Abstract
Self-myofascial release (SMR) is a popular method to potentially increase the compliance and extensibility of the fascia and reduce muscle stiffness. The purpose of this study was to examine the acute effects of posterior muscle chain SMR on flexibility, vertical jump performance and balance ability. Eighteen young participants volunteered to take part in this crossover design study. They performed two self-massage sessions in randomized order separated by at least one week. One session consisted of posterior muscle chain SMR whereas the other one was performed on the upper limbs as a control intervention (CON). Flexibility was measured with the Toe Touch Test (TTT), Weight-Bearing Lunge Test (WBLT), and Straight Leg Raise Test (SLR). Jump performance was evaluated during a squat jump, a counter movement jump and a stiffness jump. Dynamic balance ability was assessed through the Star Excursion Balance Test. All these variables were measured before and after each intervention. A significant increase in flexibility (+3.5 ± 1.8 cm, +1.6 ± 1.0°, and +7.7 ± 4.0° for the TTT, WLBT, and SLR, respectively, p < 0.003) and balance performance (4.8 ± 3.9 cm, p < 0.003) was observed following SMR intervention compared to CON. Conversely, jumping performance was unchanged in both groups. SMR improves joint flexibility and dynamic balance ability.
Key words: roller massage, foam rolling, range of motion, jumping performance, balance ability
Introduction
The fascia is a type of connective tissue that surrounds the nerves, blood vessels, but also tendons, ligaments and muscles. The myofascial network ensures the maintenance and consistency of skeletal muscle structures promoting the sliding between muscle structures, the transmission of muscular forces and the protection against muscle damage. It has been reported that when myofascia becomes dehydrated and loses its elasticity, this can lead to impaired structural alignment, decreased strength and endurance, as well as motor coordination (Barnes, 1997). During the last decade, self-myofascial release (SMR) has become a popular method which influences muscle and myofascial structures by increasing the compliance and extensibility of the fascia (Mohr et al., 2014) and reduces passive muscle stiffness (Morales-Artacho et al., 2017). It may also reduce muscle pain by decreasing delayed onset muscle soreness after intense exercise (MacDonald et al., 2013; Pearcey et al., 2015).
More recently, a growing interest in self-myofascial release has emerged in sport, enabling the pursuance of the same goal as manual massage using the individual’s mass itself and massage instruments such as a foam roller or balls. SMR has been demonstrated to provide a wide range of positive gains in physical performance. The most well-known positive effect of SMR is a gain in flexibility assessed by an increased joint range of motion in sport and rehabilitation contexts (Halperin et al., 2014; MacDonald et al., 2013; Sullivan et al., 2013). For instance, Sullivan et al. (2013) demonstrated that an intermittent 4 trial roller-massage protocol performed on the hamstring muscles increased knee joint flexibility by 4.3% (Sullivan et al., 2013), partly due to a reduced motor unit firing rate, and subsequently decreased muscle tension (Tozzi, 2012). MacDonald et al. (2013) reported similar results after hamstring SMR with an increased knee joint range of motion of 12.7% and 10.3% at the 2nd and 10th minute after SMR, respectively. Furthermore, the gain in flexibility after SMR was reported to be similar to those obtained after stretching interventions (Su et al., 2017). However, stretching interventions can negatively impact muscle performance (Behm and Kibele, 2007; Marchetti et al., 2014), while SMR was shown to have controversial effects on muscular performance. Sullivan et al. (2013) found no change in maximal isometric knee flexion torque after 1 or 2 bouts of 5 or 10 s of roller massage. In contrast, Su et al. (2017) indicated that the knee extension peak torque was increased after foam rolling massage. Moreover, Bradbury-Squires et al. (2015) demonstrated an increased neuromuscular efficiency during lunge (i.e., reduced VL EMG) as a result of roller massager application. Peacock et al. (2015) did not report any change in vertical jump performance after SMR sessions. Yet, a potential benefit of SMR to jump performance could be expected considering the decrease in muscular stiffness reported after SMR (Morales-Artacho et al., 2017) and then an increased ability to store elastic potential energy during the muscle lengthening phase of the vertical jump, especially the counter-movement jump (CMJ), as previously reported for triceps surae muscles after plyometric training (Fouré et al., 2011). Due to the variety in the design of SMR protocols, it remains difficult to determine the real effect of SMR on muscle force capacities and jump performance.
While there are numerous reports of SMR or myofascial therapy effects on joint flexibility and jump performance, only few studies have focused on dynamic balance ability and results have been quite controversial. Halperin et al. (2014) showed that static balance on one leg was not influenced by SMR. Junker and Stöggl (2019) reported that 4 weeks of SMR intervention on lower leg muscles had no effect on the dynamic balance ability using the Y balance test. Castro-Sanchez et al. (2011) assessed the effects of myofascial therapy on postural stability over a 20-week period, but failed to observe any effect. In contrast, Sefton et al. (2012) reported that 60 min of full-body manual massage (e.g., pressure points, kneading, scalp) had a positive effect on balance performance measured on a functional scale platform. In the latter study, manual therapy was assumed to increase body stability by reducing muscle coactivation. In addition, the proprioceptive effect of massage may also increase some of the determining factors of body balance (Shin and Sung, 2015). Concerning the potential effect of SMR as manual massage on the determining factors of balance ability, acute neuromuscular adaptations can be assumed such as proprioception improvement (Weerapong et al., 2005).
As described above, previous studies have indicated that SMR has a positive effect by improving flexibility, yet its influence on balance is still debated. Therefore, the aim of this study was to assess the immediate effect of posterior muscle chain SMR on flexibility, jump performance and dynamic balance ability in the same experimental population. We hypothesized that the immediate effect of SMR using the foam roller and double ball massage on the posterior muscle chain would improve flexibility and balance ability without decreasing jump performance.
Methods
Participants
Fourteen men (174 ± 4 cm, 73 ± 6 kg, 24 ± 2 years) and four women (162 ± 3 cm, 50 ± 8 kg, 23 ± 1 years) volunteered to participate in the present study. They were recreationally active (7 ± 2 hr/wk), but were not practicing any form of SMR. In addition, they had not suffered from lower limb injuries and had no history of surgery (e.g., ACL reconstruction, ankle sprain) in the 6 months preceding the study. The study was approved by the local ethics committee, “Sud-Est II” of Lyon and all participants provided written informed consent. All procedures conformed to the standards of the last version of the Declaration of Helsinki. Leading up to the experiment, participants followed their regular physical activity, but avoided strenuous loading at least 48 hours prior to testing.
Measures
Flexibility tests
The Toe Touch Test (TTT) was performed to assess the mobility and flexibility of the lower back and hamstrings. Participants were seated, legs stretched forward, feet together and bent the hip joint as far as possible without bending the knee. The furthest distance from the tip of the fingers to the bench was recorded as the best performance of the three attempts.
The Weight-Bearing Lunge Test (WBLT) was used to assess ankle dorsiflexion range of motion. Participants stood barefoot in front of the wall with 10 cm between feet and the wall. They were asked to move one leg back and then lunge forward with the front knee toward the wall. Participants moved the front foot further away from the wall if the front knee could touch the wall or, on the contrary, moved the foot closer to the wall. Participants repeated this process until achieving the optimal distance between feet and the wall with the heal remaining in contact with the ground. The maximal distance from the toe to the wall was measured with a ruler and the best performance was recorded (i.e. maximal ankle joint range of motion in dorsiflexion).
The Straight Leg Raise (SLR) test was used to assess hamstring flexibility. The maximal hip leg-trunk angle attained without pain and change in the pelvis position was measured using a camera placed 2 m from the hip and perpendicular to the participant’s sagittal plane (Gopro, Silver 4, sampling frequency 250 Hz, resolution 1080 p). Kinovea (v.0.8.27) was used to assess the SLR performance (Nor Adnan et al., 2018). Before the test, two black circle markers (25 mm diameter) were positioned on the greater trochanter and external femoral condyle to improve the spatial tracking accuracy. Participants were in a supine position on a massage table and raised the leg with the knee fully extended and the pelvis in a neutral position. The hip angle during flexion was then measured relative to the horizontal axe. All the participants performed 3 attempts for each leg. The best performance was recorded as the maximal range of motion.
Jump tests
Participants performed the conventional vertical counter-movement jump (CMJ), squat jump (SJ) and stiffness jumps (STIF). Jump performances (i.e. jump height in cm) were measured using the Optojump system (Microgate, Bolzano, Italy). Participants performed 3 jumps for each test with a 30 s rest interval between each jump. The maximal performance for each modality was recorded for further analysis.
Balance Ability Test
The modified Star Excursion Balance Test (SEBT) was used to assess balance for both legs. Three labeled lines were extended from the center of the foot in anterior (ANT, at 90 degrees), posterolateral (PL, at 45 degrees) and posteromedial (PM, at 45 degrees) directions. Participants were instructed to maintain a single leg stance with a semi-flexed knee and hands on the hips while reaching with the other leg as far as possible along the three directions. Participants had to touch the furthest point possible on the line with the most distal part of their reach foot as lightly as possible using minimal pressure to ensure that the reach leg did not provide support in the maintenance of the upright posture and that stability was achieved through balance (Mtibaa et al., 2018). Participants returned to a bilateral stance while maintaining their equilibrium. The participant was asked to complete 5 trials of the SEBT and then each participant performed 3 trials in each of the three directions with 10 s recovery between subsequent attempts.
Design and procedures
A randomized crossover design was used for this study. The experimental session consisted of SMR on the posterior muscle chain (SMR), whereas the control session consisted of SMR on the upper limbs (CON). At least one week separated the two sessions that were performed at the same time of day. Each session was composed of a 15-min standardized warm-up followed by flexibility, jump performances, and balance assessments (PRE) performed in random order to avoid a potential systematic effect of each test on the others. Next, participants performed the SMR or CON session and immediately after (POST), the same assessments as for PRE (Figure 1).
Figure 1.
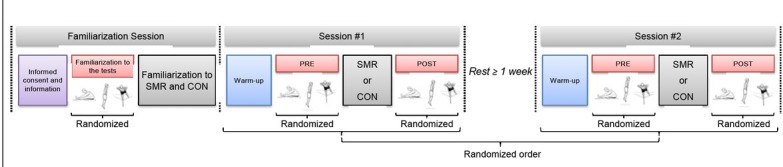
Experimental design. SMR: experimental intervention (Self-myofascial release on the posterior muscle chain), CON: control intervention (Self-myofascial release on the upper limbs). PRE: before SMR or CON, POST: after SMR or CON. Randomization was applied to determine the order of tests and sessions (cross-over design)
During the first familiarization session, all participants filled out a questionnaire concerning their age, sport experience, training volume and an injury report. Height and body mass were also measured. Participants were briefly introduced to the SMR instruments (i.e. foam roller, double balls) and the SMR movements were demonstrated by the experimenter. The instructions were standardized in order to provide all participants with the same information. During the two experimental sessions, participants performed a standardized warm-up that consisted of running at their self-paced velocity (15 min), submaximal squat jumps, counter movement jumps and stiffness jumps (5 jumps/modality with 30 s rest intervals between jumps). After the warm-up, participants performed the flexibility, jump and balance tests (Figure 1). Depending on the session, participants performed the SMR movements on the posterior muscle chain (SMR) or on the upper limbs (CON). Participants were instructed to roll the massage ball and the foam roller by applying the pressure with their bodyweight to reach discomfort yet without pain. The SMR experimental session was performed on the posterior muscle chain including the arches of the foot (60 s), calf muscles (80 s), hamstring muscles (80 s), gluteal muscles (50 s), lumbar muscles (50 s), and suboccipital muscles (40 s). SMR applications were interspaced with 10 s rest intrvals. The massage of the foot arches was performed using a simple ball (TRIGGERPOINT® MB, 6.6 cm diameter, 5 g), whereas a double ball massage (PROCIRCLE®, 12.7 cm length, 6.35 cm diameter, 400 g) was used for the massage of the suboccipital zone and a foam roller (TRIGGERPOINT® EVA, 33 cm length, 14 cm diameter, 650 g) for the other muscles. For the control session, SMR was performed with the ball massage on the arm muscles with progression order that included forearm muscles (90 s), deltoid muscles (90 s), biceps brachii muscle (90 s) and triceps brachii muscles (90 s) for similar total duration of 6 minutes. All testing sessions were performed in the same location, at the same temperature and at the same time of day.
Statistical Analysis
The interaction effects between time (PRE vs. POST; fixed effect) and groups (CON vs. SMR; fixed effect) were tested using linear mixed models. The p-value was determined with a type III ANOVA using Satterthwaite's degrees of freedom method. The level of significance was set at p < 0.0036 (Bonferroni correction: 0.05/14). A Tukey HSD post-hoc test was performed when appropriate. Cohen’s d value was calculated between the PRE and POST values for the SMR condition. The linearity and the homoscedasticity of the model residuals were graphically controlled. All models were executed from the package “lme4” (Bates et al., 2015), p-values were obtained using the package “lmerTest”(Kuznetsova et al., 2017) and post-hoc pairwise comparisons were performed with the R software package “multcomp” (R 3.5.0, RCore Team, Vienna, Austria).
Results
Flexibility tests: A significant interaction was observed between flexibility variables (p < 0.001). The SMR group improved flexibility performance by an increased score in SLR (11 ± 7%), TTT (50 ± 40%) and WBLT (22 ± 17%) (Table 1). Balance ability tests: An interaction was found for the balance variables measured with the SEBT except for the lateral and medial axis of the right leg for which no main effect was found (Table 1). It should be noted that the CON group was significantly more balanced on the medial axis for the left leg as compared to the SMR group before the intervention (p < 0.001). However, the SMR group improved their performance in the post-test and there was no difference after the intervention between groups. Post-hoc pairwise comparisons showed that the SMR group improved balance up to 8%. At the end of the intervention, the performance of the SMR group was better than the CON group on the anterior axis, and the lateral axis with the left leg (Table 1). Vertical jump performances: No interaction and no main effect in jump performances were found (p > 0.05). Jump performances were similar before and after the intervention for both the SMR and CON groups (Table 1).
Table 1.
Mean values (± SD) and relative changes in flexibility, balance, and power variables after self-myofascial release on the posterior muscle chain (SMR) and the control intervention (CON).
| Absolute data | Relative changes | |||||||
|---|---|---|---|---|---|---|---|---|
| SMR | CON | |||||||
| SMR | CON | |||||||
| PRE | POST | PRE | POST | |||||
| Flexibility | TTT (cm) | -5.92 ± 10.05 | -2.47 ± 10.10*,# | -5.27 ± 9.58 | -5.21 ± 9.79 | 3.5 ± 1.8 | 0.1 ± 0.6 | |
| WBLT (°) | Right | 7.99 ± 1.61 | 9.64 ± 1.64*,# | 7.79 ± 1.54 | 7.90 ± 1.52 | 1.6 ± 0.9 | 0.1 ± 0.3 | |
| Left | 8.62 ± 2.06 | 10.27 ± 2.01*,# | 8.75 ± 2.02 | 8.88 ± 2.08 | 1.6 ± 1.0 | 0.1 ± 0.3 | ||
| SLR (°) | Right | 75.00 ± 15.74 | 82.28 ± 16.23*,# | 73.17 ± 15.16 | 72.17 ± 14.63 | 7.3 ± 3.9 | -1.0 ± 2.9 | |
| Left | 72.50 ± 17.61 | 80.67 ± 16.34*,# | 74.22 ± 16.09 | 73.22 ± 15.26 | 8.2 ± 4.2 | -1.0 ± 1.8 | ||
| SEBT | ANT (cm) | Right | 58.63 ± 6.04 | 63.32 ± 7.11*,# | 59.58 ± 5.48 | 59.92 ± 4.98 | 4.7 ± 3.3 | 0.3 ± 1.2 |
| Left | 60.22 ± 5.97 | 64.92 ± 7.59*,# | 61.39 ± 5.47 | 61.17 ± 5.53 | 4.7 ± 2.9 | -0.2 ± 1.9 | ||
| PL (cm) | Right | 97.33 ± 6.16 | 100.53 ± 5.97 | 100.28 ± 6.00 | 101.92 ± 5.30 | 3.2 ± 5.1 | 1.6 ± 4.4 | |
| Left | 95.96 ± 7.63 | 102.44 ± 6.79*,# | 98.31 ± 6.32 | 98.61 ± 6.30 | 6.5 ± 3.3 | 0.3 ± 2.6 | ||
| PM (cm) | Right | 97.63 ± 6.86 | 102.07 ± 5.30 | 101.11 ± 5.29 | 100.81 ± 4.99 | 4.4 ± 4.2 | -0.3 ± 2.9 | |
| Left | 96.49 ± 6.15 | # 101.97 ± 6.21* | 101.11 ± 5.42 | 100.47 ± 5.00 | 5.5 ± 4.6 | -0.6 ± 2.4 | ||
| Jump Performance | SJ (cm) | 33.42 ± 8.91 | 32.47 ± 8.69 | 33.14 ± 8.80 | 32.38 ± 8.43 | -1.0 ± 1.9 | -0.8 ± 1.5 | |
| CMJ (cm) | 33.51 ± 8.43 | 33.15 ± 8.59 | 33.45 ± 8.93 | 33.11 ± 8.35 | -0.4 ± 2.0 | -0.3 ± 2.4 | ||
| STIF (cm) | 16.95 ± 9.15 | 17.17 ± 7.34 | 16.55 ± 6.83 | 17.52 ± 8.30 | 0.2 ± 2.9 | 1.0 ± 3.8 | ||
TTT: toe touch test, WBLT: weight-bearing lunge test, SLR: straight leg raise test, SEBT: star excursion balance test in three directions: anterior (ANT), posterolateral (PL) and posteromedial (PM), SJ: squat jump, CMJ: counter movement jump, STIF: stiffness jumps. *: Significantly different from PRE, #: Significantly different from CON.
Discussion
To our knowledge, this study was the first to evaluate the immediate effect of posterior muscle chain SMR on flexibility, balance and jump performance on the same experimental population. The main finding was the enhanced balance ability and flexibility without a decrease in jump performances following posterior muscle chain SMR intervention.
The benefits of SMR to flexibility found in the present study were in accordance with previous studies which demonstrated a positive effect of SMR on the range of motion (Halperin et al., 2014; MacDonald et al., 2013; Sullivan et al., 2013). Changes in myofascial tissue mechanical properties could partly contribute to the positive effect of SMR on flexibility since the colloidal substance was shown to be sensitive to mechanical stimulation and become more fluid after massage (Hotfiel et al., 2017). These modifications can reduce the adhesion between the different layers of the fascial tissues and increase connective tissues’ extensibility and compliance (Kalichman and Ben David, 2017; Schleip, 2003). For instance, it has been demonstrated that SMR performed with a foam roller enables the improvement of joint range of motion (Halperin et al., 2014; McKechnie et al., 2007; Schleip, 2003; Sullivan et al., 2013). In the same way, Drust et al. (2003) reported that SMR could also increase the temperature of the muscle and then reduce the viscosity of muscle tissue. Additionally, Hotfiel et al. (2017) demonstrated that SMR increased the blood flow and perfusion which may influence muscle temperature and thus enhance flexibility. Although these variables have not been considered in the present study, it can be hypothesized that SMR improved flexibility partially by increasing the muscle blood flow and temperature (Drust et al., 2003). Meanwhile the increase in the range of motion may be explained by mechanical pressure which can overload the mechanical receptor in myofascia with some potentially pain-relieving effects (Bialosky et al., 2009; Voogt et al., 2015). It may also decrease the stretching sensation (McKechnie et al., 2007) and thus increase stretching tolerance (Sayenko et al., 2009; Weppler and Magnusson, 2010). Surprisingly, the present study demonstrated stronger positive effects of SMR on flexibility (11 ± 7% for SLR, 50 ± 40% for TTT and 22 ± 17% for the WBLT) compared to those reported in previous studies ranging from 4.3 to 18.7% (Halperin et al., 2014; Jay et al., 2014; MacDonald et al., 2013; Sullivan et al., 2013). This may be explained by the accumulated benefits of SMR to the different muscle groups in association with the Myers’s “Anatomy Train” theory. Myers (2013) proposed that massage on a muscle group of the superficial back line including some muscle zone of the posterior muscle chain could modify the tension along the entire line. This can be related to the change in the ankle dorsiflexion range of motion with the modification of the hip angle (Andrade et al., 2016). We speculate that the accumulated benefits and SMR duration could induce a greater improvement in the range of motion. Further studies to test this hypothesis are needed to compare single and repeated bout effects of SMR on the range of motion improvement.
Although many studies reported benefits to the joint range of motion following a single session of myofascial release, only few examined the dynamic balance ability. In the present study, a significant improvement in dynamic balance ability following postural muscle chain SMR was quantified. The present results are in line with a Sefton et al.’s study which showed that 60-min of manual therapy improved dynamic balance ability measured with the functional single leg balance test (Sefton et al., 2012). Such an improvement could be attributed to numerous factors like muscle contractions, proprioception or central nervous system activation (Weerapong et al., 2005). In addition, myofascia includes a multitude of sensory nerves related to proprioceptive and mechanical receptors like Golgi receptors or Pacini receptors (Tozzi, 2012). Therefore, the pressure exerted during the SMR intervention may stimulate these mechanical receptors and improve the proprioceptive information integrated by the central nervous system to tune the activation level of the motor units (Schleip, 2003). Moreover, it has been demonstrated that ankle dorsiflexion range of motion is significantly related to the dynamic balance ability (Basnett et al., 2013; Hoch et al., 2011). Thus, the significant improvement of the ankle dorsiflexion range of motion reported in the present study may partly explain the increased performance in the SEBT. In contrast, no previous study has reported deleterious effects of SMR on dynamic balance ability. Junker and Stöggl (2019) and Halperin et al. (2014) found no chronic/acute effect of SMR on Y balance test performances. Considering the variability in SMR interventions and the few studies of SMR effects on balance ability, further studies are needed to explore more deeply the positive effects of SMR on the balance ability found in the present study, using additional investigation methods including for instance surface electromyography.
In contrast, no significant effect of SMR on jump performances was found whatever the test (i.e., CMJ, SJ, STIF). This result is in accordance with previous research (Behara and Jacobson, 2017; Healey et al., 2014) and especially the results reported by Behara and Jacobson (2017) who observed no significant difference in power and velocity during the CMJ after a single SMR intervention. Conversely, Sagiroglu et al. (2017) observed a detrimental effect on the CMJ following a single session of SMR with a grid foam roller on hamstring, quadriceps, hip and gastrocnemius muscles after aerobic running (Sağiroğlu et al., 2017). Decreased CMJ performance was assumed to be related to the increased flexibility after SMR which might temporarily decrease the muscle ability to generate power output due to the increased stretch tolerance (Behm and Kibele, 2007; Marchetti et al., 2014; McKechnie et al., 2007; Sayenko et al., 2009). However, the present study showed increased ankle dorsiflexion after SMR without any change in jump performances, although increased ankle dorsiflexion may also improve jump performance (Papaiakovou, 2013). Nevertheless, the vertical jump is a multi-joint movement that requires complex motor coordination and the muscle activation pattern has to be continuously adapted to the joint flexibility to maintain or increase jump performance (Babault et al., 2003; Kirby et al., 2011). According to different results, it can be assumed that duration, muscle groups, pressure or material used for SMR may modulate the effects on muscle force and joint flexibility. Although no quantitative assessment of the pressure was made during SMR interventions in the present study, qualitative assessment was performed throughout the experimental protocol by the same experimenter (Q.S.Z.).
The present study aimed at determining the functional effects of SMR on flexibility, balance ability, and jump performance in the same experimental population. This study addressed the effectiveness of SMR on the superficial posterior muscle chain for an immediate gain in flexibility of the hip joint with an increased dynamic balance ability and no effect on vertical jump performance. Thus, SMR can be easily integrated into the warm-up of athletes, given that a roller and a massage ball are very simple, easy-to-use, and cheap tools. It remains to determine the effect of integrated SMR as a warm-up option on the occurrence, frequency, and extent of muscle injury in the athlete’s population. Based on the current study, further studies should be performed to assess the most effective pressure to be applied and the influence of SMR on mechanical and physiological variables (e.g., electromyographic muscle activity) to better explain the positive effects of SMR, especially on the dynamic balance ability. In addition, further studies are needed to evaluate the efficacy of such an SMR prevention protocol in the warm-up to reduce the occurrence of injuries in sport.
Acknowledgements
Authors would like to thank all the participants who performed voluntarily and their best effort during protocol. Gratefully acknowledge the support of Inter-University Laboratory of Human Movement Biology (LIBM/EA 7424). The present study was funded by the China Scholarship Council (CSC) (No. 201708070091).
References
- Andrade RJ, Lacourpaille L, Freitas SR, McNair PJ, Nordez A. Effects of hip and head position on ankle range of motion, ankle passive torque, and passive gastrocnemius tension. Scand J Med Sci Sports. 2016;26:41–47. doi: 10.1111/sms.12406. [DOI] [PubMed] [Google Scholar]
- Babault N, Pousson M, Michaut A, Van Hoecke J. Effect of quadriceps femoris muscle length on neural activation during isometric and concentric contractions. J Appl Physiol (1985) 2003;94:983–990. doi: 10.1152/japplphysiol.00717.2002. [DOI] [PubMed] [Google Scholar]
- Barnes MF. The basic science of myofascial release: morphologic change in connective tissue. Journal of Bodywork and Movement Therapies. 1997;1:231–238. [Google Scholar]
- Basnett CR, Hanish MJ, Wheeler TJ, Miriovsky DJ, Danielson EL, Barr JB, Grindstaff TL. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013;8:121–128. [PMC free article] [PubMed] [Google Scholar]
- Bates D, Machler M, Bolker BM, Walker SC. Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software. 2015;67:1–48. [Google Scholar]
- Behara B, Jacobson BH. Acute Effects of Deep Tissue Foam Rolling and Dynamic Stretching on Muscular Strength, Power, and Flexibility in Division I Linemen. J Strength Cond Res. 2017;31:888–892. doi: 10.1519/JSC.0000000000001051. [DOI] [PubMed] [Google Scholar]
- Behm DG, Kibele A. Effects of differing intensities of static stretching on jump performance. Eur J Appl Physiol. 2007;101:587–594. doi: 10.1007/s00421-007-0533-5. [DOI] [PubMed] [Google Scholar]
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531–538. doi: 10.1016/j.math.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury-Squires DJ, Noftall JC, Sullivan KM, Behm DG, Power KE, Button DC. Roller-massager application to the quadriceps and knee-joint range of motion and neuromuscular efficiency during a lunge. J Athl Train. 2015;50:133–140. doi: 10.4085/1062-6050-49.5.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drust B, Atkinson G, Gregson W, French D, Binningsley D. The effects of massage on intra muscular temperature in the vastus lateralis in humans. Int J Sports Med. 2003;24:395–399. doi: 10.1055/s-2003-41182. [DOI] [PubMed] [Google Scholar]
- Fouré A, Nordez A, McNair P, Cornu C. Effects of plyometric training on both active and passive parts of the plantarflexors series elastic component stiffness of muscle-tendon complex. Eur J Appl Physiol. 2011;111:539–548. doi: 10.1007/s00421-010-1667-4. [DOI] [PubMed] [Google Scholar]
- Halperin I, Aboodarda SJ, Button DC, Andersen LL, Behm DG. Roller massager improves range of motion of plantar flexor muscles without subsequent decreases in force parameters. Int J Sports Phys Ther. 2014;9:92–102. [PMC free article] [PubMed] [Google Scholar]
- Healey KC, Hatfield DL, Blanpied P, Dorfman LR, Riebe D. The effects of myofascial release with foam rolling on performance. J Strength Cond Res. 2014;28:61–68. doi: 10.1519/JSC.0b013e3182956569. [DOI] [PubMed] [Google Scholar]
- Hoch MC, Staton GS, McKeon PO. Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport. 2011;14:90–92. doi: 10.1016/j.jsams.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Hotfiel T, Swoboda B, Krinner S, Grim C, Engelhardt M, Uder M, Heiss RU. Acute Effects of Lateral Thigh Foam Rolling on Arterial Tissue Perfusion Determined by Spectral Doppler and Power Doppler Ultrasound. J Strength Cond Res. 2017;31:893–900. doi: 10.1519/JSC.0000000000001641. [DOI] [PubMed] [Google Scholar]
- Jay K, Sundstrup E, Sondergaard SD, Behm D, Brandt M, Saervoll CA, Jakobsen MD, Andersen LL. Specific and cross over effects of massage for muscle soreness: randomized controlled trial. Int J Sports Phys Ther. 2014;9:82–91. [PMC free article] [PubMed] [Google Scholar]
- Junker D, Stöggl T. The Training Effects of Foam Rolling on Core Strength Endurance, Balance, Muscle Performance and Range of Motion: A Randomized Controlled Trial. J Sports Sci Med. 2019;18:229238. [PMC free article] [PubMed] [Google Scholar]
- Kalichman L, Ben David C. Effect of self-myofascial release on myofascial pain, muscle flexibility, and strength: A narrative review. J Bodyw Mov Ther. 2017;21:446–451. doi: 10.1016/j.jbmt.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Kirby TJ, McBride JM, Haines TL, Dayne AM. Relative net vertical impulse determines jumping performance. J Appl Biomech. 2011;27:207–214. doi: 10.1123/jab.27.3.207. [DOI] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest Package: Tests in Linear Mixed Effects Models. Journal of Statistical Software. 2017;82 [Google Scholar]
- MacDonald GZ, Penney MD, Mullaley ME, Cuconato AL, Drake CD, Behm DG, Button DC. An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J Strength Cond Res. 2013;27:812–821. doi: 10.1519/JSC.0b013e31825c2bc1. [DOI] [PubMed] [Google Scholar]
- Marchetti PH, Silva FH, Soares EG, Serpa EP, Nardi PSM, Vilela GdB, Behm DG. Upper limb static-stretching protocol decreases maximal concentric jump performance. J Sports Sci Med. 2014;13:945950. [PMC free article] [PubMed] [Google Scholar]
- McKechnie GJ, Young WB, Behm DG. Acute effects of two massage techniques on ankle joint flexibility and power of the plantar flexors. J Sports Sci Med. 2007;6:498–504. [PMC free article] [PubMed] [Google Scholar]
- Mohr AR, Long BC, Goad CL. Effect of foam rolling and static stretching on passive hip-flexion range of motion. J Sport Rehabil. 2014;23:296–299. doi: 10.1123/jsr.2013-0025. [DOI] [PubMed] [Google Scholar]
- Morales-Artacho AJ, Lacourpaille L, Guilhem G. Effects of warm-up on hamstring muscles stiffness: Cycling vs foam rolling. Scand J Med Sci Sports. 2017;27:1959–1969. doi: 10.1111/sms.12832. [DOI] [PubMed] [Google Scholar]
- Mtibaa K, Thomson A, Nichols D, Hautier C, Racinais S. Hyperthermia-induced Neural Alterations Impair Proprioception and Balance. Med Sci Sports Exerc. 2018;50:46–53. doi: 10.1249/MSS.0000000000001418. [DOI] [PubMed] [Google Scholar]
- Nor Adnan NM, Ab Patar MNA, Lee H, Yamamoto S-I, Jong-Young L, Mahmud J. Biomechanical analysis using Kinovea for sports application. IOP Conference Series: Materials Science and Engineering. 2018;342:012097. [Google Scholar]
- Papaiakovou G. Kinematic and kinetic differences in the execution of vertical jumps between people with good and poor ankle joint dorsiflexion. J Sports Sci. 2013;31:1789–1796. doi: 10.1080/02640414.2013.803587. [DOI] [PubMed] [Google Scholar]
- Pearcey GE, Bradbury-Squires DJ, Kawamoto JE, Drinkwater EJ, Behm DG, Button DC. Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. J Athl Train. 2015;50:5–13. doi: 10.4085/1062-6050-50.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sağiroğlu İ, Kurt C, Pekünlü E, Özsu İ. Residual effects of static stretching and self-myofascial-release exercises on flexibility and lower body explosive strength in well-trained combat athletes. Isokinetics and Exercise Science. 2017;25:135–141. [Google Scholar]
- Sayenko DG, Vette AH, Obata H, Alekhina MI, Akai M, Nakazawa K. Differential effects of plantar cutaneous afferent excitation on soleus stretch and H-reflex. Muscle Nerve. 2009;39:761–769. doi: 10.1002/mus.21254. [DOI] [PubMed] [Google Scholar]
- Schleip R. Fascial plasticity – a new neurobiological explanation: Part 1. Journal of Bodywork and Movement Therapies. 2003;7:11–19. [Google Scholar]
- Sefton JM, Yarar C, Berry JW. Massage Therapy Produces Short-term Improvements in Balance, Neurological, and Cardiovascular Measures in Older Persons. Int J Ther Massage Bodywork. 2012;5:16–27. doi: 10.3822/ijtmb.v5i3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin MS, Sung YH. Effects of Massage on Muscular Strength and Proprioception After Exercise-Induced Muscle Damage. J Strength Cond Res. 2015;29:2255–2260. doi: 10.1519/JSC.0000000000000688. [DOI] [PubMed] [Google Scholar]
- Su H, Chang NJ, Wu WL, Guo LY, Chu IH. Acute Effects of Foam Rolling, Static Stretching, and Dynamic Stretching During Warm-ups on Muscular Flexibility and Strength in Young Adults. J Sport Rehabil. 2017;26:469–477. doi: 10.1123/jsr.2016-0102. [DOI] [PubMed] [Google Scholar]
- Sullivan KM, Silvey DB, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013;8:228–236. [PMC free article] [PubMed] [Google Scholar]
- Tozzi P. Selected fascial aspects of osteopathic practice. J Bodyw Mov Ther. 2012;16:503–519. doi: 10.1016/j.jbmt.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Voogt L, de Vries J, Meeus M, Struyf F, Meuffels D, Nijs J. Analgesic effects of manual therapy in patients with musculoskeletal pain: a systematic review. Man Ther. 2015;20:250–256. doi: 10.1016/j.math.2014.09.001. [DOI] [PubMed] [Google Scholar]
- Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235–256. doi: 10.2165/00007256-200535030-00004. [DOI] [PubMed] [Google Scholar]
- Weppler CH, Magnusson SP. Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther. 2010;90:438–449. doi: 10.2522/ptj.20090012. [DOI] [PubMed] [Google Scholar]


