Abstract
Background
The COVID-19 pandemic has led caregivers to modify patient healthcare, with a high impact on patients with chronic pain.
Aims
To map recommendations for the management of chronic pain patients during the COVID-19 pandemic and propose a workflow for the management of these patients.
Design
This was a scoping review.
Methods
The databases searched were PubMed, Embase, CINAHL, Scopus, Cochrane Library, and LILACS. The studies were examined by two independent reviewers. The disagreements between reviewers were resolved through discussion or with a third reviewer.
Results
We presented the results in the form of a table, a workflow, and a narrative summary. The search resulted in 13 studies selected for full reading, including one consensus, five guidance documents, two expert panels, one joint statement, two educational flyers, and two free comments. We considered new technologies, including telemedicine. Each pain service needs to establish a screening model, classifying patients according to corresponding severity. Particular attention should be given to patients who use opioids and are at risk of misusing them. Nonpharmacological approaches and pain education should be maintained, considering the use of telehealth.
Conclusions
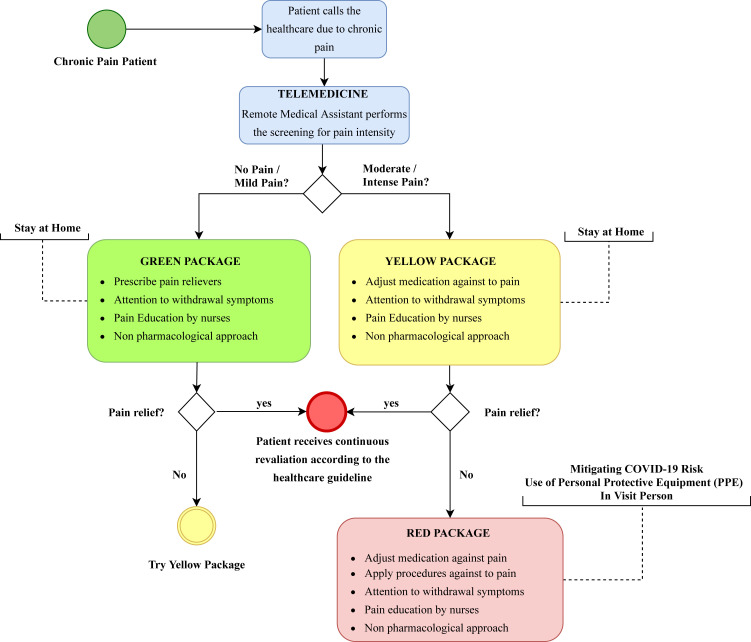
Recommendations for the management of chronic pain during COVID-19 include adjustments to the patient care model. The workflow proposes the use of telemedicine, screening for painful intensity, and the use of color-signaled intervention packages according to severity (green, yellow, and red).
Many countries have established public health measures implemented in response to the coronavirus disease 2019 (COVID-19) pandemic. For example, these measures have established a limit on how many people gather in public, helping to prevent the spread of COVID-19. Likewise, national and local health public authorities have temporarily suspended the public health services considered nonessential, including outpatient consultations and elective health procedures. The COVID-19 pandemic has affected the health monitoring services offered to patients with chronic diseases, worsening their symptoms or even their mental health (Adhikari et al., 2020; Borges do Nascimento et al., 2020; Jogalekar et al., 2020; Sohrabi et al., 2020).
In this context, the management of patients with chronic pain has been significantly affected. Chronic pain is prevalent worldwide and causes physical and psychological suffering. Factors associated with the chronic pain prevalence, such as agingcand the presence of other chronic diseases, match with the factors related to COVID-19, necessitating continuous health monitoring of the patient by a health professional essential during the pandemic (Adhikari et al., 2020; Larsson et al., 2017; Macfarlane, 2016; Mills, Nicolson, & Smith, 2019).
The treatment of the patient with chronic pain is complex and involves pharmacological and nonpharmacological therapies. Some of the medications for chronic pain, such as opioids and corticosteroids, can cause changes in the immune system, which can lead to infections such as COVID-19. Despite nonpharmacological therapies being essential to improving the quality of life of these patients, they have limitations when performed virtually. Psychological symptoms such as anxiety, depression, fear, catastrophizing, and suicidal thoughts tend to be exacerbated in times of crisis and tension, requiring greater attention (Gunnell et al., 2020; Miller, 2020; Solé et al., 2020).
Treatment interruptions for chronic pain patients due to the COVID-19 pandemic are creating a need for novel therapy alternatives using emergent technologies such as telemedicine. Many questions arise in this process: what criteria to use to perform the screening for virtual or face-to-face healthcare service for patients with chronic pain? How to monitor these patients in a telemedicine context? How to mitigate the risk of COVID-19 in cases of acute and chronic pain and the need for emergency procedures? What measures can minimize the psychological consequences of social isolation in patients who are already predisposed to anxiety and depression?
Caregivers hope to offer chronic pain patients therapy alternatives that have a lesser impact on treatment, ensuring the monitoring and control of pain and related symptoms. Scientific evidence containing guidelines for the management of patients with chronic pain during the COVID-19 pandemic is scarce in the literature. Preliminary searches on the Prospero website, PubMed, and Cochrane database have found an absence of protocols or reviews on the topic.
This scoping review gathers all the available evidence and makes it possible to identify gaps in the literature for new primary studies. The objective is mapping all recommendations on the management of chronic pain patients during the COVID-19 pandemic, and proposing a workflow for the management of such patients.
Review Question
What is known about chronic pain management during the COVID-19 pandemic?
Review Methods
Design
A scoping review was conducted through the JBI methodology for such reviews (Peters et al., 2020) and Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR; McGowan et al., 2020; Tricco et al., 2018).
Inclusion and Exclusion Criteria
Publications that met the inclusion criteria were those on the management of patients with chronic pain during the COVID-19 pandemic. For this scoping review, studies published after the pandemic (December 2019) were included. All primary research studies, reviews, meta-analyses, guidelines, and texts published on society websites were considered. There was no language restriction.
Studies that addressed acute pain or chronic pain outside the context of the COVID-19 pandemic were excluded.
Data Sources
The databases searched were PubMed, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Cochrane Library, and Latin American and Caribbean Health Sciences Literature (LILACS). The search for unpublished literature included: sites for pain organizations, the World Health Organization (WHO), the Agency for Research and Quality in Health, the Institute for Healthcare Improvement, and the Digital Library in Network of Theses and Dissertations.
Search
The search strategy was as comprehensive as possible, to identify published and unpublished studies (gray literature). A three-step search strategy was used for this review. A limited initial search of PubMed and Embase was carried out, followed by analysis of the words contained in the title and abstract and in the terms of the index used to describe the article. A complete secondary search was performed on all databases included, using the keywords and index terms identified in the initial limited search. To help identify additional studies, we conducted a tertiary literature search by examining the reference lists for all studies included in this review. Appendix 1 shows the sensitive search strategies.
Selection of Sources of Evidence
After the searches, all citations were organized in a reference manager. The studies were examined by two independent reviewers based on the inclusion criteria for the review. The selected studies were retrieved for full-text review. Disagreements between reviewers at each stage of the study selection process were resolved through discussion or with a third reviewer.
Data Extraction and Items
Data from the articles were obtained using a data extraction tool developed by the reviewers. The extracted data includes the distribution of studies by year, author, title, type of publication, and content.
Synthesis of Results
The extracted data are presented in the form of a table, a workflow, and a narrative summary. We used a graphical representation for a workflow using symbols from Business Process Modeling Notation (BPMN) published by Object Management Group (OMG; Object Management Group, 2011; Ramos-Merino, Alvarez-Sabucedo, Santos-Gago, & Sanz-Valero, 2018).
Results
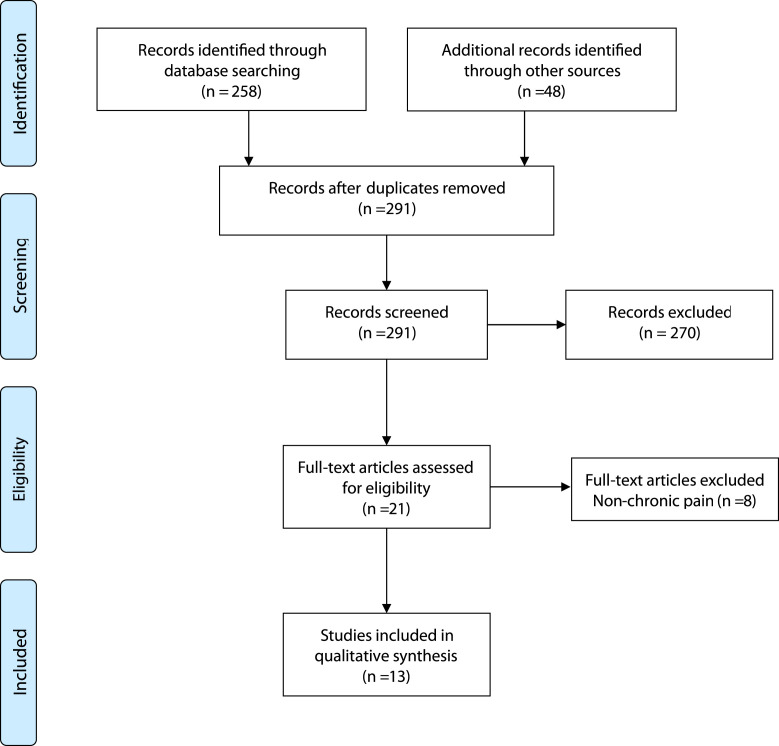
The results are presented in a PRISMA-ScR diagram flow (Fig. 1 ). The research resulted in 306 papers. After reading the title and abstract, we excluded 270 records for not meeting the inclusion criteria. The studies focused on acute pain as a symptom of COVID-19. After reading 26 studies eligible for full reading, we found that 13 studies met the inclusion criteria. Table 1 shows the characteristics of works featured. We selected one consensus, five guidance documents, two expert panels, one joint statement, two educational flyers, and two free comments, all published since 2020 due to the COVID-19 pandemic.
Figure 1.
Flow diagram.
Table 1.
Characteristics of Included Publications
| Year | Author | Title | Design and Type of Publication | Content |
|---|---|---|---|---|
| 2020 | Santhanna et al. | Caring for patients with pain during the COVID-19 pandemic | Expert opinion—consensus | Guidelines for informing doctors and healthcare professionals committed to caring for patients in pain during this period of crisis. |
| 2020 | Eccleston et al. | Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (e-health) pain management services | Narrative review—guidance | Guidance for the rapid transition to care, with discussions on the use of technology and the future of pain management centers. |
| 2020 | Cohen et al. | Pain Management Best Practices from Multispecialty Organizations during the COVID-19 Pandemic and Public Health Crises | Expert opinion—panel | Framework for pain practitioners and institutions to balance the often conflicting goals of risk mitigation for healthcare providers, risk mitigation for patients, conservation of resources, and access to pain management services. |
| 2020 | Song, et al. | Pain Management During the COVID-19 Pandemic in China: Lessons Learned | Experience report | Personal experiences of Chinese doctors and scientists working in the field of pain medicine in Wuhan, as well as in Shenzhen, seriously affected by COVID-19. |
| 2020 | Shanthanna, et al. | Recommendations on Chronic Pain Practice during the COVID-19 Pandemic | Expert opinion—joint statement | General recommendations about elective, semi-urgent and urgent pain procedures during the COVID-19 pandemic and pain medications. |
| 2020 | ASRA and ESRA | COVID-19 Guidance for Chronic Pain Patients | Gray literature - Educational flyer | Summary of recommendations. |
| 2020 | ASRA and collaborators | Chronic Pain Best Practice Guidelines | Gray literature—educational flyer | Summary of recommendations. |
| 2020 | Spine Interventional Society (SIS) | SIS Guidance on Interventional Pain Procedures During the COVID-19 Global Emergency | Gray literature—guidance on the website | Several steps to achieve goals for the U.S. healthcare system in response to COVID-19. |
| 2020 | Federacion Latinoamericana de Asociaciones para El Estudio del Dolor (FEDELAT) | Recomendacioes sobre La Practica de La Medicina Del Dolor Cronico en el Contexto de la Pandemia de COVID-19 | Gray literature—guidance on the website | Recommendations for consultations, emergency procedures, and need for hospitalization. |
| 2020 | Juan Antonio Micó Segura | COVID-19 coronavirus and chronic pain: uncertainties | Expert opinion—free comment | Reflections on the prevalence of chronic pain in the Spanish population and monitoring of patients during the COVID-19 pandemic. |
| 2020 | Editorial Board, Practical Pain Management Journal | Managing Pain and Related Symptoms during Coronavirus | Gray literature—guidance on the website | A few tips for clinicians on managing pain and related symptoms during coronavirus. |
| 2020 | Kathleen S. Brown and Daniel L. Bruns | Guidance on psychological assessment and management of chronic pain during the COVID-19 crisis | Gray literature—guidance on website, American Psychological Association (APA) | Guide to help psychologists understand the evidence base and practice recommendations for pain-related psychological assessment and interventions in a remote online format. |
| 2020 | American Pain Society regional division, Southern Pain Society | President's Column: Living with Chronic Pain During the Pandemic | Gray literature—free comment | Reflections on the limitations and difficulties of chronic pain patients during COVID-19. |
COVID-19 = coronavirus disease 2019.
In the consensus paper, the authors describe clinical guidelines focusing on caring for patients in pain during the pandemic. They discuss factors related to drugs that can affect the immune system, and thus make patients with chronic pain more predisposed to COVID-19 infection. It proposes therapeutic recommendations during consultations, the possibility of using telemedicine, biopsychosocial interventions and care during the performance of interventional procedures. The authors ultimately suggest a follow-up visit for the patient with chronic pain during the pandemic (Shanthanna et al., 2020a, 2020b).
Eccleston et al. discuss the emergency need for remote healthcare for patients with pain. Moreover, they explain concepts relating to the telemedicine approach. They present factors to consider about the prevention and control of chronic pain using telemedicine for consultations during the pandemic and highlight some evidence about the effectiveness and risks of using such technology (Eccleston et al., 2020).
Cohen et al. discuss risk mitigation in consultations and procedures during the COVID-19 crisis. The Veterans Health Administration and Armed Forces validated these recommendations. In these guidelines, the authors discuss the mitigation of general and specific intervention risks, patient flow problems and staffing plans, telemedicine options, screening recommendations, strategies to reduce psychological sequelae in healthcare providers, and resource use. They provide clinical guidelines for healthcare professionals’ mental health and screening workflows for the patients who could receive healthcare service using telemedicine (Cohen et al., 2020).
In some countries, public health services for patients with pain were interrupted temporarily, with caregivers focusing the available resources on helping patients with COVID-19 in a critical state. Healthcare professionals for patients in pain from Wuhan and Shenzhen, two provinces with high COVID-19 occurrences in China, had to reorganize their healthcare for a patient with high-intensity pain. They share their experiences related to screening patients during the pandemic. Patients were screened at different levels of care, considering the risk and symptoms of COVID-19. They were given prescription medications to manage their pain at home, along with necessary telemedicine support. Patients with severe pain or emergency conditions received immediate treatment at the clinic or were admitted for further tests and treatments (Song et al., 2020).
The American Society of Regional Anesthesia and Pain Medicine (ASRA) and the European Society for Regional Anesthesia and Pain Therapy (ESRA) have prepared a joint statement containing recommendations for the management of patients with chronic pain. The document proposes to classify the need for care and assess the patient for risk of contracting COVID-19. Another initiative by the ASRA and ESRA societies was the construction of two educational flyers focusing on COVID-19, containing a summary of the best evidence about the management of patients with chronic pain (Shanthanna et al., 2020a, 2020b).
Regarding interventional pain procedures, the Spine Intervention Society (SIS) published a guide for managing procedures for patients in pain during the COVID-19 pandemic. The guideline has six steps: (1) prioritize alternatives for personal assistance, (2) reschedule elective and non-urgent procedures, (3) prioritize procedures by performing a risk-benefit analysis, (4) prepare the environment for patients at risk of COVID-19, (5) use recommended personal protective equipment (PPE), (6) manage potential exposure (Spine Intervention Society, 2020).
The Latin American Federation of Associations for the Study of Pain (FEDELAT) published recommendations for practice in managing patients with pain, emphasizing outpatient consultations done through telemedicine, the need to prescribe pain drugs for an extended period, screening procedures for patients with symptoms of COVID-19, and urgent intervention procedures. The authors present scenarios of acute and chronic pain that requires hospitalization, showing guidance on the use of PPE and reduction of people in the patient's environment (Federación Latinoamericana de Associaciones para el Estudio del Dolor, 2020).
An article in the Journal of the Spanish Association for the Study of Pain (Micó Segura, 2020) described the impact of social distance on the wellness of patients with chronic pain. The author emphasizes that many patients with chronic pain are in the high-risk group due to aging or other comorbidities. The mental health of these patients is also compromised by social distance since anxiety and depression are common in patients with chronic pain (Micó Segura, 2020).
An editorial from the Journal of Practical Pain Management included some recommendations for patients with chronic pain during the pandemic. The authors emphasize the importance of effective communication between patients and healthcare professionals in the use of telemedicine. They also share some considerations about the use of opioids and management of anxiety in these patients, in addition to more strict hygiene measures adopted by pain clinics (PPM Editorial Board, 2020).
The American Psychological Association (APA) released guidelines on how to perform assessment and psychological intervention for patients with chronic pain during a pandemic using telemedicine as a resource. They emphasized teleneuropsychology, recognized by the APA as a practice with proven results. The guide highlights the main forms of psychological treatment used in a patient with pain, such as cognitive-behavioral therapy, relaxation techniques, mindfulness, and assessment using tools for anxiety, depression, fear, and catastrophic thoughts. They addressed questions about the use of opioids during the crisis, which should be discussed with the patient and a responsible team (American Psychological Association, 2020a, 2020b).
The Southern Pain Society, a regional division of the American Pain Society, published an article identifying the limitations that patients with chronic pain are facing in accessing integrative practices and discusses possibilities of the use of various technologies. They highlight the importance of pain education for patients as a useful tool during the pandemic (Quinlan-Colwell, 2020).
Workflow for the Management of Patients With Chronic Pain During COVID-19
This review built a workflow containing the main study recommendations. The workflow proposes that patients with chronic pain have access to telemedicine through telephone calls. During remote care, the provider treats the patient according to pain intensity. The patient is then classified by color, according to severity (green, yellow, or red). Patients without pain or with mild pain are considered elective and receive the green intervention package. Patients with moderate to severe pain are initially considered to be emergent and receive the yellow intervention package. If pain intensity worsens and pain medication fails to reduce it, the patient is considered urgent and receives the red intervention package. Urgent patients need to be assessed for risk of COVID-19 so caregivers can take infection prevention and control measures. The time for patient reassessment must follow the routine established in each service. The authors emphasize that the proposed flow must be adapted to the realities of the situation, respecting local government guidelines (Fig. 2 ).
Figure 2.
Workflow in the management of patients with chronic pain during the coronavirus disease 2019 pandemic.
Discussion
Risk Mitigation and Screening for Patients With Chronic Pain
The COVID-19 pandemic has affected the worldwide population and placed a burden on chronic pain patients. One of the most effective government measures to avoid saturating the public health system is social distancing, which, in the short term, results in changes in the work processes of health services, such as suspension of elective procedures and outpatient consultations (Brooks et al., 2020; Sohrabi et al., 2020).
Uncertainty, in the context of actions during a pandemic, occurs because of lack of information regarding the flow of patients, as well as lack of understanding and knowledge about a new disease, its consequences, and its probabilities of spreading. Healthcare professionals need to know how to mitigate risks in the planning of actions to ensure a flattening of the number of patients infected by COVID-19 (Anderson et al., 2020; Deng & Peng, 2020; Garfin et al., 2020; Hartley & Perencevich, 2020).
During the pandemic, patients in chronic pain need to be monitored by a multiprofessional team, even at a distance. At this moment, we need more rigor in the prevention and control of infection, to protect healthcare professionals and patients from the spread of the virus, especially during the asymptomatic phase of the disease, when there are no signs of contamination. Defining criteria for virtual or in-person services and assessing risks are fundamental steps for planning a good service flow (Cohen et al., 2020; Eccleston et al., 2020; Shanthanna et al., 2020a, 2020b).
Some authors suggest the previous classification of care as elective, emergent, and urgent to guide patient management during the pandemic (Shanthanna et al., 2020a, 2020b). In elective cases, the authors recommend postponing all procedures, and in cases of consultation, performing it through telemedicine. Cases considered emergent must be defined individually, considering the risks and benefits of the service and procedure. In urgent cases, the patient needs to be attended face-to-face and must be evaluated for the risk of COVID-19, taking appropriate protection and control measures to avoid the spread of disease (Shanthanna et al., 2020a, 2020b; Song et al., 2020).
Based on experience in China (Song et al., 2020), it is recommended that patients with chronic pain who need healthcare undergo strict control and be classified into levels of care based on pain intensity. The first level includes patients with mild to moderate pain, who have relatively clear etiopathogenesis with few comorbidities and are in good condition. This group was typically prescribed pain control drugs at home and telemedicine follow-up. Those who had close contact with diagnosed individuals or were suspected to have COVID-19 were placed under observation during quarantine at home. The second level included patients with mild to moderate pain, those who had symptoms like those of COVID-19, or those who had close contact with individuals diagnosed with COVID-19. The third level included patients in severe pain or undergoing emergencies, who received immediate care. Patients screened at levels 2 or 3 who had any symptoms or suspicion of COVID-19 were referred to an isolation ward for further testing and treatment (Song et al., 2020).
Patients with chronic pain deserve special attention in face-to-face care, as many are part of the group at high risk for COVID-19 since chronic pain is prevalent in the elderly and other comorbidities (Adhikari et al., 2020; Mills et al., 2019; Richardson et al., 2020). There is reason for concern about the worsening of symptoms related to chronic pain in patients infected with COVID-19 since this problem has already been observed in similar viral flus (Moldofsky & Patcai, 2011).
Patients should be transported directly to the place where they will receive treatment and avoid common areas. Ideally, there should be a separate place for the care of these patients, making it possible to disinfect the environment correctly. During all care, to prevent contamination, it is essential that their hands be properly washed, and that professionals avoid touching their face or any surface before cleaning (Cohen et al., 2020; Federación Latinoamericana de Associaciones para el Estudio del Dolor, 2020; Spine Intervention Society, 2020).
Use of Technologies to Monitor Patients With Chronic Pain During COVID-19
The current crisis, although devastating, has shown that health systems need to improve to continue their activities remotely. By immediately reorganizing with the least possible damage to chronic patients, healthcare institutions can advance the incorporation of new technologies into inpatient care. To support these changes, many regulatory measures have emerged with more flexibility. We can use a variety of video communication technologies, many of which are free or inexpensive, including tools from Google, Skype, Twitter, and Facebook (Calton et al., 2020; Ghosh et al., 2020; Hollander & Carr, 2020; Rufai & Bunce, 2020; Song et al., 2020).
Using technology for consultations and monitoring chronic pain symptoms allows patients in stable condition to remain in home isolation, reducing the risk of COVID-19 contamination. Telemedicine is an older term used to refer to technologies and telecommunications systems to administer healthcare to patients geographically separated from providers. When broadly referred to, all health care provided with the use of technologies can be called telehealth (Eccleston et al., 2020; Shanthanna et al., 2020a, 2020b).
These technologies must be used to offer the best possible experience for patients with chronic pain during the pandemic (Humphreys et al., 2020; Martínez-Sarriegui et al., 2011). The health professional, together with the patient, must establish virtual service hours, finding a quiet location with the fewest possible interruptions. Contact should occur regularly, with dates previously agreed with the patient. If possible, prioritize video calls so that there is eye contact. During the service, goals can be established to determine the objective to be met for the next meeting (Eccleston et al., 2020; Shanthanna et al., 2020a, 2020b; Song et al., 2020).
Telemedicine has been increasingly recognized as a valuable tool for healthcare professionals and patients, especially in crisis and disaster situations (Lurie & Carr, 2018). Telemedicine is considered the first healthcare approach in most cases. In the case of patients with chronic pain, telemedicine can be a valid strategy for outpatient follow-up even after the pandemic, as it presents excellent benefits relative to costs and satisfactory results in several studies (Humphreys et al., 2020; Lee et al., 2020; Martínez-Sarriegui et al., 2011; Song et al., 2020).
Other possibilities for the use of telemedicine can be monitoring of medication use, assessment of adherence to treatment, clinical control of interventional procedures, and carrying out of educational interventions by nurses, including guidance on the administration of medications and possible adverse reactions (Song et al., 2020).
Nursing pain education can help the patient to understand chronic pain and better cope with adverse impacts during social isolation. The patient is educated to identify harmful behaviors and to adopt more adaptive behaviors, with a positive impact in adherence to the care plan and response to treatment (Antunes et al., 2018).
Through videos with tutorials, it is also possible to contemplate other aspects of treatment such as psychotherapies, physical therapy, and physical exercise for pain relief (American Psychological Association, 2020a, 2020b; Federación Latinoamericana de Associaciones para el Estudio del Dolor dolor, 2020). In some cases, telemedicine can offer complementary support to home visits for patients who continuously use opioids and other drugs in an intrathecal pump or who have neuromodulation devices (Song et al., 2020).
Safety in the Prescription and Use of Medicines Chronic Pain During COVID-19
Regarding pharmacological treatments, it should be borne in mind that opioids, such as morphine or fentanyl, can have an immunosuppressive effect, an effect dependent on the dose and duration of administration. The immunosuppression produced can, in case of infection by COVID-19, favor a more severe form of the disease (Russell et al., 2020).
Buprenorphine, from animal studies, is reported as one of the opioids with the lowest magnitude of immunosuppressive effect (Boland & Pockley, 2018). In situations of high fever in patients using fentanyl patches, it should be remembered that there may be an increase in the drug's absorption, with the consequent risk of respiratory depression. The same precautions should be taken with patches of other drugs, such as buprenorphine, although the respiratory depressant effects are less than with fentanyl (Federación Latinoamericana de Associaciones para el Estudio del Dolor, 2020; Micó Segura, 2020; Shanthanna et al., 2020a, 2020b). Users of opioids may eventually require an in-person medical consultation to detect clinical elements of possible misuse of them (addictions, psychological profile, etc.; Degenhardt et al., 2019).
The use of nonsteroidal anti-inflammatory drugs has no interaction with COVID-19 infection, except for possible masking of the fever. The classic contraindications apply for the use of these drugs. There are no data to support the use of ibuprofen, despite the controversy that has surrounded it since the beginning of the crisis in Europe, with the argument that it would increase viral replication by interacting with the angiotensin-2 converting enzyme (MaassenVanDenBrink et al., 2020; Micó Segura, 2020; Shanthanna et al., 2020a, 2020b; Sodhi & Etminan, 2020).
The Latin American Federation of Associations for the Study of Pain approves of the repeated filling of prescriptions of controlled substances (opioids and psychotropics) for longer periods than usual, for 60 to 90 days, as is being practiced in several Latin countries, including through systems delivery, to reduce patient visits to the health center as much as possible (Federación, 2020). In Brazil, electronic prescriptions of controlled drugs, simple prescriptions, and medical reports were recently approved by the legislature, provided prescriptions are digitally validated (Ministério da Saúde, 2020).
Strategies to Minimize Negative Repercussions of Social Isolation in Patients With Chronic Pain
Emotional aspects and repercussions of social isolation need to be addressed during the pandemic, using a biopsychosocial model of pain management (Brooks et al., 2020; Micó Segura, 2020; Quinlan-Colwell, 2020). During the entire period of social isolation, it is essential that there be excellent communication between the team and the patient, so that patients feel safe with the treatment (PPM EditorialBoard, 2020).
The use of telehealth can promote more significant multidisciplinary interactions and facilitate the incorporation of desirablepractices by patients. Pain programs that integrate physical exercise, sleep hygiene, relaxation, and guidelines for a healthy lifestyle should be considered (Shanthanna et al., 2020a, 2020b). During follow-up, the use of positive reinforcement strategies, valuing the efforts made, serves as a motivational stimulus for the patient. Because of changes in treatment during the pandemic, it is essential for caregivers to develop a problem-solving technique around pain management. The approach must identify the causes and consequences of problems, and include solution planning (Eccleston et al., 2020).
Evidence exists that some cognitive-behavioral therapy approaches are effective for treatment of chronic pain performed remotely. During cognitive-behavioral therapy, patients who find themselves in a vicious cycle, with erroneous thoughts, catastrophizing pain, and dysfunctional behaviors such as kinesiophobia, are encouraged to substitute them for others that bring greater functionality (American Psychological Association, 2020a; Baez, Hoch, & Hoch, 2018).
Whenever possible, experimental learning should be included in the session; that is, working with the patient is a task that can help with pain control. Tasks can be hierarchical, starting with the simplest ones, and increasing in complexity as the patient gains self-confidence. Developing tasks helps the patient to re-establish a routine with daily activities that are meaningful to them. Functional gains, even if short, should be valued, and if the patient has space at home, they can take short daily walks. Complementary resources, such as books, websites, and other self-help materials, may be useful as a remote intervention (Eccleston et al., 2020).
A limitation of this review is that no primary studies on the topic were found due to the recent nature of the COVID-19 pandemic. The few publications reflect expert opinions and recommendations. Primary studies are needed evaluating the effects of COVID-19 on the clinical and therapeutic follow-up of patients with chronic pain and the appearance of pain secondary to an infection, as well as measuring the repercussions of social isolation on emotional aspects and quality of life of these patients. Future systematic reviews can be conducted to assess the effectiveness of telemedicine during the pandemic in patients with chronic pain.
Conclusions
This paper was the first review to address the management of patients with chronic pain during the COVID-19 pandemic. It proposes the organization of a workflow for the management of patients with chronic pain during COVID-19 using telemedicine care, screening for pain intensity, and intervention packages with color coding according to severity.
In conclusion, recommendations for the management of chronic pain during COVID-19 include adjustments to the patient care model. The use of technologies, especially telemedicine, was considered in the studies. Each pain service needs to establish a screening model, classifying patients according to severity. Urgent cases, which require face-to-face assistance, need to be treated in a way that minimizes the risk of COVID-19. Infection prevention and control measures must follow the recommended government guidelines. Particular attention should be given to patients who use opioids and are at risk of misuse. Nonpharmacological approaches and pain education should be maintained, considering the use of telehealth.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors wish the thank the Latin American Federation of Associations for the Study of Pain, Federal Fluminense University, Brazil, Federal University of Maranhão, Brazil, The Brazilian Centre for Evidence-based Healthcare: A JBI Centre of Excellence, and the National Institute of Traumatology and Orthopedics, Jamil Haddad, Brazil.
Footnotes
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.pmn.2020.11.010.
Supplementary Data
References
- Adhikari S.P., Meng S., Wu Y.J., Mao Y.P., Ye R.X., Wang Q.Z.…Zhou H. Epidemiology, causes, clinical manifestation and diagnosis, prevention, and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infectious Diseases of Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association (APA) Guidance on psychological assessment and management of chronic pain during the COVID-19 crisis. 2020. https://www.apaservices.org/practice/news/chronic-pain-covid-19 Retrieved from.
- American Psychological Association (APA) Pain management in a crisis. 2020. https://www.apaservices.org/practice/news/pain-management-covid-19 Retrieved from.
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antunes J.D.M., Daher D.V., Ferrari M.F.M., Pereira L.C.C.M., Faria M., Sveichtizer M.C.…Izidoro C. Práticas de enfermagem ao paciente com dor crônica: revisão integrativa. Acta Paulista de Enfermagem. 2018;31(6):681–687. [Google Scholar]
- Baez S., Hoch M.C., Hoch J.M. Evaluation of cognitive-behavioral interventions and psychoeducation implemented by rehabilitation specialists to treat fear-avoidance beliefs in patients with low back pain: A systematic review. Archives of Physical Medicine and Rehabilitation. 2018;99(11):2287–2298. doi: 10.1016/j.apmr.2017.11.003. [DOI] [PubMed] [Google Scholar]
- Borges do Nascimento I.J., Cacic N., Abdulazeem H.M., von Groote T.C., Jayarajah U., Weerasekara I.…Marcolino M.S. Novel coronavirus infection (COVID-19) in humans: A scoping review and meta-analysis. Journal of Clinical Medicine. 2020;9(4) doi: 10.3390/jcm9040941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boland J.W., Pockley A.G. Influence of opioids on immune function in patients with cancer pain: from bench to bedside. British Journal of Pharmacology. 2018;175(14):2726–2736. doi: 10.1111/bph.13903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. Journal of Pain Symptom Management. 2020 doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S.P., Baber Z.B., Buvanendran A., McLean L.T.C.B., Chen Y., Hooten W.M.…Phillips C.D.R.C. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Medicine. 2020 doi: 10.1093/pm/pnaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Grebely J., Stone J., Hickman M., Vickerman P., Marshall B.D.L.…Larney S. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 2019;394(10208):1560–1579. doi: 10.1016/S0140-6736(19)32229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng S.Q., Peng H.J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. Journal of Clinical Medicine. 2020;9(2) doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccleston C., Blyth F.M., Dear B.F., Fisher E.A., Keefe F.J., Lynch M.E.…Williams A.C.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020;161(5):889–893. doi: 10.1097/j.pain.0000000000001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federación Latinoamericana de Associaciones para el Estudio del Dolor Recomendaciones sobre la prática de la medicina del dolor cronico en el contexto de la pandemia de covid 19. 2020. http://fedelat.com/wp-content/uploads/2020/04/Fedelat-y-Covid-19-min.pdf Retrieved from.
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh P., Schwartz G., Narouze S. Twitter as a powerful tool for communication between pain physicians during COVID-19 pandemic. Regional Anesthesia and Pain Medicine. 2020 doi: 10.1136/rapm-2020-101530. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N.…Collaboration C.-S.P.R. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30171-1. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley D.M., Perencevich E.N. Public Health Interventions for COVID-19: Emerging evidence and implications for an evolving public health crisis. JAMA. 2020 doi: 10.1001/jama.2020.5910. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2003539. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Humphreys J., Schoenherr L., Elia G., Saks N.T., Brown C., Barbour S., Pantilat S.Z. Rapid implementation of inpatient telepalliative medicine consultations during COVID-19 pandemic. Journal of Pain Symptom Management. 2020 doi: 10.1016/j.jpainsymman.2020.04.001. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jogalekar M.P., Veerabathini A., Gangadaran P. Novel 2019 coronavirus: Genome structure, clinical trials, and outstanding questions. Experimental Biological Medicine (Maywood) 2020 doi: 10.1177/1535370220920540. 1535370220920540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson C., Hansson E.E., Sundquist K., Jakobsson U. Chronic pain in older adults: Prevalence, incidence, and risk factors. Scandinavian Journal of Rheumatology. 2017;46(4):317–325. doi: 10.1080/03009742.2016.1218543. [DOI] [PubMed] [Google Scholar]
- Lee I., Kovarik C., Tejasvi T., Pizarro M., Lipoff J.B. Telehealth: Helping your patients and practice survive and thrive during the COVID-19 crisis with rapid quality implementation. Journal of the American Academy of Dermatology. 2020;82(5):1213–1214. doi: 10.1016/j.jaad.2020.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N., Carr B.G. The role of telehealth in the medical response to disasters. JAMA Internal Medicine. 2018;178(6):745–746. doi: 10.1001/jamainternmed.2018.1314. [DOI] [PubMed] [Google Scholar]
- MaassenVanDenBrink A., de Vries T., Danser A.H.J. Headache medication and the COVID-19 pandemic. Journal of Headache Pain. 2020;21(1):38. doi: 10.1186/s10194-020-01106-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macfarlane G.J. The epidemiology of chronic pain. Pain. 2016;157(10):2158–2159. doi: 10.1097/j.pain.0000000000000676. [DOI] [PubMed] [Google Scholar]
- Martínez-Sarriegui I., García-Sáez G., Rigla M., Brugués E., de Leiva A., Gómez E.J., Hernando E.M. How continuous monitoring changes the interaction of patients with a mobile telemedicine system. Journal of Diabetes Science and Technology. 2011;5(1):5–12. doi: 10.1177/193229681100500102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan J., Straus S., Moher D., Langlois E.V., O’Brien K.K., Horsley T.…Tricco A.C. Reporting scoping reviews: PRISMA ScR extension. Journal of Clinical Epidemiology. 2020 doi: 10.1016/j.jclinepi.2020.03.016. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Micó Segura J.A. Coronavirus Covid-19 y dolor crónico: incertidumbres. Revista de la Sociedad Espanola de Dolor. 2020;27(2):72–73. [Google Scholar]
- Miller E. Dealing with uncertainty: Lessons learned from COVID-19. Pain Management Nursing. 2020 doi: 10.1016/j.pmn.2020.06.001. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills S.E.E., Nicolson K.P., Smith B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesiology. 2019;123(2):e273–e283. doi: 10.1016/j.bja.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministério da Saúde Portaria N° 467, De 20 De Março De 2020. 2020. http://www.in.gov.br/en/web/dou/-/portaria-n-467-de-20-de-marco-de-2020-249312996 Retrieved from.
- Moldofsky H., Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome: A case-controlled study. BMC Neurology. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Object Management Group Business process model and notation (BPMN) version 2.0. 2011. https://www.omg.org/spec/BPMN/2.0/PDF/ Retrieved from.
- Peters M., Godfrey C., McInerney P., Munn Z., Tricco A., Khalil H. Chapter 11: Scoping reviews (2020 version) In: A E., M Z., editors. Joanna Briggs Institute Reviewer’s Manual. 2020. [Google Scholar]
- PPM Editorial Board Managing chronic pain and related symptoms during coronavirus. Practical Pain Management. 2020 [Google Scholar]
- Quinlan-Colwell A. President’s column: Living with chronic pain during the COVID-19 pandemic. Southern Pain Society. 2020. https://southernpainsociety.org/presidents-column-living-with-chronic-pain-during-the-covid-19-pandemic/ Retrieved from.
- Ramos-Merino M., Alvarez-Sabucedo L.M., Santos-Gago J.M., Sanz-Valero J. A BPMN based notation for the representation of workflows in hospital protocols. Journal of Medical Systems. 2018;42(10):181. doi: 10.1007/s10916-018-1034-2. [DOI] [PubMed] [Google Scholar]
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W.…Consortium a. t.N.C.-R. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020 doi: 10.1001/jama.2020.6775. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rufai S.R., Bunce C. World leaders’ usage of Twitter in response to the COVID-19 pandemic: A content analysis. Journal of Public Health. 2020;42(3):510–516. doi: 10.1093/pubmed/fdaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B., Moss C., George G., Santaolalla A., Cope A., Papa S., Van Hemelrijck M. Associations between immune-suppressive and stimulating drugs and novel COVID-19: A systematic review of current evidence. Ecancermedicalscience. 2020;14:1022. doi: 10.3332/ecancer.2020.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanthanna H., Cohen S.P., Strand N., Lobo C., Eldabe S., Bhatia A., Narouze S. Recommendations on chronic pain practice during the COVID-19 pandemic. 2020. https://www.asra.com/page/2903/recommendations-on-chronic-pain-practice-during-the-covid-19-pandemic Retrieved from. [DOI] [PMC free article] [PubMed]
- Shanthanna H., Strand N.H., Provenzano D.A., Lobo C.A., Eldabe S., Bhatia A.…Narouze S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia. 2020 doi: 10.1111/anae.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodhi M., Etminan M. Safety of ibuprofen in patients with COVID-19: Causal or confounded? Chest. 2020 doi: 10.1016/j.chest.2020.03.040. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A.…Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) International Journal of Surgery. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solé E., Racine M., Tomé-Pires C., Galán S., Jensen M.P., Miró J. Social factors, disability, and depressive symptoms in adults with chronic pain. The Clinical Journal of Pain. 2020;36(5):371–378. doi: 10.1097/AJP.0000000000000815. [DOI] [PubMed] [Google Scholar]
- Song X.J., Xiong D.L., Wang Z.Y., Yang D., Zhou L., Li R.C. Pain management during the COVID-19 pandemic in China: Lessons learned. Pain Medicine. 2020 doi: 10.1093/pm/pnaa143. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spine Intervention Society SIS Guidance on Interventional Pain Procedures During the COVID-19 Global Emergency. 2020. https://www.spineintervention.org/page/COVID-19 Retrieved from.
- Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D.…Straus S.E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.