Anna Vermunt has a background as general practitioner and economist. Her academic interests focus on goal setting and shared decision-making in complex health-care. Furthermore she works for a strategic advisory council for the Dutch government.
Footnotes
Authors’ Note: Joint first authorship. Neeltje Vermunt developed the 3-goal model as part of her doctoral work in the Netherlands, supported by Gert Westert, PhD, Marcel Olde Rikkert, MD, PhD, Marjan J. Meinders, PhD, Mirjam Harmsen, PhD, Glyn Elwyn, BA, MD, MSc, PhD, and Jako Burgers, MD, PhD. Glyn Elwyn led a collaboration that led to the 3-talk model of shared decision-making. Glyn Elwyn and Neeltje Vermunt developed the goal-based 3-talk model of shared decision-making, including the Goal Board concept, and retain copyright on the design. Goal Board © Copyright of the Goal Board concept and layout 2018 belongs to Glyn Elwyn and Neeltje Vermunt. All rights are reserved. The Goal Board layout may not be reproduced, stored, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of both Glyn Elwyn and Neeltje Vermunt.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Financial: Glyn Elwyn has edited and published books that provide royalties on sales by the publishers: the books include Shared Decision Making (Oxford University Press) and Groups (Radcliffe Press). He has in the past provided consultancy for organizations, including (1) Emmi Solutions LLC who developed patient decision support tools; (2) National Quality Forum on the certification of decision support tools; (3) Washington State Health Department on the certification of decision support tools; and (4) SciMentum LLC, Amsterdam (workshops for shared decision making). Director of &think LLC which owns the registered trademark for Option Grids patient decision aids. He provides consultancy in the domain of shared decision-making and patient decision aids to (1) Access Community Health Network, Chicago (Federally Qualified Medical Centers), and (2) EBSCO Health Option Grids patient decision aids. Nonfinancial: He initiated the Option Grid Collaborative, and the existing tools are hosted on a website managed by Dartmouth College, on http://optiongrid.org/, and are freely available until such time as they have expired. He owns copyright in measures of shared decision-making and care integration, namely, collaboRATE, integRATE, and Observer OPTION-5 and Observer OPTION-12. These measures are freely available for use. Neeltje Vermunt is employed by the Dutch Council for Health and Society (Raad voor Volksgezondheid en Samenleving, RVS), a strategic advisory council for the Dutch government. The Council had no role in the study design, the conduct of this research, in the writing of this article, or the decision to submit it for publication.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Glyn Elwyn, BA, MD, MSc, PhD  https://orcid.org/0000-0002-0917-6286
https://orcid.org/0000-0002-0917-6286
References
- 1. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (Or it takes at least two to tango). Soc Sci Med. 1997;44:681–92. [DOI] [PubMed] [Google Scholar]
- 2. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–12. [DOI] [PubMed] [Google Scholar]
- 3. Stiggelbout AM, Pieterse AH, De Haes JCJM. Shared decision making: concepts, evidence, and practice. Patient Educ Couns. 2015;98:1172–79. [DOI] [PubMed] [Google Scholar]
- 4. Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. [DOI] [PubMed] [Google Scholar]
- 6. Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;(4):CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Montori VM, Gafni A, Charles C. A shared treatment decision-making approach between patients with chronic conditions and their clinicians: the case of diabetes. Health Expect. 2006;9:25–36. Blackwell Science Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vermunt N. Collaborative goal setting. Towards a goal-oriented approach of shared decision-making in complex elderly care [Internet]. Radboud University. 12 September 2018. Retrieved from: https://repository.ubn.ru.nl//handle/2066/194313.
- 9. Muth C, van den Akker M, Blom JW, Mallen CD, Rochon J, Schellevis FG, et al. The Ariadne principles: how to handle multimorbidity in primary care consultations. BMC Med. 2014;12:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient priority-directed decision making and care for older adults with multiple chronic conditions. Clin Geriatr Med. 2016;32:261–75. [DOI] [PubMed] [Google Scholar]
- 11. Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. BMJ. 2015;350:h176. [DOI] [PubMed] [Google Scholar]
- 12. Fried TR, Tinetti ME, Iannone L. Primary care clinicians’ experiences with treatment decision making for older persons with multiple conditions. Arch Intern Med. 2011;171:75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lorgunpai SJ, Grammas M, Lee DSH, McAvay G, Charpentier P, Tinetti ME. Potential therapeutic competition in community-living older adults in the U.S.: use of medications that may adversely affect a coexisting condition. Quinn TJ, editor. PLoS One. 2014;9:e89447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zulman DM, Asch SM, Martins SB, Kerr EA, Hoffman BB, Goldstein MK. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29:529–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wyatt KD, Stuart LM, Brito JP, Carranza Leon B, Domecq JP, Prutsky GJ, et al. Out of context: clinical practice guidelines and patients with multiple chronic conditions: a systematic review. Med Care. 2014;52:S92–100. [DOI] [PubMed] [Google Scholar]
- 16. Tinetti ME, Bogardus ST, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351:2870–4. [DOI] [PubMed] [Google Scholar]
- 17. Upshur C, Weinreb L. A survey of primary care provider attitudes and behaviors regarding treatment of adult depression: what changes after a collaborative care intervention? Prim Care Companion J Clin Psychiatry. 2008;10:182–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sinnott C, Mc Hugh S, Browne J, Bradley C. GPs’ perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open. 2013;3:e003610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc. 2012;60:E1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reuben DB, Tinetti ME. Goal-oriented patient care—an alternative health outcomes paradigm. N Engl J Med. 2012;366:777–9. [DOI] [PubMed] [Google Scholar]
- 21. Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94:291–309. [DOI] [PubMed] [Google Scholar]
- 22. Légaré F, Thompson-Leduc P. Twelve myths about shared decision making. Patient Educ Couns. 2014;96:281–6. [DOI] [PubMed] [Google Scholar]
- 23. Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA. 2012;307:2493–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Osborn R, Moulds D, Squires D, Doty MM, Anderson C. International survey of older adults finds shortcomings in access, coordination, and patient-centered care. Health Aff. 2014;33:2247–55. [DOI] [PubMed] [Google Scholar]
- 25. Grudniewicz A, Nelson M, Kuluski K, Lui V, Cunningham HV, X Nie J, et al. Treatment goal setting for complex patients: protocol for a scoping review. BMJ Open. 2016;6:e011869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vermunt NPCA, Harmsen M, Westert GP, Olde Rikkert MGM, Faber MJ. Collaborative goal setting with elderly patients with chronic disease or multimorbidity: a systematic review. BMC Geriatr. 2017;17:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vermunt NPCA, Westert GP, Olde Rikkert MGM, Faber MJ. Assessment of goals and priorities in patients with a chronic condition: a secondary quantitative analysis of determinants across 11 countries. Scand J Prim Health Care. 2018;36:80–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vermunt NP, Harmsen M, Elwyn G, Westert GP, Burgers JS, Olde Rikkert MG, et al. A three-goal model for patients with multimorbidity: a qualitative approach. Health Expect. 2018;21:528–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. van de Pol MHJ, Fluit CRMG, Lagro J, Slaats YHP, Olde Rikkert MGM, Lagro-Janssen ALM. Expert and patient consensus on a dynamic model for shared decision-making in frail older patients. Patient Educ Couns. 2016;99:1069–77. [DOI] [PubMed] [Google Scholar]
- 30. van der Weijden T, Post H, Brand PLP, van Veenendaal H, Drenthen T, van Mierlo LA, et al. Shared decision making, a buzz-word in the Netherlands, the pace quickens towards nationwide implementation. Z Evid Fortbild Qual Gesundhwes. 2017;123-124:69–74. [DOI] [PubMed] [Google Scholar]
- 31. Hoffmann T, Jansen J, Glasziou P. The importance and challenges of shared decision making in older people with multimorbidity. PLoS Med. 2018;15:e1002530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vermunt G, Elwyn G, Westert G, Harmsen M, Olde Rikkert M, Meinders M. Goal setting is insufficiently recognised as an essential part of shared decision-making in the complex care of older patients: a framework analysis. BMC Fam Pract. 2019;20:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ. 2017;359:j4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ. 2012;345:e6572. [DOI] [PubMed] [Google Scholar]
- 35. Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ Couns. 2006;63:145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Naik AD, Martin LA, Moye J, Karel MJ. Health values and treatment goals of older, multimorbid adults facing life-threatening illness. J Am Geriatr Soc. 2016;64:625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Luijks HD, Loeffen MJW, Lagro-Janssen AL, van Weel C, Lucassen PL, Schermer TR. GPs’ considerations in multimorbidity management: a qualitative study. Br J Gen Pract. 2012;62:e503–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Voigt I, Wrede J, Diederichs-Egidi H, Dierks ML, Junius-Walker U. Priority setting in general practice: health priorities of older patients differ from treatment priorities of their physicians. Croat Med J. 2010;51:483–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Reuben DB. Medical care for the final years of life. JAMA. 2009;302:2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Elwyn G, Lloyd A, May C, van der Weijden T, Stiggelbout A, Edwards AGK, et al. Collaborative deliberation: a model for patient care Patient Educ Couns. Elsevier Ireland Ltd; 2014;97:158–184. [DOI] [PubMed] [Google Scholar]
- 41. Mangin D, Heath I, Jamoulle M. Beyond diagnosis: rising to the multimorbidity challenge. BMJ. 2012;344:e3526. [DOI] [PubMed] [Google Scholar]
- 42. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. [DOI] [PubMed] [Google Scholar]
- 43. Bergman H, Karunananthan S, Robledo LMG, Brodsky J, Chan P, Cheung M, et al. Understanding and meeting the needs of the older population: a global challenge. Can Geriatr J. 2013;16:61–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bolen SD, Sage P, Perzynski AT, Stange KC. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev. 2016;17:18–32. [DOI] [PMC free article] [PubMed] [Google Scholar]