Abstract
Objectives
To estimate the effect of early application of social distancing interventions on Covid-19 cumulative mortality during the first pandemic wave.
Methods
Ecological longitudinal study using multivariable negative binomial regression for panel data. Daily numbers of Covid-19 cases and deaths, and data on social distancing interventions, for the 37 member countries of the Organization for Economic Cooperation and Development (OECD) were analysed.
Results
Covid-19 cumulative mortality over the first pandemic wave varied widely across countries (range, 4.16 to 855 deaths per million population). On average, one-day delay in application of mass gatherings ban was associated with an adjusted increase in Covid-19 cumulative mortality by 6.97% (95% CI, 3.45 to 10.5), whilst a one-day delay in school closures was associated with an increase of 4.37% (95% CI, 1.58 to 7.17) over the study period. We estimated that if each country had enacted both interventions one week earlier, Covid-19 cumulative mortality could have been reduced by an average of 44.1% (95% CI, 20.2 to 67.9).
Conclusions
Early application of mass gatherings ban and school closures in outbreak epicentres was associated with an important reduction in Covid-19 cumulative mortality during the first pandemic wave. These findings may support policy decision making.
Key words: Covid-19, Sars-cov-2, 2019-ncov, Severe acute respiratory syndrome coronavirus 2
Introduction
The World Health Organization (WHO) officially declared coronavirus disease 2019 (Covid-19), the infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a pandemic on 11 March 20201. After having spread outside the borders of China, the disease has caused more than 34 million confirmed cases and approximately one million deaths as of 1 October 20201. Although the Chinese health authorities officially reported an outbreak of a new type of pneumonia in the Wuhan region on 31 December, SARS-CoV-2 was circulating in this area as early as end of November, with the first official case diagnosed on 1 December 20192. Due to this delay, international travel restrictions were ineffective and may have contributed to a shortage of medical supplies3, hence viral spread to highly connected countries could not be avoided4. Although some countries were violently struck by the pandemic in early March5 , 6, international spread was very heterogeneous during the initial phase. In the absence of a vaccine and effective pharmacological treatments, governments started to progressively enact a wide spectrum of public health interventions, including physical and social distancing, to avoid uncontrolled viral circulation and excess mortality7. The interventions ranged from social distancing encouragement, use of mouth/face coverings and restrictions on public gatherings, to curfew and stay-at-home orders, especially in countries displaying an exponential trend of cases and deaths5, 6, 7, 8.
Observational and modelling studies have shown that most social distancing interventions significantly reduce incidence of new Covid-19 cases and deaths by comparing the observed epidemic curves with alternative scenarios assuming linear or exponential growth in the case of absence of such interventions9, 10, 11, 12, 13. Given the current evidence, it is plausible to assume that countries applying interventions at an earlier stage of the national epidemics may have been able to keep the viral spread below a certain growth threshold11. Nonetheless, whether a more effective containment of the epidemic at the initial stage is associated with reduced Covid-19 cumulative mortality over longer periods still remains to be ascertained.
The aim of the current study was to evaluate the effect of early social distancing interventions on Covid-19 cumulative mortality during the first pandemic wave. In particular, we estimated the effect of the timing of widely applied interventions, such as mass gatherings ban and school closures, in outbreak epicentres across a set of countries with different characteristics and magnitude of the spread. Our findings may support policy decision making as governments prepare for upcoming epidemic waves.
Materials and methods
We have conducted an analysis of longitudinal data on the 37 member countries of the Organization for Economic Cooperation and Development (OECD) between 1 January and 30 June 2020, that is six months observation time for each country. Our aim was to estimate the impact of early social distancing interventions on Covid-19 cumulative mortality during the first pandemic wave, given that each country has enforced interventions at a different phase of their national epidemics. To build a meaningful model of mortality, we have considered the timing of application of interventions in respect to the date that the first Covid-19 death was notified in each individual country (t0), and have adjusted for the cumulative burden of Covid-19 cases up to the same date, and for covariates expressing demographic, geographic and healthcare features of individual countries.
Social distancing interventions
We obtained data regarding the timing and nature of social distancing interventions enforced by each one of the 37 OECD countries during the observation period (1 January to 30 June 2020). The source of data was the Oxford Covid-19 Government Response Tracker7, cross-checked with the Covid-19 Health System Response Monitor (www.covid19healthsystem.org), the European Union Agency for Fundamental Rights (fra.europa.eu), the Imperial College13, and national institutional websites. We collected longitudinal data regarding social distancing interventions including closure of schools and workplaces, restrictions on mass gatherings (a combination of ban of public events and restriction on the number of people gathering in the same place), stay-at-home orders, curfew, and restrictions regarding travelling abroad and other types of travel inside the country. Information was abstracted independently by two investigators using a standardised extraction form and compared to ensure data accuracy. Since most of these measures are closely related and were implemented within a short time period in most countries, it was decided that the study would focus on the effect of the timing of two early social distancing interventions: school closures in national outbreak epicentres (i.e., areas surrounding emerging outbreaks), and mass gatherings ban (i.e., more than 1000 people) including any ban of large public event. These two measures were widely applied for long periods of time in countries with different Covid-19 mortality and characteristics, and allow for a broader generalisability of the findings.
For each individual country, we evaluated the timing of each intervention independently, as the difference in days between the date that the first Covid-19 associated death was registered (t0) and the date of application. An additional variable was derived for each social distancing intervention by adding a relevant lag-period to allow for any potential effects on daily Covid-19 mortality (see statistical analysis section)9. In each country, t0 was set to the day that the first Covid-19 associated death was registered: it provides a reliable reference date for the start of the national epidemics in comparison with the date that the first cases were notified, which is vastly biased by diagnostic capacity. Two countries (Japan and Turkey) did not ban mass gatherings, while one country (Sweden) did not close schools during the observation period. These countries were excluded from the analyses concerning the timing of interventions.
Covariates
Individual-country characteristics were screened to be included in our multivariable model as covariates, to assess the independent association of the interventions of interest with Covid-19 mortality. Primary data sources were the World Bank (data.worldbank.org), the OECD (data.oecd.org), and national institutional websites.
Adequate diagnostic capacity is the first necessary step to face epidemics. Individual countries’ testing capacity in the initial phase of the pandemic was unavailable, or unreliable, for several countries. For this reason, we computed the Covid-19 cumulative incidence of confirmed cases up to the day in which the first Covid-19 death was registered in each country (t0) by considering officially registered cases. This variable is an effective proxy for early testing and diagnostic capacity of individual countries, while also being associated with the initial magnitude of viral spread.
Demographic characteristics are associated with Covid-19 prognosis14, and potentially with the effectiveness of certain interventions; hence, we collected the proportion of the population over 65 years, 15 to 64 years, and less than 15 years of age. Additionally, the proportion of Covid-19 cases who were more than 65 years old and the male-to-female ratio were collected from national institutional reports. The proportion of the population living in urban or rural areas and population density were collected, as they may be associated with a higher individual chance of contagion and with the effectiveness of certain measures. The proportion of daily smokers and the proportion of overweight and obese inhabitants were also collected, as these factors may affect Covid-19 severity and mortality15 , 16.
To account for healthcare capacity and access to healthcare across different countries, we have considered: the number of hospital beds per 1000 population, the poverty gap and income inequality indices and the governmental health spending per capita.
It is believed that the initial international spread outside of China occurred in areas with frequent transport links to this country3, hence potentially relevant travel-related indices, such as the number of air passengers carried annually and the number of international tourism arrivals and departures, were collected. We considered the “island status” of each individual country, as it is assumed that people can move to these countries only through air or naval transportations. These variables may contribute to explain the baseline level of national epidemics. Since we assumed that most countries adopted effective interventions and achieved containment over a certain period of time, we hypothesized that the baseline level of the national epidemic is an important factor to explain the heterogeneity in Covid-19 cumulative mortality across countries during the first pandemic wave.
Statistical analysis
The outcome variable was the daily number of Covid-19 deaths in each country as reported by the WHO. However, in some countries a negative number of Covid-19 deaths was reported in certain days due to government recalculation, hence we considered the closest integer value of the 7-days moving average as the outcome variable. The denominator for estimating mortality was the official country population in 2018. Since social distancing interventions are not expected to have an immediate effect on mortality, we have considered their timing (and the interaction terms) in respect to t0 with the addition of relevant lag-times. A median lag-time of 5 days from exposure to symptom onset,17 and of 17 days from symptom onset to death9 , 18 was assumed. However, for school closures an additional period of 4 days to allow child-to-adult transmission was considered, assuming a possible infection at the asymptomatic stage9. In summary, the lag-times adopted in the main analysis were 22 days for mass gatherings ban, and 26 days for school closures.
To build the multivariable model for Covid-19 mortality, we employed negative binomial regression analyses for longitudinal data using generalized estimating equations with log link function19. In the model specification, we took into account clustering by country and used Huber-White standard error estimators which are robust to misspecifications regarding the within-country correlation structure and the assumption of covariance across countries20. The natural logarithm of the population size was included in the equation as an offset. The following equation was used:
where Y is the daily number of Covid-19 deaths in country i; γ is the timing of mass gatherings ban [i.e., the number of days elapsed from the day of the first death (t0) until the enforcement of restrictions on mass gatherings in country i] plus a lag-time of 22 days; σ is the timing of school closures (i.e., the number of days elapsed from t0 until the first school closures in outbreak epicentres in country i) plus a lag-time of 26 days; x1 is the percentage of the population living in urban areas; x2 is the number of hospital beds per 1000 population; x3 is the number of air transport passengers carried annually; x4 is a binary variable taking value 1 if country i is an island (i.e., people can move to country i only through air or naval transportations); x5 is the Covid-19 cumulative incidence of cases at t0 per million population.
The equation includes the interaction effect between the timing of each intervention [β1(β2)]; the interaction effect between the percentage of the population between 15 and 64 years of age (where β8 is the direct effect of this variable) and the Covid-19 cumulative incidence of cases at t0 expressed as natural logarithm [β8(β7)]; the interaction effect between the timing of mass gatherings ban and the natural logarithm of the population density in country i (where β9 is the direct effect of this variable) [β1(β9)]; the interaction effect between β6 (the coefficient of the binary variable x4, which takes value 1 if country i is an island) and the number of annual air transport passengers [β5(β6)]; and the interaction effect between β6 and the Covid-19 cumulative incidence of cases at t0 expressed as natural logarithm [β6(β7)].
Concerning variable x4, South Korea was considered as an island since importing foreign Covid-19 positive cases from other neighbouring countries without naval or air transportation was considered unfeasible and, at the beginning of the observation period, there were no Covid-19 confirmed cases in this country.
Potential effects associated with subsequent lifting of the two social distancing interventions occurred outside the study period, hence are not considered. Only in four countries, schools were re-opened toward the end of the observation period with mandatory social distancing measures, but, after considering the lag-time, the effective period in which this could have affected Covid-19 mortality was so short that any potential effect was deemed negligible.
To build the model we have used a stepwise approach, with entry and removal criteria specified at a p value of < 0.20 as well as the consensus opinion of a group of public health experts and methodologists. All the interaction terms included in the model were significant at a p value of < 0.05. After reaching the final model, the average marginal effect considering the other covariates at their means was computed for each independent variable21. The marginal effect (in terms of adjusted predicted relative change) can be interpreted as the average percent increase (average linear β coefficient) in one unit of variable xi on the outcome variable (Covid-19 mortality) taking into account the full model including interaction terms and approximating the effect of variable xi on the outcome variable as linear21 , 22. This provides a more substantive and practical picture of the results of a statistical model, especially when several interaction terms render the interpretation of the fitted β coefficient unfeasible21.
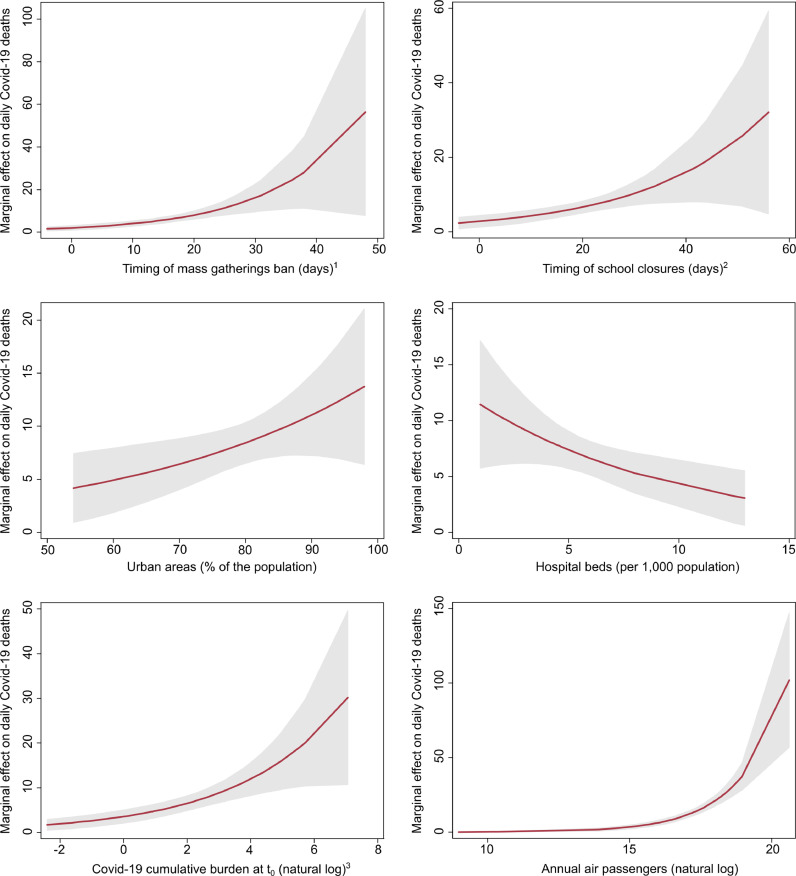
The epidemiological relevance of each independent variable in the final model was verified by computing and plotting the marginal effect of each continuous variable on Covid-19 mortality to also allow readers to observe non-linear associations21 , 23. To further verify the fitted model, we plotted the number of deaths in each country during the entire period of observation (as observed) against those predicted by the model.
Since the outcome variable of a negative binomial model is death count, in order to have interpretable results, we converted the results into predicted Covid-19 cumulative mortality. The main results are reported in terms of adjusted predicted relative change in Covid-19 cumulative mortality per million population over the observation period. We used model parameters to estimate the variation of the predicted marginal Covid-19 cumulative mortality in case of multiple alternative scenarios assuming different timing of application of each single intervention as compared to the observed dates. As sensitivity analyses, we used model parameters to estimate the relative change in Covid-19 cumulative mortality according to timing of interventions in countries with low vs high (i.e. the cut-off value equals the median) Covid-19 cumulative incidence of cases at t0, percentage of the population living in urban areas, number of hospital beds and number of annual air passengers considering the other covariates at their means. Unadjusted analyses comparing the timing of social distancing interventions across different groups were conducted using the two-sample Mann-Whitney U test. We performed the analyses using STATA version 15.0 (Stata Corp., College Station, TX, USA) and two-sided p values of < 0.05 were considered statistically significant.
Sensitivity analyses around the lag-time
Although the lag-times we used to fit the model of mortality have been already employed in the literature9 , 17, these are estimated median times. To examine the robustness of the main findings, we have conducted sensitivity analyses by using 5-days shorter (i.e. 17 days for restrictions on mass gatherings, and 21 days for those on schools) and 5-days longer lag-times (i.e. 27 days for restrictions on mass gatherings, and 31 days for those on schools) with respect to the main analyses.
Patient and public involvement
The current study did not involve patients and the public directly, as their involvement was not considered feasible. However, the main findings will be widely disseminated through official (press release, institutional websites, and repositories), personal and social media.
Results
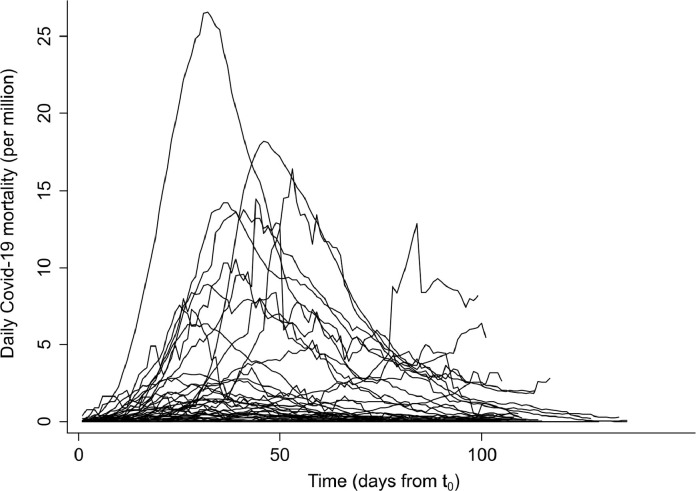
During the first pandemic wave (January 1 to June 30, 2020), Covid-19 cumulative mortality varied widely across the 37 OECD countries, ranging from 4.16 per million population in Australia to 855 per million population in Belgium (Table 1 ). The first Covid-19 death, in each country, occurred between February 13 and April 7, 2020. The peak incidence was reached after a median of 32 days from the day the first Covid-19 death was registered in each country (t0) with heterogeneous shapes of the epidemic curves (Fig. 1 ).
Table 1.
Country characteristics by coronavirus disease 2019 (Covid-19) cumulative mortality during the first pandemic wave (from January 1 to June 30, 2020).
| Country | Covid-19 cumulative mortality (per million population) | Time to reach the peak mortality from t0a (days) | Timing of mass gatherings banb (days) | Timing of school closuresb,c (days) | Hospital beds (per 1000 population) | Aged 15‒64 (% of the population) | Urban areas (% of the population) | Annual air passengers (natural log) | Density (population per km2) | Covid-19 cumulative incidence of cases at t0a (per million population) |
|---|---|---|---|---|---|---|---|---|---|---|
| Countries with low Covid-19 cumulative mortality (1st and 2nd quartiles) | ||||||||||
| Median (IQR) | 30.5 (7.69 to 52.2) | 26 (19 to 36) | −8 (−13 to −2) | −6.5 (−13 to −4) | 4.50 (3.53 to 6.54) | 65.3 (64.0 to 66.3) | 80 (68 to 86) | 16.2 (15.2 to 17.3) | 45.0 (18.0 to 113) | 87.6 (3.48 to 134) |
| Australia | 4.16 | 37 | +14 | +15 | 3.84 | 65.5 | 86 | 18.1 | 3.00 | 1.16 |
| New Zealand | 4.50 | 17 | −13 | −6 | 2.57 | 65.4 | 87 | 16.7 | 18.0 | 98.0 |
| Slovakia | 5.14 | 16 | −26 | −30 | 5.70 | 68.5 | 54 | 8.98 | 113 | 98.8 |
| South Korea | 5.46 | 36 | +1 | −17 | 12.4 | 72.8 | 81 | 18.3 | 529 | 2.05 |
| Japan | 7.69 | 71 | NA | +18 | 13.0 | 59.7 | 92 | 18.7 | 347 | 0.28 |
| Latvia | 15.6 | 19 | −22 | −22 | 5.49 | 64.0 | 68 | 15.2 | 31.0 | 257 |
| Greece | 17.8 | 22 | −3 | −13 | 4.20 | 63.7 | 79 | 16.5 | 83.0 | 9.42 |
| Lithuania | 27.8 | 26 | −8 | −7 | 6.43 | 65.2 | 68 | 10.2 | 45.0 | 25.3 |
| Iceland | 28.3 | 16 | −4 | −4 | 2.83 | 66.7 | 94 | 15.9 | 4.00 | 1164 |
| Czech Republic | 32.7 | 21 | −13 | −12 | 6.62 | 64.8 | 74 | 15.6 | 15.6 | 110 |
| Israel | 36.0 | 30 | −16 | −8 | 2.98 | 60.0 | 92 | 15.8 | 410 | 80.5 |
| Poland | 37.6 | 47 | −2 | 0 | 6.54 | 67.6 | 60 | 16.0 | 124 | 1.38 |
| Norway | 46.9 | 31 | −1 | 0 | 3.53 | 65.3 | 82 | 16.3 | 15.0 | 142 |
| Estonia | 52.2 | 12 | −1 | −20 | 4.57 | 64.0 | 69 | 10.4 | 30.0 | 307 |
| Slovenia | 53.6 | 24 | −13 | −6 | 4.43 | 65.3 | 55 | 13.9 | 103 | 134 |
| Finland | 59.5 | 32 | −9 | −5 | 3.61 | 62.3 | 85 | 16.4 | 18.0 | 94.8 |
| Hungary | 59.9 | 38 | −4 | −4 | 7.01 | 66.3 | 71 | 17.3 | 108 | 3.48 |
| Colombia | 62.3 | NA | −11 | −7 | 1.71 | 66.1 | 81 | 17.3 | 45.0 | 4.01 |
| Countries with high Covid-19 cumulative incidence of death (3rd and 4th quartiles) | ||||||||||
| Median (IQR) | 297 (152 to 522) | 39 (31 to 49) | +1 (−4 to +8) | +1 (−2 to +6) | 2.97 (2.52 to 4.63) | 65.4 (64.0 to 66.7) | 80 (74 to 88) | 17.6 (16.4 to 18.5) | 112 (65.0 to 237) | 9.26 (0.96 to 43.8) |
| Turkey | 62.8 | 34 | NA | −2 | 2.85 | 67.9 | 75 | 18.6 | 107 | 2.40 |
| Austria | 79.5 | 28 | −2 | −2 | 7.27 | 66.8 | 58 | 16.4 | 107 | 41.1 |
| Denmark | 104 | 23 | −9 | −2 | 2.6 | 64.0 | 88 | 15.7 | 138 | 150 |
| Germany | 108 | 41 | +3 | −12 | 8 | 65.0 | 77 | 18.5 | 237 | 13.8 |
| Portugal | 152 | 26 | −5 | −1 | 3.45 | 64.6 | 65 | 16.7 | 112 | 43.8 |
| Luxembourg | 181 | 28 | −4 | +3 | 4.26 | 69.5 | 91 | 14.6 | 250 | 65.8 |
| Switzerland | 197 | 31 | −6 | +8 | 4.63 | 66.6 | 74 | 17.2 | 215 | 23.9 |
| Mexico | 213 | 100 | +5 | −6 | 0.98 | 66.3 | 80 | 18 | 65.0 | 0.96 |
| Canada | 230 | 57 | +1 | +1 | 2.52 | 66.7 | 81 | 18.3 | 4.00 | 2.56 |
| Chile | 297 | 84 | −5 | −5 | 2.06 | 68.7 | 88 | 16.8 | 25.0 | 23.3 |
| Netherlands | 354 | 32 | +4 | +6 | 3.17 | 65.0 | 91 | 17.6 | 511 | 7.54 |
| Ireland | 357 | 44 | +1 | +1 | 2.97 | 65.4 | 63 | 18.9 | 71.0 | 9.26 |
| USA | 386 | 49 | +8 | +6 | 2.87 | 65.4 | 82 | 20.6 | 36.0 | 0.34 |
| France | 444 | 53 | +14 | +30 | 5.91 | 62.1 | 80 | 18.1 | 122 | 0.19 |
| Sweden | 522 | 39 | −4 | NA | 2.14 | 62.4 | 87 | 16.3 | 25.0 | 98.1 |
| Italy | 575 | 39 | +16 | 0 | 3.14 | 64.0 | 70 | 17.1 | 205 | 0.25 |
| Spain | 607 | 46 | +26 | +25 | 2.97 | 65.8 | 80 | 18.2 | 94.0 | 0.09 |
| United Kingdom | 656 | 37 | +9 | +16 | 2.46 | 63.8 | 83 | 18.9 | 275 | 2.48 |
| Belgium | 855 | 32 | +0 | +6 | 5.58 | 64.2 | 98 | 16.4 | 377 | 44.2 |
Abbreviation: NA, not available.
t0 is the calendar day of notification of the first Covid-19 death in each country.
expressed in days from t0 (negative counts mean that the intervention was enforced earlier).
school closures in national outbreak epicentres.
Fig. 1.
Epidemic curves showing Covid-19 daily mortality (as 7-days moving average) in the 37 countries of the Organization for Economic Cooperation and Development, from the calendar day of notification of the first Covid-19 death in each country (t0) until 30 June 2020. Each epidemic curve was aligned at t0. Countries showing the highest peak of Covid-19 daily mortality were: Belgium, Spain, France, Ireland, and UK.
Covid-19 cumulative incidence of confirmed cases at t0 varied from <1 to 1164 cases per million population reflecting drastically different testing and diagnostic capacities, and magnitude of the epidemic in the initial phase. Country characteristics by Covid-19 cumulative mortality are presented in Table 1. There was a very wide variability in population density and in annual air passengers carried in each country. There was less variability in the proportion of the population living in urban areas and in the proportion of the population 15 to 64 years old. The length of the ascending phase, expressed as number of days from t0 to peak daily mortality, varied across countries (median, 32; IQR, 25‒42.5) and was a median of 13 days longer amongst countries showing high Covid-19 cumulative mortality (p = .005), Table 1.
Timing of social distancing interventions
The interventions of interest were: mass gatherings ban and school closures in national outbreak epicentres. Countries enforced the mass gatherings ban a median of three days before t0 (median, −3; IQR, −9 to +3), and the first school closures a median of two days before t0 (median, −2; IQR, −7 to +4.5), Table 1.
Unadjusted analyses showed that countries with a high Covid-19 cumulative mortality over the first wave enforced mass gatherings ban a median of 9 days later and started to close the first schools a median of 7.5 days later than countries with a lower cumulative mortality (p = .003 and p = .001, respectively). Countries with a long ascending phase (based on the median) enacted mass gatherings ban a median of 9 days later and enacted the first school closures a median of 6.5 days later than countries with a short ascending phase (p < .001 and p = .007, respectively).
Adjusted analyses
According to our model, each one-day increase in the timing of mass gatherings ban was associated, on average, with an adjusted predicted relative change (PRC) of +6.97% (95% CI, +3.45 to +10.5) in Covid-19 cumulative mortality over the study period. Each one-day increase in the timing of school closures was instead associated, on average, with a PRC of +4.37% (95% CI, +1.58 to +7.17).
In an alternative scenario analysis derived from the model, we estimated that if each country had enacted both these interventions one week earlier, the predicted Covid-19 cumulative mortality of the first pandemic wave would have been reduced by an average of 44.1% (95% CI, 20.2 to 67.9). Similarly, one-week delay in the enforcement would have resulted in an estimated predicted increase I Covid-19 cumulative mortality by an average of 56.7% (95% CI, 20.4 to 93.1). Multiple alternative scenarios assuming different timing of each individual intervention are presented in Table 2 .
Table 2.
Estimated adjusted relative Covid-19 cumulative mortality over the first pandemic wave in alternative scenarios assuming different timing of application of mass gathering bans and school closures in national outbreak epicentres after fitting multivariable negative binomial regression using generalised estimating equations.
| Mass gatherings banned two weeks earlier (95% CI) | Mass gatherings banned one week earlier (95% CI) | Mass gatherings banned as observed (95% CI) | Mass gatherings banned one week later (95% CI) | Mass gatherings banned two weeks later (95% CI) | |
|---|---|---|---|---|---|
| Schools closed two weeks earlier | −72.1% (−94.0 to −50.8) | −55.2% (−78.3 to −32.2) | −25.7% (−55.6 to +4.25) | +26.3% (−32.6 to +85.1) | +119% (−20.9 to +260) |
| Schools closed one week earlier | −62.7% (−86.4 to −38.9) | −44.1% (−67.9 to −20.2) | −14.2% (−41.8 to +13.4) | +34.5% (−14.8 to +83.8) | +116% (+4.91 to +227) |
| Schools closed as observed | −49.0% (−78.7 to −19.4) | −29.4% (−56.7 to −2.16) | ‒ | +44.6% (+3.43 to +85.7) | +114% (+25.4 to +202) |
| Schools closed one week later | −29.7% (−73.3 to +13.9) | −10.1% (−46.7 to +26.5) | +17.4% (−12.1 to +47.0) | +56.7% (+20.4 to +93.1) | +114% (+38.8 to +189) |
| Schools closed two weeks later | −2.15% (−73.6 to +69.3) | +15.5% (−40.4 to +71.3) | +39.2% (−0.90 to +79.3) | +71.3% (+33.1 to +110) | +115% (+43.3 to +187) |
Abbreviation: CI, confidence interval.
Notes: Estimates in bold are statistically significant. All the estimates are adjusted for the following country-level variables: percentage of population living in urban areas; hospital beds; the natural logarithm of Covid-19 cumulative incidence of confirmed cases at t0 (where t0 equals the calendar day of notification of the first Covid-19 death in each country); the natural logarithm of annual air passengers; the island status of a country; the interaction effect between the timing of mass gatherings ban and the timing of school closures; the interaction effect between the percentage of population between 15 and 64 years of age and the Covid-19 cumulative incidence of confirmed cases at t0; the interaction effect between the timing of mass gatherings ban and the natural logarithm of the average population density; the interaction effect between the island status of a country and the number of air transport passengers carried annually; the interaction effect between the island status of a country and the Covid-19 cumulative incidence of confirmed cases at t0.
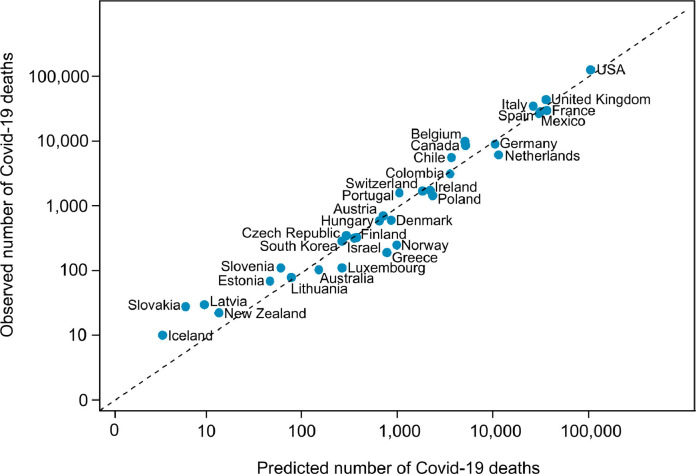
The relative change in Covid-19 cumulative mortality due to each social distancing measure was significantly modified by the timing of the other intervention (i.e. negative interaction term, data not shown). The effect of timing of mass gatherings ban was significantly increased by population density. The adjusted predicted Covid-19 cumulative mortality was higher in highly urbanised countries, those with a high number of airport passengers, and a high Covid-19 cumulative incidence of cases at t0, while it was lower in island countries and in countries with a high number of hospital beds per 1000 population (suggestive evidence). We present the plot of observed vs. predicted number of Covid-19 deaths for countries having applied mass gathering bans and school closures in national outbreak epicentres in Fig. 2 . We report the marginal effect of the timing of each intervention and of each covariate, by means of adjusted PRC, in Table 3 . Finally, we present the plots of the marginal adjusted predictions, corresponding to the timing of each intervention and to each continuous covariate, in Fig. 3 .
Fig. 2.
Graph comparing the observed number of Covid-19 deaths up to 30 June 2020, across the 34 countries having applied mass gatherings ban and school closures in national outbreak epicentres, with the number of Covid-19 deaths as predicted through multivariable negative binomial regression using generalised estimating equations.
Table 3.
Average marginal effect of timing of “mass gatherings ban” and “school closures” on Covid-19 mortality after fitting multivariable negative binomial regression using generalised estimating equations.
| Average marginal effectb on Covid-19 mortality |
|||
|---|---|---|---|
| Adjusted predicted relative change | (95% CI) | P-value | |
| Timing of social distancing interventionsa | |||
| Mass gatherings ban (days)a,c | +6.97% | (+3.45 to +10.5) | <0.001 |
| School closures (days)a,c,d | +4.37% | (+1.58 to +7.17) | 0.002 |
| Other covariates | |||
| Urban areas (% of the population)c | +2.70% | (+0.08 to +5.32) | 0.044 |
| Hospital beds (per 1000 population)c | −10.9% | (−22.4 to +0.50) | 0.061 |
| Covid-19 cumulative burden at t0 (natural log)c,e | +30.2% | (+14.8 to +45.6) | <0.001 |
| Annual air passengers (natural log)c | +60.5% | (+50.0 to +71.1) | <0.001 |
| Island countryc | |||
| No | reference | ‒ | ‒ |
| Yes | −82.6% | (−100 to −61.6) | <0.001 |
Abbreviation: CI, confidence interval.
expressed in days from t0, where t0 is the calendar day of notification of the first Covid-19 death in each country.
the marginal effect (in terms of adjusted predicted relative change) can be interpreted as the average percent increase (average linear β coefficient) in one unit of variable xi on the outcome variable (Covid-19 mortality) taking into account the full model including interaction terms, approximating the effect variable xi on the outcome variable as linear.
each independent variable is adjusted for the other variables and additional five interaction terms: -interaction effect between the timing of mass gatherings ban and the timing of school closures; -interaction effect between the percentage of the population between 15 and 64 years of age and the Covid-19 cumulative incidence of confirmed cases at t0; -interaction effect between the timing of mass gatherings ban and the natural logarithm of the average population density; -interaction effect between the island status of a country and the number of air transport passengers carried annually; -interaction effect between the island status of a country and the Covid-19 cumulative incidence of confirmed cases at t0.
school closures in national outbreak epicentres.
Covid-19 cumulative incidence of confirmed cases at t0 (per million population).
Fig. 3.
Panel graph reporting the marginal adjusted predictions corresponding to timing of mass gatherings ban and school closures in national outbreak epicentres and to each continuous covariate in the multivariable negative binomial regression using generalised estimating equations a
a the marginal plots of each continuous variable reported are adjusted for other variables at their mean values, the dichotomous variable representing the island status of a country, and additional five interaction terms:
-interaction effect between the timing of mass gatherings ban and the timing of school closures;
-interaction effect between the percentage of the population between 15 and 64 years of age and the Covid-19 cumulative incidence of confirmed cases at t0;
-interaction effect between the timing of mass gatherings ban and the natural logarithm of the average population density;
-interaction effect between the island status of a country and the number of air transport passengers carried annually;
-interaction effect between the island status of a country and the Covid-19 cumulative incidence of confirmed cases at t0.
1 expressed in days from t0, where t0 is the calendar day of notification of the first Covid-19 death in each country (negative counts mean that the intervention was enforced earlier), plus a lag-time of 22 days.
2 school closures in national outbreak epicentres expressed in days from t0, where t0 is the calendar day of notification of the first Covid-19 death in each country (negative counts mean that the intervention was enforced earlier), plus a lag-time of 26 days.
3 Covid-19 cumulative incidence of confirmed cases at t0 (per million population).
The effect of the timing of social distancing interventions on Covid-19 mortality was consistently significant across countries with different temporal application of both interventions, different Covid-19 cumulative incidence at t0, number of hospital beds, urbanisation level and number of annual air passengers (Table 4 ).
Table 4.
Adjusted stratified analysis of the marginal effect of one-day delay in “mass gatherings ban” and “school closures” on Covid-19 mortality after fitting multivariable negative binomial regression using generalised estimating equations.
| Average marginal effecta on Covid-19 mortality |
||||
|---|---|---|---|---|
| Mass gatherings ban | (95% CI) | School closures | (95% CI) | |
| Timing of social distancing interventionsb | ||||
| Countries applying both interventions earlyc (n = 12) | +7.99% | (+4.54 to +11.4) | +6.14% | (+3.04 to +9.25) |
| Countries applying both interventions latec (n = 13) | +5.09% | (+2.17 to +8.02) | +2.75% | (+0.82 to +4.68) |
| Other factors | ||||
| Covid-19 cumulative burden at t0a,d | ||||
| Low | +6.22% | (+3.28 to +9.17) | +3.04% | (+1.15 to +4.94) |
| High | +7.63% | (+3.73 to +11.5) | +5.55% | (+2.26 to +8.84) |
| Hospital beds (per 1000 population) | ||||
| Low | +6.22% | (+2.79 to +9.64) | +4.00% | (+1.46 to +6.55) |
| High | +7.72% | (+4.10 to +11.3) | +4.74% | (+1.77 to +7.71) |
| Urban areas (% of the population) | ||||
| Low | +8.28% | (+4.62 to +11.9) | +5.00% | (+2.41 to +7.58) |
| High | +5.94% | (+2.45 to +9.42) | +3.88% | (+1.06 to +6.69) |
| Annual air passengers | ||||
| Low | +7.82% | (+3.93 to +11.7) | +5.49% | (+2.30 to +8.68) |
| High | +6.01% | (+3.11 to +8.91) | +3.11% | (+1.16 to +4.82) |
Abbreviation: CI, confidence interval.
the marginal effect (in terms of adjusted predicted relative change) can be interpreted as the average percent increase (average linear β coefficient) in one unit of variable xi on the outcome variable (Covid-19 mortality) taking into account the full model including interaction terms, approximating the effect variable xi on the outcome variable as linear.
expressed in days from t0, where t0 is the calendar day of notification of the first Covid-19 death in each country.
countries were divided into early and late on the basis of the median time of application of both social distancing interventions.
Covid-19 cumulative incidence of confirmed cases at t0 (per million population).
Sensitivity analysis around the lag-time
The adjusted PRC on Covid-19 cumulative mortality associated with mass gatherings ban was +6.86% (95% CI, +3.39 to +10.3) when considering a 5-days shorter lag-time (i.e. 17 days) and +7.05% (95% CI, +3.49 to +10.6) when using a 5-days longer lag-time (i.e. 27 days), as compared to the main analysis. The adjusted PRC on Covid-19 cumulative mortality associated with school closures was +4.44% (95% CI, +1.64 to +7.23) when considering a 5-days shorter lag-time (i.e. 21 days) and +4.33% (95% CI, +1.53 to +7.13) in case of a 5-days longer lag-time (i.e. 31 days). These sensitivity analyses confirmed the robustness of the main findings.
Discussion
In this study, early application of mass gatherings ban and school closures in national outbreak epicentres was associated with an important reduction in Covid-19 mortality over the first pandemic wave. The results were robust in sensitivity analyses considering varying lag-times and across countries with different characteristics. Our model estimated that one-week earlier application of both these interventions in each country could have yielded a reduction of the overall Covid-19 mortality by more than 40%. The analysis of alternative scenarios assuming different times of application of each intervention suggests the importance of early enforcement of both public health measures. Although the concurrent application of mass gatherings ban and school closures significantly reduced mortality at any stage of the national epidemic, the relative reduction tended to be greater when both interventions were applied very precociously. Countries displaying a long ascending phase had applied both interventions of social distancing later, and were more likely to reach high Covid-19 cumulative mortality than countries with shorter ascending phases and earlier actions. These findings support the hypothesis that countries implementing social distancing interventions at an earlier stage of the national epidemics are more likely to keep the viral spread below a certain growth threshold11. Our study suggests that a more effective containment of the epidemic at the initial stage may help reduce Covid-19 cumulative mortality over longer periods.
Our findings complement and strengthen previous research on the beneficial effects of application of social distancing interventions in reducing Covid-19 incidence and mortality9, 10, 11, 12, 13 , 24 , 25. The results are in agreement with previous studies postulating a greater effectiveness of school closures and other social distancing measures at earlier stages of the national epidemics9 , 10. As indicated by the UK Department of Health's scientific summary on the effectiveness of health measures for containment of epidemics, studies in this field use a variety of methods and approaches, hence a direct comparison of their results is often challenging26. For instance, Auger and colleagues estimated that the predicted Covid-19 mortality in US states decreased by more than 50% for each additional week of state-wide school closures9. Conversely, Islam and colleagues provided much more conservative estimates, and suggested that there was a 15% reduction in the incidence of Covid-19 cases when school closures, workplace closures and mass gatherings ban were in place10. However, these studies estimated the effectiveness of health policy measures by comparing the observed data with alternative scenarios assuming a linear or exponential growth of the epidemic curve had countries never implemented the interventions of interest9 , 10. For this reason, it is difficult to directly compare the results of our study, which aimed to estimate the effect of the timing of social distancing interventions on Covid-19 cumulative mortality. Our findings add to the existing evidence, and could help health policy makers to plan the optimal timing of social distancing measures in upcoming pandemic waves.
In this large analysis of longitudinal data concerning the effect of early application of mass gatherings ban and school closures in national outbreak epicentres on Covid-19 mortality, the 37 OECD countries were included. We use a comprehensive and robust methodological approach to build a meaningful model of Covid-19 mortality across a set of countries with different characteristics and magnitude of national epidemics, thus allowing broad generalisability. Our study answers key questions regarding the timing of two very widely applied measures of social distancing, suggesting that a concurrent, early enforcement of mass gatherings ban and school closures is significantly associated with a large reduction in Covid-19 mortality. The secondary analyses agree with previous suggestive evidence that a combination of interventions without banning mass gathering might not be able to flatten the epidemic curve10. A major strength of the study is that we have considered daily Covid-19 deaths as the outcome variable. We have avoided to rely on daily reported Covid-19 cases, as these data have variable quality, accuracy, and vastly depend on testing capacity27. In this study we have considered that each country enforced the interventions at a different stage of the national epidemics. To build a meaningful model of mortality, we have assessed the timing of application of social distancing measures in respect to the date in which the first Covid-19 death has been notified in each individual country, and have also adjusted for the cumulative burden of Covid-19 cases up to the same date. To allow adjustment for the baseline level of the national epidemics, we have also considered important structural covariates. The mortality model displays good predictive power and accounts for variables such as urbanisation, population density, age structure of the population, number of hospital beds, volume of air passengers and geography, also including several interaction terms. Finally, most studies have estimated the short-term effect of public health measures on the Covid-19 pandemic9 , 10 , 24, while we have studied a longer time-period, hoping to be more informative to policy makers28.
Nonetheless, our study has several limitations. Over the study period, countries have enacted multiple social distancing interventions, including closing schools, workplaces, prohibiting large gatherings, but also increased healthcare funding29, increased supply of ventilators, masks and protective equipments30, deployment of healthcare professionals5, or mobile phone apps for tracing Covid-19 contacts31 , 32. We cannot exclude that a portion of the predicted effect may have been related to other, concurrent, policies applied. This is a common, yet important, limitation of these kind of studies9 , 10. When governments decide to act, this usually involves a number of health policy interventions, which are implemented over a small timeframe, thus, completely isolating the effect of each single intervention is deemed impossible9. Other authors, however, have shown that there is a diminishing effect when considering more than one physical distancing intervention, and that adding additional measures over school closures, workplace closures, mass gatherings ban did not reduce Covid-19 incidence further10.
In comparison with interrupted time series analysis, the study approach does not rely on any explicit assumption regarding the slope of the epidemic curve in each single country;[9,10] thus, the model cannot infer what would have happened had these countries never applied the measures. Nonetheless, this approach permits using the marginal estimates of the overall model to provide a robust estimate of the potential effect the timing of such interventions may exert on Covid-19 cumulative mortality using the entire sample. To infer about the timing of interventions, previous studies had to rely on stratified analyses and, as stated by the authors, their conclusion on this topic should be interpreted with caution.9 , 10
Finally, Covid-19 deaths could be underreported especially in countries with a very high Covid-19 mortality5. However, using Covid-19 cases as the outcome variable would have been a much weaker approach for the reasons discussed previously.
Despite limitations, the timing of social distancing interventions has a strong and consistent effect on Covid-19 mortality. Our findings suggest the need for a very timely and concurrent application of mass gathering bans and school closures in national outbreak epicentres. We have confirmed previous preliminary evidence10 that closing schools earlier without concurrent enforcement of mass gatherings ban may have a small to null impact on the epidemic curve. In Europe and USA, schools reopening has been associated with a new wave of Covid-19 cases in the end of September to beginning of October 2020. Our study suggests that keeping mass gatherings ban enforced and apply school closures in outbreak epicentres as soon as significant local surges of new cases are identified may be an effective containment strategy to reduce Covid-19 mortality. Local and temporary school closures may be an effective and sustainable containment measure in many countries. Country-wide school closures for extended periods of time disrupt everyday life by modifying schedules, affecting how people travel and engage in group activities9, and may have detrimental consequences to the social-emotional, behavioural, and mental health development of children and adolescents33. To be able to act early and avoid country-wide school closures, governmental testing capacity should be increased, and aggressive and comprehensive testing strategies should be implemented at the general population level and in schools34, 35, 36.
The findings support the hypothesis that countries applying social distancing interventions at an earlier stage of the national epidemics may be more likely to keep the viral spread below a certain growth threshold, and that possibly, a more effective containment of the epidemic at the initial stage, might help reducing Covid-19 cumulative mortality over longer periods. This study provides useful information that may help health policy makers to plan the optimal timing of social distancing measures in upcoming pandemic waves.
Further research is warranted to verify whether the timing of other types of health policy interventions is associated with reduced Covid-19 mortality over meaningful periods of time, and to study the optimal sequence of such interventions in the short, medium and long term. Additional research is needed on the effectiveness of several interventions for which there is still scant evidence about their potential to reduce Covid-19 mortality. More work is needed to improve the reliability and accuracy of data on Covid-19 cases, testing capacity and, to a lesser extent deaths, to allow for meaningful cross-country comparisons. More efforts should be put into considering the compliance to different health policy interventions. Finally, additional research should investigate the impact of lifting different interventions over time, to permit governments to dynamically and effectively gauge the benefit-risk balance of health policy actions on national epidemic curves.
Contributors
GKN, SB and PB conceptualised the study with input from the co-authors. DP performed the statistical analysis and prepared the first draft of the manuscript with statistical inputs and oversight from SB. All authors are guarantors for the study. All authors revised the manuscript, provided critical scholarly feedback, and approved the final version of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Not required as data are anonymised, aggregated without any personal information, and publicly available.
Data sharing
All the data used in this study are publicly available and properly cited. However, all the data used in this study will be made available upon request.
Declaration of Competing Interest
None
References
- 1.World Health Organization. WHO Coronavirus Disease (COVID-19) dashboard. Accessed 1 October 2020. Available at: https://covid19.who.int/
- 2.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devi S. Travel restrictions hampering COVID-19 response. Lancet. 2020;395:1331–1332. doi: 10.1016/S0140-6736(20)30967-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cauchemez S., Kiem C.T., Paireau J. Lockdown impact on COVID-19 epidemics in regions across metropolitan France. Lancet. 2020;396:1068–1069. doi: 10.1016/S0140-6736(20)32034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hale T., Petherick A., Phillips T. Variation in government responses to COVID-19. Blavatnik Sch Gov. 2020 https://www.bsg.ox.ac.uk/sites/default/files/2020-05/BSG-WP-2020-032-v6.0.pdf Available at: [Google Scholar]
- 8.Gudbjartsson D.F., Helgason A., Jonsson H. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382:2302–2315. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auger K.A., Shah S.S., Richardson T. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA. 2020;324:859–870. doi: 10.1001/jama.2020.14348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Islam N., Sharp S.J., Chowell G. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020;370:m2743. doi: 10.1136/bmj.m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dehning J., Zierenberg J., Spitzner F.P. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369:eabb9789. doi: 10.1126/science.abb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsiang S., Allen D., Annan-Phan S. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584:262–267. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 13.Flaxman S., Mishra S., Gandy A. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 14.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng Z., Peng F., Xu B. Risk factors of critical and mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81:e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popkin B.M., Du S., Green W.D. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21:e13128. doi: 10.1111/obr.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauer S.A., Grantz K.H., Bi Q. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beigel J.H., Tomashek K.M., Dodd L.E. Remdesivir for the treatment of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007764. [DOI] [PubMed] [Google Scholar]
- 19.Ballinger G. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2004;7:127–150. [Google Scholar]
- 20.Fitzmaurice G.M., Laird N.M., Ware J.H. Wiley-Interscience; Hoboken NJ: 2004. Applied longitudinal analysis. [Google Scholar]
- 21.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12:308–333. [Google Scholar]
- 22.Cameron A.C., Trivedi P.K. Cambridge University Press; New York: 2005. Microeconometrics: Methods and Applications. [Google Scholar]
- 23.Royston P. marginscontplot: plotting the marginal effects of continuous predictors. Stata J. 2013;13:510–527. [Google Scholar]
- 24.Pan A., Liu L., Wang C. Association of public health interventions with the epidemiology of the covid-19 outbreak in Wuhan, China. JAMA. 2020;323:1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cowling B.J., Ali S.T., Ng T.W.Y. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.xxx . Department of Health; 2011. Pandemic Influenza Preparedness Team Scientific summary of pandemic influenza and its mitigation: scientific evidence base review. [Google Scholar]
- 27.Floyd T., Rogers J. Lockdown-type measures look effective against covid-19. BMJ. 2020;370:m2809. doi: 10.1136/bmj.m2809. [DOI] [PubMed] [Google Scholar]
- 28.Kupferschmidt K. Ending coronavirus lockdowns will be a dangerous process of trial and error. Science. 2020 doi: 10.1126/science.abc2507. [DOI] [Google Scholar]
- 29.Legido-Quigley H., Asgari N., Teo Y.Y. Are high-performing health systems resilient against the COVID-19 epidemic. Lancet. 2020;395:848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages – the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 31.Tian H., Liu Y., Li Y. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buckee C.O., Balsari S., Chan J. Aggregated mobility data could help fight COVID-19. Science. 2020;368:145–146. doi: 10.1126/science.abb8021. [DOI] [PubMed] [Google Scholar]
- 33.The Lancet Child & Adolescent Health . Pandemic school closures: risks and opportunities. Vol. 4. Lancet Child Adolesc Health; 2020. p. 341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The Lancet COVID-19: too little, too late? Lancet. 2020;395:755. doi: 10.1016/S0140-6736(20)30522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Lancet COVID-19 in the USA: a question of time. Lancet. 2020;395:1229. doi: 10.1016/S0140-6736(20)30863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beeching N.J., Fletcher T.E., Beadsworth M.K.J. Covid-19: testing times. BMJ. 2020;369:m1403. doi: 10.1136/bmj.m1403. [DOI] [PubMed] [Google Scholar]