Abstract
AIM
To investigate the proportion and characteristic of emmetropia in schoolchildren aged 6-11, especially estimate the normal value of ocular biometric parameters of emmetropia.
METHODS
A population-based cross-sectional study was conducted on children aged 6-11y in Shenzhen. Totally, 2386 schoolchildren from two primary schools were involved. The axial length (AL) and the corneal radius of curvature (CRC) were measured by partial coherence laser interferometry. Noncycloplegic refraction and refractive astigmatism (RA) was measured using autorefraction. The axial length-to-corneal radius of curvature ratio (AL/CRC), corneal astigmatism (CA) and spherical equivalent refraction (SER) were calculated.
RESULTS
The proportion of emmetropia in elementary school students was 41.30%. This percentage decreased gradually from 6 to 11 years of age and decreased rapidly after 9 years of age. The mean and 95%CI of each parameter were provided for boys and girls aged 6 to 11 years of age with emmetropia according to each age group. The change trend of parameters of boys and girls are similar. After 7 years of age, the AL of non-emmetropia started to increase faster than that of emmetropia. The change trend of AL/CRC was the same as that of AL. The other parameters tend to be stable after 7 years of age.
CONCLUSION
The age of 7-9 is an important period for the changes of refractive state and ocular biometric parameters of primary school students, and it is a special focus period for children myopia prevention. The normal value and variation of ocular biometric parameters of emmetropia can provide the basis for the clinical judgment of whether or not children's ocular biometric parameters obtained by single measurement and changes obtained by multiple measurements are abnormal.
Keywords: axial length, corneal radius of curvature, myopia, emmetropia, children
INTRODUCTION
The prevalence of myopia has been increasing in recent decades, especially in East Asia. Myopia may cause poor vision or even permanent visual impairment, which may lead to inconvenience in life and limited employment opportunities. Therefore, myopia has become a research hotspot in recent years[1]. In a large number of myopia related studies, the axial length (AL), corneal radius of curvature (CRC) and objective noncycloplegic refraction have become commonly used research parameters due to their convenient detection and good repeatability[2]–[4]. In China, many single and multiple tests of AL, CRC, and objective noncycloplegic refraction have been performed. The Chinese government has tried to establish a refractive development profile for each child and adolescent by obtaining these data[5]. However, there is no research report on the distribution and variation of the AL and CRC of students of different ages, so the doctors cannot judge whether the single measurement results are abnormal, nor can judge whether the changes obtained by multiple measurement results are in the normal range. The doctors have an urgent need to study the distribution and variation of AL and CRC. Therefore, the researches carried out this prospective cross-sectional study. The study analyzed the distribution of AL, CRC, axial length-to-corneal radius of curvature ratio (AL/CRC), corneal astigmatism (CA), refractive astigmatism (RA) and the relationship between these parameters and age in emmetropic children. The research results will provide a clear indication for the clinical judgment of whether or not children's ocular biometric parameters obtained by single measurement and changes obtained by multiple measurements are abnormal.
SUBJECTS AND METHODS
Ethical Approval
The study adhered to the tenet of the Helsinki Declaration. Ethics Committee approval was obtained from the Seventh Affiliated Hospital of Sun Yat-sen University Ethics Committee. After explaining the purpose and procedure of the study to the parents in detail, the written informed consent was obtained.
Population
When conducting routine school vision screening in 2019 in Guangming District, Shenzhen, China, the study randomly selected two primary schools for detailed ocular biometric parameters, including uncorrected visual acuity, objective noncycloplegic refraction, AL, CRC. Because of the non-invasive nature of the examination, apart from 4 students who were absent due to illness and 7 students who had severe ocular diseases affecting vision other than refractive error, 2386 primary students participated in the examination. The study obtained complete data comprised of 2097 students aged 6-11, and then 866 emmetropias were selected by uncorrected visual acuity (UCVA) and spherical equivalent refraction (SER; UCVA≥5.0 and +0.50≥SER≥-0.50 D for the right eye).
Refraction and Biometric Parameters Measurements
During the examination, each student was assigned a unique QR code identification number. In a fixed room, the study first checked their uncorrected visual acuity, then their objective noncycloplegic refraction, and finally their AL and CRC.
The UCVA was measured using a standard logarithmic visual acuity chart (Yuehua Medical Devices Co., Ltd., Shantou, Guangdong, China)[6]. The inspection distance was 5 meters, and the brightness value was within the standard recommended value range[7]. The study first checked their right eye and then their left eye. Vision results were reported in decimal form. The objective noncycloplegic refraction was measured using desktop autorefractor (KR8900; Topcon Corp., Japan)[8]. The device automatically extracts the average spherical power, cylindrical power, and axis after three consecutive measurements.
The AL and CRC were measured using a noncontact optical biometry device (IOL Master 500; Carl Zeiss Meditec, Germany)[9]. The AL was measured continuously for 5 times, and the CRC 3 times. The result was obtained by averaging multiple measurement results with SNR>2. All measurements were checked under the natural pupil.
Definitions
Using the data of the autorefractor, the SER was calculated by adding together the spherical diopter and half of the cylindrical diopter. The AL was directly measured by the IOL Master. The CRC was the average of the longest and shortest CRC measured by IOL master. The AL/CRC was defined as the AL divided by the CRC[10]. The corneal K value was calculated by using the data of the corneal curvature radius and the formula K (D)=337.5/CRC (mm). The CA was calculated as CA=Kmin-Kmax, where Kmin represents the corneal K value with the lowest refractive index, and Kmax represents the corneal K value with the highest refractive index. The refraction astigmatism used the data of the cylindrical diopter measured by the autorefractor[11].
Statistical Analysis
The Kolmogorov-Smirnov test, Skewness and Kurtosis were used to evaluate the normality of the variables AL, CRC, AL/CRC, CA, and RA. The t-test was used to analyze the differences between eyes and between genders. Variance analysis was used to analyze the parameters of different age groups, and the mean value, standard deviation, and 95% confidence interval (CI) of each parameter were calculated. The association between ocular biometric parameters and age were determined using linear regression models. Two-sided P-values below 0.05 were statistically significant and analyzed using the statistical software package SPSS Statistics for Windows (version 24.0, IBM Corp., USA).
RESULTS
Among the 2386 enrolled students, 282 were out of the age range and 7 had no successful biometric measurements, leaving a total of 2097 students 6 to 11 years of age in the study. The mean age was 9.06±1.68y, with no statistically significant gender difference (P=0.114). All biometric parameters (AL, CRC, AL/CRC, CA, RA) of 2097 students were not normally distributed. Totally, 866 emmetropias were selected by UCVA and SER (UCVA≥5.0 for both eyes and +0.50 ≥SER≥-0.50 D for the right eye) from 2097 students. The AL of 866 emmetropias was normally distributed (P=0.131). After grouping by gender, the AL also obeyed normal distribution (P=0.200). After grouping the parameters by age, the AL of each age group was also normally distributed (P=0.200). According to the Kurtosis and Skewness values, other parameters of 866 emmetropias were generally accepted as the normal distribution. The students' characteristics and the prevalence of emmetropia are shown in Table 1. The proportion of emmetropia in elementary school students was 41.30%. The percentage of emmetropia decreased gradually as the age increases from 6 to 11 years of age, and decreased significantly after 9 years of age.
Table 1. The student characteristic and prevalence of emmetropia at each age.
| Characteristic | Total | Age (y) |
|||||
| 6 | 7 | 8 | 9 | 10 | 11 | ||
| Total students, n | 2097 | 360 | 352 | 367 | 297 | 352 | 369 |
| Boys | 1198 | 217 | 191 | 216 | 194 | 179 | 201 |
| Girls | 899 | 143 | 161 | 151 | 103 | 173 | 168 |
| Emmetropic students, n | 866 | 183 | 175 | 174 | 134 | 109 | 91 |
| Boys | 533 | 118 | 96 | 110 | 90 | 64 | 55 |
| Girls | 333 | 65 | 79 | 64 | 44 | 45 | 36 |
| Proportion ofemmetropia (%) | 41.30 | 50.8 | 49.7 | 47.4 | 45.1 | 31.0 | 24.7 |
Biometric parameters of the emmetropia as a function of gender and eye are shown in Table 2. In addition to RA, there were differences between genders in other parameters. The parameters of AL, CRC, and AL/CRC for boys were larger than those for girls in both eyes. The parameters of AL, CRC, AL/CRC showed no difference between the left and right eyes.
Table 2. Ocular biometric parameters of the emmetropic population as a function of gender and eye.
| Parameters (n=866) | Right eye | Left eye | Pa |
| AL (mm) | |||
| Total | 23.04±0.75 | 23.04±0.76 | 0.857 |
| Boys | 23.24±0.69 | 23.25±0.71 | 0.510 |
| Girls | 22.72±0.72 | 22.70±0.73 | 0.166 |
| Pb | <0.001 | <0.001 | |
| CRC (mm) | |||
| Total | 7.80±0.25 | 7.80±0.25 | 0.618 |
| Boys | 7.84±0.25 | 7.84±0.25 | 0.666 |
| Girls | 7.72±0.24 | 7.72±0.25 | 0.797 |
| Pb | <0.001 | <0.001 | |
| AL/CRC | |||
| Total | 2.96±0.06 | 2.96±0.07 | 0.762 |
| Boys | 2.96±0.06 | 2.96±0.07 | 0.397 |
| Girls | 2.94±0.06 | 2.94±0.07 | 0.396 |
| Pb | <0.001 | <0.001 | |
| CA (diopter) | |||
| Total | -1.02±0.55 | -1.08±0.59 | <0.001 |
| Boys | -0.96±0.53 | -1.01±0.57 | <0.001 |
| Girls | -1.11±0.55 | -1.20±0.61 | <0.001 |
| Pb | <0.001 | <0.001 | |
| RA (diopter) | |||
| Total | -0.27±0.37 | -0.33±0.47 | <0.001 |
| Boys | -0.26±0.37 | -0.32±0.45 | <0.001 |
| Girls | -0.29±0.37 | -0.33±0.49 | 0.06 |
| Pb | 0.209 | 0.735 |
AL: Axial length; CRC: Corneal radius of curvature; AL/CRC: Axial length-to-corneal radius of curvature ratio; CA: Corneal astigmatism; RA: Refractive astigmatism. Data are mean±standard deviation unless otherwise indicated. aBetween the right eye and left eye, P<0.05 was considered statistically significant. bBetween boys and girls, P<0.05 was considered statistically significant.
There was a high correlation between right and left eye parameters, the data for the right eyes were used in the following analysis. Ocular biometric parameters of the emmetropia as a function of gender and age are shown in Table 3. Statistically significant differences in AL were found between boys and girls of all ages between 6 and 11 years of age, with boys having longer AL than girls of all ages. A growing trend of mean AL was observed as age increases in boys and girls. Statistically significant differences in CRC were not found between boys and girls who are 10 and 11 years of age, but gender differences were significant in other age groups. Boys had longer CRC than girls.
Table 3. The emmetropic parameters of the right eye as a function of gender and age.
| Parameters (n=866) | Age (y) |
Pa | |||||
| 6 | 7 | 8 | 9 | 10 | 11 | ||
| AL (mm) | |||||||
| Total | 22.71 ±0.74 | 22.88±0.68 | 23.02±0.70 | 23.25±0.69 | 23.24±0.71 | 23.49±0.70 | <0.001 |
| Boys | 22.92±0.70 | 23.09±0.63 | 23.24±0.57 | 23.41±0.68 | 23.44±0.65 | 23.69±0.67 | <0.001 |
| Girls | 22.32±0.66 | 22.62±0.66 | 22.65±0.74 | 22.94±0.59 | 22.96±0.69 | 23.18±0.64 | <0.001 |
| Pb | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| CRC (mm) | |||||||
| Total | 7.74±0.27 | 7.80±0.23 | 7.80±0.23 | 7.82±0.26 | 7.80±0.27 | 7.86±0.26 | 0.013 |
| Boys | 7.79±0.27 | 7.86±0.22 | 7.87±0.21 | 7.86±0.27 | 7.83±0.26 | 7.88±0.27 | 0.112 |
| Girls | 7.66±0.24 | 7.73±0.23 | 7.69±0.24 | 7.76±0.22 | 7.75±0.28 | 7.82±0.25 | 0.007 |
| Pb | 0.002 | <0.001 | <0.001 | 0.035 | 0.121 | 0.237 | |
| AL/CRC | |||||||
| Total | 2.93±0.06 | 2.93±0.06 | 2.95±0.05 | 2.97±0.06 | 2.98±0.06 | 2.99±0.07 | <0.001 |
| Boys | 2.94±0.06 | 2.94±0.05 | 2.95±0.05 | 2.98±0.06 | 2.99±0.06 | 3.01±0.07 | <0.001 |
| Girls | 2.91±0.06 | 2.93±0.06 | 2.94±0.05 | 2.96±0.06 | 2.96±0.06 | 2.97±0.05 | <0.001 |
| Pb | 0.002 | 0.21 | 0.234 | 0.046 | 0.011 | 0.003 | |
| CA (diopter) | |||||||
| Total | -0.74±0.73 | -1.11±0.48 | -1.10±0.44 | -1.06±0.49 | -1.07±0.43 | -1.10±0.44 | <0.001 |
| Boys | -0.69±0.70 | -1.03±0.47 | -1.04±0.43 | -1.02±0.49 | -1.02±0.45 | -1.05±0.41 | <0.001 |
| Girls | -0.82±0.78 | -1.21±0.49 | -1.19±0.46 | -1.15±0.47 | -1.14±0.39 | -1.19±0.47 | <0.001 |
| Pb | 0.248 | 0.013 | 0.029 | 0.157 | 0.142 | 0.126 | |
| RA (diopter) | |||||||
| Total | -0.39±0.42 | -0.27±0.36 | -0.22±0.36 | -0.22±0.34 | -0.22±0.29 | -0.27±0.34 | <0.001 |
| Boys | 0.20±0.36 | 0.07±0.35 | 0.07±0.32 | 0.08±0.34 | 0.07±0.26 | 0.00±0.29 | 0.002 |
| Girls | -0.44±0.44 | -0.34±0.33 | -0.25±0.37 | -0.20±0.35 | -0.18±0.26 | -0.25±0.33 | <0.001 |
| Pb | 0.243 | 0.042 | 0.327 | 0.647 | 0.252 | 0.572 | |
AL: Axial length; CRC: Corneal radius of curvature; AL/CRC: Axial length-to-corneal radius of curvature ratio; CA: Corneal astigmatism; RA: Refractive astigmatism. Data are mean±standard deviation unless otherwise indicated. aAcross different age groups, P<0.05 was considered statistically significant. bBetween boys and girls, P<0.05 was considered statistically significant.
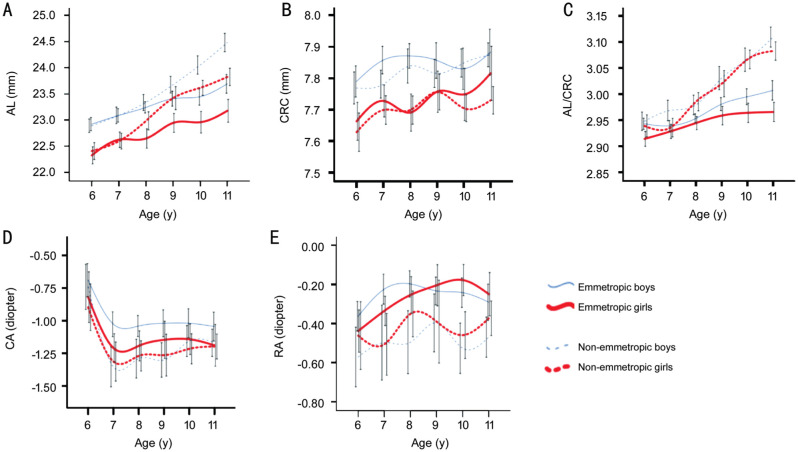
The 95%CI of the mean ocular biometric parameters of emmetropia by gender and age is shown in Table 4. Figure 1 showing the change of right eye biometric parameters of ametropia and emmetropia from 6 to 11 years of age. We can see that the changing trends of the parameters of boys and girls are the same. The AL increased from 6 to 11 years of age, the separation between emmetropia and non-emmetropia began after 7 years of age, and non-emmetropia changes faster than emmetropia after 7 years of age. AL continued to increase by about 0.156 mm-0.174 mm per year in emmetropia (linear regression equation: ALBoys=0.156×age+21.884; ALGirls=0.174×age+21.206). The trend of AL/CRC was the same as that of AL. AL/CRC of emmetropia increased by about 0.015 mm-0.012 mm per year (linear regression equation: ALBoys=0.015×age+2.836; ALGirls=0.012×age+2.835). The other parameters (CRC, CA, and RA) tended to stabilize after the age of 7.
Table 4. Right eye parameters in emmetropia.
| Parameters (n=866) | Age (y) |
|||||
| 6 | 7 | 8 | 9 | 10 | 11 | |
| AL (mm) | ||||||
| Total | 22.60-22.82 | 22.77-22.98 | 22.91-23.13 | 23.14-23.37 | 23.11-23.38 | 23.34-23.63 |
| Boys | 22.79-23.05 | 22.96-23.22 | 23.13-23.35 | 23.26-23.55 | 23.28-23.61 | 23.51-23.87 |
| Girls | 22.16-22.49 | 22.47-22.77 | 22.46-22.83 | 22.76-23.12 | 22.75-23.16 | 22.96-23.39 |
| CRC (mm) | ||||||
| Total | 7.71-7.78 | 7.76-7.83 | 7.77-7.84 | 7.78-7.88 | 7.77-7.85 | 7.80-7.91 |
| Boys | 7.74-7.84 | 7.81-7.90 | 7.83-7.91 | 7.80-7.91 | 7.76-7.90 | 7.81-7.96 |
| Girls | 7.60-7.72 | 7.68-7.78 | 7.63-7.75 | 7.69-7.82 | 7.70-7.89 | 7.67-7.83 |
| AL/CRC | ||||||
| Total | 2.92-2.94 | 2.93-2.94 | 2.94-2.96 | 2.96-2.98 | 2.97-2.99 | 2.97-3.00 |
| Boys | 2.93-2.95 | 2.93-2.95 | 2.94-2.96 | 2.97-2.99 | 2.98-3.01 | 2.99-3.03 |
| Girls | 2.90-2.93 | 2.91-2.94 | 2.93-2.96 | 2.94-2.98 | 2.95-2.98 | 2.95-2.98 |
| CA (diopter) | ||||||
| Total | -0.84 to -0.63 | -1.18 to -1.04 | -1.16 to -1.03 | -1.15 to -0.98 | -1.15 to -0.99 | -1.19 to -1.01 |
| Boys | -0.82 to -0.56 | -1.12 to -0.93 | -1.12 to -0.96 | -1.12 to -0.92 | -1.13 to -0.91 | -1.16 to -0.93 |
| Girls | -1.01 to -0.62 | -1.32 to -1.10 | -1.31 to -1.08 | -1.29 to -1.00 | -1.26 to -1.03 | -1.35 to -1.03 |
| RA (diopter) | ||||||
| Total | 0.15 to -0.26 | 0.02 to -0.13 | 0.00-0.09 | -0.01 to -0.11 | -0.02 to -0.08 | -0.07 to -0.05 |
| Boys | 0.14-0.27 | -0.00-0.14 | 0.01-0.13 | 0.01-0.15 | 0.00-0.13 | -0.08-0.07 |
| Girls | -0.54 to -0.33 | -0.41 to -0.26 | -0.35 to -0.16 | -0.31 to -0.10 | -0.26-0.10 | -0.36-0.12 |
AL: Axial length; CRC: Corneal radius of curvature; AL/CRC: Axial length-to-corneal radius of curvature ratio; CA: Corneal astigmatism; RA: Refractive astigmatism. Data are 95%CI unless otherwise indicated.
Figure 1. The change of right eye biometric parameters of ametropia and emmetropia from 6 to 11 years of age.
A: AL; B: CRC; C: AL/CRC; D: CA; E: RA. The 95%CIs are included in each graph.
DISCUSSION
This is the first study to report the distribution and variation of ocular biometric parameters among Chinese emmetropic children ranging from 6 to 11 years of age. The AL of 866 emmetropias was normally distributed. There were significant differences between genders in all parameters except RA, and the measurements obtained from boys were in general larger than those of girls. AL, CRC, and AL/CRC showed no difference between the left and right eyes except for CA, RA. Boys and girls had similar variations trend in all parameters. The AL and AL/CRC increased from 6 to 11 years of age, and the growth rate of non-emmetropia was faster than emmetropia after 7 years of age. The AL of boys/girls continued to increase by about 0.156-0.174 mm per year in emmetropia. The other parameters (CRC, CA, and RA) tended to stabilize after the age of 7. The proportion of emmetropia in elementary school students was 41.30%. The percentage of emmetropia decreased gradually with increasing age and decreased significantly after 9 years of age. Therefore, the age of 7-9 was an important stage for separating the emmetropia and non-emmetropia. AL and CRC increased with age and boys had higher measurements than girls, which may be related to the physical growth of children[12]–[13], and the developmental differences between boys and girls[14]. Considering the increase of AL/CRC with age in emmetropia, the researches should ignore the physiological increase of AL/CRC when judging the progression of myopia. Some research results also confirmed that AL/CRC was not useful in determining the magnitude of myopia or monitoring progression[15]. CA approached approximately -1.00 D after the age of 7, and RA approached zero with increasing age, which may be related to the perfect development of refractive growth in the human eye.
Evolution has produced the emmetropia mechanism, which makes the best match between AL and the optical system. The growth of eyes is affected by time, light, regulation, and close working. Most eyes are emmetropia at about 6 years old[16]. In some studies, the AL was divided by age[17], but it was not divided by SER at the same time, so the obtained AL development may not be accurate. Choosing the parameters obtained from emmetropia can help us to better understand the growth and development of the eye itself, but there are few studies on emmetropia at present. Dogan et al[18] conducted a study of 50 children aged 6-16 with emmetropia and found that among children aged 6-10, AL was 23.13±0.55 mm and K was 42.59±6.06 D. Li et al[19] studied 318 7-year-old children with emmetropia and found that 7-year-old children with emmetropia had AL of 23.23±0.62 mm and CRC of 7.78±0.25 mm, of which boys' AL was 23.39±0.60 mm and CR was 7.83±0.24 mm, girl's AL was 23.00±0.60 mm, CRC was 7.71±0.24 mm. It was found that the AL and CRC of boys were higher than that of girls. Atchison et al[20] studied a total of 106 emmetropias aged 20-70y, with males having AL of 23.79±0.55 mm and CRC of 7.87±0.20 mm and females having AL of 23.17±0.77 mm and CRC of 7.72±0.25 mm. It was found that the AL of this age group increased by 0.0113 mm per year without a significant increase in the CRC[20]. Tideman et al[21] studied 1926 9-year-old children with emmetropia and found that 9-year-old children with emmetropia had AL of 23.08±0.67 mm (95%CI: 22.02-24.23), CRC of 7.79±0.25 mm (95%CI: 7.39-8.22), and AL/CRC of 2.96±0.06 (95%CI: 2.87-3.06). Most of these results were similar to ours, but there were also slight differences, which may be due to the sample size, age and race selection.
Our criteria for emmetropia selection were UCVA≥5.0 and +0.50≥SER≥-0.50 D. Many researchers have made comparative studies of cycloplegic autorefraction and noncycloplegic autorefraction. Choong et al[22] found that under the condition of noncycloplegic autorefraction, the negative degree of the autorefractor would be overcorrected, leading to overdiagnosis of myopia. Fotouhi et al[23] found that noncycloplegic autorefraction overestimated the degree of myopia and underestimated the degree of hyperopia. Lai et al[24] combined UCVA with noncycloplegic autorefraction, which improved the specificity of predicting ametropia without reducing the sensitivity, and the symmetry of both eyes can increase the accuracy. Ma et al[25] found that when UCVA was combined with noncycloplegic autorefraction, UCVA≤20/20, SER≤-0.75 D, and the sensitivity and specificity for judging myopia were 84.4% and 90.5%. Sankaridurg et al[26] found that the accuracy of judging emmetropia using only the SE (-0.75 to +0.75 D) of noncycloplegic autorefraction was 78%, and the accuracy was adjusted to 82.3% after adjusting for age and UCVA, and using other SER cutoffs may change the prediction of the model value. Based on this, the study adjusted the cutoff value to -0.50≤SER≤+0.50 D and introduced UCVA≥=5.0 for both eyes, which greatly improved the accuracy of our prediction of emmetropia and increased the reliability of our results.
Our data confirmed that there were significant differences in AL and CRC for different genders and that AL and CRC in boys were larger than those in girls, which was consistent with some previous reports[27]–[31]. The boy's AL was about 0.5 mm larger than the girl's, and the boy's CRC is about 0.1 mm larger than the girl's. From the perspective of age change, the trend of parameter change in boys and girls was generally similar, and the AL continued to increase with age, which was also consistent with some previous reports[32]–[34]. The researches speculate that with the increase of age, the increase of CRC before the age of 7 may compensate for the increase of AL to a certain extent and play a role in maintaining emmetropia. Previous studies also reported that corneal flattening seemed to compensate for the increase of AL[35]–[37]. After the age of 7, AL was increasing while CRC was stable but not increasing. It was speculated that the lens may play an important role in maintaining the emmetropia, which was also confirmed by some research results[38]. Moreover, the development of the lens may be an important reason for myopia, the role and mechanism of the lens in refractive development will be a hot spot in myopia research[39]–[40].
The limitation of this study is that the standard for selecting the emmetropia is SER of noncycloplegic optometry, but the accuracy of emmetropia prediction is greatly improved by increasing UCVA≥5.0 and adjusting SER cutoff value (-0.50 to +0.50 D). In addition, the age of the study population is 6-11 years of age. If the population of 12-18 years of age can be included in the future, it will better reflect the distribution of biological parameters of adolescents with emmetropia and the law of change with age. Third, the accurate evaluation of the longitudinal age change was not possible because this was a cross-sectional study. Despite these limitations, the researches believe that our study provides a valuable reference for the clinical judgment of the normality of ocular biometric parameters of Chinese schoolchildren aged 6-11y.
In conclusion, the age of 7-9 is an important period for the changes of refractive state and ocular biometric parameters of primary school students, and it is a special focus period for children myopia prevention. The normal value and variation of ocular biometric parameters of emmetropia can provide the basis for the clinical judgment of whether or not children's ocular biometric parameters obtained by single measurement and changes obtained by multiple measurements are abnormal.
Acknowledgments
Authors' contributions: Jiang XM and Wu JS had full access to all of the data in the study and together with all co-authors take responsibility for the integrity of the data and the accuracy of the data analysis. Jiang XM and Wu JS designed the study, analysed the data, and drafted and revised the manuscript. Lu YY, Han X and Tan Q collected and managed the data. All authors reviewed and approved the manuscript.
Foundation: Supported by the National Natural Science Foundation of China for Youth (No.81500755).
Conflicts of Interest: Jiang XM, None; Lu YY, None; Han X, None; Tan Q, None; Wu JS, None.
REFERENCES
- 1.Dolgin E. The myopia boom. Nature. 2015;519(7543):276–278. doi: 10.1038/519276a. [DOI] [PubMed] [Google Scholar]
- 2.He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, Smith W, Rose K, Morgan IG. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 3.Zhao KK, Yang Y, Wang H, Li L, Wang ZY, Jiang F, Qu JF. Axial length/corneal radius of curvature ratio and refractive development evaluation in 3- to 4-year-old children: the Shanghai Pudong Eye Study. Int J Ophthalmol. 2019;12(6):1021–1026. doi: 10.18240/ijo.2019.06.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yotsukura E, Torii H, Inokuchi M, Tokumura M, Uchino M, Nakamura K, Hyodo M, Mori K, Jiang XY, Ikeda SI, Kondo S, Negishi K, Kurihara T, Tsubota K. Current prevalence of myopia and association of myopia with environmental factors among schoolchildren in Japan. JAMA Ophthalmol. 2019;137(11):1233–1239. doi: 10.1001/jamaophthalmol.2019.3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu RY, Qu XM. Setting the individual file of ocular refractive development of children is the primary procedure in the prevention of myopia. Zhonghua Yan Ke Za Zhi. 2009;45(7):577–579. [PubMed] [Google Scholar]
- 6.Wang F, Xiao L, Meng X, Wang L, Wang D. Development of corneal astigmatism (CA) according to axial length/corneal radius (AL/CR) ratio in a one-year follow-up of children in Beijing, China. J Ophthalmol. 2018;2018:4209236. doi: 10.1155/2018/4209236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lempert P. Standardized measurements of visual acuity for clinical research. Ophthalmology. 1996;103(7):994–995. doi: 10.1016/s0161-6420(96)30551-4. [DOI] [PubMed] [Google Scholar]
- 8.Shi XY, Ke YF, Jin N, Zhang HM, Wei RH, Li XR. The prevalence of vision impairment and refractive error in 3654 first year students at Tianjin Medical University. Int J Ophthalmol. 2018;11(10):1698–1703. doi: 10.18240/ijo.2018.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.He M, Kong X, Chen Q, Zeng Y, Huang Y, Zhang J, Morgan IG, Meltzer ME, Jin L, Congdon N. Two-year changes in refractive error and related biometric factors in an adult Chinese population. JAMA Ophthalmol. 2014;132(8):978–984. doi: 10.1001/jamaophthalmol.2014.1011. [DOI] [PubMed] [Google Scholar]
- 10.Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, Meng M, Jonas JB. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120(2):277–283. doi: 10.1016/j.ophtha.2012.07.086. [DOI] [PubMed] [Google Scholar]
- 11.Liu YC, Chou P, Wojciechowski R, Lin PY, Liu CJ, Chen SJ, Liu JH, Hsu WM, Cheng CY. Power vector analysis of refractive, corneal, and internal astigmatism in an elderly Chinese population: the Shihpai Eye Study. Invest Ophthalmol Vis Sci. 2011;52(13):9651–9657. doi: 10.1167/iovs.11-7641. [DOI] [PubMed] [Google Scholar]
- 12.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 13.de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137(1):144–148. doi: 10.1093/jn/137.1.144. [DOI] [PubMed] [Google Scholar]
- 14.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jong M, Sankaridurg P, Naduvilath TJ, Li W, He M. The relationship between progression in axial length/corneal radius of curvature ratio and spherical equivalent refractive error in myopia. Optom Vis Sci. 2018;95(10):921–929. doi: 10.1097/OPX.0000000000001281. [DOI] [PubMed] [Google Scholar]
- 16.Collins MJ. Myopia and emmetropisation. Clin Exp Optom. 2017;100(2):105–106. doi: 10.1111/cxo.12531. [DOI] [PubMed] [Google Scholar]
- 17.Bach A, Villegas VM, Gold AS, Shi W, Murray TG. Axial length development in children. Int J Ophthalmol. 2019;12(5):815–819. doi: 10.18240/ijo.2019.05.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dogan M, Elgin U, Sen E, Tekin K, Yilmazbas P. Comparison of anterior segment parameters and axial lengths of myopic, emmetropic, and hyperopic children. Int Ophthalmol. 2019;39(2):335–340. doi: 10.1007/s10792-017-0816-8. [DOI] [PubMed] [Google Scholar]
- 19.Li SM, Wang N, Zhou Y, Li SY, Kang MT, Liu LR, Li H, Sun YY, Meng B, Zhan SY, Atchison DA. Paraxial schematic eye models for 7- and 14-year-old Chinese children. Invest Ophthalmol Vis Sci. 2015;56(6):3577–3583. doi: 10.1167/iovs.15-16428. [DOI] [PubMed] [Google Scholar]
- 20.Atchison DA, Markwell EL, Kasthurirangan S, Pope JM, Smith G, Swann PG. Age-related changes in optical and biometric characteristics of emmetropic eyes. J Vis. 2008;8(4):29.1–29.20. doi: 10.1167/8.4.29. [DOI] [PubMed] [Google Scholar]
- 21.Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, Klaver CCW. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301–309. doi: 10.1111/aos.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol. 2006;142(1):68–74. doi: 10.1016/j.ajo.2006.01.084. [DOI] [PubMed] [Google Scholar]
- 23.Fotouhi A, Morgan IG, Iribarren R, Khabazkhoob M, Hashemi H. Validity of noncycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol. 2012;90(4):380–386. doi: 10.1111/j.1755-3768.2010.01983.x. [DOI] [PubMed] [Google Scholar]
- 24.Lai YH, Tseng HY, Hsu HT, Chang SJ, Wang HZ. Uncorrected visual acuity and noncycloplegic autorefraction predict significant refractive errors in Taiwanese preschool children. Ophthalmology. 2013;120(2):271–276. doi: 10.1016/j.ophtha.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 25.Ma Y, He X, Zou H, Lu L, Qu X, Zhu J. Myopia screening: combining visual acuity and noncycloplegic autorefraction. Optom Vis Sci. 2013;90(12):1479–1485. doi: 10.1097/OPX.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 26.Sankaridurg P, He X, Naduvilath T, Lv M, Ho A, Smith E, 3rd, Erickson P, Zhu J, Zou H, Xu X. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol. 2017;95(7):e633–e640. doi: 10.1111/aos.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin LL, Shih YF, Hsiao CK, Chen CJ, Lee LA, Hung PT. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Asso. 2001;100(10):684–691. [PubMed] [Google Scholar]
- 28.Zadnik K, Manny RE, Yu JA, Mitchell GL, Cotter SA, Quiralte JC, Shipp M, Friedman NE, Kleinstein R, Walker TW, Jones LA, Moeschberger ML, Mutti DO, Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci. 2003;80(3):226–236. doi: 10.1097/00006324-200303000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Ojaimi E, Rose KA, Morgan IG, Smith W, Martin FJ, Kifley A, Robaei D, Mitchell P. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46(8):2748–2754. doi: 10.1167/iovs.04-1324. [DOI] [PubMed] [Google Scholar]
- 30.Li SM, Iribarren R, Kang MT, Li H, Li SY, Liu LR, Sun YY, Meng B, Zhan SY, Rozema JJ, Wang N. Corrigendum: corneal power, anterior segment length and lens power in 14-year-old Chinese children: the Anyang childhood eye study. Sci Rep. 2016;6:26919. doi: 10.1038/srep26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang SK, Guo Y, Liao C, Chen Y, Su G, Zhang G, Zhang L, He M. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. 2018;136(9):1017–1024. doi: 10.1001/jamaophthalmol.2018.2658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. 1985;103(6):785–789. doi: 10.1001/archopht.1985.01050060045020. [DOI] [PubMed] [Google Scholar]
- 33.Zadnik K, Mutti DO, Mitchell GL, Jones LA, Burr D, Moeschberger ML. Normal eye growth in emmetropic schoolchildren. Optom Vis Sci. 2004;81(11):819–828. doi: 10.1097/01.opx.0000145028.53923.67. [DOI] [PubMed] [Google Scholar]
- 34.Selović A, Juresa V, Ivankovic D, Malcic D, Selović Bobonj G. Relationship between axial length of the emmetropic eye and the age, body height, and body weight of schoolchildren. Am J Hum Biol. 2005;17(2):173–177. doi: 10.1002/ajhb.20107. [DOI] [PubMed] [Google Scholar]
- 35.Grosvenor T, Goss DA. Role of the cornea in emmetropia and myopia. Optom Vis Sci. 1998;75(2):132–145. doi: 10.1097/00006324-199802000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, Moeschberger ML, Zadnik K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005;46(9):3074–3080. doi: 10.1167/iovs.04-1040. [DOI] [PubMed] [Google Scholar]
- 37.González Blanco F, Sanz Ferńandez JC, Muńoz Sanz MA. Axial length, corneal radius, and age of myopia onset. Optom Vis Sci. 2008;85(2):89–96. doi: 10.1097/OPX.0b013e3181622602. [DOI] [PubMed] [Google Scholar]
- 38.Hagen LA, Gilson SJ, Akram MN, Baraas RC. Emmetropia is maintained despite continued eye growth from 16 to 18 years of age. Invest Ophthalmol Vis Sci. 2019;60(13):4178–4186. doi: 10.1167/iovs.19-27289. [DOI] [PubMed] [Google Scholar]
- 39.Iribarren R, Morgan IG, Chan YH, Lin X, Saw SM. Changes in lens power in Singapore Chinese children during refractive development. Invest Ophthalmol Vis Sci. 2012;53(9):5124–5130. doi: 10.1167/iovs.12-9637. [DOI] [PubMed] [Google Scholar]
- 40.He JC. A model of the effect of lens development on refraction in schoolchildren. Optom Vis Sci. 2017;94(12):1129–1137. doi: 10.1097/OPX.0000000000001146. [DOI] [PubMed] [Google Scholar]