Abstract
The coronavirus disease 2019 (COVID-19) is a global health emergency of unprecedented proportions. Countries around the world have taken extraordinary steps to control the disease. The preventive measures face challenges in low and lower middle income countries (LICs and LMICs). Especially the marginalized communities, e.g., women are the hardest hit of the virus. This study took Bangladesh as a representative LMIC and aimed to determine the level of knowledge, perception, attitude, and preparedness related to COVID-19 among the adult women in the country. Using a comprehensive questionnaire, we channeled a cross-sectional study among adult women in Bangladesh. Participant's self-reported data on the knowledge, attitude, and preparedness were tabulated and analyzed using suitable statistical tools. A total of 1,869 adults from 61 districts of Bangladesh took part in this study. Ninety seven percentage of the participants claimed to have heard of COVID-19 before it arrived in Bangladesh. Regarding the general knowledge related to COVID-19's causal agent, symptoms, and treatment, the positive response rate was nearly 80%, with a mean of 10.68 ± 1.72. Younger and educated women had better knowledge levels compared to the older and lower-educated participants (p < 0.01). More efforts are required to educate women with older age and lower socioeconomic status. An overall positive attitude and perception were observed, although a significant proportion of the participants opined that the Government's efforts in controlling the outbreak were not adequate. Although the participants had a satisfactory level of knowledge and a positive attitude in adopting preventive measures against COVID-19, greater efforts are needed from the healthcare authorities and Government.
Keywords: COVID-19, SARS-CoV-2, women, health literacy, knowledge, awareness, preparedness, attitude
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new member of the coronaviridae family of RNA viruses (1). Infection with SARS-COV-2, leading to coronavirus disease 2019 (COVID-19) in humans, can result in respiratory syndromes ranging from an uncomplicated upper respiratory tract distress to severe viral pneumonia with multiorgan failure and death (2). This new virus transmits by droplets from asymptomatic or oligosymptomatic patients and proximally through aerosols in health care environments (3, 4). Within months after the first infection detected in humans late in 2019, this highly contagious virus with the ability to cause severe respiratory disease has hit the health systems across the world (5). In around 6 months after the first emergence of the virus, nearly 4.5 million confirmed cases have been identified in 185 countries around the globe, and over 300 thousand people have died of the disease (6).
The disease has evolved into a pandemic, and the World Health Organization (WHO) has declared it a global health emergency of unprecedented proportions (7). The outbreak substantially impacted millions of people around the world. As there is yet a vaccine or treatment strategy to be approved for COVID-19, only strong infection control measures can help minimize the spread of the virus in the community and health care facilities. Countries worldwide adopted extraordinary control measures soon after the virus's emergence, and a multi-level stress-coping-adjustment procedure is in progress (8). In order to execute the control measures effectively, every individual across the world requires to pay attention to the dramatically changing messages about public health and take prompt actions to limit the virus spread and individual risk (7, 8). Lessons learned from previous outbreaks indicate that poor knowledge, attitudes, and perception (KAP) toward infectious diseases and health literacy may challenge the efforts to prevent the spread of disease (9). Besides, under-estimating potential risk, stigmatization, panic emotions, and wrong measures to avoid the infection may affect combating such a situation (10).
However, the prevailing rhetoric related to the pandemic is often not intelligible and evenly disseminated to the mass people (11). Consequently, the messaging regarding the strategic measures and imminent threat of COVID-19 pandemic is at odds, leading to miscommunication, public confusion, and inaction (12). The situation is far more complicated in low and lower-middle-income countries (LICs and LMICs), like in Bangladesh, where significant portions of the population have minimal health literacy (13, 14). Among the people in these underprivileged communities, women are even more disadvantaged due to cultural norms and values. A large proportion of women in these countries have negligible access to information (15). As a result, women in LICs and LMICs supposedly have lower knowledge-index. In the situation of a health emergency, when knowing and understanding the critical and rapidly changing health messages come with foremost importance, people living in marginalized communities, like the women in LICs and LMICs with limited access to information, may experience extremely inadequate health communication (16, 17). The limitations of health communication can potentially lead these people to be further marginalized and exposed to elevated risks (17, 18).
We did a time-sensitive study among the adult women representing different social groups of Bangladesh, an LMIC in Southeast Asia. Non-therapeutic preventive measures to limit the spread of SARS-CoV-2, e.g., social distancing, faced an enormous challenge during the early stage of the outbreak in Bangladesh. With a huge lack of diagnostic and hospital facilities and poor coordination of management strategies, the country was walloped by the emergence of the virus (19). Assumably, health literacy, and awareness among the mass people, especially among the marginalized population like the women, would be vital to control the virus spread and mitigate the pandemic's impact. This study aimed to assess knowledge, attitudes, and perceptions about COVID-19 among the female population in a resource-limited LMIC.
Methods
Study Design and Population
This cross-sectional survey took place during the initial weeks of lockdown enforced in Bangladesh. Only adult women of Bangladeshi nationality, who are not working in the medical field, were recruited in the study using convenience and snowball sampling methods. Given the current situation, a thorough community-based survey was not feasible. We collected the data through telephone, online, or in-person interviews, when possible. A team comprised of graduate students who majored in health and life sciences, clinicians, and statisticians conducted the questionnaire-based interviews.
Measurements
The newly prepared questionnaire consisted of five parts concerning the demographic backgrounds of the participants, and their knowledge, attitude, and preparedness (KAP) related to COVID-19. Following the guidelines for clinical and community management of COVID-19 by authorized bodies, we developed this questionnaire to assess the self-reported KAP of the participants (7, 20–22). The questionnaire included 15, 25, and 17 items related to the knowledge, attitude/perception, and preparedness of the women related to COVID-19. Each positive response (correct answer, where applicable) in the knowledge section was given 1 point, whereas a negative response received a 0 point.
Validation of the Questionnaire
We evaluated the newly prepared questionnaire in a preliminary study. Initially, we asked a group of Bangladeshi researchers in the field of epidemiology to independently assess the degree to which the questionnaire is relevant and is able to measure women's KAP regarding COVID-19 correctly. In terms of language, formatting, and contents, we made essential modifications to the questionnaire to address their comments. Later on, to pre-test the questionnaire, we interviewed 35 participants twice 15 days apart using the modified questionnaire. Obtained data were used to assess internal consistency and test-retest reliabilities using Cronbach's α and intra-class correlation analysis. Both assessments indicated satisfactory levels of reliability of the questionnaire (Cronbach's α = 0.79, intra-class correlation coefficient = 0.96). No data from the above mentioned 35 participants were included in the final analyses.
Statistical Analysis
We evaluated all data using the Statistical Package for the Social Sciences (IBM SPSS, v 22.0; Chicago, IL) software (23). Associations between participant characteristics and survey responses were then examined in bivariate analyses using Student's t-tests, z-statistic, χ2 tests, or analysis of variance (ANOVA), as suitable. For the continuous outcome of a perceived concern, we used multivariable linear regression models to estimate least-squares means (with 95% confidence intervals). The quantitative variables were reported either as mean ± standard deviation or frequency (%). All computations included the KAP variables as primary covariates of interest. Other variables affecting the KAP were also analyzed using appropriate statistical tools. All analyses were performed at α-levels of 0.05 and 0.01 (p = 0.05 and p = 0.01, respectively).
Ethics Statement
The internal Ethical Review Board (ERB) at the Department of Biochemistry and Molecular Biology, Shahjalal University of Science and Technology approved the study protocol (Reference ID: 02/BMB/2020). All participants in this study provided informed consent as per the World Medical Association (Helsingin julistus). No participants received any monetary rewards for participating in the study.
Results
Participants' Characteristics
In total, our interviewers invited 3,150 adult women to participate in this study, of which 1,246 declined to participate (Supplementary Table 1). A total of 1,904 women took part in the interviews; however, we excluded questionnaires of 35 participants due to incompleteness. Henceforth, the final analysis of this study consisted of data obtained from 1869 women, giving an overall response rate of 59.33%.
The mean age of the participants was 29.545 ± 12.009 years (range: 18–86 years), with over 40% (43.23%) of them aged 18 to 30 years and only 5.67% aged 60 years and above (Table 1, Supplementary Figure 1). The sample pool consisted of diverse socioeconomic backgrounds, originating from 61 of 64 districts of Bangladesh (Table 1, Supplementary Figures 1, 2). Over 50% (51.20%) of the participants had higher secondary or more education, with 17.39% of them being university or college graduates. Nearly one-third of the participants (32.69%) were students, another one-third (37.72%) were either unemployed, retired, or housewives (not involved in earning). Besides, ~60% (61.10%) of participants were either single or ever married at the time of the study. In terms of religious background, over 86% (86.35%) of participants were Muslims (Table 1). Over 10% (12.09%) of all participants had multiple clinical conditions (>1 clinical conditions), including coronary complications, respiratory, and pulmonological complications (Supplementary Table 2). Nearly 10% (9.84%) of the participants reported that they frequently experienced feverish symptoms.
Table 1.
Sociodemographic characteristics of participants.
| Variables | Value (n = 1,869) |
|---|---|
| Age (years) | 29.545 ± 12.009 |
| Marital status (n, %) | |
| Single | 801, 42.86 |
| Married | 727, 38.90 |
| Ever married | 341, 18.24 |
| Education level (n, %) | |
| No schooling | 88, 4.71 |
| Primary | 240, 18.84 |
| Secondary | 508, 27.18 |
| Higher secondary | 632, 33.81 |
| University/college | 325, 17.39 |
| Other | 76, 4.07 |
| Occupation (n, %) | |
| Unemployed/retired | 294, 15.73 |
| Student | 611, 32.69 |
| Self-employed | 43, 2.30 |
| Business | 102, 5.45 |
| Maidservants/household helping hands | 146, 7.81 |
| Service holder in a Government organization | 105, 5.61 |
| Service holder in a non-government/private organization | 157, 8.40 |
| Housewives (not involved in earning) | 411, 21.99 |
| Religion (n, %) | |
| Islam | 1,614, 86.35 |
| Hindu | 214, 11.44 |
| Buddhist | 27, 1.44 |
| Christian | 05, 0.27 |
| Prefer not to say | 09, 0.48 |
| Ethnicity (n, %) | |
| Bengali | 1,848, 98.88 |
| First nations/tribal | 21, 1.12 |
Knowledge Related to COVID-19
97% (n = 1,813) of all participants reported having heard of the COVID-19 outbreak. Out of the 1,813 participants who had heard of the outbreak, 1,759 (97.02%) knew that the virus had arrived in Bangladesh (Table 2). The source of knowledge for most the participant was internet (n = 1,173, 64.7%) and the TV (n = 919, 50.69%) (Supplementary Table 3). Over two-thirds (67.84%) of the participants claimed that they knew about COVID-19 after its emergence in China and before it arrived in Bangladesh (Supplementary Figure 3). Overall, the positive response rate was nearly 80% (Table 2). The total knowledge score ranged from 4 to 14, with a mean of 10.68 ± 1.72.
Table 2.
Women's knowledge related to COVID-19.
| Response | |||
|---|---|---|---|
| Yes (n, %) | No (n, %) | Maybe (n, %) | |
| Knows about contagious diseases | 1,616, 86.46 | 178, 9.52 | 75, 4.01 |
| Knows about viral flus | 1,573, 84.16 | 231, 12.36 | 65, 3.48 |
| Has idea about the general flu protocol of WHO | 1,248, 66.77 | 450, 24.08 | 171, 9.15 |
| Knows what causes (causal agent) COVID-19 | 1,529, 81.81 | 256, 13.7 | 84, 4.49 |
| Knows that COVID-19 is a contagious disease | 1,424, 76.19 | 331, 17.71 | 114, 6.1 |
| Knows about the mode of transmission of COVID-19 | 1,506, 80.58 | 265, 14.18 | 98, 5.24 |
| Knows about the symptoms of COVID-19 | 1,440, 77.05 | 315, 16.85 | 114, 6.1 |
| Knows about the unavailability of COVID-19 treatments | 1,501, 80.31 | 267, 14.29 | 101, 5.4 |
| Knows who are the vulnerable group to COVID-19 | 1,488, 79.61 | 276, 14.77 | 105, 5.62 |
| Knows what quarantine means | 1,392, 74.48 | 359, 19.21 | 118, 6.31 |
| Knows what social distancing means | 1,424, 76.2 | 332, 17.76 | 113, 6.04 |
| Overall response rate (mean ± SD) | 78.51 ± 5.06 | 15.86 ± 3.7 | 5.63 ± 1.42 |
Table 2, Supplementary Figure 4 presents the outcomes of knowledge assessment of the women regarding COVID-19's mode of transmission, common symptoms, vulnerable groups, and rhetoric related to the pandemic.
Perceptions and Attitudes Related to COVID-19
Nearly 4 out of 5 (83.28%) women acknowledged that they fear COVID-19 (Table 3). Over 50% (52.56%) of the participants were concerned because they have older family members. Around 3 out of 4 participants perceived COVID-19 as a dangerous public health threat (75.46%). However, they thought it to be common cases of flu (72.59%) (Table 3). One-fourth of the women (25.32%) assumed that COVID-19 is a curse from the GOD. Only ~40% of women thought that people around them are aware of the COVID-19 situation. The majority of the participants responded that Bangladesh's efforts and preparations in COVID-19 management was not enough and satisfying (Table 3). 46.8% thought that the media coverage about this disease is exaggerated. Two out of five women (39.33%) thought that the Bangladesh Government's timely measures could help reduce the spread of the virus, while only one-third (34.80%) thought that the doctors and nurses in Bangladesh are trained to handle COVID-19 patients. Over 85% (87.42%) opined that the Government should subsidize for treatment of COVID-19 patients. More than a half (53.94%) thought that the Government was not transparent on COVID-19 related information. Nearly half (46.39%) of the women feared that COVID-19 would result in a devastating fatality in the country (Table 3).
Table 3.
Perceptions of the women about COVID-19.
| Perceptions and attitudes about COVID-19 | Response (n = 1,813) | ||
|---|---|---|---|
| Yes (n, %) | No (n, %) | Maybe (n, %) | |
| I fear COVID-19 | 1,510, 83.29 | 179, 9.87 | 124, 6.84 |
| I am scared because my family have older (>60 yrs) adults (including me) | 953, 52.56 | 261, 14.4 | 599, 33.0 |
| COVID-19 is like the common-flus | 1,316, 72.58 | 348, 19.19 | 149, 8.22 |
| COVID-19 is a dangerous public health threat | 1,368, 75.46 | 249, 13.73 | 196, 10.81 |
| I am satisfied with Bangladesh's efforts to tackle the pandemic | 849, 46.83 | 760, 41.92 | 204, 11.25 |
| COVID-19 arrived in Bangladesh by people coming from abroad | 1,227, 67.68 | 311, 17.15 | 275, 15.17 |
| COVID-19 is a religious curse | 459, 25.32 | 1090, 60.12 | 264, 14.56 |
| Aggressive screening would help the management of COVID-19 | 1,556, 85.82 | 158, 8.71 | 99, 5.46 |
| Bangladesh have enough facilities for screening COVID-19 | 683, 37.67 | 743, 40.98 | 387, 21.35 |
| People around you are aware of the current situation | 726, 40.04 | 928, 51.19 | 159, 8.77 |
| Bangladesh have enough ventilation facilities to help critical patients | 629, 34.69 | 853, 47.05 | 331, 18.26 |
| Timely measures by the Government could help reduce the spread of COVID-19 in Bangladesh | 771, 42.53 | 713, 39.33 | 329, 18.15 |
| The government should subsidize for treatment of COVID-19 | 1,585, 87.42 | 129, 7.16 | 99, 5.46 |
| Bangladeshi doctors and nurses are trained to treat COVID-19 patients | 631, 34.80 | 826, 45.56 | 356, 19.64 |
| The mosques and religious congregations should remain discontinued | 845, 46.61 | 742, 40.93 | 226, 12.47 |
| Bangladesh is economically able to tackle COVID-19 challenge | 507, 27.96 | 1193, 65.80 | 113, 6.23 |
| COVID-19 pandemic may cause a food crisis in the country | 852, 46.99 | 813, 44.84 | 148, 8.16 |
| Hand sanitizers, hand soaps, and masks should be available freely | 1,127, 62.16 | 556, 30.67 | 130, 7.17 |
| Bangladeshi doctors have enough personal protective equipment | 919, 50.69 | 771, 42.53 | 123, 6.78 |
| The pandemic will severely hamper the education system | 1,316, 72.59 | 354, 19.58 | 142, 7.83 |
| COVID-19 will cause devastating fatality in Bangladesh | 841, 46.39 | 631, 34.80 | 341, 18.81 |
| Media coverage about this disease is exaggerated | 848, 46.77 | 649, 35.8 | 316, 17.43 |
| The government is transparent on COVID-19 information in Bangladesh | 609, 33.59 | 978, 53.94 | 226, 12.47 |
| Bangladesh is dependent on foreign grants for controlling COVID-19 | 763, 42.08 | 825, 45.5 | 225, 12.41 |
| Bangladesh will collapse due to COVID-19 pandemic | 786, 43.35 | 753, 41.53 | 274, 15.11 |
Preparedness Related to COVID-19
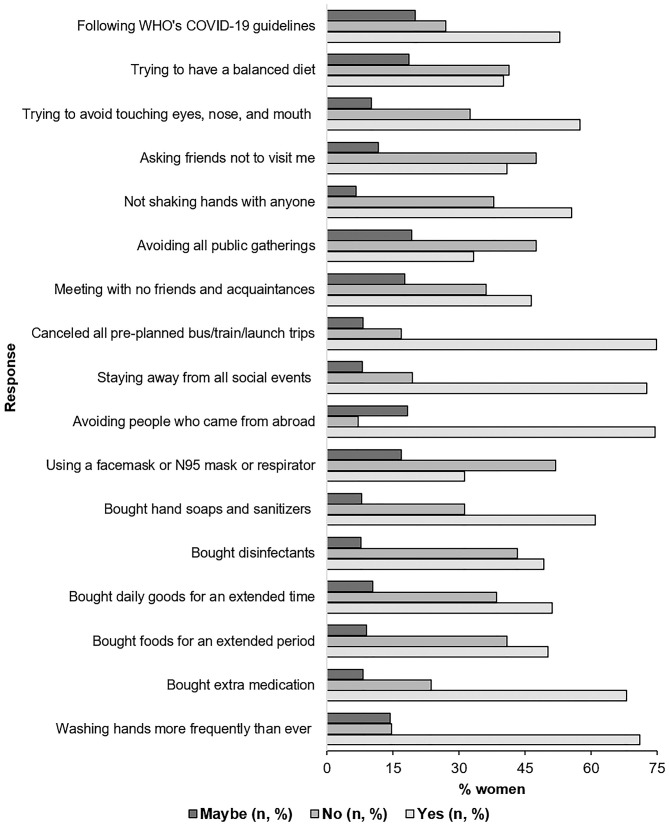
Figure 1 presents the preparedness of the women to limit the spread of COVID-19 and their responses. Seventy one percentage of participants reported that they are washing their hands more frequently than ever and for an extended period (Figure 1). They also reported that they managed to buy extra foods (50.27%), medicines (68.16%), daily goods (51.16%) for an extended period, and also bought disinfectants and hand soaps/sanitizers as precautions (48.66% and 61%, respectively) (Figure 1). Two out of five of every woman who participated claimed that they were avoiding to meet with their friends even if they have no symptoms (46.51%), to attend any public gatherings (e.g., political or religious gatherings) (38.82%) and places where many people used to gather (42.21%). Over 70% (74.59%) of the participants also claimed to abstain from meeting with anyone who has recently come from abroad. Nearly 60% (58.49%) of the women reported that they were trying to follow the guidelines of WHO regarding COVID-19. Around 40% of the participants (40.07%) women were using either a facemask or a KN95 mask/respirator (Figure 1).
Figure 1.
Womens preparedness related to COVID-19.
Sociodemographic Characteristics and COVID-19 Related Knowledge
We observed a significantly different mean knowledge scores between different age groups (p < 0.01) (Table 4). Compared to the younger age groups, participants aged 51–60 years and >60 years had a significantly lower mean knowledge score (9.70 ± 1.6 and 9.95 ± 1.99, respectively). Also, women from urban areas had a significantly higher mean knowledge score (10.87 ± 1.65) compared to residents from rural areas (10.01 ± 1.79) (p < 0.01). The knowledge mean scores did not correlate significantly to the education-levels of the women (p = 0.001). Also, women who did not participate in active earning (unemployed/retired and housewives) had a significantly lower knowledge level (p = 0.0018).
Table 4.
Factors affecting the knowledge score of women.
| Predictor | Knowledge score (mean, SD) | p-value |
|---|---|---|
| Age (years) | ||
| 18–30 | 10.89 ± 1.75 | < 0.001 |
| 31–40 | 10.8 ± 1.64 | |
| 41–50 | 10.82 ± 1.76 | |
| 51–60 | 9.7 ± 1.6 | |
| >60 | 9.95 ± 1.99 | |
| Education | ||
| High school or below | 10.61 ± 1.71 | 0.001 |
| College/university or above | 10.93 ± 1.74 | |
| Marital status | ||
| Single | 10.77 ± 1.7 | |
| Married | 10.62 ± 1.78 | |
| Ever married | 10.59 ± 1.63 | |
| Area of residence | ||
| Urban | 10.87 ± 1.65 | <0.001 |
| Rural | 10.01 ± 1.79 | |
| Slum | 9.68 ± 1.7 | |
| Occupation | ||
| Student | 11.01 ± 1.8 | 0.1249 |
| Involved in active earning | 10.86 ± 1.5 | |
| Unemployed/retired and housewives | 10.56 ± 1.82 | 0.0018 |
SD, standard deviation.
Discussion
With one of the world's densest populations, Bangladesh is an LMIC in Southeast Asia. Like most other LICs and LMICs, it has limited health facilities, and its citizens' health literacy level is not satisfactory (24, 25). As a result, it supposedly faces a significant challenge in implementing any health measures. Besides, many senior citizens and mid-aged people in the country have non-communicable disorders, including chronic obstructive pulmonary disease (11.9%), cardiac disorders (4.5%), diabetes (9.7%), and asthma (5.2%) (26–29). These people with multiple comorbidities are also especially vulnerable to emerging infectious diseases, e.g., the COVID-19.
As the COVID-19 outbreak quickly surges around the globe, every country is taking extraordinary measures to control its spread. Since there is yet a vaccination or effective treatment strategy against the disease, the control measures basically include non-therapeutic preventive strategies. Effective implementation of these measures requires wholehearted efforts by the government bodies, together with personal understanding and practices, and it depends on the KAP of the general public about the disease. Usually, in the LICs and LMICs, general people, especially the marginalized communities like the females, are less aware of health-related issues. The health-related marginalization of women is due to the availability of few recourses to access health service and literacy. As a result, they show poor perception and attitude toward health issues. While combating a global health crisis like the COVID-19 pandemic, the poor KAP of women may hamper the implementation of control and mitigation strategies. They remain at the core of the fight against the COVID-19 pandemic (30). It is also reported that women, especially the women workers, are among the hardest-hit groups by COVID-19 in Bangladesh (31). Here we present the results of a survey about the KAP of the Bangladeshi women toward the COVID-19 disease. It represents the first study to evaluate the KAP-level among women in LICs and LMICs, including Bangladesh.
The educated women, having an equivalent or higher education than higher-secondary level (51.2%), dominated the study population (Table 1). Also, a significant proportion of the women were students, preferably of college or university levels (Table 1). From the perspective of religious background, ethnicity, the structure of the studied population was comparable with the general female population of Bangladesh (Table 1) (32). Interestingly, the prevalence of comorbid conditions was relatively high compared to the country's overall frequency (26–29). Nearly 40% of the women (40.67%), among who were invited to participate, declined to participate (Supplementary Table 1). The reason for declining to participate included no time for participating (60.67%), lack of interest (29.13%), and fear of forgery (11.56%). The final sample included data from 1,869 women, representing an ideal survey sample size (at a 99% confidence interval, the limit of precision of 1%) (Supplementary Table 1). Overall, though educated women dominated the sample population, it was diverse and corresponded to the general trends of Bangladesh's population. However, as we distributed the survey using convenience and snowball methods, it may have influenced the general characteristics of the sample population. Given the overall situation due to COVID-19, we were unable to conduct a more rigorous survey, and this represents a major limitation of this study.
In general, women who participated in our study had good general knowledge about the disease, its mode of transmission, and prevention (Table 2). The primary sources of knowledge on COVID-19 among women included the internet (64.7%) and TV (50.69%) (Supplementary Table 2). A possible reason for the internet being the most favored source of knowledge could be the inclusion of more young women, e.g., students who used to surf the internet more than the mid-aged and older women. These channels of knowledge, e.g., the internet and TV, provide an uncomplicated and accessible way to receive information related to COVID-19; these can also provide misinformation, fabricated data, and rumors (33, 34). Henceforth, caution about the use of these channels must be in place (34–36). The overall response rate was nearing 80% (78.51 ± 5.06)%, and the average knowledge score was 10.68/16 (±1.72), denoting a satisfactory level of knowledge on COVID-19's causal agent, mode of transmission, symptoms, vulnerability group, relevant rhetorics, and treatment. Women's COVID-19 related knowledge level observed in this study exceeded the knowledge levels of both general (includes both men and women) and female sub-groups reported in two other recent studies held in Bangladesh (37, 38). Given that both of these studies report the outcomes based on sample populations dominated by young and educated individuals, it indicates that women in Bangladesh are more knowledgeable about COVID-19 than men.
We observed a comparatively lower COVID-19 related knowledge level among older women (Supplementary Figure 1). These results are similar to the outcomes reported for the general population of Bangladesh, Egypt, and China, where participants with high socioeconomic status were more knowledgeable than participants coming with lower status (10, 35, 37, 38). It indicates that extensive efforts are required to deliver messages to the older group of women, who may have difficulties accessing the most favorable sources of COVID-19 related knowledge.
When analyzing women's perception and attitude toward COVID-19, we found that over four of five women were scared of the infection, and the primary reason (52.56%) for their fear was due to the presence of older individuals in their family (Table 3). A similar response was reported from other studies held on general populations as well (10, 35). Unlike previous reports in other LMICs, around half of the participants assumed that the media was exaggerating the risk (Table 3) (35, 39).
The majority of the women opined that the Bangladeshi administration and health professionals had inadequate preparations to combat the outbreak. Many of the women were also concerned about the awareness of the people around them. It is apparent in the participants' opinion that Bangladeshi authorities failed to manage the COVID-19 outbreak better, which could lead to a devastating fatality in the country. Bangladesh's poor preparation for tackling the COVID-19 situation was also reported in a recent interagency memo of the United Nations, led by the WHO (40). Although most of the participants were concerned about a possible economic crisis, they opined that the Government should subsidize the treatment of COVID-19. Concerns over the Government's transparency regarding COVID-19 related information, suppressing unrestricted dissents, the possibility of food unavailability in the future, and education of children (and themselves) were also in place. Many were scared that the country would collapse in tackling the pandemic. However, the authorities of Bangladesh have repeatedly claimed that their prompt measures kept the outbreak of COVID-19 well under control in the country, and the Government is fully transparent about its policies to mitigate the situation (41–44).
One-fourth of our participants assumed the COVID-19 as a religious curse. In response to the extraordinary situations due to COVID-19, many countries curbed the religious congregations, and some Muslim-dominant countries even temporarily amended the adhan (call for prayer) to urge followers to pray in their homes than to come to the mosques (45). Bangladesh also suspended regular and special prayers in the mosques and applied restrictions to all other religious groups (46). Interestingly, a mixed opinion was observed regarding public religious congregations among the women in Bangladesh (Table 3). A possible reason for this mixed opinion could be the strong influence of religious beliefs among the population of semi-conservative societal structure in Bangladesh- where people used to face dilemmas in amending religious practices even when there are logical grounds (47).
Participants in our study showed a sort of good personal preparedness in response to COVID-19 (Figure 1). They considered the value of frequent handwashing for an extended time, avoiding to touch eyes, nose, and mouth, and limited personal contact. However, the proportion of women was low compared to the general population (internet users), as described by previous studies held in Bangladesh, where ~95% of participants were practicing social distancing (37). In our study, ~75% of the participants avoided social gatherings, meeting with people coming from abroad, and canceled preplanned visits during the summer vacations. Nearly half of the women stocked more foods, daily goods, and regularly needed medicines for a longer time. Also, many of them bought hand soaps, sanitizers, and disinfectants. Around 40% of women were using a facemask or KN95 mask or a respirator. The percentage of participants practicing the use of masks was comparable with the reports from Egypt, but not with China, where almost all participants reported putting face masks when they go out (10, 35). It is apparent that the use of masks was substantially low among women in Bangladesh as compared to the internet users (men and women) in the country, >91% of whom used to put a mask when going outside the home (37). Regarding the use of masks, the Center for Disease Control and Prevention (CDC) emphasized putting face coverings in areas where the transmission is at the community level, while WHO recommends using it for those who have respiratory symptoms or are caring for another person with symptoms (48, 49). It is crucial to develop local guidelines for mask-use in Bangladesh by the health experts and Government bodies. Unnecessary use of masks needs to be prevented while confirming that the health risk is not hampered during this unprecedented time. Similar guidelines are also needed for the use of hand soaps, sanitizers, and disinfectants, as overuse of these chemical substances may harm the dermatological aspects of men.
Bangladesh's efforts in controlling the COVID-19 pandemic had numerous limitations (19). As the country had, like almost all other countries, no experience in facing a coronavirus outbreak, weakness in its preparation is relatable. Besides, as a small country with limited resources but a huge population, its efforts faced enormous challenges (19). The KAP of its citizens, including marginalized communities like women, was satisfactory at individual levels, which is essential to control the infection (9, 10, 50). However, the country's efforts seem to fail in controlling the spread (37, 38). As of early October, 6 months after the detection of the first COVID-19 case in Bangladesh, the number of active and new cases is increasing by leaps and bounds (51). A similar situation is observed in other LMICs in Bangladesh's neighborhood and beyond (39, 52–54). Although the Governments of the countries have taken significant measures to limit the spread of the disease, more effort is needed to support the most affected groups.
This study indicates that the healthcare authorities, media, and Governments in LICs and LMICs should be more careful and transparent in spreading knowledge to its people, especially to those who are marginalized, e.g., women and older individuals with low socioeconomic status, when fighting a pandemic like the COVID-19.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Review Board (ERB), Department of Biochemistry and Molecular Biology, School of Life Sciences, Shahjalal University of Science and Technology, Sylhet - 3114, Bangladesh (Reference ID: ERB/02/BMB/2020). The patients/participants provided their informed consent to participate in this study.
Author Contributions
MH conceived the study. MH, SA, YA, and NA designed the study. MU, YA, BS, RR, RI, and NA conducted the surveys. SA analyzed and interpreted the data. AN and NH helped the interpretation of the data. SA and MU wrote the draft manuscript. SA and NA carried out the revisions. All authors approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors take this opportunity to thank the members of the Community of Biotechnology (Bangladesh) and other volunteer interviewers (n = 83) for their invaluable cooperation during the surveys. The authors are grateful to the participants for having confidence and trust in the interviewers/researchers and sharing information.
Footnotes
Funding. SA was supported by the Maternal and Child Health (MatCH) program and the Alberta Innovates Graduate Student Scholarship (AIGSS). MH was supported by the Research Center of Shahjalal University of Science and Technology (SUST Research Center).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.571689/full#supplementary-material
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bai Y, Yao L, Wei T, Tian F, Jin D-Y, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. (2020) 323:1406. 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in wuhan, china, of novel coronavirus–infected pneumonia. N Engl J Med. (2020) 382:1199–207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Du Toit A. Outbreak of a novel coronavirus. Nat Rev Microbiol. (2020) 18:123. 10.1038/s41579-020-0332-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. (2020) 2:533–4. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organiztaion WHO Virtual Press Conference on COVID-19. Who.int; (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2 (accessed April 15, 2020). [Google Scholar]
- 8.Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, et al. COVID-19: towards controlling of a pandemic. Lancet. (2020) 395:1015–8. 10.1016/S0140-6736(20)30673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SH. The SARS epidemic in Hong Kong: what lessons have we learned? J R Soc Med. (2003) 96:374–8. 10.1258/jrsm.96.8.374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhong B-L, Luo W, Li H-M, Zhang Q-Q, Liu X-G, Li W-T, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. (2020) 16:1745–52. 10.7150/ijbs.45221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maci SM. Institutional popularization of medical knowledge: the case of pandemic influenza A (H1N1): Stefania Maci. In: Bongo G, Caliendo G, editors. The Language of Popularization- Die Sprache der Popularisierung. Bern: Peter Lang AG; (2014). p. 165–89. [Google Scholar]
- 12.Ioannidis JPA. Coronavirus disease 2019: the harms of exaggerated information and non-evidence-based measures. Eur J Clin Invest. (2020) 50:e13223. 10.1111/eci.13223 [DOI] [PubMed] [Google Scholar]
- 13.Singh K, Chaudhuri S. Confronting Disparities in the Time of COVID-19. Center for Policy Studies; (2020). Available online at: http://www.cps.iitb.ac.in/confronting-disparities-in-the-time-of-covid-19/ (accessed April 15, 2020). [Google Scholar]
- 14.Das S, Mia MN, Hanifi SMA, Hoque S, Bhuiya A. Health literacy in a community with low levels of education: findings from Chakaria, a rural area of Bangladesh. BMC Public Health. (2017) 17:203. 10.1186/s12889-017-4097-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acilar A. Exploring the aspects of digital divide in a developing country. Issues Inform Sci Inform Technol. (2011) 8:231–44. 10.28945/1415 [DOI] [Google Scholar]
- 16.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. (2005) 165:1946–52. 10.1001/archinte.165.17.1946 [DOI] [PubMed] [Google Scholar]
- 17.Mantwill S, Monestel-Umaña S, Schulz PJ. The relationship between health literacy and health disparities: a systematic review. PLoS ONE. (2015) 10:e0145455. 10.1371/journal.pone.0145455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolf MS, Serper M, Opsasnick L, O'Conor RM, Curtis LM, Benavente JY, et al. Awareness, attitudes, and actions related to covid-19 among adults with chronic conditions at the onset of the U.S. Outbreak. Ann Intern Med. (2020) 173:100–9. 10.7326/M20-1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anwar S, Nasrullah M, Hosen MJ. COVID-19 and Bangladesh: challenges and how to address them. Front Public Health. (2020) 8:154. 10.3389/fpubh.2020.00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.General Office of the National Health Commission of the People's Republic of China . Guideline for the Diagnosis and Treatment Of 2019 Novel Coronavirus (2019-Ncov) Infected Pneumonia (the Third Trial Version). nhc.gov.cn; (2020). Available online at: http://www.nhc.gov.cn/jkj/s3577/202001/dd1e502534004a8d88b6a10f329a3369.shtml (accessed April 15, 2020). [Google Scholar]
- 21.National Health Commission of the People's Republic of China A Protocol for Community Prevention and Control of the 2019 Novel Coronavirus (2019-nCoV) Infected Pneumonia (trial version). nhc.gov.cn. Available online at: http://www.nhc.gov.cn/jkj/s3577/202001/dd1e502534004a8d88b6a10f329a3369.shtml (accessed April 15, 2020). [Google Scholar]
- 22.Institute of Epidemiology Disease Control and Research COVID-19. iedcr.gov.bd; (2020). Available online at: https://www.iedcr.gov.bd/index.php/component/content/article/73-ncov-2019 (accessed April 11, 2020). [Google Scholar]
- 23.Cronk BC. How to Use SPSS : A Step-By-Step Guide to Analysis and Interpretation. New York, NY: Routledge; (2019). [Google Scholar]
- 24.Maina J Ouma PO Macharia PM Alegana VA Mitto B Fall IS . A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Sci Data. (2019) 6:134. 10.1038/s41597-019-0142-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leslie HH, Spiegelman D, Zhoub X, Kruka ME. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ. (2017) 95:738–48. 10.2471/BLT.17.191916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sutradhar I, Das Gupta R, Hasan M, Wazib A, Sarker M. Prevalence and risk factors of chronic obstructive pulmonary disease in bangladesh: a systematic review. Cureus. (2019) 11:e3970. 10.7759/cureus.3970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khanam F, Hossain MB, Mistry SK, Afsana K, Rahman M. Prevalence and risk factors of cardiovascular diseases among Bangladeshi adults: findings from a cross-sectional study. J Epidemiol Glob Health. (2019) 9:176–184. 10.2991/jegh.k.190531.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akter S, Rahman MM, Abe SK, Sultana P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ. (2014) 92:204–13A. 10.2471/BLT.13.128371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bishwajit G, Tang S, Yaya S, Feng Z. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chron Obstruct Pulmon Dis. (2017) 12:1093–9. 10.2147/COPD.S133148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramos G. Women at the Core of the Fight Against COVID-19 Crisis. (2020). Available online at: http://www.oecd.org/coronavirus/policy-responses/women-at-the-core-of-the-fight-against-covid-19-crisis-553a8269/#blocknotes-d7e2908 (accessed October 04, 2020).
- 31.UN Women. Far From the Spotlight, Women Workers are Among the Hardest Hit by COVID-19 in Bangladesh. unwomen.org; (2020). Available online at: https://www.unwomen.org/en/news/stories/2020/4/feature-women-workers-hardest-hit-by-covid-19-in-bangladesh (accessed May 28, 2020). [Google Scholar]
- 32.Bangladesh Bureau of Statistics Population and Housing Census 2011 - National volume 2: Union Statistics. Dhaka; (2015). Available online at: http://www.bbs.gov.bd/WebTestApplication/userfiles/Image/NationalReports/Union~Statistics.pdf [Google Scholar]
- 33.Tasnim S, Hossain MM, Mazumder H. Impact of rumors and misinformation on COVID-19 in social media. J Prev Med Public Health. (2020) 53:171–4. 10.3961/jpmph.20.094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. (2020) 27:taaa031. 10.1093/jtm/taaa031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdelhafiz AS, Mohammed Z, Ibrahim ME, Ziady HH, Alorabi M, Ayyad M, et al. Knowledge, perceptions, and attitude of egyptians towards the novel coronavirus disease (COVID-19). J Community Health. (2020) 45:881–90. 10.1007/s10900-020-00827-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Llewellyn S. Covid-19: how to be careful with trust and expertise on social media. BMJ. (2020) 368:m1160. 10.1136/bmj.m1160 [DOI] [PubMed] [Google Scholar]
- 37.Rahman A, Sathi NJ. knowledge-attitude-and-preventive-practices-toward-Covid-19-among-bangladeshi-internet-users. Electron J Gen Med. (2020) 17:em245 10.29333/ejgm/8223 [DOI] [Google Scholar]
- 38.Haque T, Hossain KM, Bhuiyan MMR, Ananna SA, Chowdhury SH, Islam MR, et al. Knowledge, attitude and practices (KAP) towards COVID-19 and assessment of risks of infection by SARS-CoV-2 among the Bangladeshi population: an online cross sectional survey. Preprint. (2020). 10.21203/rs.3.rs-24562/v1 [DOI] [Google Scholar]
- 39.Krishna PR, Undela K, Sathyanarayana BG, Palaksha S. Knowledge and beliefs of general public of india on covid-19: a web-based cross-sectional survey. medRxiv. Preprint. (2020). 10.1101/2020.04.22.20075267 [DOI] [Google Scholar]
- 40.Netra News. United Nations Interagency COVID-19 Memo: Without Interventions, “Upto 2 Million” People May Die in Bangladesh. Netra.news; (2020). Available online at: https://netra.news/2020/united-nations-interagency-covid-19-memo-without-interventions-upto-2-million-people-may-die-in-bangladesh-928 [Google Scholar]
- 41.TBS News. Early Readiness Kept COVID-19 Cases in Check. tbsnews.net; (2020). Available online at: https://tbsnews.net/coronavirus-chronicle/covid-19-bangladesh/early-preparation-kept-number-corona-patients-check-62587 [Google Scholar]
- 42.TBS News. Coronavirus Situation in Bangladesh Still Better Than Europe, America. tbsnews.net (2020) Available online at: https://tbsnews.net/coronavirus-chronicle/covid-19-bangladesh/coronavirus-situation-bangladesh-still-better-europe
- 43.Bangladesh Awami League Government's Initiative to Fight Coronavirus. albd.org; (2020). Available online at: https://www.albd.org/articles/news/33163/Government's-initiative-to-fight-Coronavirus (accessed June 2, 2020). [Google Scholar]
- 44.Wahiduzzaman A. Bangladesh is suppressing free speech during the COVID-19 pandemic. The Diplomat. (2020). Available online at: https://thediplomat.com/2020/04/bangladesh-is-suppressing-free-speech-during-the-covid-19-pandemic/
- 45.Middle east eye Coronavirus: Mosques in Kuwait Amend Call to Prayer to Include “pray in your Homes.” middleeasteye.net; (2020). Available online at: https://www.middleeasteye.net/news/coronavirus-mosques-kuwait-call-prayer-announces-pray-your-homes [Google Scholar]
- 46.Sakib SN. COVID-19: Bangladesh Halts Prayers at Mosques. AA.com; (2020) Available online at: https://www.aa.com.tr/en/asia-pacific/covid-19-bangladesh-halts-prayers-at-mosques/1794191 [Google Scholar]
- 47.Rashiduzzaman M. Bangladesh: MUSLIM Identity, Secularism, and the Politics of Nationalism. Religion and Politics in the Developing World: Explosive Interactions. New York, NY: Taylor and Francis group; (2018). p. 128–142. [Google Scholar]
- 48.Centers for Disease Control and Prevention Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission. cdc.gov; (2020). Available online at: Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission (accessed April 4, 2020). [Google Scholar]
- 49.World Health Organiztaion Coronavirus Disease (COVID-19) Advice for the Public: When and How to Use Masks. who.int; (2020). [Google Scholar]
- 50.Nour MO, Babilghith AO, Natto HA, Al-Amin FO, Alawneh SM. Knowledge, attitude and practices of healthcare providers towards MERS-CoV infection at Makkah hospitals, KSA. Int Res J Med Med Sci. (2015) 3:103–12. Available online at: http://www.netjournals.org/z_IRJMMS_15_046.html [Google Scholar]
- 51.Worldometer Covid-19 Coronavirus Pandemic. Worldometers.info; (2020). p. 1689–99. [Google Scholar]
- 52.Salman M, Mustafa ZU, Asif N, Zaidi HA, Hussain K, Shehzadi N, et al. Knowledge, attitude and preventive practices related to COVID-19: a cross-sectional study in two Pakistani university populations. Drugs Ther Perspect. (2020) 36: 319–25. 10.1007/s40267-020-00737-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saqlain M, Munir MM, Rehman S ur, Gulzar A, Naz S, Ahmed Z, et al. Knowledge, attitude, practice and perceived barriers among healthcare professionals regarding COVID-19: a cross-sectional survey from Pakistan. J Hosp Infect. (2020) 105 419–23. 10.1016/j.jhin.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kamate S, Sharma S, Thakar S, Srivastava D, Sengupta K, Hadi AJ, et al. Assessing knowledge, attitudes and practices of dental practitioners regarding the COVID-19 pandemic: a multinational study. Dent Med Probl. (2020) 57:11–7. 10.17219/dmp/119743 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.