Abstract
Introduction
Frontal fibrosing alopecia (FFA) is a lymphocytic primary cicatricial alopecia typically involving the frontotemporal hairline. It may be associated with the presence of facial papules (FP) that clinically appear as noninflammatory, monomorphic, white-yellowish papules. Lichen planus pigmentosus (LPPigm) is characterized by the presence of asymptomatic grayish pigmented macules, predominantly in sun-exposed and flexural areas.
Case Report
A 58-year-old, Caucasian, phototype III woman presented with a symmetrical, band-like, frontotemporal alopecia with regression of the hairline; bilateral eyebrow loss; diffuse, symmetrical hyperpigmentation of the face; and some asymptomatic, flesh-colored, monomorphic papules on the chin. Based on clinical, dermoscopic, and histological findings, the diagnosis of FFA associated with FP and LPPigm was established.
Discussion/Conclusion
The peculiarity of our report is represented by the triple association of FFA, FP, and LPPigm in a Caucasian skin type III woman, as it has been rarely reported. Clinicians should be aware of this association also in subjects with phototype ≤III, as its recognition may be useful for diagnostic and prognostic purposes: the observation of LPPigm of the face may suggest to check for early FFA, and in case of FFA associated with FP, a poorer FFA prognosis may likely be expected.
Keywords: Frontal fibrosing alopecia, Facial papules, Lichen planus pigmentosus, Dermoscopy, Lichen planus, Scarring alopecia, Hyperpigmentation, Quality of life
Established Facts
In the last few years, there has been a dramatic increase in cases of frontal fibrosing alopecia (FFA) reported worldwide.
The association of FFA, facial papules, and lichen pigmentosus has been reported mainly in subjects with phototype ≥IV.
Novel Insights
We report the association of FFA, facial papules, and lichen pigmentosus in a phototype III Caucasian woman.
Clinicians should be aware of this association also in subjects with fair skin, as it may be useful for diagnostic and prognostic purposes.
Introduction
Frontal fibrosing alopecia (FFA) is a lymphocytic primary cicatricial alopecia presenting with band-like scarring hair loss typically involving the frontotemporal region of the scalp, although upper preauricular and occipital localization may occur. The disease affects more frequently Caucasian postmenopausal women; however, around 20% of cases occurs in premenopausal women and few cases (1–2%) in men [1, 2]. The pathogenesis is still unknown, and several hypotheses have been proposed about genetic basis and possible triggering factors (hormones, neurogenic inflammation, smoking, UV filters, and ingredients in leave-on facial products) [3, 4, 5, 6, 7]. Loss of eyebrows is a common feature (50–80% of cases) of FFA and hairs of other body areas are less often involved [8, 9, 10, 11, 12, 13].
FFA may be associated with the presence of facial papules (FP) that clinically appear as noninflammatory, monomorphic, white-yellowish follicular papules, in a cobblestone-like pattern distribution and usually involving the temporal areas, which are commonly asymptomatic, although rarely they may be accompanied by an intense burning or itching sensation [14]. Although some authors have proposed that FP are secondary to fibrosed vellus hairs [12, 15, 16], more recently, prominent sebaceous lobules with dilated ducts associated with an abnormal elastic framework have been described as main histopathological findings [17].
Lichen planus pigmentosus (LPPigm) is characterized by the presence of persistent and asymptomatic grayish pigmented macules, predominantly in sun-exposed and flexural areas with symmetrical distribution. It is a disease of the middle-aged, with onset in the third to fourth decades of life and a slightly greater incidence in females. It is more common in darker Fitzpatrick phototypes (IV–V). The etiology is still unclear, although it is thought to be a type hypersensitivity IV reaction to unknown antigen with lichenoid inflammation, leading to melanin incontinence and superficial dermal pigmentation [18, 19, 20, 21, 22, 23, 24]. Some chemical and physical agents (hepatitis C virus, allyl isothiocyanate present in mustard oil, amla oil, cosmetics such as hair dye, fragrances, nickel, and UV radiations) may play an important pathogenetic role [19, 20, 24]. LPPigm needs to be differentiated from other causes of acquired dermal macular hyperpigmentation, such as exogenous ochronosis, melasma, ashy dermatosis, and pigmented contact dermatitis/Riehl's melanosis [25, 26, 27]. Herein, we report the clinical, dermoscopic, and histological findings of a rare association of FFA, LPPigm, and FP in a Caucasian woman.
Case Report
A 58-year-old, Caucasian, phototype III, postmenopausal woman presented to our clinic with an 8-year history of progressive hair loss of the frontotemporal scalp and bilateral eyebrow loss. She also developed an asymptomatic hyperpigmentation on the face from about 1 year. The patient reported the use of topical cosmetic products for hair loss and hair dye and a treatment with platelet-rich plasma injections without beneficial results. She denied any styling practices implying traction or chemical processes.
Clinical examination revealed a symmetrical, band-like, frontotemporal hair loss with a 3-cm regression of the hairline. The hairless scalp appeared pale, smooth, and slightly shiny with visible temporal veins. The patient also had bilateral eyebrow loss and was tattooed to improve her cosmetic appearance. Moreover, a diffuse, symmetrical hyperpigmentation of the face mainly involving the cheeks and the periocular and temporal regions, with grayish-blue macules of various sizes and irregular and poorly defined borders were evident (shown in Fig. 1). Finally, some asymptomatic, flesh-colored, monomorphic papules were present on the chin (shown in Fig. 2). The examination of visible mucosae and nails did not reveal any abnormality.
Fig. 1.
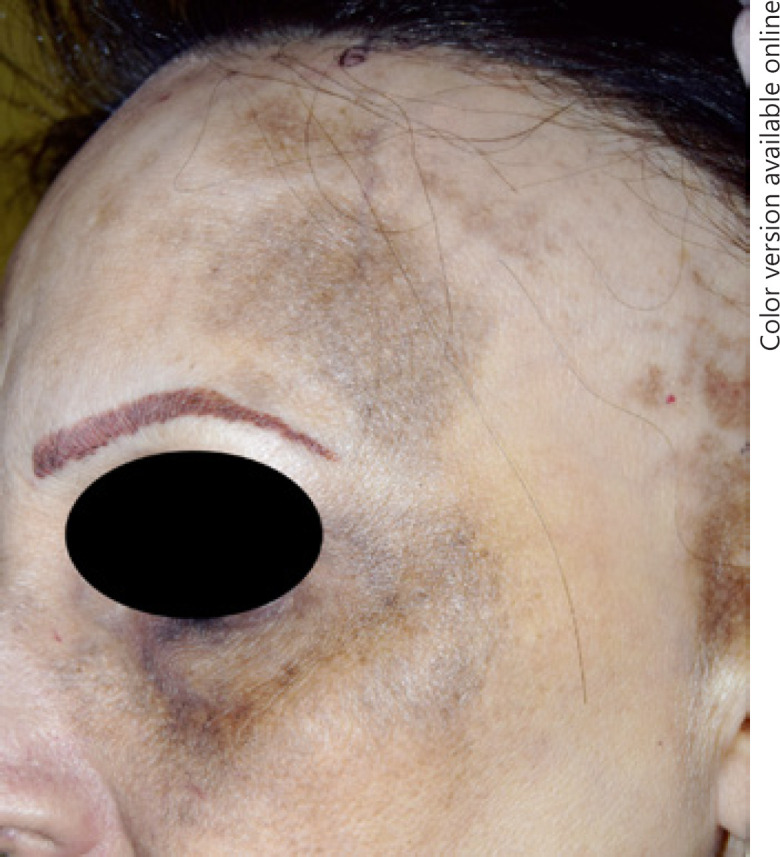
A 58-year-old, Caucasian, phototype III woman showing a band-like, frontotemporal hair loss with regression of the hairline, eyebrow loss, and a hyperpigmentation of the face involving the cheeks and the periocular and temporal areas.
Fig. 2.

The same patient showed asymptomatic, flesh-colored, monomorphic papules and hyperpigmentation of the chin.
Polarized dermoscopy (×10, Illuco IDS-1100®; Tre T Medical, Camposano, Italy) showed absence of follicular openings on the frontotemporal hairless scalp, absence of vellus hair at the level of the hairline, and perifollicular hyperkeratosis of the terminal hairs, all suggestive of FFA (shown in Fig. 3). Polarized dermoscopy of the pigmented macules of the face showed a grey-blue “dotted/speckled” pattern characterized by the presence of slate grey-to-blue dots and globules, and perifollicular pigmentation (“pseudonetwork” pattern) (shown in Fig. 4). Finally, papules of the chin showed at dermoscopy a homogeneous whitish aspect.
Fig. 3.
Polarized dermoscopy (×10) showing absence of follicular openings on the frontotemporal hairless scalp, absence of vellus hair at the level of the hairline, and perifollicular hyperkeratosis of the terminal hairs.
Fig. 4.
Polarized dermoscopy (×10) of the pigmented macules of the face showing a grey-blue “dotted/speckled” pattern characterized by the presence of slate grey-to-blue dots and globules, and perifollicular pigmentation (“pseudonetwork” pattern).
Histopathologic examination of a biopsy from the frontal hairline area confirmed the diagnosis of scarring alopecia, with fibrosis and mild perifollicular lymphohistiocytic inflammatory infiltrate in the upper dermis. Histopathology of the hyperpigmented skin of the temporal region showed a dermal lichenoid lymphohistiocytic infiltrate with basal cell degeneration, pigmentary incontinence, and dermal melanophages. Routine hematological and biochemical parameters were normal. Based on clinical, dermoscopic [28, 29], and histological findings, the diagnosis of FFA associated with LPPigm and FP was established.
Discussion
The peculiarity of our report is represented by the triple association of FFA, FP, and LPPigm in a Caucasian, skin type III woman. FFA and LPPigm are 2 clinical variants included in the wide spectrum of lichen planus [30]. Their association was first reported by Dlova [31] in 24 Afro-Americans (23 females, 1 male). Later, about 100 cases have been reported worldwide [30, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43]. Epidemiologic data of the association are conflicting, due to the lack of large case series. Some authors reported that it occurs more frequently in premenopausal women (age range: 25–56 years), while others showed a more frequent involvement of postmenopausal age [31, 39, 40]. Moreover, in some studies, FFA precedes the onset of LPPigm, in others LPPigm proceeds to FFA [31, 37, 39, 42]. Interestingly, the association between FFA and LPPigm is rare in Caucasian women with 9 skin phototype ≤III reported cases [32, 35, 39, 40].
The concomitant presence of FFA and FP is variably reported ranging from 3 to 22% [44], whereas the triple association of FFA, LPPigm, and FP has been reported in 29 patients [15, 31, 39, 40]. To our knowledge, the association in Caucasians with fair skin (Fitzpatrick type ≤III) has been reported in 3 patients only [39].
In the last few years, there has been a dramatic increase in cases of FFA reported worldwide, and the possible presence of LPPigm and FP suggests that the inflammatory process may be systemic and not limited to the scalp [45]. Moreover, as FFA may negatively influence patient's quality of life with relevant psychological distress, the association with LPPigm and/or other facial changes may further worsen its impact [46].
Clinicians should be aware of this association also in subjects with phototype ≤III, as its recognition may be useful for diagnostic and prognostic purposes: the observation of LPPigm of the face may suggest to check for early FFA, and in case of FFA associated with FP, a poorer FFA prognosis may likely be expected [15, 36, 47].
Statement of Ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient has given her written informed consent to publish photos and details of the case.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding.
Author Contributions
A.E.V., F.L., F.D., and G.M. (1) made substantial contributions to the conception or design of the work, or to the acquisition, analysis, or interpretation of data for the work; (2) participated in drafting the work or revising it critically for important intellectual content; (3) approved the final version to be published; and (4) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- 1.Banka N, Mubki T, Bunagan MJ, McElwee K, Shapiro J. Frontal fibrosing alopecia: a retrospective clinical review of 62 patients with treatment outcome and long-term follow-up. Int J Dermatol. 2014;53((11)):1324–30. doi: 10.1111/ijd.12479. [DOI] [PubMed] [Google Scholar]
- 2.Samrao A, Chew AL, Price V. Frontal fibrosing alopecia: a clinical review of 36 patients. Br J Dermatol. 2010;163((6)):1296–300. doi: 10.1111/j.1365-2133.2010.09965.x. [DOI] [PubMed] [Google Scholar]
- 3.Aldoori N, Dobson K, Holden CR, McDonagh AJ, Harries M, Messenger AG. Frontal fibrosing alopecia: possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol. 2016;175((4)):762–7. doi: 10.1111/bjd.14535. [DOI] [PubMed] [Google Scholar]
- 4.Callander J, Frost J, Stone N. Ultraviolet filters in hair-care products: a possible link with frontal fibrosing alopecia and lichen planopilaris. Clin Exp Dermatol. 2018;43((1)):69–70. doi: 10.1111/ced.13273. [DOI] [PubMed] [Google Scholar]
- 5.Iorizzo M, Tosti A. Frontal fibrosing alopecia: an update on pathogenesis, diagnosis, and treatment. Am J Clin Dermatol. 2019;20((3)):379–90. doi: 10.1007/s40257-019-00424-y. [DOI] [PubMed] [Google Scholar]
- 6.Moreno-Arrones OM, Saceda-Corralo D, Rodrigues-Barata AR, Castellanos-González M, Fernández-Pugnaire MA, Grimalt R, et al. Risk factors associated with frontal fibrosing alopecia: a multicentre case-control study. Clin Exp Dermatol. 2019;44((4)):404–10. doi: 10.1111/ced.13785. [DOI] [PubMed] [Google Scholar]
- 7.Photiou L, Nixon RL, Tam M, Green J, Yip L. An update of the pathogenesis of frontal fibrosing alopecia: what does the current evidence tell us? Australas J Dermatol. 2019;60((4)):335–6. doi: 10.1111/ajd.13128. [DOI] [PubMed] [Google Scholar]
- 8.Bolduc C, Sperling LC, Shapiro J. Primary cicatricial alopecia: lymphocytic primary cicatricial alopecias, including chronic cutaneous lupus erythematosus, lichen planopilaris, frontal fibrosing alopecia, and Graham-Little syndrome. J Am Acad Dermatol. 2016;75((6)):1081–99. doi: 10.1016/j.jaad.2014.09.058. [DOI] [PubMed] [Google Scholar]
- 9.Chew AL, Bashir SJ, Wain EM, Fenton DA, Stefanato CM. Expanding the spectrum of frontal fibrosing alopecia: a unifying concept. J Am Acad Dermatol. 2010;63((4)):653–60. doi: 10.1016/j.jaad.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 10.Faulkner CF, Wilson NJ, Jones SK. Frontal fibrosing alopecia associated with cutaneous lichen planus in a premenopausal woman. Australas J Dermatol. 2002;43((1)):65–7. doi: 10.1046/j.1440-0960.2002.00558.x. [DOI] [PubMed] [Google Scholar]
- 11.Kossard S, Lee MS, Wilkinson B. Postmenopausal frontal fibrosing alopecia: a frontal variant of lichen planopilaris. J Am Acad Dermatol. 1997;36((1)):59–66. doi: 10.1016/s0190-9622(97)70326-8. [DOI] [PubMed] [Google Scholar]
- 12.Tan KT, Messenger AG. Frontal fibrosing alopecia: clinical presentations and prognosis. Br J Dermatol. 2009;160((1)):75–9. doi: 10.1111/j.1365-2133.2008.08861.x. [DOI] [PubMed] [Google Scholar]
- 13.To D, Beecker J. Frontal fibrosing alopecia: update and review of challenges and successes. J Cutan Med Surg. 2018;22((2)):182–9. doi: 10.1177/1203475417736279. [DOI] [PubMed] [Google Scholar]
- 14.López-Pestaña A, Tuneu A, Lobo C, Ormaechea N, Zubizarreta J, Vildosola S, et al. Facial lesions in frontal fibrosing alopecia (FFA): clinicopathological features in a series of 12 cases. J Am Acad Dermatol. 2015;73((6)):987.e1–6. doi: 10.1016/j.jaad.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 15.Krueger L, Svigos K, Brinster N, Elbuluk N. Frontal fibrosing alopecia: cutaneous associations in women with skin of color. Cutis. 2018;102((5)):335–8. [PubMed] [Google Scholar]
- 16.Donati A, Molina L, Doche I, Valente NS, Romiti R. Facial papules in frontal fibrosing alopecia: evidence of vellus follicle involvement. Arch Dermatol. 2011;147((12)):1424–7. doi: 10.1001/archdermatol.2011.321. [DOI] [PubMed] [Google Scholar]
- 17.Pirmez R, Barreto T, Duque-Estrada B, Quintella DC, Cuzzi T. Facial papules in frontal fibrosing alopecia: beyond vellus hair follicle involvement. Skin Appendage Disord. 2018;4((3)):145–9. doi: 10.1159/000481695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cobos G, Kim RH, Meehan S, Elbuluk N. Lichen planus pigmentosus and lichen planopilaris. Dermatol Online J. 2016;22((12)):13030/qt7hp8n6dn. [PubMed] [Google Scholar]
- 19.Gupta D, Thappa DM. Dermatoses due to Indian cultural practices. Indian J Dermatol. 2015;60((1)):3–12. doi: 10.4103/0019-5154.147778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanwar AJ, Dogra S, Handa S, Parsad D, Radotra BD. A study of 124 Indian patients with lichen planus pigmentosus. Clin Exp Dermatol. 2003;28((5)):481–5. doi: 10.1046/j.1365-2230.2003.01367.x. [DOI] [PubMed] [Google Scholar]
- 21.Rieder E, Kaplan J, Kamino H, Sanchez M, Pomeranz MK. Lichen planus pigmentosus. Dermatol Online J. 2013;19((12)):20713. [PubMed] [Google Scholar]
- 22.Savoia F, Sacchelli L, Tabanelli M, Neri I, Sechi A, Baraldi C, et al. Lichen planus pigmentosus: a case series with different ethnical, clinical and dermoscopic features. G Ital Dermatol Venereol. 2019 Feb 4; doi: 10.23736/S2784-8671.19.06242-4. [DOI] [PubMed] [Google Scholar]
- 23.Schneider MR, Schmidt-Ullrich R, Paus R. The hair follicle as a dynamic miniorgan. Curr Biol. 2009;19((3)):R132–42. doi: 10.1016/j.cub.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Vachiramon V, Suchonwanit P, Thadanipon K. Bilateral linear lichen planus pigmentosus associated with hepatitis C virus infection. Case Rep Dermatol. 2010;2((3)):169–72. doi: 10.1159/000320775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang L, Xu AE. Four views of Riehl's melanosis: clinical appearance, dermoscopy, confocal microscopy and histopathology. J Eur Acad Dermatol Venereol. 2014;28((9)):1199–206. doi: 10.1111/jdv.12264. [DOI] [PubMed] [Google Scholar]
- 26.Errichetti E, Stinco G. The practical usefulness of dermoscopy in general dermatology. G Ital Dermatol Venereol. 2015;150((5)):533–46. [PubMed] [Google Scholar]
- 27.Errichetti E, Angione V, Stinco G. Dermoscopy in assisting the recognition of ashy dermatosis. JAAD Case Rep. 2017;3((6)):482–4. doi: 10.1016/j.jdcr.2017.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lacarrubba F, Micali G, Tosti A. Absence of vellus hair in the hairline: a videodermatoscopic feature of frontal fibrosing alopecia. Br J Dermatol. 2013;169((2)):473–4. doi: 10.1111/bjd.12316. [DOI] [PubMed] [Google Scholar]
- 29.Dai H, Jiang HY, Xu AE. Detection of lichen planus pigmentosus with dermoscopy and reflectance confocal microscopy. Skin Res Technol. 2018;24((4)):699–700. doi: 10.1111/srt.12475. [DOI] [PubMed] [Google Scholar]
- 30.Berliner JG, McCalmont TH, Price VH, Berger TG. Frontal fibrosing alopecia and lichen planus pigmentosus. J Am Acad Dermatol. 2014;71((1)):e26–7. doi: 10.1016/j.jaad.2013.12.031. [DOI] [PubMed] [Google Scholar]
- 31.Dlova NC. Frontal fibrosing alopecia and lichen planus pigmentosus: is there a link? Br J Dermatol. 2013;168((2)):439–42. doi: 10.1111/j.1365-2133.2012.11146.x. [DOI] [PubMed] [Google Scholar]
- 32.Franco-Muñoz M, García-Arpa M, Lozano-Masdemont B, Ramos-Rodríguez C. Frontal fibrosing alopecia and extrafacial lichen planus pigmentosum in a caucasian woman. An Bras Dermatol. 2017;92((5 Suppl 1)):76–8. doi: 10.1590/abd1806-4841.20176638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gavazzoni Dias MFR, Rezende HD, Lofeu Cury A, Trüeb RM, Vilar E. Hyperpigmented upper eyelid: a clue to the diagnosis of facial lichen planus pigmentosus in a patient with frontal fibrosing alopecia. Skin Appendage Disord. 2018;4((4)):335–8. doi: 10.1159/000487338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumaran MS, Razmi T M, Vinay K, Parsad D. Clinical, dermoscopic, and trichoscopic analysis of frontal fibrosing alopecia associated with acquired dermal macular hyperpigmentation: a cross sectional observational case-control study. J Am Acad Dermatol. 2018;79((3)):588–91. doi: 10.1016/j.jaad.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Kushner CJ, Concha JSS, Pearson DR, Werth VP. Lichen planus pigmentosus and frontal fibrosing alopecia mimicking discoid lupus erythematosus. Arthritis Rheumatol. 2019;71((3)):478. doi: 10.1002/art.40779. [DOI] [PubMed] [Google Scholar]
- 36.Mervis JS, Borda LJ, Miteva M. Facial and extrafacial lesions in an ethnically diverse series of 91 patients with frontal fibrosing alopecia followed at a single center. Dermatology. 2019;235((2)):112–9. doi: 10.1159/000494603. [DOI] [PubMed] [Google Scholar]
- 37.Mulinari-Brenner FA, Guilherme MR, Peretti MC, Werner B. Frontal fibrosing alopecia and lichen planus pigmentosus: diagnosis and therapeutic challenge. An Bras Dermatol. 2017;92((5 Suppl 1)):79–81. doi: 10.1590/abd1806-4841.20175833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rao R, Sarda A, Khanna R, Balachandran C. Coexistence of frontal fibrosing alopecia with lichen planus pigmentosus. Int J Dermatol. 2014;53((5)):622–4. doi: 10.1111/j.1365-4632.2012.05630.x. [DOI] [PubMed] [Google Scholar]
- 39.Romiti R, Biancardi Gavioli CF, Anzai A, Munck A, Costa Fechine CO, Valente NYS. Clinical and histopathological findings of frontal fibrosing alopecia-associated lichen planus pigmentosus. Skin Appendage Disord. 2017;3((2)):59–63. doi: 10.1159/000456038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pirmez R, Duque-Estrada B, Donati A, Campos-do-Carmo G, Valente NS, Romiti R, et al. Clinical and dermoscopic features of lichen planus pigmentosus in 37 patients with frontal fibrosing alopecia. Br J Dermatol. 2016;175((6)):1387–90. doi: 10.1111/bjd.14722. [DOI] [PubMed] [Google Scholar]
- 41.Robles-Méndez JC, Rizo-Frías P, Herz-Ruelas ME, Pandya AG, Ocampo Candiani J. Lichen planus pigmentosus and its variants: review and update. Int J Dermatol. 2018;57((5)):505–14. doi: 10.1111/ijd.13806. [DOI] [PubMed] [Google Scholar]
- 42.Uwakwe LN, Cardwell LA, Dothard EH, Baroudi BI, McMichael AJ. Frontal fibrosing alopecia and concomitant lichen planus pigmentosus: a case series of seven African American women. J Drugs Dermatol. 2018;17((4)):397–400. [PubMed] [Google Scholar]
- 43.Walker JL, Robinson-Bostom L, Landow S. Four diseases, two associations, one patient: a case of frontal fibrosing alopecia, lichen planus pigmentosus, acne rosacea, and morbihan disease. Skinmed. 2016;14((3)):225–8. [PubMed] [Google Scholar]
- 44.Flores-Terry MÁ, García-Arpa M, Franco-Muñóz M, González-Ruiz L. Facial papules in frontal fibrosing alopecia: good response to isotretinoin. Actas Dermosifiliogr. 2018;109((9)):831–3. doi: 10.1016/j.ad.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 45.Mirmirani P, Tosti A, Goldberg L, Whiting D, Sotoodian B. Frontal fibrosing alopecia: an emerging epidemic. Skin Appendage Disord. 2019;5((2)):90–3. doi: 10.1159/000489793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saceda-Corralo D, Pindado-Ortega C, Moreno-Arrones ÓM, Fernández-González P, Rodrigues-Barata AR, Jaén-Olasolo P, et al. Health-related quality of life in patients with frontal fibrosing alopecia. JAMA Dermatol. 2018;154((4)):479–80. doi: 10.1001/jamadermatol.2017.6330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dhurat R, Shukla D, Dandale A, Ghate S, Agrawal S, Shanshanwal S. Early diagnosis and prompt treatment improves quality of life in patients with frontal fibrosing alopecia. Skin Appendage Disord. 2019 Apr;5((3)):172–6. doi: 10.1159/000495117. [DOI] [PMC free article] [PubMed] [Google Scholar]




