Abstract
Parkinson’s disease (PD) is diagnosed when patients exhibit bradykinesia with tremor and/or rigidity, and when these symptoms respond to dopaminergic medications. Yet in the last years there was a greater recognition of additional aspects of the disease including non-motor symptoms and prodromal states with associated pathology in various regions of the nervous system. In this review we discuss current concepts of two major alterations found during the course of the disease: cytoplasmic aggregates of the protein α-synuclein and the degeneration of dopaminergic neurons. We provide an overview of new approaches in this field based on current concepts and latest literature. In many areas, translational research on PD has advanced the understanding of the disease but there is still a need for more effective therapeutic options based on the insights into the basic biological phenomena.
Keywords: α-Synuclein, Pre-formed fibrils, Protein aggregates, Aggresome, Dopamine deficiency, Medium spiny neurons, Autophagy
Introduction to Parkinson’s disease (PD)
PD is diagnosed when patients exhibit bradykinesia with tremor and/or rigidity, and when these symptoms respond to dopaminergic medications [1]. In the past few years, additional aspects of the disease including non-motor symptoms and prodromal states with associated pathology in various regions of the nervous system gained increasing attention. The non-motor symptoms affect the quality of life because they cannot be treated as well as the typical motor symptoms, thus constituting one of the most important therapeutic challenges in PD therapy. The other challenge lies in the management of motor fluctuations, i.e. the PD motor symptoms remain responsive to dopaminergic medications but the mobility is tightly linked to serum concentrations, which requires short dosing-intervals or the use of medication pumps. In the brains of PD patients, we have found two major pathologies, cytoplasmic aggregates of alpha-synuclein (aSyn) and degeneration of dopaminergic neurons. The current therapies and translational research are focusing on these two aspects, which will be discussed in the following.
Part 1: Synuclein pathology
In 1997, we began to know that rare familial forms of PD could be caused by point mutations in the aSyn gene SNCA [2], including the mutations of A53T, A30P, E46K, H50Q and G51D, and duplication of the SNCA locus. In addition, polymorphisms in the SNCA locus are a risk factor for sporadic PD [3, 4]. Following the detection of PD-associated mutations, aSyn was identified as a major constituent of Lewy bodies (LB) [5]. These cytosolic inclusions of aggregated proteins were first described histologically by Fritz Heinrich Lewy in 1912 and associated with PD by Konstantin Nikolaevich Trétiakoff in 1919 [6]. Almost a century later, Heiko Braak described the distribution of LB in the brain and suggested that the aSyn pathology spreads along the axonal projections [7]. According to this concept, the aSyn pathology starts in the periphery and enters the brain through the olfactory bulb or along the vagal nerve [8]. Then it spreads transsynaptically to the limbic system respectively to further brainstem nuclei including the substantia nigra pars compacta. Subsequently, the pathology spreads to the neocortical areas [9].
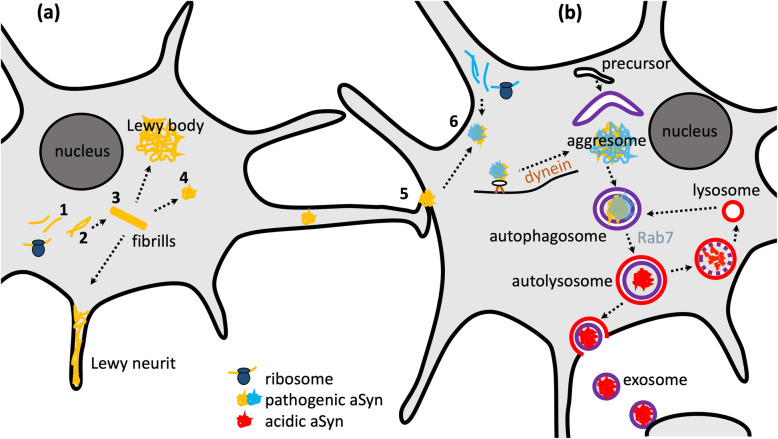
Lewy neurites are swollen neurites that contain aSyn filaments [10] and in fact incorporate the majority of aSyn aggregates [11]. Dystrophic aSyn-positive neurites have also been observed in the peripheral nervous system [12]. In addition to PD, other disorders are also associated with aSyn aggregates, including dementia with Lewy bodies and multisystem atrophy (MSA). In MSA, aSyn aggregates are located in glial rather than in neuronal cells [13]. The emergence and spread of the aSyn pathology are illustrated in Fig. 1a.
Fig. 1.
Aggregation, transport and clearance of α-synuclein. a Concept of aggregation and spreading: After ribosomal translation of pathogenic α-synuclein (aSyn), monomers (1) form oligomers (2) and primary nucleation with formation of the first aggregate takes place. Subsequent steps are fibril elongation (3) and secondary nucleation with formation of further nuclei, e.g. by fibrils breaking (4). The aggregates are transported along the axonal projections, secreted and taken up by a neighboring cell (5). The aggregation of aSyn monomers is greatly enhanced by addition of even small quantities of aggregates, which serve as nuclei and replace the slow step of primary nucleation by the faster step of secondary nucleation. This process is called seeding (6). b Transport and autophagic clearance of aSyn: Aggregates are dynein-dependently transported to the perinuclear region to form aggresomes. Parts of the cytosol containing aggregates get engulfed by a membrane to form autophagosomes. Subsequently, Rab7 regulates the trafficking of autophagosomal and lysosomal vesicles and their fusion towards autolysosomes, followed by degradation of the vesicle content. There is also evidence for the secretion via exosomal release
Clinical correlates of synuclein pathology
The concept of the spreading aSyn pathology has convinced clinicians because it is consistent with the fact that PD motor symptoms are accompanied by and often preceded by non-motor symptoms. This concept also led to the definition of prodromal or pre-motor stage of PD [14]. Early non-motor symptoms include hyposmia [15] – plausibly caused by aSyn pathology in the olfactory bulb - and gastrointestinal symptoms [16] – plausibly caused by aSyn pathology in the vagus nerve. The rapid-eye-movement sleep behavioral disorder is caused by dysfunction of a specific brainstem nucleus and is one of the most specific predictors of PD [17]. The most important non-motor symptom of advanced PD is dementia, which is plausibly caused by cortical aSyn pathology [18].
It should be noted, however, that the correlation between the distribution of Lewy bodies in the brain and clinical symptoms is not perfect. There are patients with “incidental” Lewy bodies that clinically do not differ from age-matched controls and patients with an “atypical” distribution pattern of aSyn pathology [19]. Furthermore, even some familial forms of PD lack Lewy bodies [20]. Some authors have argued that the clinical symptoms are better explained by the distribution of Lewy neurites than by Lewy bodies given that the former likely produce greater functional impairment [21].
The non-motor symptoms are prominent features of PD and constitute a major impact on quality of life [22]. This can be attributed to the fact that classical motor symptoms respond well to dopaminergic medication, whereas symptomatically, the non-motor symptoms often cannot be treated well.
Synuclein aggregation and spreading
aSyn aggregation has been studied extensively in vitro, using biophysical methods to assess different steps of the aggregation process and measure different aSyn species [23]. Steps of aggregation include primary nucleation (i.e. formation of the first aggregate from monomeric aSyn), fibril elongation/aggregate growth, and secondary nucleation (formation of further nuclei, e.g. by fibrils breaking) (Fig. 1a). Small molecules can inhibit the aggregation by interfering with any of these steps [24, 25]. We have recently demonstrated that an engineered β-wrappin can bind to the αSyn monomer and prevent aSyn aggregation in a substoichiometric manner [23]. Aggregation of aSyn monomer is greatly enhanced by addition of even small quantities of aggregates, which serve as nuclei and replace the slow step of primary nucleation by the faster step of secondary nucleation. This process is called seeding (step 6 in Fig. 1).
The spread of aSyn pathology through the brain can therefore be decomposed into three distinct processes: (i) the transport of aSyn aggregates along the axonal projections to new brain areas, (ii) the secretion and uptake of aSyn aggregates and (iii) seeding (Fig. 1). The transport was initially described as mainly retrograde, but both directions have been observed in cellular and mouse models [26, 27]. The mechanisms of secretion and uptake remain to be clarified, however, the exosomal release and endocytosis have been proposed to be involved [28–30]. Some evidence has suggested that the aSyn secretion is dependent on the presynaptic activity [31–33] and the lysosomal processing may also be involved in the transmission [34, 35]. The endogenous synuclein and a fibrillary structure of aSyn are not essential for the spread of aSyn through the brain [36, 37], and environmental toxins can trigger aSyn aggregation [8].
Although aSyn fibrils consisting largely of beta-sheets are considered the major constituents of Lewy bodies and Lewy neurites, the beta-sheet formation is not necessary for aSyn toxicity [38, 39]. One of the most controversial questions about aSyn aggregation is whether different synucleinopathies, specifically PD and MSA, are characterized and/or caused by different “strains” of aSyn aggregates [40]. A recent refinement of the “protein misfolding cyclic amplification” method has indicated that PD and MSA are indeed characterized by different strains of aSyn aggregates and that their differences can be detected even in cerebrospinal fluid from PD and MSA patients [41]. Also in mouse models, different pathologies have been observed following injection of “PD” and “MSA” seeds [42, 43].
Aggregate clearance and functional significance of Lewy bodies
Cells do not remain passive to the formation of aSyn aggregates. Using fluorescently tagged aSyn and live-cell microscopy we observed active transport of aSyn aggregates towards a perinuclear region where aggregates accumulate [44]. This region is called aggresome and is located at the microtubule organizing center [45]. The transport of aggregates towards the aggresome is mediated by microtubules and dynein motors (Fig. 1b). Aggregates are recruited to dynein motors by different adaptor proteins, including p62, heat-shock proteins and HDAC6 [46]. Ubiquitination is a typical first step for the recognition of aggregates by this system, but it is neither necessary nor required [47].
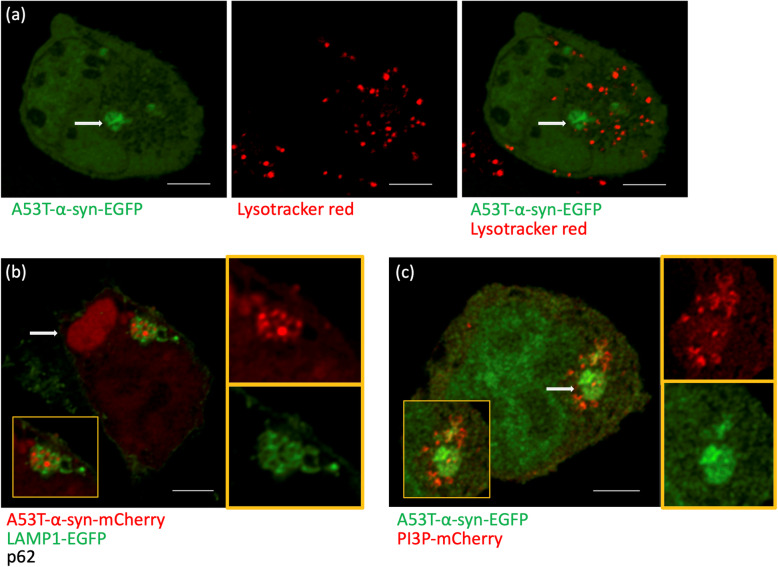
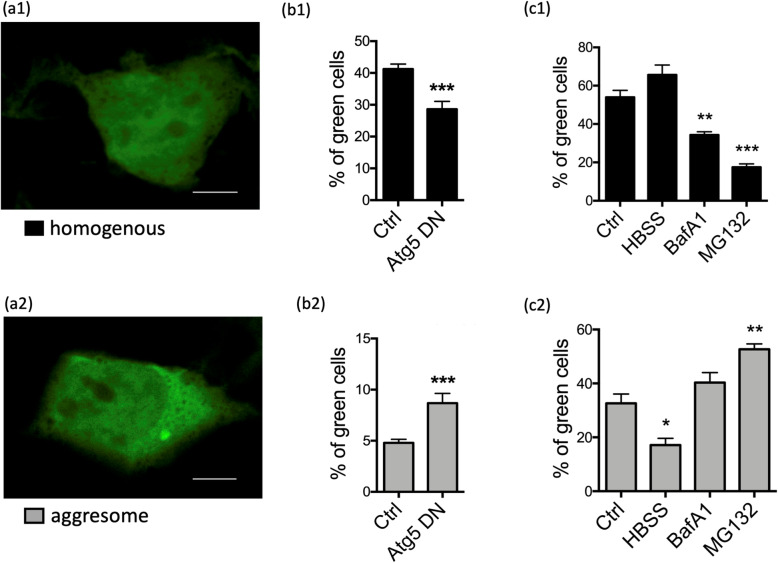
Cells can degrade aSyn aggregates [44] and they do so mainly by autophagy [48] (Fig. 1b). Autophagy can be stimulated by starvation and by other mechanisms including the Ras-related in brain 7 (Rab7) pathway [49]. The purpose of aggregate transport to the aggresome is to bring together the aggregates and the degradation machinery, i.e. precursors of autophagic vesicles [46, 50]. Autophagosomes are degraded by fusion with lysosomes. This accumulation of autophagosomes and lysosomes around aggresomes and aggregates is illustrated in Fig. 2. Consequently, interfering with dynein functions impairs autophagic degradation of protein aggregates [51]. Overexpression of the cargo protein p62 leads to the formation of large “p62 bodies”, which are to some extent similar to aggresomes [52]. The P62 bodies are also observed with coexpression of p62 and aSyn (Fig. 2b). Autophagy can be induced by starvation (“HBSS” in Fig. 3c1 and c2), leading to more cells without aggregates and a particularly strong reduction of aggresomes rather than that of small dispersed aggregates. The increased aggregate clearance was also observed to be induced by Rab7 and its effector FYCO1 (FYVE and coiled-coil domain 1) [49, 53]. Conversely, blocking the induction of autophagy with a dysfunctional version of the autophagic membrane protein Atg5 leads to a strong increase of aggresomes (Fig. 3b2) and the presence of p62 bodies in neurons of mouse cortex and striatum [52]. The autophagic clearance can also be inhibited by bafilomycin, which blocks the fusion of autophagosomes with lysosomes (Fig. 3c1 and c2). Inhibiting the proteasome (e.g. by MG132) also leads to a strong increase in aggresomes (Fig. 3c2), but this effect is based on the fact that the proteasome clears monomeric synuclein [48]. Thus the proteasome inhibition increases aggregates by increased formation but not by reduced clearance. This reasoning highlights the importance of time-resolved laboratory methods like time-lapse imaging.
Fig. 2.
α-Synuclein particles and acidic compartments by light microscopy. a Deconvolved confocal images of live HEK293T cells transfected with A53T-α-synuclein (Syn)-EGFP and treated with lysotracker red for 2 h at 37 °C. Arrows show an aggresome. Note the distribution of lysotracker-positive vesicles close to the aggresome and other αSyn aggregates. b Deconvolved confocal image of HEK293T cells transfected with A53T-α-Syn-mCherry, the lysosomal marker LAMP1-EGFP and the cargo protein p62 without fluorescent tag. Enlarged insets show a cluster of LAMP1-decorated vesicles colocalizing with aSyn. Arrow shows a large aggresome, so called “p62 body”. c Deconvolved confocal image of HEK293T cells transfected with A53T-α-syn-EGFP and a biosensor of the autophagosome lipid phosphatidylinositol 3-phosphate (PI3P) tagged to mCherry. Enlarged insets show the PI3P-positive vesicles around the aggresome (arrow), consistent with the hypothesis that autophagosomes degrade aggresomes. In panels b-c, the red and green channels of the insets are shown individually next to the merged images. Scale bars, 5 μm. Original data
Fig. 3.
α-Synuclein and autophagy. a HEK293 cells were transfected with EGFP-tagged A53T-α-synuclein and manually classified due to the distribution of EGFP. a1 A representative example of homogenous distribution of EGFP, as the healthy phenotype. a2 A representative example of a cell containing an aggresome. Scale bars, 5 μm. b HEK293 cells were transfected with EGFP-tagged A53T-α-synuclein and the dominant negative version of autophagy-related protein 5 (Atg5). Significances from t-test; n = 3 independent experiments. c HEK293 cells were transfected with EGFP-tagged A53T-α-synuclein and cells were incubated with 0.2 μM Bafilomycin A1 (BafA1) for 4 h to block autophagy or with 5 μM proteasome inhibitor MG132 for 4 h. Starvation was induced by complete medium exchange for Hank’s balanced salts (HBSS) for 4 h. One-way ANOVA was significant, results from post-hoc test are indicated (n = 3 independent experiments). Graphs represent mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001. Original data
Lewy bodies are related to aggresomes [54] and thus signal the occurrence of aggregated proteins. Yet, they are considered part of the cellular defense against protein aggregates and not toxic per se. Aggresomes are the meeting place for aggregates, autophagic membranes, and even lysosomes. Consequently, they are composed not only of densely packed aggregates but also of other cellular components including microtubule-associated proteins [55] and vesicle membranes [56]. The formation of Lewy bodies is in fact a slow maturation process that involves many steps after accumulation of aggregates and vesicles, including posttranslational modifications of aSyn [57]. These findings provide an explanation for the observation in our own work of vesicles positive for the autophagosome lipid phosphatidylinositol 3-phosphate (Fig. 3c) and Rab7 [49].
Open questions and future perspectives
Several antibodies against aSyn are currently under testing in PD patients. They are well tolerated and have shown a reduction of serum aSyn [58]. This strategy builds on early findings in an aSyn-based mouse model [59, 60], but important questions remain unresolved: (1) What is the ideal epitope against which, antibodies should be targeted? Is it the C-terminus or the N-terminus? Is it monomers, oligomers or fibrils, full-length or truncated aSyn, native or aSyn with posttranslational modifications? (2) Can systemic administration of an antibody deplete aSyn in the brain? Could intrathecal antibodies deplete aSyn in the basal ganglia and brainstem nuclei? (3) How often will antibodies have to be applied and how long will it take to expect an effect on PD symptoms? Can we expect an effect even in manifested PD or do we have to start even earlier? (4) Which PD symptoms are good primary endpoints for aSyn-directed trials? Since dopamine depletion is already quite advanced at the time of diagnosis, and since the dopamine-responsive symptoms are alleviated by current treatments, the non-motor symptoms likely are better candidates. But which non-motor symptoms can be assessed quantitatively and progress in a linear way?
While some of these questions can only be addressed in PD patients, some can be addressed in aSyn-based animal models - certainly in the near future. Which is the best animal model for these investigations? In rodents, many current studies used viral overexpression of aSyn or the administration of pre-formed aSyn fibrils [42, 61–63]. Viral overexpression induces aSyn aggregates, degeneration of dopaminergic neurons and a behavioral phenotype [64, 65]. The validity of aSyn overexpression is supported by the fact that PD can be caused by triplications of the aSyn locus and that polymorphisms in the aSyn promoter region (which affect aSyn expression levels) are important risk factors for sporadic PD. Fibrils can be generated in vitro from recombinant aSyn protein [66], and have been extracted from diseased brains of rodent models or patients [67, 68]. These models have been instrumental to investigate the existence of aSyn strains (see above) and support prion-like properties of aSyn pathology [69]. Work on aSyn aggregation in PD patients is hampered by the fact that brain pathology is available only post mortem. aSyn-based biomarkers in cerebrospinal fluid are under way [70], but still much less developed than for Alzheimer’s disease. aSyn pathology in skin biopsies has shown promise to develop into a biomarker to confirm the diagnosis and possibly even quantify synucleinopathy [71].
Part 2: Dopamine deficiency
Responsiveness of PD motor symptoms to dopaminergic medication is one of the great medical achievements of the twentieth century [72], constitutes a major diagnostic criterion [1], and highlights the importance of dopaminergic neuron degeneration in PD. Still, many fundamental questions remain unresolved, including the question why dopaminergic neurons in the substantia nigra degenerate in PD even though they are not the only or even the first neurons to show aSyn pathology. Moreover, it has remained enigmatic through which changes in neuronal structure and/or function dopamine deficiency causes PD motor symptoms.
Selective vulnerability of substantia nigra dopaminergic neurons
Many types of neurons acquire aSyn pathology, but it is mainly dopaminergic neurons in the substantia nigra pars compacta (SNc) that degenerate in PD. Further cell types include noradrenaline and serotonin neurons in the locus coeruleus and raphe [73, 74]. It is therefore plausible to assume that the catecholamine production renders neurons particularly sensitive to neurodegeneration and aSyn toxicity. Indeed, dopamine can form toxic quinones with aSyn [75] and oxidative stress is critical for the propagation of aSyn pathology [8, 64] and neuronal dysfunction [76]. Moreover, catecholamine synthesis is associated with oxidative stress and dopaminergic neurons predominantly degenerate upon systemic exposure to mitochondrial complex I inhibitors such as rotenone [77]. This is consistent with the epidemiological finding that exposure to insecticides constitutes a risk factor for PD [78, 79]. Conversely, aSyn modulates dopaminergic neurotransmission [80], and the induction of aSyn pathology leads to degeneration of dopaminergic neurons [81, 82].
Yet, there are also arguments against the notion that dopamine production is the critical feature that explains degeneration of this neuronal population in PD. The most important argument is the fact that the neighboring population of dopaminergic neurons in the ventral tegmental area degenerates much less in PD patients. Moreover, even among the dopaminergic neurons of the SNc, caudal and ventrolateral subpopulations are affected more strongly [83]. Consequently, additional features of SNc dopaminergic neurons have been tested for their capacity to explain selective vulnerability. These features include firing patterns, specific ion channels and morphological features such as their long and highly branched axons [84–86].
The latter aspect is supported by the notion that dopaminergic axon terminals in the striatum degenerate earlier in PD than their somata in the substantia nigra [87]. The fact that most of the striatal axon terminals are already lost at the time of diagnosis (and at least 50% of substantia nigra dopaminergic neurons) indicates that there is a long time of prodromal PD, consistent with the findings from Lewy pathology. The advanced degeneration of the dopaminergic system at the time of diagnosis means that the dynamic range for further neurodegeneration after diagnosis is small. Classical dopamine-dependent motor symptoms are therefore not good candidates to monitor neurodegeneration in clinical trials with possible neuroprotective strategies. In addition, this notion gives rise to the question of what underlies the qualitative differences between the response to dopaminergic medications in early as compared to advanced PD patients (see below).
Effects of dopamine deficiency on neuronal activity
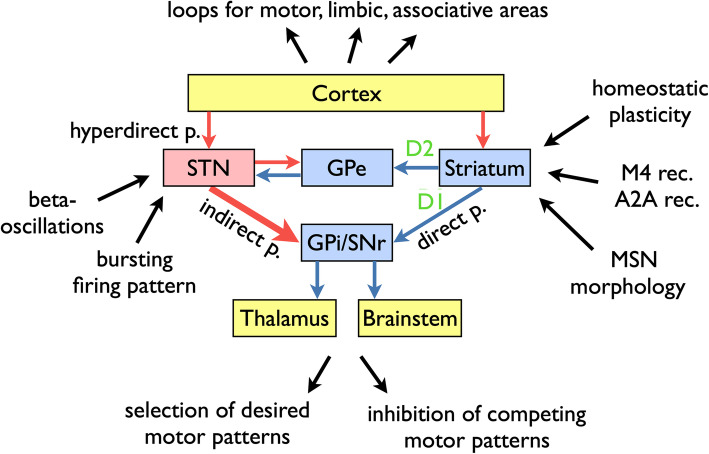
The dominating model of how dopamine deficiency causes the cardinal motor symptoms was established based on the electrophysiological recordings in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-treated primates [88]. Since its original description, it has been modified and expanded [89, 90]. In the “rate model” [91] (Fig. 4), the striatum functions as the primary entry structure for the basal ganglia and projects to its output nuclei (globus pallidus par interna, GPi, and substantia nigra pars reticulata, SNr) through two pathways: the direct pathway consists of D1 dopamine receptor-bearing striato-pallidal projection neurons; and the indirect pathway is gated by D2 dopamine receptors and projects from striatum to the output nuclei through the globus pallidus pars externa and the subthalamic nucleus (STN). The GABAergic output nuclei project to the thalamus (primarily ventral anterior and ventral lateral nuclei).
Fig. 4.
Schematic representation of the basal ganglia circuitry and changes observed in PD patients and models. Distinct loops exist for motor, limbic and associative circuitry. The basal ganglia disinhibit desired motor patterns and inhibit competing motor patterns. The circuitry includes the direct pathway from striatum to GPi/SNr, gated by D1 dopamine receptors, the indirect pathway through GPe and STN, gated by D2 dopamine receptors, and the hyperdirect pathway from cortex to STN. The striatal circuitry is modulated in addition by M4 muscarine and A2A adenosine receptors. In PD, changes occur not only in the firing rate (in particular increased rate of STN firing), but also in the firing patterns, notably the pathological beta-oscillation and increased firing in bursts. Chronic dopamine deficiency leads to the (homeostatic) changes in MSN excitability and morphology. Display of circuitry inspired by Hutchison et al., 2004 [91]. Blue arrows indicate GABAergic projections, and red arrows indicate glutamatergic projections. Abbreviations: p, pathway; rec., receptor; STN, subthalamic nucleus; GPe, globus pallidus pars externa; GPi, globus pallidus pars interna; SNr, substantia nigra pars reticulata; MSN, medium spiny neurons
The physiological function of this basal ganglia circuitry is to gate motor patterns, i.e., it serves as a “brake” for movements. This brake is too tight in PD and not tight enough in chorea. Our current understanding of basal ganglia functioning includes the following additional aspects:
The basal ganglia are not simply a brake but both serve to allow (disinhibit) a desired motor pattern and inhibit competing motor patterns [92].
The striatum is not the only input structure for the basal ganglia; there is also a “hyperdirect pathway” to the subthalamic nucleus [91].
Movements are not only regulated by the projection from GPi/SNr to the thalamus but also through projections to brainstem nuclei, in particular the pedunculopontine nucleus [90].
The basal ganglia are not one big structure for motor control, but consist of several loops that regulate motor, limbic and associative functions [93].
Explaining the therapeutic mechanism of chronic high-frequency stimulation of the STN in PD patients has been a major challenge for the basal ganglia model. One solution to this challenge is to focus on the spatial and temporal patterns of neuronal activity, instead of the overall firing rate. For instance, recordings in PD patients and nonhuman primate models have suggested that a bursting firing pattern is more common and that correlations between neurons are altered [90]. Moreover, oscillations in the basal ganglia circuitry are important determinants of patients’ mobility [91, 94, 95]. Beta oscillations in particular are associated with impaired movement. Their detection can be used to find the best spot for therapeutic STN stimulation. The specific inhibition of these oscillations by phase-locked stimulation can change PD motor symptoms. Importantly, only altered firing patterns and oscillations but not changes in firing rate can explain the emergence of tremor in PD patients. In simple terms, therapeutic deep brain stimulation works mainly by cancelling these pathological firing patterns but not by altering the overall rate of neuronal activity.
Cellular consequences of dopamine deficiency
Dopaminergic neurons project to virtually all areas of the brain. The densest network of dopaminergic axon terminals is located in the striatum. Spiny projection neurons (or medium spiny neurons, MSNs) are the most abundant cell type in the striatum and thus are most directly affected by dopamine deficiency in PD. From the rate model explained above, we expect D1-MSNs to be less active with dopamine depletion and D2-MSNs to be hyperactive. Yet, MSNs do not remain passive with dopamine depletion. Animal experiments have shown that MSNs rather change their excitability in order to compensate for the loss of dopaminergic innervation. Thus, D1-MSNs increase their electrical excitability and D2-MSNs decrease their electrical excitability after prolonged dopamine depletion. In addition, both types of MSN also change their morphology, showing less complex dendritic arborizations and fewer spines with a reduced number of glutamatergic synapses [96–98]. Similar changes in MSN dendritic arborizations have also been observed in PD patients [99].
These findings – primarily in PD rodent models – highlight the notion that even though it is dopaminergic neurons that degenerate in PD, many more cell types change their functioning in response to dopamine depletion. These “homeostatic” changes are affected by dopaminergic mediation [97, 98] and both the consequences of dopamine depletion and the consequences of excessive dopamine substitution might not be fully reversible. Accordingly, even transient administration of dopamine antagonists can induce lasting movement disorders termed tardive dyskinesias [100].
Moreover, the clinical effects of dopaminergic medications last much longer than what would be expected from pharmacokinetics alone. For levodopa, this “long-duration response” [101] has been partially explained by levodopa storage in dopaminergic terminals. Yet, a long duration response is also seen for dopamine agonists with short half-life [102]. In the classical ELLDOPA trial, the long-duration response - i.e. the difference after 2 weeks without medication in patients either treated for 1 year with levodopa as compared to placebo – made up 50% of the total response to levodopa [103]. It is plausible to assume that the changes in MSN excitability and morphology at least partially underlie the long-duration response to dopamine depletion and dopaminergic medication.
In addition to facilitating movement, dopamine serves as a reward-based teaching signal in many brain areas [104]. Consequently, dopamine deficiency not only leads to the altered steady-state activity, excitability and morphology, but in addition to alterations in long-term potentiation (LTP) and long-term depression (LTD), the neurophysiological correlates of learning and memory. Specifically, dopamine depletion reduces both LTP and LTD induction in the striatum. Short-term and long-term dopamine substitution have different effects, with short-term substitution leading to recovery of LTP and LTD and long-term high-dose substitution leading to a loss of LTD and a loss of LTP depotentiation [105]. These effects could underlie the occurrence of dyskinesias and impulse control disorder in PD patients.
Future perspectives for translational research
At the timepoint of PD diagnosis, motor symptoms can be readily and continually alleviated by dopaminergic medication whereas in advanced disease, dopaminergic medication may trigger dyskinesia and hallucinations and the duration of the effect is much shorter. The majority of dopaminergic axon terminals are already lost at the timepoint of diagnosis [87]. The qualitative and quantitative differences in the response to dopamine between early and late PD can not only be explained by the progressive loss of dopaminergic terminals. Rather, adaptive and maladaptive changes in the striatum and further basal ganglia nuclei must contribute to these differential effects. We are only beginning to understand the molecular mechanisms behind these changes. Even fundamental biological phenomena such as the adaptation in electrical excitability in response to the changing synaptic inputs are only beginning to be unraveled [106]. Cellular and animal models of dopamine depletion will be critical to address these questions and hold great promise to develop new non-dopaminergic therapies that have the potential to avoid these long-term consequences of dopamine depletion and substitution. In this research, classical toxin-based models of PD (like the 6-OHDA or MPTP models) are used not to study the pathways of dopaminergic neuron degeneration but to determine the consequences of long-term dopamine deficiency. In particular, therapeutic approaches with striatal interneurons [107], M4 muscarine receptors [108] and A2A adenosine receptors [109] have shown promising results.
Conclusion
PD is a paradigmatic neurodegenerative and movement disorder. Translational studies are aimed into understanding PD pathogenesis and pathophysiology and addressing diverse areas of biophysics, cell biology and neuroscience. In most aspects we have only given a broad overview of current concepts. For a more detailed description we refer to the suggested reading listed below. In many areas, translational research on PD has catalyzed a better understanding of basic biological phenomena, including intrinsically disordered proteins, autophagy, mitochondrial function, homeostatic plasticity and basal ganglia physiology. In some instances, we even had to revise fundamental biological concepts. For instance, the spread of individual aSyn molecules across several synapses and the emerging knowledge about exosomes indicate that neurons are less self-contained entities as stated by the “neuron doctrine” that has dominated neuroscience since the 1890s. Translational research is appealing because of its inherent promise to produce new and refined treatments for human diseases. But it requires a detailed understanding of basic biological phenomena and therefore cannot be conceived without basic sciences.
Suggested reading
Synuclein pathology
Braak H, Ghebremedhin E, Rüb U, Bratzke H, Del Tredici K. Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res. 2004;318:121–134.
Synuclein aggregation and aggregation inhibitors
Pujols J, Peña-Díaz S, Pallarès I, Ventura S. Chemical chaperones as novel drugs for Parkinson’s disease. Trends Mol Med. 2020;26:408–421.
Aggregate clearance and the functional significance of Lewy bodies
Lamark T, Johansen T. Aggrephagy: selective disposal of protein aggregates by macroautophagy. Int J Cell Biol. 2012;2012:736905–21.
Selective vulnerability of substantia nigra dopaminergic neurons
Surmeier DJ, Obeso JA, Halliday GM. Selective neuronal vulnerability in Parkinson disease. Nat Rev. Neurosci. 2017;18:101–113.
Effects of dopamine deficiency on neuronal activity
Wichmann T. Changing views of the pathophysiology of Parkinsonism. Mov Disord 2019;34:1130–1143.
Cellular consequences of dopamine deficiency
Zhai S, Shen W, Graves SM, Surmeier DJ. Dopaminergic modulation of striatal function and Parkinson’s disease. J Neural Transm. 2019;126: 411–422.
Acknowledgements
Not applicable.
Abbreviations
- aSyn
alpha-synuclein
- Atg5
Autophagy related 5
- GPe
Globus pallidus pars externa
- GPi
Globus pallidus par interna
- LTD
Long-term depression
- LTP
Long-term potentiation
- MSN
Medium spiny neuron
- PD
Parkinson’s disease
- Rab7
Ras-related in brain 7
- SNc
Substantia nigra pars compacta
- SNr
Substantia nigra pars reticulate
- STN
Subthalamic nucleus
Authors’ contributions
ED interpreted the relevant literature and wrote the manuscript with support from BF. Conception was done by BF and ED. TS and LD carried out the experiments. HR and BF substantively revised it. All authors read and approved the final manuscript.
Funding
Work in the Falkenburger lab was funded by the German Research Foundation (DFG, FA 658/3–1). Open Access funding enabled and organized by Projekt DEAL
Availability of data and materials
The raw data and materials used and mentioned in Figs. 2 and 3 are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591–1601. doi: 10.1002/mds.26424. [DOI] [PubMed] [Google Scholar]
- 2.Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, et al. Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science. 1997;276(5321):2045–2047. doi: 10.1126/science.276.5321.2045. [DOI] [PubMed] [Google Scholar]
- 3.Klein C, Westenberger A. Genetics of Parkinson’s disease. Cold Spring Harb Perspect Med. 2012;2(1):a008888. doi: 10.1101/cshperspect.a008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singleton AB, Hardy JA, Gasser T. The birth of the modern era of Parkinson’s disease genetics. J Parkinsons Dis. 2017;7(s1):S87–S93. doi: 10.3233/JPD-179009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spillantini MG, Schmidt ML, Lee VMY, Trojanowski JQ, Jakes R, Goedert M. Alpha-synuclein in Lewy bodies. Nature. 1997;388(6645):839–840. doi: 10.1038/42166. [DOI] [PubMed] [Google Scholar]
- 6.Holdorff B, Rodrigues e Silva AM, Dodel R. Centenary of Lewy bodies (1912–2012) J Neural Transm. 2013;120(4):509–516. doi: 10.1007/s00702-013-0984-2. [DOI] [PubMed] [Google Scholar]
- 7.Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197–211. doi: 10.1016/S0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 8.Pan-Montojo F, Schwarz M, Winkler C, Arnhold M, O’Sullivan GA, Pal A, et al. Environmental toxins trigger PD-like progression via increased alpha-synuclein release from enteric neurons in mice. Sci Rep. 2012;2(1):898. doi: 10.1038/srep00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beach TG, Adler CH, Lue L, Sue LI, Bachalakuri J, Henry-Watson J, et al. Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol. 2009;117(6):613–634. doi: 10.1007/s00401-009-0538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M. alpha-Synuclein in filamentous inclusions of Lewy bodies from Parkinson’s disease and dementia with lewy bodies. Proc Natl Acad Sci U S A. 1998;95(11):6469–6473. doi: 10.1073/pnas.95.11.6469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz-Schaeffer WJ. The synaptic pathology of alpha-synuclein aggregation in dementia with Lewy bodies, Parkinson“s disease and Parkinson”s disease dementia. Acta Neuropathol. 2010;120(2):131–143. doi: 10.1007/s00401-010-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doppler K, Brockmann K, Sedghi A, Wurster I, Volkmann J, Oertel WH, et al. Dermal phospho-alpha-synuclein deposition in patients with Parkinson’s disease and mutation of the glucocerebrosidase gene. Front Neurol. 2018;9:1094. doi: 10.3389/fneur.2018.01094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wakabayashi K, Yoshimoto M, Tsuji S, Takahashi H. Alpha-synuclein immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett. 1998;249(2–3):180–182. doi: 10.1016/S0304-3940(98)00407-8. [DOI] [PubMed] [Google Scholar]
- 14.Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois B, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord. 2015;30(12):1600–1611. doi: 10.1002/mds.26431. [DOI] [PubMed] [Google Scholar]
- 15.Haehner A, Masala C, Walter S, Reichmann H, Hummel T. Incidence of Parkinson’s disease in a large patient cohort with idiopathic smell and taste loss. J Neurol. 2019;266(2):339–345. doi: 10.1007/s00415-018-9135-x. [DOI] [PubMed] [Google Scholar]
- 16.Klingelhoefer L, Reichmann H. The gut and nonmotor symptoms in Parkinson’s disease. Int Rev Neurobiol. 2017;134:787–809. doi: 10.1016/bs.irn.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 17.Krohn L, Wu RYJ, Heilbron K, Ruskey JA, Laurent SB, Blauwendraat C, et al. Fine-mapping of SNCA in rapid eye movement sleep behavior disorder and overt synucleinopathies. Ann Neurol. 2020;87(4):584–98. doi: 10.1002/ana.25687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith C, Malek N, Grosset K, Cullen B, Gentleman S, Grosset DG. Neuropathology of dementia in patients with Parkinson’s disease: a systematic review of autopsy studies. J Neurol Neurosurg Psychiatry. 2019;90(11):1234–1243. doi: 10.1136/jnnp-2019-321111. [DOI] [PubMed] [Google Scholar]
- 19.Coughlin DG, Petrovitch H, White LR, Noorigian J, Masaki KH, Ross GW, et al. Most cases with Lewy pathology in a population-based cohort adhere to the Braak progression pattern but “failure to fit” is highly dependent on staging system applied. Parkinsonism Relat Disord. 2019;64:124–131. doi: 10.1016/j.parkreldis.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wszolek ZK, Pfeiffer RF, Tsuboi Y, Uitti RJ, McComb RD, Stoessl AJ, et al. Autosomal dominant parkinsonism associated with variable synuclein and tau pathology. Neurology. 2004;62(9):1619–1622. doi: 10.1212/01.WNL.0000125015.06989.DB. [DOI] [PubMed] [Google Scholar]
- 21.Schulz-Schaeffer WJ. Neurodegeneration in Parkinson disease: moving Lewy bodies out of focus. Neurology. 2012;79(24):2298–2299. doi: 10.1212/WNL.0b013e318278b6a7. [DOI] [PubMed] [Google Scholar]
- 22.Martinez Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR. NMSS Validation Group. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord. 2011;26(3):399–406. doi: 10.1002/mds.23462. [DOI] [PubMed] [Google Scholar]
- 23.Agerschou ED, Flagmeier P, Saridaki T, Galvagnion C, Komnig D, Heid L, et al. An engineered monomer binding-protein for α-synuclein efficiently inhibits the proliferation of amyloid fibrils. Elife. 2019;8:e46112. doi: 10.7554/eLife.46112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pujols J, Peña-Díaz S, Pallarès I, Ventura S. Chemical chaperones as novel drugs for Parkinson’s disease. Trends Mol Med. 2020;26(4):408–421. doi: 10.1016/j.molmed.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Burmann BM, Gerez JA, Matečko-Burmann I, Campioni S, Kumari P, Ghosh D, et al. Regulation of α-synuclein by chaperones in mammalian cells. Nature. 2020;577(7788):127–132. doi: 10.1038/s41586-019-1808-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mao X, Ou MT, Karuppagounder SS, Kam TI, Yin X, Xiong Y, et al. Pathological α-synuclein transmission initiated by binding lymphocyte-activation gene 3. Science. 2016;353(6307):1513. doi: 10.1126/science.aah3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freundt EC, Maynard N, Clancy EK, Roy S, Bousset L, Sourigues Y, et al. Neuron-to-neuron transmission of α-synuclein fibrils through axonal transport. Ann Neurol. 2012;72(4):517–524. doi: 10.1002/ana.23747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stopschinski BE, Holmes BB, Miller GM, Manon VA, Vaquer-Alicea J, Prueitt WL, et al. Specific glycosaminoglycan chain length and sulfation patterns are required for cell uptake of tau versus α-synuclein and β-amyloid aggregates. J Biol Chem. 2018;293(27):10826–10840. doi: 10.1074/jbc.RA117.000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ngolab J, Trinh I, Rockenstein E, Mante M, Florio J, Trejo M, et al. Brain-derived exosomes from dementia with Lewy bodies propagate α-synuclein pathology. Acta Neuropathol Comm. 2017;5(1):46. doi: 10.1186/s40478-017-0445-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Danzer KM, Kranich LR, Ruf WP, Cagsal-Getkin O, Winslow AR, Zhu L, et al. Exosomal cell-to-cell transmission of alpha synuclein oligomers. Mol Neurodegener. 2012;7:42. doi: 10.1186/1750-1326-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emmanouilidou E, Minakaki G, Keramioti MV, Xylaki M, Balafas E, Chrysanthou-Piterou M, et al. GABA transmission via ATP-dependent K+ channels regulates α-synuclein secretion in mouse striatum. Brain. 2016;139(Pt 3):871–890. doi: 10.1093/brain/awv403. [DOI] [PubMed] [Google Scholar]
- 32.Saridaki T, Falkenburger BH. Transport and clearance of α-synuclein aggregates. FASEB. 2014;18:1–42. [Google Scholar]
- 33.Yamada K, Iwatsubo T. Extracellular α-synuclein levels are regulated by neuronal activity. Mol Neurodegener. 2018;13(1):9–8. doi: 10.1186/s13024-018-0241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karpowicz RJ, Haney CM, Mihaila TS, Sandler RM, Petersson EJ, Lee VMY. Selective imaging of internalized proteopathic α-synuclein seeds in primary neurons reveals mechanistic insight into transmission of synucleinopathies. J Biol Chem. 2017;292(32):13482–13497. doi: 10.1074/jbc.M117.780296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abounit S, Bousset L, Loria F, Zhu S, de Chaumont F, Pieri L, et al. Tunneling nanotubes spread fibrillar α-synuclein by intercellular trafficking of lysosomes. EMBO J. 2016;35(19):2120–2138. doi: 10.15252/embj.201593411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helwig M, Klinkenberg M, Rusconi R, Musgrove RE, Majbour NK, El-Agnaf OMA, et al. Brain propagation of transduced α-synuclein involves non-fibrillar protein species and is enhanced in α-synuclein null mice. Brain. 2016;139(Pt 3):856–870. doi: 10.1093/brain/awv376. [DOI] [PubMed] [Google Scholar]
- 37.Ulusoy A, Musgrove RE, Rusconi R, Klinkenberg M, Helwig M, Schneider A, et al. Neuron-to-neuron α-synuclein propagation in vivo is independent of neuronal injury. Acta Neuropathologica Communications. 2015;3(1):197. doi: 10.1186/s40478-015-0198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karpinar DP, Balija MBG, Kügler S, Opazo F, Rezaei-Ghaleh N, Wender N, et al. Pre-fibrillar alpha-synuclein variants with impaired beta-structure increase neurotoxicity in Parkinson’s disease models. EMBO J. 2009;28(20):3256–3268. doi: 10.1038/emboj.2009.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prots I, Grosch J, Brazdis RM, Simmnacher K, Veber V, Havlicek S, et al. α-Synuclein oligomers induce early axonal dysfunction in human iPSC-based models of synucleinopathies. Proc Natl Acad Sci U S A. 2018;115(30):7813–7818. doi: 10.1073/pnas.1713129115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peelaerts W, Bousset L, Baekelandt V, Melki R. ɑ-Synuclein strains and seeding in Parkinson’s disease, incidental Lewy body disease, dementia with Lewy bodies and multiple system atrophy: similarities and differences. Cell Tissue Res. 2018;105(20):84–18. doi: 10.1007/s00441-018-2839-5. [DOI] [PubMed] [Google Scholar]
- 41.Shahnawaz M, Mukherjee A, Pritzkow S, Mendez N, Rabadia P, Liu X, et al. Discriminating α-synuclein strains in Parkinson’s disease and multiple system atrophy. Nature. 2020;578(7794):273–277. doi: 10.1038/s41586-020-1984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peelaerts W, Bousset L, Van der Perren A, Moskalyuk A, Pulizzi R, Giugliano M, et al. α-Synuclein strains cause distinct synucleinopathies after local and systemic administration. Nature. 2015;522(7556):340–344. doi: 10.1038/nature14547. [DOI] [PubMed] [Google Scholar]
- 43.Lau A, So RWL, Lau HHC, Sang JC, Ruiz-Riquelme A, Fleck SC, et al. α-Synuclein strains target distinct brain regions and cell types. Nat Neurosci. 2020;23(1):21–31. doi: 10.1038/s41593-019-0541-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Opazo F, Krenz A, Heermann S, Schulz JB, Falkenburger BH. Accumulation and clearance of -synuclein aggregates demonstrated by time-lapse imaging. J Neurochem. 2008;106(2):529–540. doi: 10.1111/j.1471-4159.2008.05407.x. [DOI] [PubMed] [Google Scholar]
- 45.Kopito RR. Aggresomes, inclusion bodies and protein aggregation. Trends Cell Biol. 2000;10(12):524–530. doi: 10.1016/S0962-8924(00)01852-3. [DOI] [PubMed] [Google Scholar]
- 46.Lamark T, Johansen T. Aggrephagy: selective disposal of protein aggregates by macroautophagy. Int J Cell Biol. 2012;2012(12):736905–736921. doi: 10.1155/2012/736905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bersuker K, Brandeis M, Kopito RR. Protein misfolding specifies recruitment to cytoplasmic inclusion bodies. J Cell Biol. 2016;213(2):229–241. doi: 10.1083/jcb.201511024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ebrahimi-Fakhari D, Cantuti-Castelvetri I, Fan Z, Rockenstein E, Masliah E, Hyman BT, et al. Distinct roles in vivo for the ubiquitin-proteasome system and the autophagy-lysosomal pathway in the degradation of α-synuclein. J Neurosci. 2011;31(41):14508–14520. doi: 10.1523/JNEUROSCI.1560-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dinter E, Saridaki T, Nippold M, Plum S, Diederichs L, Komnig D, et al. Rab7 induces clearance of α-synuclein aggregates. J Neurochem. 2016;138(5):758–774. doi: 10.1111/jnc.13712. [DOI] [PubMed] [Google Scholar]
- 50.Iwata A, Riley BE, Johnston JA, Kopito RR. HDAC6 and microtubules are required for autophagic degradation of aggregated huntingtin. J Biol Chem. 2005;280(48):40282–40292. doi: 10.1074/jbc.M508786200. [DOI] [PubMed] [Google Scholar]
- 51.Ravikumar B, Acevedo-Arozena A, Imarisio S, Berger Z, Vacher C, O’Kane CJ, et al. Dynein mutations impair autophagic clearance of aggregate-prone proteins. Nat Genet. 2005;37(7):771–776. doi: 10.1038/ng1591. [DOI] [PubMed] [Google Scholar]
- 52.Liu X, Li Y, Wang X, Xing R, Liu K, Gan Q, et al. The BEACH-containing protein WDR81 coordinates p62 and LC3C to promote aggrephagy. J Cell Biol. 2017;216(5):1301–1320. doi: 10.1083/jcb.201608039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saridaki T, Nippold M, Dinter E, Roos A, Diederichs L, Fensky L, et al. FYCO1 mediates clearance of α-synuclein aggregates through a Rab7-dependent mechanism. J Neurochem. 2018;146(4):474–492. doi: 10.1111/jnc.14461. [DOI] [PubMed] [Google Scholar]
- 54.Olanow CW, Perl DP, DeMartino GN, McNaught KSP. Lewy-body formation is an aggresome-related process: a hypothesis. Lancet Neurol. 2004;3(8):496–503. doi: 10.1016/S1474-4422(04)00827-0. [DOI] [PubMed] [Google Scholar]
- 55.McCormack A, Keating DJ, Chegeni N, Colella A, Wang JJ, Chataway T. Abundance of synaptic vesicle-related proteins in alpha-synuclein-containing protein inclusions suggests a targeted formation mechanism. Neurotox Res. 2019;35(4):883–897. doi: 10.1007/s12640-019-00014-0. [DOI] [PubMed] [Google Scholar]
- 56.Shahmoradian SH, Lewis AJ, Genoud C, Hench J, Moors TE, Navarro PP, et al. Lewy pathology in Parkinson’s disease consists of crowded organelles and lipid membranes. Nat Neurosci. 2019;22(7):1099–1109. doi: 10.1038/s41593-019-0423-2. [DOI] [PubMed] [Google Scholar]
- 57.Mahul-Mellier AL, Burtscher J, Maharjan N, Weerens L, Croisier M, Kuttler F, et al. The process of Lewy body formation, rather than simply α-synuclein fibrillization, is one of the major drivers of neurodegeneration. Proc Natl Acad Sci U S A. 2020;117(9):4971–4982. doi: 10.1073/pnas.1913904117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jankovic J, Goodman I, Safirstein B, Marmon TK, Schenk DB, Koller M, et al. Safety and tolerability of multiple ascending doses of PRX002/RG7935, an anti–α-synuclein monoclonal antibody, in patients with Parkinson disease: A Randomized Clinical Trial. JAMA Neurol. 2018;75(10):1206–1214. doi: 10.1001/jamaneurol.2018.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Masliah E, Rockenstein E, Adame A, Alford M, Crews L, Hashimoto M, et al. Effects of alpha-synuclein immunization in a mouse model of Parkinson’s disease. Neuron. 2005;46(6):857–868. doi: 10.1016/j.neuron.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 60.Games D, Valera E, Spencer B, Rockenstein E, Mante M, Adame A, et al. Reducing C-terminal-truncated alpha-synuclein by immunotherapy attenuates neurodegeneration and propagation in Parkinson’s disease-like models. J Neurosci. 2014;34(28):9441–9454. doi: 10.1523/JNEUROSCI.5314-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Masuda-Suzukake M, Nonaka T, Hosokawa M, Kubo M, Shimozawa A, Akiyama H, et al. Pathological alpha-synuclein propagates through neural networks. Acta Neuropathol Comm. 2014;2(1):88. doi: 10.1186/s40478-014-0088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu Q, Takano H, Riddle DM, Trojanowski JQ, Coulter DA, Lee VMY. α-Synuclein (αSyn) preformed fibrils induce endogenous αSyn aggregation, compromise synaptic activity and enhance synapse loss in cultured excitatory hippocampal neurons. J Neurosci. 2019;39(26):5080–5094. doi: 10.1523/JNEUROSCI.0060-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sacino AN, Brooks M, McGarvey NH, McKinney AB, Thomas MA, Levites Y, et al. Induction of CNS α-synuclein pathology by fibrillar and non-amyloidogenic recombinant α-synuclein. Acta Neuropathol Comm. 2013;1(1):38. doi: 10.1186/2051-5960-1-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Musgrove RE, Helwig M, Bae EJ, Aboutalebi H, Lee SJ, Ulusoy A, et al. Oxidative stress in vagal neurons promotes parkinsonian pathology and intercellular α-synuclein transfer. J Clin Invest. 2019;129(9):3738–3753. doi: 10.1172/JCI127330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Crabbé M, Van der Perren A, Kounelis S, Lavreys T, Bormans G, Baekelandt V, et al. Temporal changes in neuroinflammation and brain glucose metabolism in a rat model of viral vector-induced α-synucleinopathy. Exp Neurol. 2019;320:112964. doi: 10.1016/j.expneurol.2019.112964. [DOI] [PubMed] [Google Scholar]
- 66.Volpicelli-Daley LA, Luk KC, Lee VMY. Addition of exogenous α-synuclein preformed fibrils to primary neuronal cultures to seed recruitment of endogenous α-synuclein to Lewy body and Lewy neurite-like aggregates. Nat Protoc. 2014;9(9):2135–2146. doi: 10.1038/nprot.2014.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Recasens A, Dehay B, Bové J, Carballo-Carbajal I, Dovero S, Pérez-Villalba A, et al. Lewy body extracts from Parkinson disease brains trigger α-synuclein pathology and neurodegeneration in mice and monkeys. Ann Neurol. 2014;75(3):351–362. doi: 10.1002/ana.24066. [DOI] [PubMed] [Google Scholar]
- 68.Mougenot AL, Nicot S, Bencsik A, Morignat E, Verchère J, Lakhdar L, et al. Prion-like acceleration of a synucleinopathy in a transgenic mouse model. Neurobiol Aging. 2012;33(9):2225–2228. doi: 10.1016/j.neurobiolaging.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 69.Brundin P, Melki R. Prying into the prion hypothesis for Parkinson’s disease. J Neurosci. 2017;37(41):9808–9818. doi: 10.1523/JNEUROSCI.1788-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Singer W, Schmeichel AM, Shahnawaz M, Schmelzer JD, Boeve BF, Sletten DM, et al. Alpha-synuclein oligomers and neurofilament light chain in spinal fluid differentiate multiple system atrophy from lewy body synucleinopathies. Ann Neurol. 2020. 10.1002/ana.25824. [DOI] [PMC free article] [PubMed]
- 71.Tsukita K, Sakamaki-Tsukita H, Tanaka K, Suenaga T, Takahashi R. Value of in vivo α-synuclein deposits in Parkinson’s disease: A systematic review and meta-analysis. Mov Disord. 2019;34(10):1452–1463. doi: 10.1002/mds.27794. [DOI] [PubMed] [Google Scholar]
- 72.Obeso JA, Stamelou M, Goetz CG, Poewe W, Lang AE, Weintraub D, et al. Past, present, and future of Parkinson’s disease: A special essay on the 200th Anniversary of the Shaking Palsy. Mov Disord. 2017;32(9):1264–1310. doi: 10.1002/mds.27115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zarow C, Lyness SA, Mortimer JA, Chui HC. Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch Neurol. 2003;60(3):337–341. doi: 10.1001/archneur.60.3.337. [DOI] [PubMed] [Google Scholar]
- 74.Espay AJ, LeWitt PA, Kaufmann H. Norepinephrine deficiency in Parkinson’s disease: the case for noradrenergic enhancement. Mov Disord. 2014;29(14):1710–1719. doi: 10.1002/mds.26048. [DOI] [PubMed] [Google Scholar]
- 75.Giasson BI, Duda JE, Murray IV, Chen Q, Souza JM, Hurtig HI, et al. Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science. 2000;290(5493):985–989. doi: 10.1126/science.290.5493.985. [DOI] [PubMed] [Google Scholar]
- 76.Burbulla LF, Song P, Mazzulli JR, Zampese E, Wong YC, Jeon S, et al. Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson’s disease. Science. 2017;357(6357):1255–1261. doi: 10.1126/science.aam9080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sherer TB, Kim JH, Betarbet R, Greenamyre JT. Subcutaneous rotenone exposure causes highly selective dopaminergic degeneration and alpha-synuclein aggregation. Exp Neurol. 2003;179(1):9–16. doi: 10.1006/exnr.2002.8072. [DOI] [PubMed] [Google Scholar]
- 78.Klingelhoefer L, Reichmann H. Pathogenesis of Parkinson disease--the gut-brain axis and environmental factors. Nature. 2015;11(11):625–636. doi: 10.1038/nrneurol.2015.197. [DOI] [PubMed] [Google Scholar]
- 79.Mahlknecht P, Gasperi A, Djamshidian A, Kiechl S, Stockner H, Willeit P, et al. Performance of the Movement Disorders Society criteria for prodromal Parkinson’s disease: A population-based 10-year study. Mov Disord. 2018;33(3):405–413. doi: 10.1002/mds.27281. [DOI] [PubMed] [Google Scholar]
- 80.Butler B, Sambo D, Khoshbouei H. Alpha-synuclein modulates dopamine neurotransmission. J Chem Neuroanat. 2017;83–84:41–49. doi: 10.1016/j.jchemneu.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Luk KC, Kehm V, Carroll J, Zhang B, O’Brien P, Trojanowski JQ, et al. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science. 2012;338(6109):949–953. doi: 10.1126/science.1227157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Matsui H, Kenmochi N, Namikawa K. Age- and α-synuclein-dependent degeneration of dopamine and noradrenaline neurons in the annual killifish Nothobranchius furzeri. Cell Rep. 2019;26(7):1727–1733.e6. doi: 10.1016/j.celrep.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 83.Jellinger KA. Neuropathology of sporadic Parkinson’s disease: evaluation and changes of concepts. Mov Disord. 2012;27(1):8–30. doi: 10.1002/mds.23795. [DOI] [PubMed] [Google Scholar]
- 84.Surmeier DJ, Obeso JA, Halliday GM. Selective neuronal vulnerability in Parkinson disease. Nat Rev Neurosci. 2017;18(2):101–113. doi: 10.1038/nrn.2016.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sulzer D, Surmeier DJ. Neuronal vulnerability, pathogenesis, and Parkinson’s disease. Mov Disord. 2013;28(6):715–724. doi: 10.1002/mds.25187. [DOI] [PubMed] [Google Scholar]
- 86.Liss B, Haeckel O, Wildmann J, Miki T, Seino S, Roeper J. K-ATP channels promote the differential degeneration of dopaminergic midbrain neurons. Nat Neurosci. 2005;8(12):1742–1751. doi: 10.1038/nn1570. [DOI] [PubMed] [Google Scholar]
- 87.Kordower JH, Olanow CW, Dodiya HB, Chu Y, Beach TG, Adler CH, et al. Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain. 2013;136(Pt 8):2419–2431. doi: 10.1093/brain/awt192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Albin RL, Young AB, Penney JB. The functional anatomy of basal ganglia disorders. Trends Neurosci. 1989;12(10):366–375. doi: 10.1016/0166-2236(89)90074-X. [DOI] [PubMed] [Google Scholar]
- 89.DeLong M, Wichmann T. Update on models of basal ganglia function and dysfunction. Parkinsonism Relat Disord. 2009;15:S237–S240. doi: 10.1016/S1353-8020(09)70822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wichmann T. Changing views of the pathophysiology of Parkinsonism. Mov Disord. 2019;34(8):1130–1143. doi: 10.1002/mds.27741. [DOI] [PubMed] [Google Scholar]
- 91.Hutchison WD. Neuronal oscillations in the basal ganglia and movement disorders: evidence from whole animal and human recordings. J Neurosci. 2004;24(42):9240–9243. doi: 10.1523/JNEUROSCI.3366-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mink JW. The basal ganglia and involuntary movements: impaired inhibition of competing motor patterns. Arch Neurol. 2003;60(10):1365–8. [DOI] [PubMed]
- 93.Volkmann J, Daniels C, Witt K. Neuropsychiatric effects of subthalamic neurostimulation in Parkinson disease. Nat Rev Neurol. 2010;6(9):487–498. doi: 10.1038/nrneurol.2010.111. [DOI] [PubMed] [Google Scholar]
- 94.Moll CKE, Engel AK. Phase matters: cancelling pathological tremor by adaptive deep brain stimulation. Brain. 2017;140(1):5–8. doi: 10.1093/brain/aww308. [DOI] [PubMed] [Google Scholar]
- 95.Holt AB, Kormann E, Gulberti A, Pötter Nerger M, McNamara CG, Cagnan H, et al. Phase-dependent suppression of beta oscillations in Parkinson’s disease patients. J Neurosci. 2019;39(6):1119–1134. doi: 10.1523/JNEUROSCI.1913-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ingham CA, Hood SH, Arbuthnott GW. Spine density on neostriatal neurones changes with 6-hydroxydopamine lesions and with age. Brain Res. 1989;503(2):334–338. doi: 10.1016/0006-8993(89)91686-7. [DOI] [PubMed] [Google Scholar]
- 97.Fieblinger T, Graves SM, Sebel LE, Alcacer C, Plotkin JL, Gertler TS, et al. Cell type-specific plasticity of striatal projection neurons in parkinsonism and L-DOPA-induced dyskinesia. Nat Commun. 2014;5(1):5316. doi: 10.1038/ncomms6316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Suarez LM, Alberquilla S, García-Montes JR, Moratalla R. Differential synaptic remodeling by dopamine in direct and indirect striatal projection neurons in Pitx3−/− mice, a genetic model of Parkinson’s disease. J Neurosci. 2018;38(15):3619–3630. doi: 10.1523/JNEUROSCI.3184-17.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stephens B, Mueller AJ, Shering AF, Hood SH, Taggart P, Arbuthnott GW, et al. Evidence of a breakdown of corticostriatal connections in Parkinson’s disease. Neuroscience. 2005;132(3):741–754. doi: 10.1016/j.neuroscience.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 100.Ali Z, Roque A, El-Mallakh RS. A unifying theory for the pathoetiologic mechanism of tardive dyskinesia. Med Hypotheses. 2020;140:109682. doi: 10.1016/j.mehy.2020.109682. [DOI] [PubMed] [Google Scholar]
- 101.Nutt JG, Carter JH, Van Houten L, Woodward WR. Short- and long-duration responses to levodopa during the first year of levodopa therapy. Ann Neurol. 1997;42(3):349–355. doi: 10.1002/ana.410420311. [DOI] [PubMed] [Google Scholar]
- 102.Stocchi F, Vacca L, Berardelli A, De Pandis F, Ruggieri S. Long-duration effect and the postsynaptic compartment: study using a dopamine agonist with a short half-life. Mov Disord. 2001;16(2):301–305. doi: 10.1002/mds.1070. [DOI] [PubMed] [Google Scholar]
- 103.Fahn S, Oakes D, Shoulson I, Kieburtz K, Rudolph A, Lang A, et al. Levodopa and the progression of Parkinson’s disease. New Eng J Med. 2004;351(24):2498–2508. doi: 10.1056/NEJMoa033447. [DOI] [PubMed] [Google Scholar]
- 104.Schultz W. Recent advances in understanding the role of phasic dopamine activity. F1000Res. 2019;8(1680):1680. doi: 10.12688/f1000research.19793.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Calabresi P, Ghiglieri V, Mazzocchetti P, Corbelli I, Picconi B. Levodopa-induced plasticity: a double-edged sword in Parkinson’s disease? Phil Trans R Soc B. 2015;370(1672):20140184. doi: 10.1098/rstb.2014.0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tyssowski KM, Letai KC, Rendall SD, Tan C, Nizhnik A, Kaeser PS, et al. Firing rate homeostasis can occur in the absence of neuronal activity-regulated transcription. J Neurosci. 2019;39(50):9885–99. [DOI] [PMC free article] [PubMed]
- 107.Tanimura A, Du Y, Kondapalli J, Wokosin DL, Surmeier DJ. Cholinergic interneurons amplify thalamostriatal excitation of striatal indirect pathway neurons in Parkinson’s disease models. Neuron. 2019;101(3):444–446. doi: 10.1016/j.neuron.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 108.Moehle MS, Conn PJ. Roles of the M4 acetylcholine receptor in the basal ganglia and the treatment of movement disorders. Mov Disord. 2019;34(8):1089–1099. doi: 10.1002/mds.27740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fernández-Dueñas V, Ferré S, Ciruela F. Adenosine A2A-dopamine D2 receptor heteromers operate striatal function: impact on Parkinson’s disease pharmacotherapeutics. Neural Regen Res. 2018;13(2):241–243. doi: 10.4103/1673-5374.226388. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data and materials used and mentioned in Figs. 2 and 3 are available from the corresponding author on reasonable request.