Abstract
Aim
This study investigated the risk of osteoporosis or bone fractures (vertebrae, hip and others) in hysterectomized women in Taiwan.
Materials and methods
This is a retrospective population-based cohort study from 2000 to 2013. Women aged ≥30 years who underwent hysterectomy between 2000 and 2012 were included in this study. The comparison group was randomly selected from the database with a 1:4 matching with age and index year. Incidence rate and hazard ratios of osteoporosis and bone fracture between hysterectomized women and the comparison group were calculated. Cox proportional hazard regressions were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs).
Results
We identified 9,189 hysterectomized women and 33,942 age-matched women without a hysterectomy. All women were followed for a median time of about 7 years. The adjusted hazard ratio (aHR) of subsequent osteoporosis or bone fracture was higher in the hysterectomy women (2.26, 95% confidence interval [CI] = 2.09–2.44) than in the comparison group. In the subgroup analysis, oophorectomy and estrogen therapy increase the risk of osteoporosis or fracture in both groups. Regarding the fracture site, the aHR of vertebral fracture (4.92, 95% CI = 3.78–6.40) was higher in the hysterectomized women than in the comparison group. As follow-up time increasing, the aHR of vertebral fracture in hysterectomized women were 4.33 (95% CI = 2.99–6.28), 3.89 (95% CI = 2.60–5.82) and 5.42 (95% CI = 2.66–11.01) for <5, 5–9 and ≥9 years of follow-up, respectively.
Conclusions
In conclusion, we found that hysterectomized women might be associated with increased risks of developing osteoporosis or bone fracture.
Introduction
Osteoporosis and its associated fragility fractures are a significant global issue with an impact on humans second only to cardiovascular disease [1,2]. Osteoporosis is a skeletal system disease that reduces bony mass and disrupts the bone structure, causing decreased bone strength and leading to fragility fractures. Moreover, women were found to have double the risk for osteoporosis and triple the risk for fragility fractures compared with men at age 50 [3]. Furthermore, fractures are notorious for increased mortality, morbidity, disabilities in daily living, social costs, and psychogenic problems [4].
Hysterectomy, a surgery to remove the uterus, is the most common gynecologic operation worldwide, including in the United States and Taiwan [5–7]. Hysterectomy is thought to be related to multiple comorbidities because it might be related to earlier physiological menopause than in the general population, which results in earlier hormonal changes and may be related to osteoporosis and bone fractures [8].
Since osteoporosis and bone fracture have a strong relationship with menopause and hormone changes, we hypothesized that hysterectomy may increase the risk of osteoporosis and bone fracture. However, there are scarce studies discussing the association between hysterectomy and osteoporosis or fracture. The previous study showed hysterectomy was associated with bone loss, however, the study sample size was small [9]. Another study also with a small sample size showed hysterectomy associated with a decreased bone mineral density in the lumbar spine and hip [10]. There were two population-based studies regarding the relationship between hysterectomy and long-term osteoporotic fracture or bone mineral density [11,12]. However, there was no study discussing both outcomes together.
This retrospective study used the Taiwan National Health Insurance (TNHI) Database of one million randomly sampling cohort from a total of 23 million people in Taiwan to investigate the risk of developing osteoporosis and bone fracture for women with hysterectomy.
Materials and methods
Data source
This retrospective cohort study was conducted using claims data from the Longitudinal Health Insurance Database 2000 (LHID 2000), which is a subset of the National Health Insurance Research Database (NHIRD). The NHIRD was built by the National Health Research Institute; it contains 23 million NHI enrollees, which includes approximately 99% of the population of Taiwan. More than 20,000 medical care facilities, including hospitals, clinics, and pharmacies, which represent over 93% of all healthcare facilities in Taiwan, were contracted by the NHI project. The NHIRD includes outpatient and inpatient information about medication use, surgical procedures, intervention procedures, and clinical prescriptions. The NHRI claims that there are no statistically significant differences in the data on age, geographic region, and health care costs from the LHID 2000 and all claims data. Disease diagnoses were identified by the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). This database has been validated by many studies [13–15] and proved the correct coding and disease. This study was approved by the Institutional Review Board of China Medical University and the Hospital Research Ethics Committee (IRB permit number: CMUH-104-REC2-115) and is in compliance with institutional guidelines. The written informed consent was waived due to low risk and approved by the institutional IRB.
Sample participants
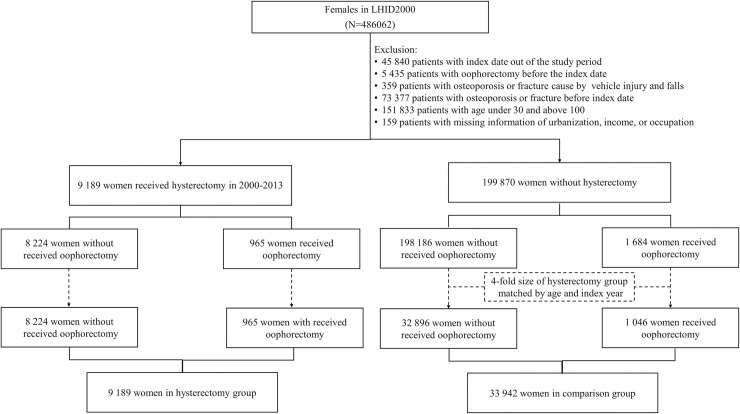
We retrospectively examined the hysterectomy and matched non-hysterectomy cohorts to investigate the relationship between hysterectomy and the risk of osteoporosis or bone fracture (ICD-9-CM code 800–829). The hysterectomy cohort included women aged ≥30 years who underwent hysterectomy (NHI claim codes 97020K, 97021A, 97022B, 97025K, 97026A, 97027B, 97027C, 97035K, 97036A, and 97037B) between January 1, 2000 and December 31, 2012. We defined the first date undergoing a hysterectomy in the study period as the index year. The comparison cohort was randomly selected from those beneficiaries without hysterectomy with matching by age (±5 years), and index year at a ratio of 1:4 with frequency matching. Women under 30 years old or above 100 years old and with a history of osteoporosis, bone fracture and oophorectomy before the index date were excluded from the present study. Patients with bone fracture that caused by vehicle injury and falls were also eliminated. Both cohorts were followed-up until the women developing osteoporosis, fracture, death, withdrew from the NHI program, or December 31, 2013, whichever occurred first. This study also considered confounding factors, such as the urbanization of residence, monthly income, occupation, and Charlson comorbidity index (CCI) [16]. We categorized into 4 levels of urbanization of where a subject lived (level 1, most urbanized; level 4, least urbanized). How the income and urbanization affect the medical resources used have been reported [17,18]. The study flow chart is illustrated in Fig 1.
Fig 1. Study flow chart: The participants population enrolled from the National Health Insurance Research Database.
Outcomes
The outcomes in this study were osteoporosis (NHI claim codes 733.0) or fracture (NHI claim codes 733.1, 800–804, 807–819, 822–829); vertebral fracture (NHI claim codes 805–806); hip fracture (NHI claim codes 820–821) diagnosed with 2 times of clinic visits and one time of hospitalization. In Taiwan, the diagnosis of osteoporosis was made by a Dual-energy X-ray absorptiometry (DEXA) exam. The other diagnostic modalities are history (age, menopause) and plain X-ray of vertebrae, hip or wrist.
Comorbidities
We also considered whether the women had an increased risk of osteoporosis or fracture due to undergoing unilateral (NHI claim codes 80802C, 80807C) or bilateral (NHI claim codes 80807B, 80811C, 80812C, 80602B, 80602C, and 80802B) oophorectomy. Associated comorbidities were also considered potential confounding factors to determine associations between women with or without hysterectomy. The CCI was used to determine the severity of comorbidities in this study. The CCI score is a widely used clinical index for a variety of disorders and cancers [19,20]. The higher the CCI, the more severe the comorbidities. We also included prescriptions for Estradiol and Premarin in the database (ATC codes G03C) during the study period. Women were considered as estrogen therapy (ET) users if they received in-hospital estrogen therapy for more than 30 days.
Statistical analysis
We used standard mean difference (SMD), which indicates there was a neglected difference when SMD <0.1, to examine the differences between categorical and continuous baseline characteristics, such as age, gender, urbanization of residence, monthly income, occupation, and CCI. Cox proportional hazard regressions were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). To evaluate the proportional hazard assumption of the Cox regression model, we added an interaction term between the study groups (hysterectomy/comparison group) and the logarithm of age in the Cox regression model. We also performed an analysis stratified by follow-up duration. The cumulative incidence of osteoporosis or bone fracture survival curves were plotted by the Kaplan–Meier estimator, and the log-rank test was used to evaluate the difference between the two groups. We used univariable and multivariable Poisson regression analysis to estimate the incidence rate ratio (IRR) and 95% CI of two groups. All statistical analyses were performed using SAS version 9.4 software (SAS Institute, Cary, NC, USA). The significance threshold was set at 0.05 for a two-tailed p-value.
Results
Subject characteristics
Fig 1 shows the flowchart used to select the hysterectomy and comparison groups from the NHIRD. After frequency matching, our study cohort consisted of 43,131 women. The hysterectomy cohort included 9,189 women and the comparison cohort included 33,711 women (Fig 1). The study subjects were predominantly insured persons from 40 to 49 years old (61%) who lived in a high degree of urbanization, had an insurance premium between 15,000 and 30,000, and had a white-collar occupation. A total of 965 and 1,046 women underwent oophorectomy in the hysterectomy cohort and comparison cohort, respectively. The hysterectomy cohort had a higher proportion of women with a CCI score of 2 than the comparison cohort (Table 1). The median follow-up time was 6.66 and 7.32 year in the hysterectomy group and the comparison group, respectively.
Table 1. Baseline characteristics in women with and without hysterectomy.
| Hysterectomy | Comparison group | ||
|---|---|---|---|
| (n = 9 189) | (n = 33 942) | SMD | |
| Age, years | |||
| 30–39 | 1285 (13.98) | 5063 (14.92) | 0.03 |
| 40–49 | 5692 (61.94) | 20795 (61.27) | 0.01 |
| 50–59 | 1481 (16.12) | 5348 (15.76) | 0.01 |
| ≧60 | 731 (7.96) | 2736 (8.06) | 0.004 |
| median (Q1-Q3) | 45.45 (42.22–49.78) | 44.24 (41.42–49.77) | 0.03 |
| Urbanization | |||
| 1 | 3066 (33.37) | 11972 (35.27) | 0.04 |
| 2 | 2797 (30.44) | 10158 (29.93) | 0.01 |
| 3 | 1518 (16.52) | 5532 (16.3) | 0.01 |
| 4 | 1808 (19.68) | 6280 (18.5) | 0.03 |
| Insurance premium | |||
| 0~15000 | 2067 (22.49) | 8293 (24.43) | 0.05 |
| 15000~30000 | 5434 (59.14) | 19181 (56.51) | 0.05 |
| ≧30000 | 1688 (18.37) | 6468 (19.06) | 0.02 |
| Occupation | |||
| White collar | 4853 (52.81) | 19442 (57.28) | 0.08 |
| Blue collar | 3715 (40.43) | 12146 (35.78) | 0.09 |
| Other | 621 (6.76) | 2354 (6.94) | 0.09 |
| Oophorectomy | 965 (10.50) | 1046 (3.08) | 0.30 |
| Charlson comorbidity index | |||
| 0 | 8323 (90.58) | 31913 (94.02) | 0.13 |
| 1 | 355 (3.86) | 1039 (3.06) | 0.04 |
| ≧2 | 511 (5.56) | 990 (2.92) | 0.13 |
| Estrogen treatment | |||
| Estradiol and premarin | 38 (0.41) | 59 (0.17) | 0.04 |
| Follow up times, year | |||
| median (Q1-Q3) | 6.66 (3.78–10.14) | 7.32 (4.26–10.67) | 0.12 |
SMD: Standard mean difference.
Risk of osteoporosis or fracture
In the hysterectomy group (n = 1049), the years (mean [SD]) from the index date through outcome was 4.97 [3.01] years, while in the comparison group (n = 1867), there were 5.09 [3.02] years.
Table 2 shows the incidence and HR of osteoporosis or fracture in women with hysterectomy compared to those without hysterectomy. Overall, the risk of osteoporosis or bone fracture in women with hysterectomy was significantly higher than that in the comparison group [incidence rate (IR) = 7.3 per 1,000 person-years vs 16.4 per 1,000 person-years; adjusted HR (aHR) = 2.26, 95% CI = 2.09–2.44].
Table 2. Incidence rate and hazard ratio of osteoporosis or bone fracture in women with hysterectomy and oophorectomy compared with the comparison group.
| Crude | Adjusted* | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Event | PY | IR | HR (95% CI) | p-value | HR (95% CI) | p-value | ||
| Osteoporosis or bone fracture | |||||||||
| Hysterectomy | Oophorectomy | ||||||||
| No | No | 32896 | 1776 | 243262 | 7.30 | 1.00 (reference) | 1.00 (reference) | ||
| No | unilateral | 477 | 36 | 3503 | 10.28 | 1.40 (1.01,1.95) | 0.04 | 1.63 (1.17,2.27) | 0.004 |
| No | bilateral | 569 | 55 | 5128 | 10.73 | 1.44 (1.10,1.89) | 0.01 | 2.04 (1.55,2.67) | <0.001 |
| Yes | No | 8224 | 954 | 57885 | 16.48 | 2.27 (2.10,2.45) | <0.001 | 2.26 (2.09,2.44) | <0.001 |
| Yes | unilateral | 531 | 22 | 2608 | 8.44 | 1.21 (0.80,1.85) | 0.37 | 1.30 (0.86,1.99) | 0.22 |
| Yes | bilateral | 434 | 73 | 3727 | 19.59 | 2.66 (2.10,3.36) | <0.001 | 2.95 (2.33,3.73) | <0.001 |
| Osteoporosis | |||||||||
| Hysterectomy | Oophorectomy | ||||||||
| No | No | 32242 | 1122 | 243262 | 4.61 | 1.00 (reference) | 1.00 (reference) | ||
| No | unilateral | 453 | 12 | 3503 | 3.43 | 0.77 (0.43,1.35) | 0.36 | 0.94 (0.53,1.65) | 0.82 |
| No | bilateral | 534 | 20 | 5128 | 3.90 | 0.85 (0.55,1.32) | 0.47 | 1.36 (0.87,2.12) | 0.17 |
| Yes | No | 7655 | 385 | 57885 | 6.65 | 1.50 (1.34,1.69) | <0.001 | 1.52 (1.36,1.71) | <0.001 |
| Yes | unilateral | 517 | 8 | 2608 | 3.07 | 0.70 (0.35,1.40) | 0.31 | 0.76 (0.38,1.52) | 0.44 |
| Yes | bilateral | 389 | 28 | 3727 | 7.51 | 1.72 (1.18,2.50) | 0.005 | 1.96 (1.34,2.85) | <0.001 |
| Hip fracture | |||||||||
| Hysterectomy | Oophorectomy | ||||||||
| No | No | 31198 | 78 | 243262 | 0.32 | 1.00 (reference) | 1.00 (reference) | ||
| No | unilateral | 442 | 1 | 3503 | 0.29 | 0.90 (0.13,6.47) | 0.92 | 1.08 (0.15,7.80) | 0.94 |
| No | bilateral | 517 | 3 | 5128 | 0.59 | 1.86 (0.59,5.91) | 0.29 | 3.27 (1.02,10.51) | 0.05 |
| Yes | No | 7288 | 18 | 57885 | 0.31 | 1.02 (0.61,1.70) | 0.95 | 1.07 (0.64,1.79) | 0.80 |
| Yes | unilateral | 509 | 2 | 2608 | 0.77 | -- | -- | ||
| Yes | bilateral | 363 | 2 | 3727 | 0.54 | 1.88 (0.46,7.64) | 0.38 | 2.75 (0.67,11.28) | 0.16 |
| Vertebral fracture | |||||||||
| Hysterectomy | Oophorectomy | ||||||||
| No | No | 31225 | 105 | 243262 | 0.43 | 1.00 (reference) | 1.00 (reference) | ||
| No | unilateral | 447 | 6 | 3503 | 1.71 | 4.03 (1.77,9.17) | <0.001 | 4.64 (2.03,10.6) | <0.001 |
| No | bilateral | 517 | 3 | 5128 | 0.59 | 1.33 (0.42,4.20) | 0.62 | 1.79 (0.56,5.68) | 0.32 |
| Yes | No | 7390 | 120 | 57885 | 2.07 | 5.02 (3.86,6.52) | <0.001 | 4.92 (3.78,6.40) | <0.001 |
| Yes | unilateral | 510 | 1 | 2608 | 0.38 | 0.98 (0.14,7.00) | 0.98 | 1.05 (0.15,7.56) | 0.96 |
| Yes | bilateral | 367 | 6 | 3727 | 1.61 | 3.87 (1.70,8.80) | 0.001 | 4.50 (1.97,10.29) | <0.001 |
| Other bone fracture | |||||||||
| Hysterectomy | Oophorectomy | ||||||||
| No | No | 31599 | 479 | 243262 | 1.97 | 1.00 (reference) | 1.00 (reference) | ||
| No | unilateral | 459 | 18 | 3503 | 5.14 | 2.59 (1.62,4.14) | <0.001 | 2.94 (1.83,4.71) | <0.001 |
| No | bilateral | 544 | 30 | 5128 | 5.85 | 2.92 (2.02,4.22) | <0.001 | 3.59 (2.47,5.21) | <0.001 |
| Yes | No | 7723 | 453 | 57885 | 7.83 | 4.04 (3.56,4.60) | <0.001 | 3.97 (3.49,4.51) | <0.001 |
| Yes | unilateral | 522 | 13 | 2608 | 4.98 | 2.60 (1.50,4.52) | <0.001 | 2.66 (1.53,4.61) | <0.001 |
| Yes | bilateral | 398 | 37 | 3727 | 9.93 | 5.17 (3.70,7.22) | <0.001 | 5.44 (3.89,7.61) | <0.001 |
PY: Person-years; IR: Incidence rate per 1,000 person-years; HR: Hazard ratio; CI: Confidence interval.
*: Model was adjusted for age, urbanization, insurance premium, occupation, estrogen treatment, and Charlson comorbidity index.
For osteoporosis or bone fracture, compared with the women without hysterectomy and oophorectomy, the women with only hysterectomy had a higher risk of 2.26-fold (95% CI = 2.09–2.44). The risk of osteoporosis in women with hysterectomy only was also significantly higher than that in the comparison group (aHR = 1.52, 95% CI = 1.36–1.71).
For hip fracture, the hysterectomy had no higher risk than the comparison cohort (aHR = 1.07, 95% CI = 0.64–1.79). For vertebral fracture, the hysterectomy only had a higher risk than the comparison cohort (aHR = 4.92, 95% CI = 3.78–6.40). For other bone fracture, the risk in women with hysterectomy only was 3.97-fold (95%CI = 3.49–4.51) higher than that of the comparison cohort.
Bilateral oophorectomies also associated with an increased risk of osteoporosis and bone fracture in the comparison group and in the hysterectomy group (aHR = 2.04, 95% CI = 1.55–2.67; aHR = 2.95, 95% CI = 2.33–3.73, respectively).
Subgroup analysis of the risk of osteoporosis or fracture with age
The incidence rate and HR of osteoporosis or fracture in women with hysterectomy or oophorectomy stratified by age are shown in Table 3.
Table 3. Adjusted hazard ratio and 95% confidence interval of osteoporosis or fracture between women with hysterectomy or oophorectomy stratified by age.
| Comparison group without oophorectomy | Comparison group with oophorectomy | Hysterectomy only | Hysterectomy with oophorectomy | ||||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR* (95% CI) | p-value | HR* (95% CI) | p-value | HR* (95% CI) | p-value | |
| Osteoporosis | |||||||
| All | 1.00 (reference) | 0.84 (0.59,1.2) | 0.35 | 1.44 (1.28,1.61) | <0.001 | 1.30 (0.94,1.82) | 0.12 |
| Age | |||||||
| 30–39 | 1.00 (reference) | 0.77 (0.24,2.48) | 0.66 | 2.31 (1.39,3.84) | 0.001 | 1.00 (0.14,7.28) | 1.00 |
| 40–49 | 1.00 (reference) | 1.05 (0.61,1.82) | 0.86 | 1.67 (1.42,1.97) | <0.001 | 2.03 (1.38,2.99) | <0.001 |
| 50–59 | 1.00 (reference) | 2.46 (1.43,4.22) | 0.001 | 1.18 (0.90,1.56) | 0.23 | 0.84 (0.37,1.88) | 0.67 |
| ≧60 | 1.00 (reference) | 0.41 (0.1,1.65) | 0.21 | 1.37 (1.08,1.74) | 0.01 | 0.55 (0.14,2.23) | 0.41 |
| Hip fracture | |||||||
| All | 1.00 (reference) | 1.52 (0.56,4.17) | 0.41 | 0.92 (0.55,1.54) | 0.74 | 1.00 (0.25,4.08) | 1.00 |
| Age | |||||||
| 30–39 | 1.00 (reference) | -- | 7.87 (1.20,51.62) | 0.03 | -- | ||
| 40–49 | 1.00 (reference) | -- | 1.19 (0.48,2.95) | 0.70 | 1.90 (0.26,14.14) | 0.53 | |
| 50–59 | 1.00 (reference) | 4.50 (0.56,36.26) | 0.16 | 0.91 (0.20,4.15) | 0.90 | 3.09 (0.38,24.87) | 0.29 |
| ≧60 | 1.00 (reference) | 3.84 (1.18,12.47) | 0.02 | 0.76 (0.34,1.70) | 0.51 | -- | |
| Vertebral fracture | |||||||
| All | 1.00 (reference) | 2.47 (1.25,4.88) | 0.01 | 4.67 (3.59,6.08) | <0.001 | 2.75 (1.28,5.91) | 0.01 |
| Age | |||||||
| 30–39 | 1.00 (reference) | 1.25 (0.15,10.57) | 0.84 | 8.60 (3.4,21.72) | <0.001 | 5.99 (0.73,48.92) | 0.09 |
| 40–49 | 1.00 (reference) | 3.00 (1.21,7.43) | 0.02 | 3.19 (2.22,4.56) | <0.001 | 2.98 (1.20,7.41) | 0.02 |
| 50–59 | 1.00 (reference) | 5.70 (0.71,45.90) | 0.10 | 10.03 (4.38,22.97) | <0.001 | 3.59 (0.44,29.31) | 0.23 |
| ≧60 | 1.00 (reference) | 6.15 (1.43,26.45) | 0.01 | 7.73 (4.45,13.43) | <0.001 | -- | |
| Other bone fracture | |||||||
| All | 1.00 (reference) | 2.83 (2.10,3.80) | <0.001 | 3.91 (3.44,4.45) | <0.001 | 4.16 (3.10,5.57) | <0.001 |
| Age | |||||||
| 30–39 | 1.00 (reference) | 3.27 (1.66,6.45) | <0.001 | 6.31 (4.09,9.74) | <0.001 | 9.50 (4.38,20.63) | <0.001 |
| 40–49 | 1.00 (reference) | 2.76 (1.79,4.25) | <0.001 | 3.33 (2.83,3.92) | <0.001 | 4.18 (2.95,5.92) | <0.001 |
| 50–59 | 1.00 (reference) | 4.78 (2.30,9.95) | <0.001 | 4.51 (3.26,6.26) | <0.001 | 2.85 (1.24,6.59) | 0.01 |
| ≧60 | 1.00 (reference) | 8.49 (3.82,18.88) | <0.001 | 5.93 (4.04,8.72) | <0.001 | 1.75 (0.24,12.79) | 0.58 |
PY: Person-years; IR: Incidence rate per 1,000 person-years; HR: Hazard ratio; CI: Confidence interval.
*: Model was adjusted for age, urbanization, insurance premium, occupation, estrogen treatment, and Charlson comorbidity index.
For osteoporosis, the hysterectomy only women had a higher risk than the women without hysterectomy and oophorectomy in age group 30 to 39 (aHR = 2.31, 95% CI = 1.39–3.84), age group 40 to 49 (aHR = 2.03, 95% CI = 1.38–2.99) and in those over 60 years old (aHR = 1.37, 95% CI = 1.08–1.74). The women with hysterectomy plus oophorectomy also had a higher risk than the women without hysterectomy and oophorectomy in 40- to 49-year-olds (aHR = 2.03, 95% CI = 1.38–2.99).
For hip, the hysterectomy only women a higher risk than the women without hysterectomy and oophorectomy in age group 30–39 (aHR = 7.87, 95% CI = 1.20, 51.62).
The risk of vertebral fracture and other bone fracture were higher in women with hysterectomy only than those without hysterectomy among all age groups.
Risk of vertebral and other bone fractures
Tables 4 and 5 present the risks of vertebral fracture and other fractures in women with hysterectomy compared with the comparison group stratified by follow-up year.
Table 4. Risk of vertebral fracture in women with hysterectomy compared with the comparison group stratified by follow-up year.
| Comparison group | Hysterectomy | Crude | Adjusted* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Follow time | N | Event | PY | IR | N | Event | PY | IR | HR (95% CI) | p-value | HR (95% CI) | p-value |
| <5 | 32189 | 54 | 148499 | 0.36 | 8267 | 59 | 39044 | 1.51 | 4.37 (3.02,6.33) | <0.001 | 4.33 (2.99,6.28) | <0.001 |
| 5–9 | 32135 | 47 | 114049 | 0.41 | 8208 | 49 | 30847 | 1.59 | 4.09 (2.74,6.10) | <0.001 | 3.89 (2.60,5.82) | <0.001 |
| ≧9 | 32088 | 13 | 138354 | 0.09 | 8159 | 19 | 38228 | 0.50 | 5.71 (2.82,11.55) | <0.001 | 5.42 (2.66,11.01) | <0.001 |
PY: Person-years; IR: Incidence rate per 1,000 person-years; HR: Hazard ratio; CI: Confidence interval.
*: Model was adjusted for age, urbanization, insurance premium occupation, estrogen treatment, and Charlson comorbidity index.
Table 5. Risk of other bone fractures in women with hysterectomy compared with the comparison group stratified by follow-up year.
| Comparison group | Hysterectomy | Crude | Adjusted* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Follow time | N | Event | PY | IR | N | Event | PY | IR | HR (95% CI) | p-value | HR (95% CI) | p-value |
| <5 | 32602 | 299 | 148499 | 2.01 | 8643 | 283 | 39044 | 7.25 | 3.69 (3.13,4.34) | <0.001 | 3.61 (3.06,4.25) | <0.001 |
| 5–9 | 32303 | 159 | 114049 | 1.39 | 8360 | 154 | 30847 | 4.99 | 3.76 (3.01,4.7) | <0.001 | 3.68 (2.95,4.60) | <0.001 |
| ≧9 | 32144 | 69 | 138354 | 0.50 | 8206 | 66 | 38228 | 1.73 | 3.73 (2.66,5.22) | <0.001 | 3.69 (2.63,5.17) | <0.001 |
PY: Person-years; IR: Incidence rate per 1,000 person-years; HR: Hazard ratio; CI: Confidence interval.
*: Model was adjusted for age, urbanization, insurance premium, occupation, estrogen treatment, and Charlson comorbidity index.
For the vertebral fracture, compared with the comparison cohort, the hysterectomy cohort had a 4.33-fold (95% CI = 2.99–6.28) higher risk in five years or shorter of follow up time, 3.89-fold (95% CI = 2.60–5.82) after five to nine years of follow-up and a 5.42-fold (95% CI = 2.66–11.01) higher risk after more than nine years of follow-up (Table 4).
For other fractures, the adjusted hazards were about 3.6 to 3.7 in every follow-up periods. (Table 5).
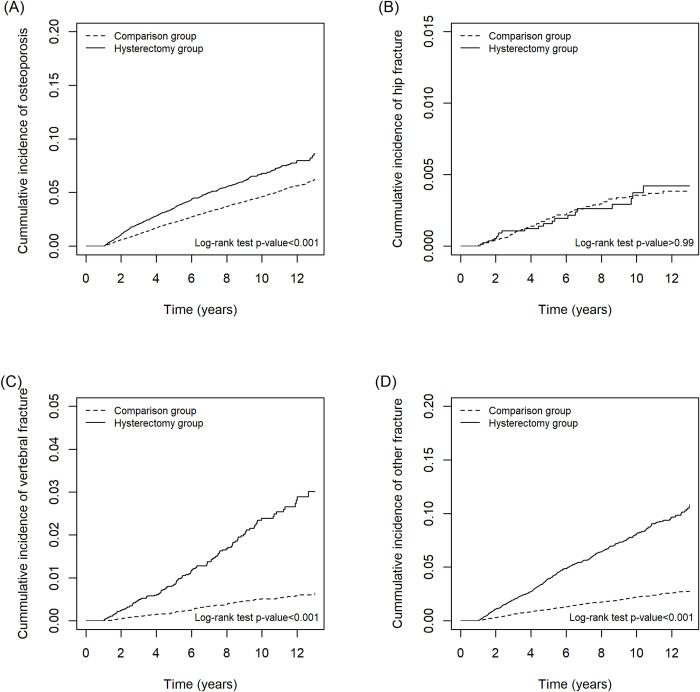
Fig 2 presents the cumulative incidence of each event shown by the Kaplan–Meier curves for osteoporosis, hip fracture, vertebral fracture, and other fractures outcomes.
Fig 2.
Kaplan–Meier curves showing the cumulative incidence of (A) osteoporosis, (B) hip fracture, (C) vertebral fracture, and (D) other fracture in women receiving hysterectomy (dashed line) compared with the age- and comorbidity-matched comparison group (solid line).
Stratified analysis between ET and hysterectomy on the risk of osteoporosis and fracture
Table 6 attempted to evaluate the interaction of ET and hysterectomy on the risk of osteoporosis and fracture. Women with ET alone increased risk of osteoporosis or bone fracture (adjusted incidence rate ratio [IRR] = 3.49, 95% CI = 2.10–5.81). Moreover, the adjusted IRR of hip fracture was increased to 9.59 (95% CI = 2.33–39.58) and that of vertebral fracture was increase to 26.33 (95% CI = 11.44, 60.60) in women with ET only. For women with both hysterectomy and ET, the adjusted IRR of Osteoporosis or bone fracture and Other bone fracture were 2.74 (95% CI = 1.23–6.12) and 6.73 (95% CI = 2.51–18.05), respectively.
Table 6. The incidence rate ratio of osteoporosis or fracture interacts with estrogen treatment.
| IRR (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hysterectomy | Estrogen treatment | N | Event | PY | IR | Crude | p-value | Adjusted* | p-value |
| Osteoporosis or bone fracture | |||||||||
| No | No | 33833 | 1852 | 251443 | 7.37 | 1.00 (reference) | 1.00 (reference) | ||
| No | Yes | 59 | 15 | 450 | 33.31 | 4.65 (2.80,7.73) | <0.001 | 3.49 (2.10,5.81) | <0.001 |
| Yes | No | 9151 | 1043 | 64012 | 16.29 | 2.09 (1.93,2.25) | <0.001 | 2.05 (1.90,2.21) | <0.001 |
| Yes | Yes | 38 | 6 | 208 | 28.85 | 2.89 (1.30,6.44) | <0.001 | 2.74 (1.23,6.12) | 0.01 |
| Osteoporosis | |||||||||
| No | No | 33180 | 1149 | 247968 | 4.63 | 1.00 (reference) | 1.00 (reference) | ||
| No | Yes | 49 | 5 | 398 | 12.57 | 2.95 (1.22,7.09) | 0.02 | 2.18 (0.90,5.25) | 0.08 |
| Yes | No | 8527 | 419 | 60769 | 6.90 | 1.42 (1.27,1.59) | <0.001 | 1.41 (1.26,1.58) | <0.001 |
| Yes | Yes | 34 | 2 | 193 | 10.36 | 1.70 (0.42,6.80) | 0.45 | 1.55 (0.39,6.20) | 0.54 |
| Hip fracture | |||||||||
| No | No | 32111 | 80 | 242384 | 0.33 | 1.00 (reference) | 1.00 (reference) | ||
| No | Yes | 46 | 2 | 374 | 5.35 | 17.45 (4.29,70.99) | <0.001 | 9.59 (2.33,39.58) | 0.002 |
| Yes | No | 8128 | 20 | 58914 | 0.34 | 0.99 (0.61,1.61) | 0.96 | 1.01 (0.62,1.64) | 0.98 |
| Yes | Yes | 32 | 0 | 187 | 0.00 | -- | -- | ||
| Vertebral fracture | |||||||||
| No | No | 32139 | 108 | 242607 | 0.45 | 1.00 (reference) | 1.00 (reference) | ||
| No | Yes | 50 | 6 | 402 | 14.94 | 35.71 (15.7,81.25) | <0.001 | 26.33 (11.44,60.60) | <0.001 |
| Yes | No | 8235 | 127 | 59515 | 2.13 | 4.59 (3.55,5.93) | <0.001 | 4.45 (3.44,5.76) | <0.001 |
| Yes | Yes | 32 | 0 | 187 | 0.00 | -- | -- | ||
| Other bone fracture | |||||||||
| No | No | 32556 | 525 | 244617 | 2.15 | 1.00 (reference) | 1.00 (reference) | ||
| No | Yes | 46 | 2 | 369 | 5.42 | 2.70 (0.67,10.81) | 0.16 | 2.59 (0.65,10.41) | 0.18 |
| Yes | No | 8607 | 499 | 61372 | 8.13 | 3.60 (3.18,4.06) | <0.001 | 3.53 (3.12,3.99) | <0.001 |
| Yes | Yes | 36 | 4 | 202 | 19.81 | 6.89 (2.58,18.43) | <0.001 | 6.73 (2.51,18.05) | <0.001 |
PY: Person-years; IR: Incidence rate per 1,000 person-years; HR: Hazard ratio; CI: Confidence interval.
*: Model was adjusted for age, urbanization, insurance premium, occupation, estrogen treatment, and Charlson comorbidity index.
Discussion
This population cohort study evaluated 9,189 hysterectomized women and 33,942 matched comparisons. Both groups were primarily middle-aged women with a median age of 45. After a median of 6.66 years of follow-up, women with hysterectomy had an overall 2.26-fold higher risk of developing osteoporosis or fracture. Furthermore, the hysterectomized women had a 4.92-fold higher risk of vertebral fracture compared with the comparison group.
Anti-Mullerian hormone (AMH) was used to quantify the ovarian reserve [21]. The normal value is between 2–4 ng/ml [22]. Several longitudinal studies about ovary-sparing hysterectomy with ovarian reserve have shown that premenopausal hysterectomy can cause earlier ovarian failure and decrease AMH levels one year after the procedure [23,24]. There are multiple theories of why hysterectomy with ovarian reserve leads to ovarian failure, including decreased blood flow to the ovaries after utero-ovarian ligament ligation, paracrine or endocrine effects from the uterus to the ovary, or an increase in uterus inhibition of pituitary follicle-stimulating hormone [12]. The previous study explored whether laparoscopic hysterectomy could affect ovarian reserve compared to non-laparoscopic hysterectomy. They showed both kinds of hysterectomy could decrease AMH [25]. Moreover, in the laparoscopy group, the cause of decreasing AMH may be due to electrocauterization. A randomized trial of hysterectomy with or without salpingectomy also showed decreased AMH (from 1.44 to 1.13 ng/ml) after both kinds of surgeries [26]. However, we did not have data of the AMH of each woman in our database. In our study, we found hysterectomy itself could be associated with an increased risk of osteoporosis and fracture might related to a decreased AMH.
Premenopausal oophorectomy can cause immediate surgical-related menopause. Ovarian dysfunction contributes to bone mineral density decline and increases the risk of osteoporosis and fracture [27,28]. The previous study showed postmenopausal women received BSO, the risk of fracture increased than the expected fracture rate (standardized incidence ratio [SIR], 1.54; 95% CI, 1.29–1.82) [29]. They concluded postmenopausal androgen produced by ovary may associated with a decreased incidence of fracture. However, a prospective cohort study examined the association between hysterectomy plus BSO and hip fracture risk, they found BSO were not associated with an increased risk of hip fracture (HR = 0.83 [95% CI = 0.63–1.10]) [30]. The same with the above study, our study found women with hysterectomy plus bilateral oophorectomy associated with an increased risk of osteoporosis or bone fracture.
Hormone therapy (HT) may decrease the risk of osteoporosis and bone fracture [31]. One systematic review including 28 studies had been shown the overall relative risk of HT was 0.74 (95% CI 0.69–0.80) for total fractures, 0.72 (95% CI 0.53–0.98) for hip fractures, and 0.63 (95% CI 0.44–0.91) for vertebral fractures [31]. However, the other study showed estrogen therapy was not associated with a reduction in overall fracture risk (hazard ratio [HR], 0.90; 95% CI, 0.64–1.28) and osteoporotic fractures (HR, 0.80; 95% CI, 0.52–1.23) [29]. Another study also showed the standard dose of HT was not adequate for bone mineral density in premature ovarian failure women [32]. In this study, we found the association between estrogen therapy and the risk of osteoporosis and bone fracture.
A national cohort study from South Korea revealed that osteoporosis had an aHR of 1.45 in the hysterectomy group, which was similar to our study [12]. However, the risk of the major complication was in osteoporosis and fracture was not investigated. In our study, we found a nearly 4.5-fold increased risk of vertebral fracture in the hysterectomy group. Furthermore, vertebral fracture had the highest risk during more than nine years of long-term follow-up.
Bone density decline is the main reason for osteoporotic fracture, and it independently increases the incidence of fracture [33]. Vertebral and femoral fractures are the two leading locations of osteoporotic fractures. According to a worldwide study, vertebral fractures comprise 16% of total osteoporotic fractures [34]. Furthermore, women with a vertebral fracture experience a 3.7 times higher mortality rate during the first year after vertebral fracture compared with those who did not have a vertebral fracture.
Controversially, a population-based cohort study in 2008 reported that hysterectomy elevated overall fracture risk, but the only statistically significant increases were found for fractures in the hands and feet. No significant increase in fractures was found in traditional osteoporotic fracture sites such as the hip, spine, or distal forearm [11]. A possible reason for these different results is that this study included cancer and pre-cancerous conditions in their operation indication, which might affect the fracture risk.
Strengths and limitations
Our study is population-based assessment research, and this study design can minimize selection bias. Additionally, the study data were adjusted through conventional medical histories, related comorbidities, and comorbidity severity. However, our study has some potential limitations. First, medications or supplements that may be related to osteoporosis or fracture were not considered. There are several different types of supplements that claim to prevent osteoporosis, such as fish oil, Vitamin D, glucosamine, etc. Second, lab data including bone mineral density, calcium, magnesium, and phosphate levels were not collected in the TNHI database. Third, the diagnostic code for fractures could not differentiate between osteoporotic fractures or fractures caused by other reasons. Instead, we considered the two leading sites of osteoporotic fractures, hip and vertebral, in our study subjects. Fourth, the proportion of CCI at 1 or 2 was higher in the hysterectomy group than in the comparison group, which may be a potential confounder. Body mass index, alcohol consumption, history of endocrine disease, physical inactivity, medication, eating habits, family history of osteoporosis, and smoking history are also important factors in the risk of osteoporosis. However, they were not recorded in the database. Taking oral contraceptives may also contribute to the risk of osteoporosis. However, the database also did not record the prescription of oral contraceptives due to self-paid.
Conclusion
Hysterectomy might be associated with the slightly increased risk of osteoporosis and vertebral fracture in middle-aged women. Based on the study results, women who undergo hysterectomy should be screened more readily or counseled regarding this risk of osteoporosis or fracture.
Abbreviations
- CI
confidence interval
- HR
hazard ratio
- LHID
Longitudinal Health Insurance Database
- MrOS
Osteoporotic Fractures in Men
- TNHI
Taiwan National Health Insurance
- NHIRD
National Health Insurance Research Database
- OR
odds ratio
- CCI
Charlson comorbidity index
- BSO
bilateral salpingo-oophorectomy
- SIR
standardized incidence ratio
- ET
estrogen therapy
- HT
Hormone therapy
- AMH
anti-Mullerian hormone
- IRR
incidence rate ratio
Data Availability
All relevant data were showed in the manuscript.
Funding Statement
This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212- 133004), China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021), MOST Clinical Trial Consortium for Stroke (MOST 107-2321-B-039 -004-), Tseng-Lien Lin Foundation, Taichung, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
References
- 1.Yu P-A, Hsu W-H, Hsu W-B, Kuo L-T, Lin Z-R, Shen W-J, et al. The effects of high impact exercise intervention on bone mineral density, physical fitness, and quality of life in postmenopausal women with osteopenia: A retrospective cohort study. Medicine. 2019;98: e14898 10.1097/MD.0000000000014898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O’Malley CD. Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos. 2014;9: 182 10.1007/s11657-014-0182-3 [DOI] [PubMed] [Google Scholar]
- 3.Masi L. Epidemiology of osteoporosis. Clin Cases Miner Bone Metab. 2008;5: 11–13. [PMC free article] [PubMed] [Google Scholar]
- 4.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10: 937–948. 10.2147/TCRM.S72456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu M-P, Huang K-H, Long C-Y, Tsai E-M, Tang C-H. Trends in various types of surgery for hysterectomy and distribution by patient age, surgeon age, and hospital accreditation: 10-year population-based study in Taiwan. J Minim Invasive Gynecol. 2010;17: 612–619. 10.1016/j.jmig.2010.04.010 [DOI] [PubMed] [Google Scholar]
- 6.Falcone T, Walters MD. Hysterectomy for benign disease. Obstet Gynecol. 2008;111: 753–767. 10.1097/AOG.0b013e318165f18c [DOI] [PubMed] [Google Scholar]
- 7.Ding D-C, Chu T-Y, Chang Y-H. Trend changes in the proportion of minimal invasive hysterectomies over a five-year period: A single-center experience. Tzu Chi Med J. 2012;24: 136–138. [Google Scholar]
- 8.Siddle N, Sarrel P, Whitehead M. The effect of hysterectomy on the age at ovarian failure: identification of a subgroup of women with premature loss of ovarian function and literature review. Fertil Steril. 1987;47: 94–100. 10.1016/s0015-0282(16)49942-5 [DOI] [PubMed] [Google Scholar]
- 9.Durães Simões R, Chada Baracat E, Szjenfeld VL, de Lima GR, José Gonçalves W, de Carvalho Ramos Bortoletto C. Effects of simple hysterectomy on bone loss. Sao Paulo Med J. 1995;113: 1012–1015. 10.1590/s1516-31801995000600003 [DOI] [PubMed] [Google Scholar]
- 10.Larcos G. Hysterectomy with ovarian conservation: effect on bone mineral density. Aust N Z J Obstet Gynaecol. 1998;38: 452–454. 10.1111/j.1479-828x.1998.tb03111.x [DOI] [PubMed] [Google Scholar]
- 11.Melton LJ 3rd, Achenbach SJ, Gebhart JB, Babalola EO, Atkinson EJ, Bharucha AE. Influence of hysterectomy on long-term fracture risk. Fertil Steril. 2007;88: 156–162. 10.1016/j.fertnstert.2006.11.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi HG, Jung YJ, Lee SW. Increased risk of osteoporosis with hysterectomy: A longitudinal follow-up study using a national sample cohort. Am J Obstet Gynecol. 2019;220: 573.e1–573.e13. 10.1016/j.ajog.2019.02.018 [DOI] [PubMed] [Google Scholar]
- 13.Shen Y-C, Chen W, Tsai I-J, Wang J-H, Lin S-Z, Ding D-C. Association of hysterectomy with bipolar disorder risk: A population-based cohort study. Depress Anxiety. 2019;36: 543–551. 10.1002/da.22904 [DOI] [PubMed] [Google Scholar]
- 14.Lin L-Y, Warren-Gash C, Smeeth L, Chen P-C. Data resource profile: the National Health Insurance Research Database (NHIRD). Epidemiol Health. 2018;40: e2018062 10.4178/epih.e2018062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hung L-C, Sung S-F, Hsieh C-Y, Hu Y-H, Lin H-J, Chen Y-W, et al. Validation of a novel claims-based stroke severity index in patients with intracerebral hemorrhage. J Epidemiol. 2017;27: 24–29. 10.1016/j.je.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lix LM, Quail J, Teare G, Acan B. Performance of comorbidity measures for predicting outcomes in population-based osteoporosis cohorts. Osteoporos Int. 2011;22: 2633–2643. 10.1007/s00198-010-1516-7 [DOI] [PubMed] [Google Scholar]
- 17.Liu CY, Hung YT, Chuang YL, Chen YJ, Weng… - J Health Manag WS, 2006. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. 2006. [Google Scholar]
- 18.Lin S-M, Yang S-H, Liang C-C, Huang H-K. Proton pump inhibitor use and the risk of osteoporosis and fracture in stroke patients: a population-based cohort study. Osteoporos Int. 2018;29: 153–162. 10.1007/s00198-017-4262-2 [DOI] [PubMed] [Google Scholar]
- 19.McGregor JC, Kim PW, Perencevich EN, Bradham DD, Furuno JP, Kaye KS, et al. Utility of the Chronic Disease Score and Charlson Comorbidity Index as comorbidity measures for use in epidemiologic studies of antibiotic-resistant organisms. Am J Epidemiol. 2005;161: 483–493. 10.1093/aje/kwi068 [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40: 373–383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 21.Szydłowska I, Marciniak A, Brodowska A, Lisak M, Przysiecka S, Różański J. Assessment of ovarian reserve as an indicator of fertility and health consequences in patients with chronic kidney disease stages 3–4. Gynecol Endocrinol. 2018;34: 944–948. 10.1080/09513590.2018.1473364 [DOI] [PubMed] [Google Scholar]
- 22.Chen M-J, Yang W-S, Chen C-L, Wu M-Y, Yang Y-S, Ho H-N. The relationship between anti-Mullerian hormone, androgen and insulin resistance on the number of antral follicles in women with polycystic ovary syndrome. Hum Reprod. 2008;23: 952–957. 10.1093/humrep/den015 [DOI] [PubMed] [Google Scholar]
- 23.Moorman PG, Myers ER, Schildkraut JM, Iversen ES, Wang F, Warren N. Effect of hysterectomy with ovarian preservation on ovarian function. Obstet Gynecol. 2011;118: 1271–1279. 10.1097/AOG.0b013e318236fd12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morin NA. Association of Ovary-Sparing Hysterectomy With Ovarian Reserve. Obstetrics and gynecology. 2016. p. 655 10.1097/AOG.0000000000001606 [DOI] [PubMed] [Google Scholar]
- 25.Cho H-Y, Park ST, Kyung MS, Park S-H. Assessment of ovarian reserve after hysterectomy: Laparoscopic vs. non-laparoscopic surgery. Eur J Obstet Gynecol Reprod Biol. 2017;210: 54–57. 10.1016/j.ejogrb.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 26.Asgari Z, Tehranian A, Rouholamin S, Hosseini R, Sepidarkish M, Rezainejad M. Comparing surgical outcome and ovarian reserve after laparoscopic hysterectomy between two methods of with and without prophylactic bilateral salpingectomy: A randomized controlled trial. J Cancer Res Ther. 2018;14: 543–548. 10.4103/0973-1482.193114 [DOI] [PubMed] [Google Scholar]
- 27.Szeliga A, Maciejewska-Jeske M, Męczekalski B. Bone health and evaluation of bone mineral density in patients with premature ovarian insufficiency. Prz Menopauzalny. 2018;17: 112–116. 10.5114/pm.2018.78552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prior JC, Vigna YM, Wark JD, Eyre DR, Lentle BC, Li DKB, et al. Premenopausal ovariectomy-related bone loss: a randomized, double-blind, one-year trial of conjugated estrogen or medroxyprogesterone acetate. J Bone Miner Res. 1997;12: 1851–1863. 10.1359/jbmr.1997.12.11.1851 [DOI] [PubMed] [Google Scholar]
- 29.Melton LJ 3rd, Khosla S, Malkasian GD, Achenbach SJ, Oberg AL, Riggs BL. Fracture risk after bilateral oophorectomy in elderly women. J Bone Miner Res. 2003;18: 900–905. 10.1359/jbmr.2003.18.5.900 [DOI] [PubMed] [Google Scholar]
- 30.Jacoby VL, Grady D, Wactawski-Wende J, Manson JE, Allison MA, Kuppermann M, et al. Oophorectomy vs ovarian conservation with hysterectomy: cardiovascular disease, hip fracture, and cancer in the Women’s Health Initiative Observational Study. Arch Intern Med. 2011;171: 760–768. 10.1001/archinternmed.2011.121 [DOI] [PubMed] [Google Scholar]
- 31.Zhu L, Jiang X, Sun Y, Shu W. Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials. Menopause. 2016;23: 461–470. 10.1097/GME.0000000000000519 [DOI] [PubMed] [Google Scholar]
- 32.Giraldo H, Benetti-Pinto C, Ferreira V, Garmes H, Yela D, Giraldo P. Standard hormone therapy is inadequate for bone density in premature ovarian insufficiency. Gynecol Endocrinol. 2017;33: 283–286. 10.1080/09513590.2016.1257602 [DOI] [PubMed] [Google Scholar]
- 33.Watson NR, Studd JW, Garnett T, Savvas M, Milligan P. Bone loss after hysterectomy with ovarian conservation. Obstet Gynecol. 1995;86: 72–77. 10.1016/0029-7844(95)00100-6 [DOI] [PubMed] [Google Scholar]
- 34.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17: 1726–1733. 10.1007/s00198-006-0172-4 [DOI] [PubMed] [Google Scholar]