We evaluated if the COVID-19 pandemic influences parents’ intentions to have their children receive the 2020–2021 seasonal influenza vaccination.
Abstract
OBJECTIVES:
Evaluate if the coronavirus disease 2019 (COVID-19) pandemic influences parents’ intentions to have their children receive the 2020–2021 seasonal influenza vaccination.
METHODS:
In May 2020, we recruited 2164 US parents and guardians of children ages 6 months to 5 years to complete a brief online survey that examined parental behavior and decision-making in response to experimental stimuli and real-world events. We estimated a multivariate multinomial logistic regression (controlling for key demographics) to assess the relationship between a child’s 2019–2020 influenza vaccination status and the COVID-19 pandemic’s influence on a parent’s intentions for their child’s 2020–2021 influenza vaccination.
RESULTS:
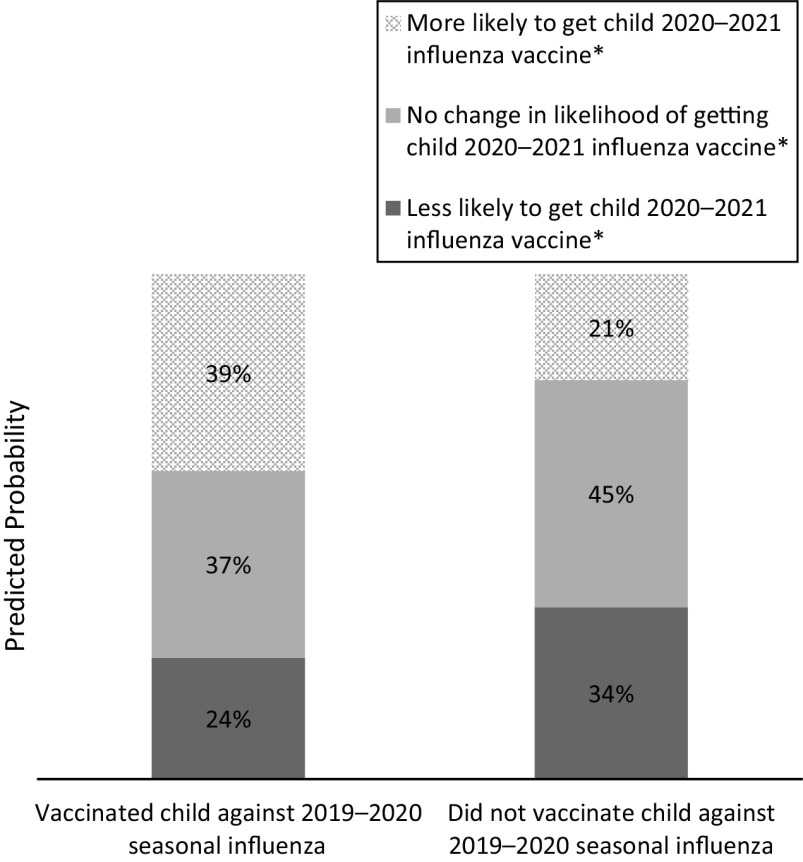
Changes in vaccination intentions significantly differed between parents whose children received the 2019–2020 influenza vaccine compared with those whose children did not (P < .001). Specifically, among parents whose children did not receive the 2019–2020 vaccine, 34% (95% confidence interval [CI]: 30%–37%) reported that the COVID-19 pandemic made them less likely to have their child receive the 2020–2021 vaccine. Among those whose children did receive the 2019–2020 vaccine, this figure was just 24% (95% CI: 22%–27%). Conversely, only 21% (95% CI: 18%–24%) of parents whose children did not receive the 2019–2020 vaccine reported that the COVID-19 pandemic made them more likely to have their child receive the 2020–2021 vaccine, compared with 39% (95% CI: 36%–41%) of parents whose children did receive the 2019–2020 vaccine.
CONCLUSIONS:
The COVID-19 pandemic alone does not appear sufficient to encourage the uptake of pediatric seasonal influenza vaccination. Instead, the COVID-19 pandemic may exacerbate polarity in vaccination uptake.
What’s Known on This Subject:
The convergence of coronavirus disease 2019 (COVID-19) and influenza could result in considerable morbidity and mortality, and pediatric vaccination will be key to mitigating a dual epidemic. Yet, we do not know if the COVID-19 pandemic influences parents’ pediatric influenza vaccination intentions.
What this Study Adds:
The COVID-19 pandemic alone does not appear sufficient to encourage the uptake of pediatric seasonal influenza vaccination. Instead, the COVID-19 pandemic may exacerbate polarity in vaccination uptake.
Experts warn that the convergence of coronavirus disease 2019 (COVID-19) and seasonal influenza this year will result in considerable morbidity and mortality.1 Yet, only ∼60% of children in the United States receive a seasonal influenza vaccination annually.2 Pediatric vaccination will be an important component to mitigating a dual influenza and COVID-19 epidemic. Vaccinating children is necessary not only to prevent influenza in children3 but also to establish herd immunity within the general population.4 Recent influenza vaccination coverage has been too low to achieve herd immunity.4 The COVID-19 pandemic has increased uptake of some health-protective behaviors, including increased hand-washing and social distancing.5,6 The pandemic may also encourage vaccination behavior, but this remains unknown.
Past behavior consistently emerges as a strong predictor of future behavior across a variety of health behaviors.7–10 This literature would thus suggest that whether a parent vaccinated their child against seasonal influenza in a previous year would strongly predict their intentions for influenza vaccination in the current year. Yet, we have not studied this phenomenon of past vaccination behavior predicting future behavior in the context of a major disruption such as a pandemic.
Ouellette and Wood8 theorized that novel behaviors are unable to be governed by habit and are thus more likely the result of conscious and intentional processes. Although pediatric influenza vaccination is not a new behavior, parents are living in new contexts. Living in a pandemic has resulted in parents re-evaluating what used to be their “default options,” such as sending their children to school for in-person instruction. Likewise, previous routine behaviors such as pediatric vaccinations may now be novel decisions that require conscious processing. In this study, we explore if the COVID-19 pandemic influences parents’ intentions to have their children receive the seasonal influenza vaccination. Specifically, we evaluate if previous influenza vaccination behavior is associated with parents’ pediatric influenza vaccination intentions for the 2020–2021 influenza season.
Methods
Participants
In May 2020, we recruited a diverse national convenience sample of 2164 US parents or guardians (hereafter referred to as “parents”) of children ages 6 months to 5 years through Dynata, a survey research firm, as part of a larger research study that examined parental behavior and decision-making in response to experimental stimuli and real-world events. The primary study examined the effect of different children’s storybook messages on parents’ message reactions. For that study, we calculated sample size needs to detect a small effect (Cohen f = 0.1) or larger with 90% power.
Procedures
Participants provided informed consent, completed a 15-minute online survey, and received incentives from Dynata (eg, gift cards) for participating. The Harvard TH Chan School of Public Health Institutional Review Board approved this study.
Measures
The primary outcome was the extent to which a parent’s intentions for getting their child the seasonal influenza vaccination for the 2020–2021 season changed, if at all, as a result of the COVID-19 pandemic. We measured change categorically, with response options ranging from 1 (I became much less likely to get my child the flu shot next year) to 5 (I became much more likely to get my child the flu shot next year).
Our focal predictor was the child’s seasonal influenza vaccination status for the previous season (2019–2020). Parents answered the question: “Did your child get the flu shot for the 2019–2020 flu season? This includes a flu shot received between September 2019 and today.” To obtain a random sampling of ages, we asked parents with >1 child between 6 months and 5 years old to answer for their child who had the most recent birthday.
We collected demographic characteristics including child’s age and sex; parent’s age, sex, relationship to the focal child, education, race and ethnicity, and political affiliation; and household income, household size, and the number of children age <18 living in the household. We assessed household income in the following categories: <$10 000, $10 000 to $14 999, $15 000 to $24 999, $25 000 to $34 999, $35 000 to $49 999, $50 000 to $74 999, $75 000 to $99 999, $100 000 to $149 999, $150 000 to $199 999, and ≥$200 000. Given the majority of households included 3 to 4 individuals (coinciding with 200% of the federal poverty level ranging from $43 404 to $52 400), we categorized “low income” as <$50 000 annually.
Analysis
The analytic sample included respondents with complete information on covariates (n = 1893). Respondents with incomplete information on all covariates had children that were slightly younger, were more likely to be guardians, had slightly lower levels of education, were more likely to be a member of a racial group that was not white or African American, were more likely to affiliate as Republican or Independent, had larger households, and were lower income compared with respondents with complete information (Supplemental Table 2). We do not expect these differences to bias results, however, given the high proportion (ie, 87%) of respondents with complete information.11
We first calculated descriptive statistics, stratified by child’s seasonal influenza vaccination status for the 2019–2020 season. We then estimated a multivariate multinomial logistic regression (controlling for the above demographics) to assess the relationship between children’s 2019–2020 influenza vaccination status and the COVID-19 pandemic’s influence on parents’ intentions for their child’s 2020–2021 influenza vaccination. We coded parent intentions as (1) becoming more likely, (2) no change, or (3) becoming less likely to get their child the influenza vaccination. We report results from the multinomial model as adjusted predicted probabilities of becoming more likely to vaccinate their child, becoming less likely to vaccinate their child, or experiencing no change in vaccination intentions as a result of the COVID-19 pandemic.
Results
Table 1 provides descriptive and bivariate statistics for the analytic sample. A majority (60%) of parents reported the COVID-19 pandemic changed their seasonal influenza vaccination intentions for their children. Changes in vaccination intentions significantly differed between parents whose children received the 2019–2020 influenza vaccine compared with those whose children did not (P < .001). Specifically, among parents whose children did not receive the 2019–2020 influenza vaccine, 34% reported that the COVID-19 pandemic made them less likely to have their child receive the 2020–2021 influenza vaccine compared with their plans before the pandemic. Among those whose children did receive the 2019–2020 influenza vaccine, this figure was just 25%. Conversely, only 21% of parents whose children did not receive the 2019–2020 influenza vaccine reported that the COVID-19 pandemic made them more likely to have their child receive the 2020–2021 influenza vaccine, compared with 38% of parents whose children did receive the 2019–2020 influenza vaccine.
TABLE 1.
Descriptive Statistics, Stratified by Child’s 2019–2020 Seasonal Influenza Vaccination Status
| Total (n = 1893), n (%) | Did Not Receive 2019–2020 Influenza Vaccine (n = 674), n (%) | Received 2019–2020 Influenza Vaccine (n = 1219), n (%) | P | |
|---|---|---|---|---|
| Change in child’s 2020–21 influenza vaccination intentions due to COVID-19 | <.001a | |||
| Less likely | 532 (28) | 230 (34) | 302 (25) | |
| No change | 753 (40) | 303 (45) | 450 (37) | |
| More likely | 608 (32) | 141 (21) | 467 (38) | |
| Child age | .55 | |||
| 6–11 mo | 281 (15) | 94 (14) | 187 (15) | |
| 12–23 mo | 239 (13) | 81 (12) | 158 (13) | |
| 2 y | 340 (18) | 119 (18) | 220 (18) | |
| 3 y | 359 (19) | 128 (19) | 231 (19) | |
| 4 y | 310 (16) | 125 (19) | 185 (15) | |
| 5 y | 365 (19) | 127 (19) | 238 (20) | |
| Child gender | .42 | |||
| Male | 934 (49) | 320 (47) | 614 (50) | |
| Female | 912 (48) | 335 (50) | 577 (47) | |
| Transgender, nonbinary, or another gender | 47 (2) | 19 (3) | 28 (2) | |
| Relationship to child | .07 | |||
| Parent | 1584 (84) | 550 (82) | 1034 (85) | |
| Guardian | 309 (16) | 124 (18) | 185 (15) | |
| Parent gender | .001a | |||
| Male | 545 (29) | 176 (26) | 369 (30) | |
| Female | 1306 (69) | 473 (70) | 833 (68) | |
| Transgender, nonbinary, or another gender | 42 (2) | 25 (4) | 17 (1) | |
| Parent age | .75 | |||
| 18–24 | 549 (29) | 191 (28) | 358 (29) | |
| 25–34 | 819 (43) | 293 (43) | 526 (43) | |
| 35–44 | 420 (22) | 148 (22) | 272 (22) | |
| 45–54 | 63 (3) | 23 (3) | 40 (3) | |
| 55+ | 42 (2) | 19 (3) | 23 (2) | |
| Parent education | .04a | |||
| Less than high school | 93 (5) | 37 (5) | 56 (5) | |
| High school | 368 (19) | 151 (22) | 217 (18) | |
| Some college | 354 (19) | 129 (19) | 225 (18) | |
| College graduate | 1078 (57) | 357 (53) | 721 (59) | |
| Parent race | .06 | |||
| White | 644 (34) | 212 (31) | 432 (35) | |
| Black or African American | 855 (45) | 322 (48) | 533 (44) | |
| American Indian or Alaska Native | 62 (3) | 30 (4) | 32 (3) | |
| Asian American or Pacific Islander | 47 (3) | 15 (2) | 32 (3) | |
| Other or Multiracial | 285 (15) | 95 (14) | 190 (16) | |
| Parent ethnicity | .12 | |||
| Hispanic | 922 (49) | 312 (46) | 610 (50) | |
| Non-Hispanic | 971 (51) | 362 (54) | 609 (50) | |
| Political affiliation | .28 | |||
| Democrat | 973 (51) | 330 (49) | 643 (53) | |
| Republican | 413 (22) | 156 (23) | 257 (21) | |
| Independent | 507 (27) | 188 (28) | 319 (26) | |
| Household size, mean (SD) | 3.6 (2.5) | 3.7 (2.5) | 3.6 (2.5) | .68 |
| Household income | .04a | |||
| Low income | 913 (48) | 347 (51) | 566 (46) | |
| Middle or high income | 980 (52) | 327 (49) | 653 (54) |
P values according to Pearson χ2 test. Low-income is defined as < $50 000 per year.
Indicates significant differences at α = 0.05.
These bivariate associations were confirmed in the multivariate adjusted analysis (Fig 1). Specifically, the multinomial logistic regression model suggests that, among parents whose children did not receive the 2019–2020 influenza vaccine, 34% (95% confidence interval [CI]: 30%–37%) reported that the COVID-19 pandemic made them less likely to have their child receive the 2020–2021 influenza vaccine. Among those whose children did receive the 2019–2020 influenza vaccine, this figure was just 24% (95% CI: 22%–27%). Conversely, only 21% (95% CI: 18%–24%) of parents whose children did not receive the 2019–2020 influenza vaccine reported that the COVID-19 pandemic made them more likely to have their child receive the 2020–2021 influenza vaccine, compared with 39% (95% CI: 36%–41%) of parents whose children did receive the 2019–2020 vaccine.
FIGURE 1.
Adjusted predicted probabilities for parents’ changes in intentions for children’s influenza vaccination as a result of the COVID-19 pandemic, according to 2019–2020 influenza vaccination status. *Indicates significant differences in adjusted predicted probabilities between parents whose child did versus did not receive the 2019–2020 influenza vaccination. Model adjusted for child’s age and sex; caregiver’s relationship to child; parent age, sex, education, race and ethnicity, and political affiliation; and household income (low income: <$50 000 annual) and size.
Given the collinearity between household size and number of children under the age of 18 years in the household, we did not include number of children as a covariate in the final model. However, sensitivity analyses including number of children instead of household size as a covariate revealed nearly identical results (Supplemental Fig 2).
Discussion
Parents reported polarized intentions regarding their children’s future seasonal influenza vaccination in response to the COVID-19 pandemic: those whose children had previously received the influenza vaccination reported a higher likelihood of future vaccination as a result of the pandemic, whereas those whose children had not received the vaccination reported a decreased likelihood. These results suggest that overall seasonal influenza vaccination rates may not increase simply because of an ongoing infectious disease pandemic. Instead, a significant predictor of future behavior remains past behavior.5 Thus, targeted efforts are likely to be needed to encourage uptake of the seasonal influenza vaccination.
Overall, we found that the majority of parents (60%) intend to change their pediatric influenza vaccination behavior this year as a result of the COVID-19 pandemic. On the surface, this suggests that COVID-19 may be disrupting the otherwise powerful influence of past behavior on future behavior for many parents. However, a closer examination of changes in parents’ intentions suggests that the opposite may be happening with regard to pediatric influenza vaccination, whereby past behaviors become increasingly entrenched. Ouellette and Wood8 proposed two pathways by which past behavior relates to future behavior: a direct and indirect pathway. The direct pathway models an automatic and habitual process,12 whereas in the indirect pathway, past behavior affects future behavior via conscious, intentional processes.13,14 Before the COVID-19 pandemic, parental vaccination behavior may have existed on the direct (ie, automatic) pathway. Disruptions caused by the pandemic may have moved parents’ vaccination decisions into a more intentional process. However, the influence of the pandemic on vaccination intentions does not appear to operate in the same way for all parents. Instead, it appears that the pandemic could lead to increasing polarization of parents’ pediatric influenza vaccination behaviors, whereby those previously not vaccinating report becoming even less likely to vaccinate in the future.
The question remains: How do we increase influenza vaccination uptake during the COVID-19 era? Psychological science offers insight into promising strategies for increasing vaccination.15 As one example, researchers have found that stronger social norms are associated with higher vaccination intentions and uptake,16,17 suggesting that social norms messaging (eg, through social media, mass media campaigns, or health care providers) could increase parents’ intentions to vaccinate their children. Strategies to close the “intention–behavior” gap, such as sending vaccination reminders18 and encouraging parents to form implementation intentions,19 can then help ensure those who intend to vaccinate follow through with these plans. Another approach is presumptive announcements, in which health care providers frame vaccination as the default behavior. Researchers in a recent randomized controlled trial with 30 clinics found that training physicians to offer vaccine recommendations as presumptive announcements significantly increased human papilloma virus vaccine initiation among 11- and 12-year-olds.20 A similar approach could be extended to seasonal influenza vaccination.
One limitation of the present analysis is the reliance on a convenience sample. However, the study team established a priori recruitment quotas to ensure a racially and ethnically diverse sample. Specifically, the survey firm recruited parents into the survey so that at least 25% of the sample would be Hispanic and another 25% would be African American (with the remainder recruited as a convenience sample without respect to race and ethnicity). Another limitation is that we surveyed parents in May 2020, and results may not generalize to later in the pandemic. Additionally, we assessed intentions to vaccinate; future research will clarify the COVID-19 pandemic’s influence on actual vaccination behaviors.
Conclusions
The COVID-19 pandemic alone does not appear sufficient to encourage the uptake of pediatric seasonal influenza vaccination. Instead, the COVID-19 pandemic may exacerbate polarity in vaccination uptake.
Acknowledgments
We thank Dina Goodman, MSPH, and Meg Salvia, MS, RDN, for their contributions to data collection and preparation.
Glossary
- CI
confidence interval
- COVID-19
coronavirus disease 2019
Footnotes
Dr Sokol conceptualized and designed the study aims, conducted the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Grummon led data collection, supported the conceptualization of the study aims, reviewed and revised the analytic plan, and critically reviewed and revised the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Sokol was supported by a postdoctoral award through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (F32HD100021-01) of the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Gostin LO, Salmon DA. The dual epidemics of COVID-19 and influenza: vaccine acceptance, coverage, and mandates. JAMA. 2020;324(4):335–336 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Flu vaccination coverage, United States, 2018–19 influenza season. 2019. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm. Accessed July 28, 2020
- 3.Michiels B, Govaerts F, Remmen R, Vermeire E, Coenen S. A systematic review of the evidence on the effectiveness and risks of inactivated influenza vaccines in different target groups. Vaccine. 2011;29(49):9159–9170 [DOI] [PubMed] [Google Scholar]
- 4.Plans-Rubió P. The vaccination coverage required to establish herd immunity against influenza viruses. Prev Med. 2012;55(1):72–77 [DOI] [PubMed] [Google Scholar]
- 5.Bourassa KJ, Sbarra DA, Caspi A, Moffitt TE. Social distancing as a health behavior: county-level movement in the United States during the COVID-19 pandemic is associated with conventional health behaviors. Ann Behav Med. 2020;54(8):548–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020;1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown DJ, Hagger MS, Hamilton K. The mediating role of constructs representing reasoned-action and automatic processes on the past behavior-future behavior relationship. Soc Sci Med. 2020;258:113085. [DOI] [PubMed] [Google Scholar]
- 8.Ouellette JA, Wood W. Habit and intention in everyday life: the multiple processes by which past behavior predicts future behavior. Psychol Bull. 1998;124(1):54 [Google Scholar]
- 9.Aarts H, Verplanken B, Van Knippenberg A. Predicting behavior from actions in the past: repeated decision making or a matter of habit? J Appl Soc Psychol. 1998;28(15):1355–1374 [Google Scholar]
- 10.Sheeran P, Conner M. Degree of reasoned action predicts increased intentional control and reduced habitual control over health behaviors. Soc Sci Med. 2019;228:68–74 [DOI] [PubMed] [Google Scholar]
- 11.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci. 2007;8(3):206–213 [DOI] [PubMed] [Google Scholar]
- 12.Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Pers Soc Psychol Rev. 2004;8(3):220–247 [DOI] [PubMed] [Google Scholar]
- 13.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211 [Google Scholar]
- 14.Schwarzer R, Hamilton K. Changing behaviour using the health action process approach. Handb Behav Change. 2020;89–103 [Google Scholar]
- 15.Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149–207 [DOI] [PubMed] [Google Scholar]
- 16.Juraskova I, O’Brien M, Mullan B, Bari R, Laidsaar-Powell R, McCaffery K. HPV vaccination and the effect of information framing on intentions and behaviour: an application of the theory of planned behaviour and moral norm. Int J Behav Med. 2012;19(4):518–525 [DOI] [PubMed] [Google Scholar]
- 17.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst Rev. 2018;1:CD003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milkman KL, Beshears J, Choi JJ, Laibson D, Madrian BC. Using implementation intentions prompts to enhance influenza vaccination rates. Proc Natl Acad Sci USA. 2011;108(26):10415–10420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics. 2017;139(1):e20161764. [DOI] [PMC free article] [PubMed] [Google Scholar]