Abstract
Diabetes, a disease with high prevalence in China, is a major risk factor of cardiovascular disease. Hesperidin is a flavanone glycoside with anti-hyperglycemic and anti-hyperlipidemic activities. Therefore, the present study aimed to investigate the potential preventive effect of hesperidin against type 2 diabetes mellitus (T2DM) using a rat model of alloxan and high fat diet (HFD)-induced insulin resistance. Male Sprague Dawley rats were orally administered with 100 mg/kg hesperidin or vehicle (sodium carboxy methyl cellulose) for 35 days. Insulin resistance was induced by feeding animals a HFD for 3 weeks (from day 7) and then with an alloxan injection on day 28. Results from the in vivo study demonstrated that hesperidin improved fasting serum glucose (from 19.8 to 10.6 mmol/l) without changing the fasting insulin level, suggesting that hesperidin prevented the development of insulin resistance and diabetes by improving insulin sensitivity. In the oral glucose tolerance test, the development of impaired glucose tolerance was also prevented by hesperidin treatment. Hesperidin was found to regulate glycolysis and gluconeogenesis by enhancing the activity of glucokinase, inducing the phosphorylation of insulin receptor (IR) and phosphoinositide-dependent kinase 1 (PDK1), while decreasing the activity of glucose-6-phosphatase and phosphoenolpyruvate carboxykinase in the liver. In a cell-based assay, hesperidin increased glucose uptake in primary rat adipocytes. Collectively, the present study identified the potent preventive effect of hesperidin against HFD-induced insulin resistance by activating the IR/PDK1 pathway. The current results may provide a potential strategy lacking sides effects to improve metabolic health and reduce risks.
Keywords: type 2 diabetes mellitus, insulin resistance, animal model, glucose uptake
Introduction
Diabetes mellitus (DM) is a group of metabolic diseases characterized by hyperglycemia, which is caused by impaired insulin secretion or dysregulated biological function, or both (1). DM is the leading risk factor of cardiovascular disease, which has the highest mortality rate in China (2,3). Moreover the prevalence of diabetes and prediabetes among the Chinese population increased substantially from 9.7 and 15.5% in 2010 to 11.6 and 50.1% in 2013, respectively (3,4). Thus, developing a strategy for disease control in diabetes at the prediabetic stage is urgently required (5,6).
Insulin resistance is a pathological condition in which cells fail to respond physiologically to the hormone insulin, leading to excess secretion of insulin as compensation to maintain the stability of blood glucose, eventually accelerating the development of type 2 DM (T2DM) (7,8). Targeting insulin resistance has been used as a first line strategy to treat diabetes (2). The insulin receptor (IR) is a tetramer, which consists of two α subunits and two β subunits connected via disulfide bonds. The α subunit is extracellular and presents binding sites of insulin, while the β subunit is composed of a transmembrane domain and a intracellular kinase domain, acting as a signal transducer (9,10). By binding to IR, the PI3K-dependent signaling pathway is initiated, which leads to the recruitment and interaction of the IR substrate and PI3K, eventually resulting in the activation of AKT via phosphoinositide-dependent kinase 1 (PDK1) (9,10).
In traditional Chinese medicine (TCM) theory, herbs such as Polygonatum odoratum, Pueraria lobata and Astragalus membranaceus, are considered as treatments of diabetes for 1,000s of years (11), and demonstrate fewer side effects compared with conventional medicine (12,13). In plants, various bioflavonoids have been reported to mitigate hyperglycemia or diabetes (14-17). Hesperidin is a flavanone glycoside that abundantly exists in lemon and sweet orange (18). Previous studies have revealed anti-hyperglycemic and anti-hyperlipidemic effects of hesperidin in diabetic rats, but the molecular mechanism remains unknown (19-22). The present study aimed to investigate the potential preventive effect of hesperidin against T2DM using a rat model of alloxan and high fat diet (HFD)-induced insulin resistance. Furthermore, the current study examined the underlying molecular mechanism via which hesperidin improved glucose metabolism by activating the IR/PDK1 pathway.
Materials and methods
Reagents
Hesperidin was purchased from Sigma-Aldrich (Merck KGaA), and was suspended in 0.5% sodium carboxy methyl cellulose (CMC-Na) for animal study or DMSO for cell-based assay.
Glucose uptake assay
Healthy rat subcutaneous adipocytes were isolated as previously described (23) and cultured in DMEM (Gibco; Thermo Fisher Scientific, Inc.) with 10% FBS (Gibco; Thermo Fisher Scientific, Inc.) at 37˚C in a humidified 5% CO2 atmosphere. The cells were treated with 3, 10, 30 or 100 µg/ml hesperidin at 37˚C and subsequently incubated without-serum at 37˚C overnight. Following the treatment, 1 nM insulin (Sigma-Aldrich; Merck KGaA) and a cocktail containing 2-deoxyglucose and 3H-2-deoxyglucose were applied to the cells and incubated at 37˚C for 2 h. Cytochalasin B (10 μM; Sigma-Aldrich; Merck KGaA) served as non-specific 2-deoxyglucose uptake to account for non-insulin induced glucose uptake under the same conditions. Cells were then washed and lysed. Glucose uptake was measured using Tri-Carb Liquid Scintillation Counter (PerkinElmer, Inc.) as counts per well and calculated by setting 0% as the effect of 1 nM insulin (negative control) and 100% as the effect of 100 nM insulin (positive control).
Animals and insulin resistance model
A total of 24 male Sprague Dawley rats (weight, 150-200 g; age, 6-7 weeks) were purchased from Vital River Laboratories, Co., Ltd., and housed in a temperature and humidity-controlled room (22-23˚C; 45-65%; 12 h light/dark cycle) with free access to food and water. Rats were administered either a HFD or a standard rat chow (control diet; Vital River Laboratories Co., Ltd.). All animals received humane care, and all experimental protocols were approved by Institutional Animal Care and Use Committee of Heilongjiang University of Chinese Medicine.
The insulin resistance model was induced following the protocol approved by China Food and Drug Administration (24). After 1-week acclimation with the control diet, the rats were divided into three groups (n=8 per group), including naïve group, model group and hesperidin group. The naïve and model groups were orally administered with vehicle (CMC-Na; 5 ml/kg) for 35 days, while the hesperidin group was treated with 100 mg/kg hesperidin for the same period. After being fed with control diet for 1 week, both model and hesperidin groups were given HFD for another 3 weeks. Then, they were fasted for 24 h with free access to water prior to intraperitoneal injection of alloxan (103-105 mg/kg; Sigma-Aldrich; Merck KGaA). HFD was given for another 3-5 days after the injection. At the end of the model establishment, an oral glucose tolerance test (OGTT) was performed before the animals were sacrificed via CO2 euthanasia. Samples of blood (1 ml), liver and epididymal adipose tissue were collected for further analysis.
OGTT
After fasting for 3-4 h, the rats were administered 2.5 g/kg glucose via oral gavage. Then, drop blood (15 µl) was sampled via the tail vein at 0, 15, 30, 60, 90 and 120 min post-glucose challenge, after which blood glucose was determined using a glucometer (ACCU-CHEK; Roche Diabetes Care, Inc.). The area under curve (AUC) was calculated using GraphPad Prism 6.0 (GraphPad Software, Inc.).
Biochemistry analysis
The serum levels of glucose (cat. no. F006-1-1), insulin (cat. no. H203), triglyceride (TG; cat. no. F001-1-1), total cholesterol (TC; cat. no. F002-1-1) and free fatty acid (FFA; cat. no. A042-2-1) were determined with commercially available kits from Nanjing Jiancheng Bioengineering Institute, according to the manufacturer's instructions.
Hepatic enzyme activity assay
Glucokinase activity was determined as described by Davidson and Arion (25). Liver samples were homogenized in buffer containing 50 mmol/l Tris-HCl (pH 7.4), 100 mmol/l KCl, 10 mmol/l mercaptoethanol and 1 mmol/l EDTA (Sigma-Aldrich; Merck KGaA). Homogenates were centrifuged at 100,000 x g at 4˚C for 1 h before the post-microsomal supernatant was used for the spectrophotometric continuous assay (Thermo Fisher Scientific, Inc.), in which the formation of glucose-6-phosphate from glucose at 27˚C for 1 h was coupled to its oxidation by glucose-6-phosphate dehydrogenase and NAD. Glucose-6-phosphatase activity was determined in the hepatic microsome using a spectrophotometric assay developed by Alegre et al (26). The reaction mixture contained 100 mmol/l sodium HEPES, 26.5 mmol/l glucose-6-phospate, 1.8 mmol/l EDTA, 2 mmol/l NADP+, 0.6 kIU/l mutarotase and 6 kIU/l glucose dehydrogenase. Phosphoenolpyruvate carboxykinase activity was measured using the spectrophotometric assay developed by Bentle and Lardy (27). The reaction mixture contained 50 mmol/l sodium HEPES, 1 mmol/l IDP, 1 mmol/l MnCl2, 1 mmol/l dithiothreitol, 0.25 mmol/l NADH, 2 mmol/l phosphoenolpyruvate, 50 mmol/l NaHCO3 and 7.2 U malic dehydrogenase. The enzyme activity was measured at 25˚C for 1 h, based on a decrease in the absorbance at 340 nm using a microplate reader (Thermo Fisher Scientific, Inc.).
Western blotting
Protein extracted from adipose tissue using RIPA lysis buffer (Beyotime Institute of Biotechnology) for 30 min, and then boiled with 5X loading buffer (Beyotime Institute of Biotechnology). Total protein was quantified using a bicinchoninic acid assay and 50 µg protein was separated via 12% SDS-PAGE. The separated proteins were transferred to PVDF membranes before being blocked with 5% non-fat dry milk in TBT-0.1% Tween-20 for 1 h at room temperature. The PVDF membrane was then incubated with primary antibodies of IR (cat. no. 23413; 1:1,000), phosphorylated (p)-IR (cat. no. 2969; 1:1,000), PDK1 (cat. no. 13037; 1:1,000,) p-PDK1 (cat. no. 3438; 1:1,000) or GAPDH (cat. no. 5174; 1:1,000; each, Cell Signaling Technology.) overnight at 4˚C. Horseradish peroxidase (HRP)-conjugated anti-mouse IgG (cat. no. 7076; 1:2,000) and HRP-conjugated anti-rabbit IgG antibodies (cat. no. 7074; 1:2,000; Cell Signaling Technology, Inc.) were then added and incubated for 2 h at room temperature, after which the horseradish peroxidase-conjugated protein was detected using a chemiluminescent horseradish peroxidase substrate solution (EMD Millipore). The specificity of the p-IR antibody was Tyr1150/1151, and the specificity of the p-PDK1 antibody was Ser241. The expression of protein was quantified using Image-Pro Plus software (version 6.0; Media Cybernetics, Inc.).
Statistical analysis
Quantitative data are presented as the mean ± SD, and were analyzed using GraphPad Prism 6.0 (GraphPad Software, Inc.). Differences between groups were analyzed using a two-way repeated measures ANOVA for OGTT, or one-way ANOVA with Tukey's or Dunnett's multiple comparison test for other studies. P<0.05 was considered to indicate a statistically significant difference. Experiments were repeated ≥3 times.
Results
Hesperidin prevents hyperglycemia in diabetic rats without changing insulin level
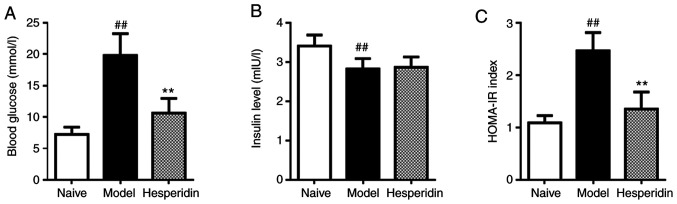
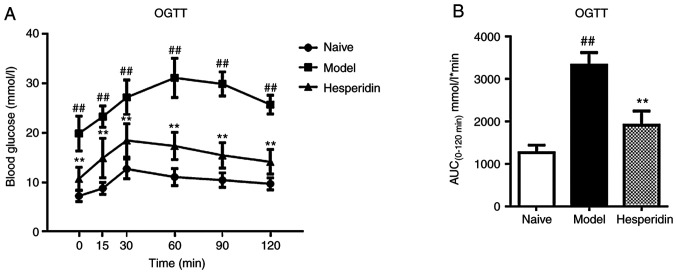
In order to examine the preventive effect of hesperidin on diabetes, a rat model of insulin resistance was induced using alloxan and HFD, which can mimic the natural progress of diabetes. After model induction, compared with the naïve group, the level of fasting blood glucose was significantly increased from 7.2 to 19.8 mmol/l (Fig. 1A), while the insulin level was decreased from 3.4 to 2.8 mIU/l (Fig. 1B), causing the insulin resistance index to almost double (Fig. 1C). In addition, OGTT demonstrated that the levels of blood glucose at different time points after glucose challenge were significantly increased compared with the naïve group (Fig. 2A). The AUC was increased by 160% compared with naïve group (Fig. 2B).
Figure 1.
Effect of hesperidin on blood glucose and insulin levels. Rats were treated with alloxan and high fat diet to induce diabetes before blood was sampled to determine (A) blood glucose and (B) insulin levels. (C) Insulin resistance index was assessed using the HOMA-IR = fasting glucose (mmol/l) x fasting insulin (mIU/ml)/22.5. Data are presented as the mean ± SD, n=8. ##P<0.01 vs. naïve group; **P<0.01 vs. model group. HOMA-IR, homeostasis model assessment-insulin resistance.
Figure 2.
Effect of hesperidin on OGTT results. At the end of the model establishment, rats were administered 2.5 g/kg glucose via oral gavage with before blood was sampled at 0, 15, 30, 60, 90 and 120 min post-glucose challenge. (A) Blood glucose levels during OGTT. (B) AUC calculated using GraphPad Prism. Data are presented as the mean ± SD, n=8. ##P<0.01 vs. naïve group; **P<0.01 vs. model group. OGTT, Oral glucose tolerance test; AUC, Area under the curve.
In diabetic rats, 100 mg/kg hesperidin significantly reduced blood glucose level from 19.8 to 10.6 mmol/l compared with the model group (Fig. 1A). Furthermore, compared with the model group, blood glucose levels at different time points after glucose challenge were significantly reduced, with the AUC value decreasing by 42% (Fig. 2), but blood insulin levels remained similar (Fig. 1B). These effects led to a decrease in the insulin resistance index in the hesperidin group compared with the model group (Fig. 1C), suggesting that hesperidin may alleviate hyperglycemia by improving insulin sensitivity. Therefore, the results indicated that hesperidin prevented hyperglycemia after 5-week-treatment in diabetic rats, suggesting possible diabetes prevention using a natural product.
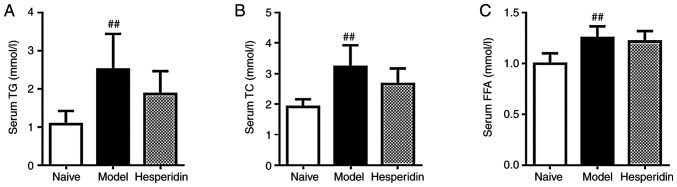
Hesperidin has no significant effect on lipid metabolism
The levels of TG, TC and FFA were significantly elevated in the model group compared with the naïve group, indicating dysfunctional lipid metabolism in this model (Fig. 3). Hesperidin treatment did not alter TG, TC or FFA levels compared with the model group, indicating that hesperidin had limited efficacy in improving lipid metabolism (Fig. 3).
Figure 3.
Effect of hesperidin on TG, TC and FFA levels. At the end of the model establishment, blood samples were collected for determination of the serum levels of (A) TG, (B) TC and (C) FFA. Data are presented as the mean ± SD, n=8. ##P<0.01 vs. naïve group. TG, triglyceride; TC, total cholesterol; FFA, free fatty acid.
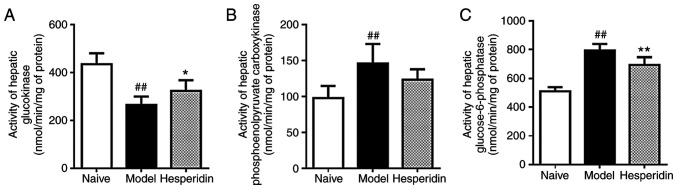
Role of hesperidin on glucose regulating enzymes
In the liver, significant glucokinase activity, glucose-6-phosphatase and phosphoenolpyruvate carboxykinase were identified between the naïve group and the model group (Fig. 4). Hesperidin induced glucokinase activity, but decreased the activity of glucose-6-phosphatase and phosphoenolpyruvate carboxykinase compared with the model group (Fig. 4), which are vital hepatic glucose regulating enzymes involved in glycolysis and gluconeogenesis (28).
Figure 4.
Effect of hesperidin on the activity of glucose regulating enzymes. Activities of (A) hepatic glucokinase, (B) glucose-6-phosphatase and (C) phosphoenolpyruvate carboxykinase were analyzed using enzyme and substrate system, and data were recorded via a colorimetric method. Data are presented as the mean ± SD, n=8. ##P<0.01 vs. naïve group; **P<0.01 vs. model group; *P<0.05 vs. model group.
Hesperidin improves insulin sensitivity by activating the insulin receptor pathway
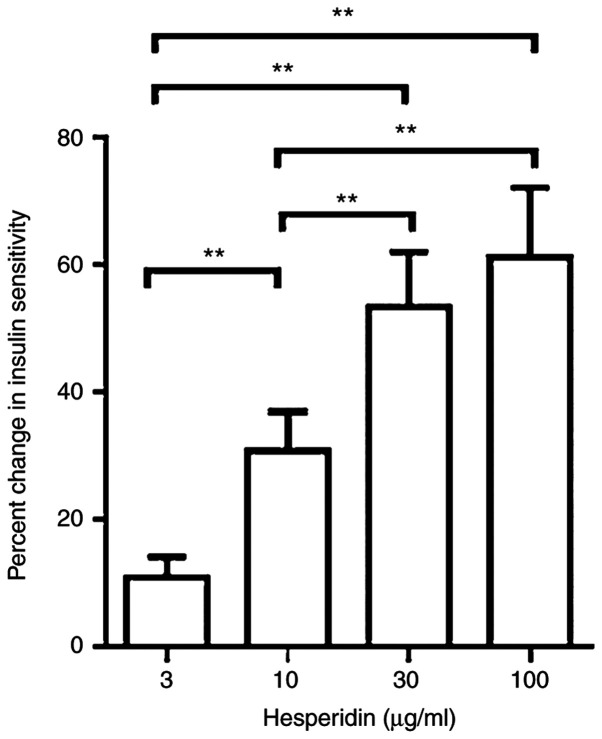
In the glucose uptake assay, a significant dose-dependent effect was observed, in which 3, 10, 30 and 100 µg/ml hesperidin increased insulin sensitivity by 11, 31, 54 and 61%, respectively, compared with the negative control (Fig. 5).
Figure 5.
Effects of hesperidin on glucose uptake. Primary rat adipocytes were starved before glucose uptake was initiated with the addition of a cocktail containing 2-deoxyglucose and 3H-2-deoxyglucose and allowed to incubate with test articles for 2 h. Data were measured and calculated by setting 0% as the effect of 1 nM insulin and 100% as the effect of 100 nM insulin. Differences between groups were analyzed using one-way ANOVA with Tukey’s multiple comparison test. Data are presented as the mean ± SD, n=8. **P<0.01.
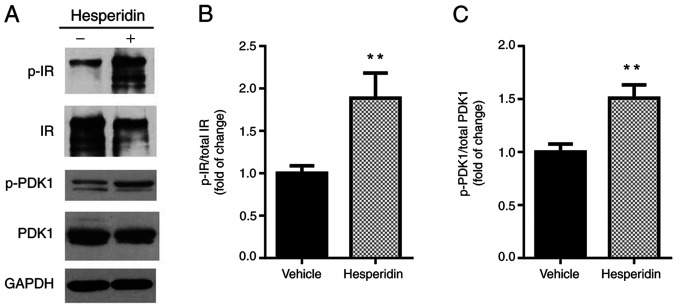
Western blot analysis was conducted to investigate the underlying molecular mechanism via which hesperidin regulated insulin sensitivity. The total expression levels of IR and PDK1 were not changed after hesperidin treatment, but the phosphorylation of these proteins was significantly increased by 89 and 51%, respectively (Fig. 6). Collectively, these findings suggested that hesperidin may improve insulin sensitivity by activating the IR/PDK1 pathway.
Figure 6.
IR/PDK1 involved mechanism in the protective effects of hesperidin. At the termination of animal study, fat tissues were collected for western blot analysis. GAPDH was used as the loading control. All expression data were normalized to GAPDH. (A) Representative blot. Statistical analysis of (B) IR and (C) PDK1 expression levels. Data are presented as the mean ± SD. Experiments were repeated ≥3 times. **P<0.01 vs. vehicle group. IR, insulin receptor; PDK1, phosphoinositide-dependent kinase 1; p-, phosphorylated.
Discussion
Previous studies have reported antidiabetic effects of hesperidin in HFD + streptozocin rats, Goto-Kakizaki rats and C57BL/KsJ-db/db mice (19-22). The present study established a diabetic rat model using HFD and alloxan, which represents a closer mimic of the pathogenesis of insulin resistance (24). Moreover, this model is well-established and recommended by the China Food and Drug Administration to evaluate the efficacies of TCM (29,30). Homeostatic model assessment (HOMA) is a widely reported method to quantify insulin resistance (31). The cut-off values in the current study of HOMA-insulin resistance may be utilized for identifying insulin resistance, indicating the clinical and epidemiological importance (32). In addition, according to the Experimental Methodology of Pharmacology (4th edition), rats with fasting blood glucose level of >16.7 mmol/l are considered as diabetic rats (33). The present study successfully induced insulin resistance in the model with an increased fasting blood glucose level (19.8 mmol/l) and HOMA-insulin resistance (2.5) in the model group. It was identified that hesperidin treatment significantly improved fasting blood glucose and oral glucose tolerance, but had limited effects on TG, TC and FFA levels, suggesting its antidiabetic functionality was exerted exclusively by regulating glucose metabolism.
Hyperglycemia may be attributed to decreased hepatic glycogen synthesis and increased hepatic glucose production, which may be the result of decreased glucokinase activities and increased glucose-6-phosphatase and phosphoenolpyruvate carboxykinase activities in a diabetic state (34,35). Hepatic glucokinase can be the most sensitive indicator of the glycolytic pathway in diabetes and its increase can accelerate the utilization of blood glucose for glycogen storage in the liver (36). Glucose-6-phosphatase and phosphoenolpyruvate carboxykinase are two critical enzymes in the metabolic pathway of gluconeogenesis to release glucose by the liver (37-39). In the current study, hesperidin induced glucokinase activity, while decreased the activities of glucose-6-phosphatase and phosphoenolpyruvate carboxykinase in liver to maintain glucose homeostasis.
If not transported across the cell membrane for further utilization, blood glucose will undergo glycolysis or aerobic oxidation in the circulating system (40). A commonly used approach to treat diabetes is to enhance glucose uptake (41). Hesperidin and naringin are glycosides of hesperitin and naringenin, sharing similar flavanone structures (18). Dhanya et al (42) observed a 2-fold increase in the uptake of fluorescent labeled glucose after naringin treatment in differentiated L6 myoblast, while Zygmunt et al (43) reported that naringenin stimulated glucose uptake in L6 myotubes in a dose- and time-dependent manner. The present study identified increased glucose uptake induced by 3-100 µg/ml hesperidin in rat subcutaneous adipocytes. However, in contrast, Yang et al (44) revealed that hesperetin decreased IR-phosphorylation and impaired glucose uptake in human breast cancer cells. Therefore, these flavanones and their glycosides may have complicated effects in different tissues or cells.
The IR signal pathway serves a key role in the regulation of glucose homeostasis (9,10). Molecular docking assays have been used to investigate the interaction between IR tyrosine kinase with individual flavonoids, and based on Autodock binding energies it was hypothesized that flavonones, such as hesperitin and naringenin, are potent activators of IR tyrosine kinase (45). However, there is lacking evidence from in vivo studies to support this hypothesis. The present study identified significantly increased phosphorylation of IR in adipose tissues after hesperidin treatment, as well as the enhanced phosphorylation of PDK1, which is a critical kinase responsible to transduce the signal from IR to AKT (46). Therefore, these findings suggest that hesperidin may prevent hyperglycemia and diabetes by activating the IR/PDK1 pathway.
In conclusion, the present study demonstrated the potent preventive effect of hesperidin using a rat model of alloxan and HFD-induced insulin resistance, as well as identified the underlying mechanism via which hesperidin alleviated hyperglycemia by activating the IR/PDK1 signaling pathway. Considering the increasing diabetic population and the fewer side effects of natural products, hesperidin administration may be an effective strategy for preventing diabetes and alleviating hyperglycemia.
Acknowledgements
Not applicable.
Funding
This work was supported by the General Program of National Natural Science Foundation of China (grant no. 81573935), Scientific and Technological Projects of Educational Bureau of Heilongjiang Province (grant no. 12531604) and Research and Development Program of Application Technology of Harbin (Out Standing Academic Leader; Category B; grant no. 2015RAXYJ053).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
LL and DZ designed the study. PP, JJ and GZ acquired the data. PP, YS and YH analyzed the data. PP and DZ drafted the manuscript. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
The present study and all animal experiments were approved by the Ethics Committee Institutional Animal Care and Use Committee of Heilongjiang University of Chinese Medicine.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Elizabeth MM, Alarcon-Aguilar J F, Clara OC, Escobar-Villanueva , Carmen M. Pancreatic β-cells and type 2 diabetes development. Curr Diabetes Rev. 2017;13:108–121. doi: 10.2174/1573399812666151020101222. [DOI] [PubMed] [Google Scholar]
- 2.2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40 (Suppl 1):S11–S24. doi: 10.2337/dc17-S005. American Diabetes Association. [DOI] [PubMed] [Google Scholar]
- 3.Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, et al. 2010 China Noncommunicable Disease Surveillance Group: Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 4.Yang SH, Dou KF, Song WJ. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:2425–2426. doi: 10.1056/NEJMoa0908292. author reply 2426. [DOI] [PubMed] [Google Scholar]
- 5.Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, Li Y, Zhao Z, Qin X, Jin D, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317:2515–2523. doi: 10.1001/jama.2017.7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang L, Shao J, Bian Y, Wu H, Shi L, Zeng L, Li W, Dong J. Prevalence of type 2 diabetes mellitus among inland residents in China (2000-2014): A meta-analysis. J Diabetes Investig. 2016;7:845–852. doi: 10.1111/jdi.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, Mori Y, Ide T, Murakami K, Tsuboyama-Kasaoka N, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001;7:941–946. doi: 10.1038/90984. [DOI] [PubMed] [Google Scholar]
- 8.DeFronzo RA, Ferrannini E. Insulin resistance A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991;14:173–194. doi: 10.2337/diacare.14.3.173. [DOI] [PubMed] [Google Scholar]
- 9.Leto D, Saltiel AR. Regulation of glucose transport by insulin: Traffic control of GLUT4. Nat Rev Mol Cell Biol. 2012;13:383–396. doi: 10.1038/nrm3351. [DOI] [PubMed] [Google Scholar]
- 10.Pollak M. The insulin and insulin-like growth factor receptor family in neoplasia: An update. Nat Rev Cancer. 2012;12:159–169. doi: 10.1038/nrc3215. [DOI] [PubMed] [Google Scholar]
- 11.Zhang H, Tan C, Wang H, Xue S, Wang M. Study on the history of Traditional Chinese Medicine to treat diabetes. Eur J Integr Med. 2010;2:41–46. [Google Scholar]
- 12.Calixto JB. Efficacy, safety, quality control, marketing and regulatory guidelines for herbal medicines (phytotherapeutic agents) Braz J Med Biol Res. 2000;33:179–189. doi: 10.1590/s0100-879x2000000200004. [DOI] [PubMed] [Google Scholar]
- 13.Valli G, Giardina EG. Benefits, adverse effects and drug interactions of herbal therapies with cardiovascular effects. J Am Coll Cardiol. 2002;39:1083–1095. doi: 10.1016/s0735-1097(02)01749-7. [DOI] [PubMed] [Google Scholar]
- 14.Ong KC, Khoo HE. Insulinomimetic effects of myricetin on lipogenesis and glucose transport in rat adipocytes but not glucose transport translocation. Biochem Pharmacol. 1996;51:423–429. doi: 10.1016/0006-2952(95)02195-7. [DOI] [PubMed] [Google Scholar]
- 15.Hsu FL, Liu IM, Kuo DH, Chen WC, Su HC, Cheng JT. Antihyperglycemic effect of puerarin in streptozotocin-induced diabetic rats. J Nat Prod. 2003;66:788–792. doi: 10.1021/np0203887. [DOI] [PubMed] [Google Scholar]
- 16.Choi JS, Yokozawa T, Oura H. Improvement of hyperglycemia and hyperlipemia in streptozotocin-diabetic rats by a methanolic extract of Prunus davidiana stems and its main component, prunin. Planta Med. 1991;57:208–211. doi: 10.1055/s-2006-960075. [DOI] [PubMed] [Google Scholar]
- 17.Shisheva A, Shechter Y. Quercetin selectively inhibits insulin receptor function in vitro and the bioresponses of insulin and insulinomimetic agents in rat adipocytes. Biochemistry. 1992;31:8059–8063. doi: 10.1021/bi00149a041. [DOI] [PubMed] [Google Scholar]
- 18.Garg A, Garg S, Zaneveld LJ, Singla AK. Chemistry and pharmacology of the Citrus bioflavonoid hesperidin. Phytother Res. 2001;15:655–669. doi: 10.1002/ptr.1074. [DOI] [PubMed] [Google Scholar]
- 19.Jung UJ, Lee MK, Jeong KS, Choi MS. The hypoglycemic effects of hesperidin and naringin are partly mediated by hepatic glucose-regulating enzymes in C57BL/KsJ-db/db mice. J Nutr. 2004;134:2499–2503. doi: 10.1093/jn/134.10.2499. [DOI] [PubMed] [Google Scholar]
- 20.Akiyama S, Katsumata S, Suzuki K, Nakaya Y, Ishimi Y, Uehara M. Hypoglycemic and hypolipidemic effects of hesperidin and cyclodextrin-clathrated hesperetin in Goto-Kakizaki rats with type 2 diabetes. Biosci Biotechnol Biochem. 2009;73:2779–2782. doi: 10.1271/bbb.90576. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed OM, Mahmoud AM, Abdelmoneim A, Ashour MB. Antidiabetic effects of hesperidin and naringin in type 2 diabetic rats. Diabetol Croat. 2012;41:53–67. doi: 10.1016/j.jdiacomp.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Shi X, Liao S, Mi H, Guo C, Qi D, Li F, Zhang C, Yang Z. Hesperidin prevents retinal and plasma abnormalities in streptozotocin-induced diabetic rats. Molecules. 2012;17:12868–12881. doi: 10.3390/molecules171112868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu X, Motoshima H, Mahadev K, Stalker TJ, Scalia R, Goldstein BJ. Involvement of AMP-activated protein kinase in glucose uptake stimulated by the globular domain of adiponectin in primary rat adipocytes. Diabetes. 2003;52:1355–1363. doi: 10.2337/diabetes.52.6.1355. [DOI] [PubMed] [Google Scholar]
- 24. China Food and Drug Administration (CFDA): Technical standards for testing and assessment of health food. CFDA, 2003. [Google Scholar]
- 25.Davidson AL, Arion WJ. Factors underlying significant underestimations of glucokinase activity in crude liver extracts: Physiological implications of higher cellular activity. Arch Biochem Biophys. 1987;253:156–167. doi: 10.1016/0003-9861(87)90648-5. [DOI] [PubMed] [Google Scholar]
- 26.Alegre M, Ciudad CJ, Fillat C, Guinovart JJ. Determination of glucose-6-phosphatase activity using the glucose dehydrogenase-coupled reaction. Anal Biochem. 1988;173:185–189. doi: 10.1016/0003-2697(88)90176-5. [DOI] [PubMed] [Google Scholar]
- 27.Bentle LA, Lardy HA. Interaction of anions and divalent metal ions with phosphoenolpyruvate carboxykinase. J Biol Chem. 1976;251:2916–2921. [PubMed] [Google Scholar]
- 28.Nordlie RC, Foster JD. A retrospective review of the roles of multifunctional glucose-6-phosphatase in blood glucose homeostasis: Genesis of the tuning/retuning hypothesis. Life Sci. 2010;87:339–349. doi: 10.1016/j.lfs.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y, Li X, Xie C, Luo X, Bao Y, Wu B, Hu Y, Zhong Z, Liu C, Li M. Prevention effects and possible molecular mechanism of mulberry leaf extract and its formulation on rats with insulin-insensitivity. PLoS One. 2016;11(e0152728) doi: 10.1371/journal.pone.0152728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang Y, Dong H, Wang M, Zhang J. Quercetin isolated from Toona sinensis leaves attenuates hyperglycemia and protects hepatocytes in high-carbohydrate/high-fat diet and alloxan induced experimental diabetic mice. J Diabetes Res. 2016;2016(8492780) doi: 10.1155/2016/8492780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 32.Geloneze B, Vasques AC, Stabe CF, Pareja JC, Rosado LE, Queiroz EC, Tambascia MA. HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS) Arq Bras Endocrinol Metabol. 2009;53:281–287. doi: 10.1590/s0004-27302009000200020. BRAMS Investigators. [DOI] [PubMed] [Google Scholar]
- 33.Wei W, Wu XM. Li: Experimental Methodology of Pharmacology. 4th edition. People's Medical Publishing House, Beijing, 2010 (In Chinese). [Google Scholar]
- 34.DeFronzo RA. Lilly lecture 1987. The triumvirate: Beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes. 1988;37:667–687. doi: 10.2337/diab.37.6.667. [DOI] [PubMed] [Google Scholar]
- 35.Reaven GM. Pathophysiology of insulin resistance in human disease. Physiol Rev. 1995;75:473–486. doi: 10.1152/physrev.1995.75.3.473. [DOI] [PubMed] [Google Scholar]
- 36.Iynedjian PB, Gjinovci A, Renold AE. Stimulation by insulin of glucokinase gene transcription in liver of diabetic rats. J Biol Chem. 1988;263:740–744. [PubMed] [Google Scholar]
- 37.Massillon D, Chen W, Barzilai N, Prus-Wertheimer D, Hawkins M, Liu R, Taub R, Rossetti L. Carbon flux via the pentose phosphate pathway regulates the hepatic expression of the glucose-6-phosphatase and phosphoenolpyruvate carboxykinase genes in conscious rats. J Biol Chem. 1998;273:228–234. doi: 10.1074/jbc.273.1.228. [DOI] [PubMed] [Google Scholar]
- 38.Lochhead PA, Salt IP, Walker KS, Hardie DG, Sutherland C. 5-aminoimidazole-4-carboxamide riboside mimics the effects of insulin on the expression of the 2 key gluconeogenic genes PEPCK and glucose-6-phosphatase. Diabetes. 2000;49:896–903. doi: 10.2337/diabetes.49.6.896. [DOI] [PubMed] [Google Scholar]
- 39.Al-Quraishy S, Dkhil MA, Abdel Moneim AE. Anti-hyperglycemic activity of selenium nanoparticles in streptozotocin-induced diabetic rats. Int J Nanomedicine. 2015;10:6741–6756. doi: 10.2147/IJN.S91377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Govers R. Cellular regulation of glucose uptake by glucose transporter GLUT4. Adv Clin Chem. 2014;66:173–240. doi: 10.1016/b978-0-12-801401-1.00006-2. [DOI] [PubMed] [Google Scholar]
- 41.Natali A, Ferrannini E. Effects of metformin and thiazolidinediones on suppression of hepatic glucose production and stimulation of glucose uptake in type 2 diabetes: A systematic review. Diabetologia. 2006;49:434–441. doi: 10.1007/s00125-006-0141-7. [DOI] [PubMed] [Google Scholar]
- 42.Dhanya R, Arun KB, Nisha VM, Syama HP, Nisha P, Santhosh Kumar TR, Jayamurthy P. Preconditioning L6 muscle cells with naringin ameliorates oxidative stress and increases glucose uptake. PLoS One. 2015;10(e0132429) doi: 10.1371/journal.pone.0132429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zygmunt K, Faubert B, MacNeil J, Tsiani E. Naringenin, a citrus flavonoid, increases muscle cell glucose uptake via AMPK. Biochem Biophys Res Commun. 2010;398:178–183. doi: 10.1016/j.bbrc.2010.06.048. [DOI] [PubMed] [Google Scholar]
- 44.Yang Y, Wolfram J, Boom K, Fang X, Shen H, Ferrari M. Hesperetin impairs glucose uptake and inhibits proliferation of breast cancer cells. Cell Biochem Funct. 2013;31:374–379. doi: 10.1002/cbf.2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ganugapati J, Baldwa A, Lalani S. Molecular docking studies of banana flower flavonoids as insulin receptor tyrosine kinase activators as a cure for diabetes mellitus. Bioinformation. 2012;8:216–220. doi: 10.6026/97320630008216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen P, Alessi DR, Cross DAE. PDK1, one of the missing links in insulin signal transduction? FEBS Lett. 1997;410:3–10. doi: 10.1016/s0014-5793(97)00490-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.