Abstract
AIM
To investigate the clinical efficacy and safety of femtosecond laser-assisted steepest-meridian clear corneal incisions for correcting preexisting corneal astigmatism performed at the time of cataract surgery.
METHODS
This prospective case series study comprised consecutive age-related cataract patients with corneal regular astigmatism (range: +0.75 to +2.50 D) who had femtosecond laser-assisted steepest-meridian clear corneal incisions (single or paired). Corneal astigmatism was performed with the Pentacam preoperatively and 3mo postoperatively. Total corneal astigmatism and steepest-meridian measured in the 3-mm central zone were used to guide the location, size and number of clear corneal incision. The vector analysis of astigmatic change was performed using the Alpins method.
RESULTS
Totally 138 eyes of 138 patients were included. The mean preoperative corneal astigmatism was 1.31±0.41 D, and was significantly reduced to 0.69±0.34 D (equivalent to difference vector) after surgery (P<0.01). The surgically-induced astigmatism was 1.02±0.54 D. The correction index (ratio of target induced astigmatism and surgically-induced astigmatism: 0.72±0.36) as well as the magnitude of error (difference between surgically-induced astigmatism and target induced astigmatism: -0.29±0.51) represented a slight under correction. For angle of error, the arithmetic mean was 1.11±13.70, indicating no significant systematic alignment errors.
CONCLUSION
Femtosecond-assisted steepest-meridian clear corneal incision is a fast, customizable, adjustable, precise, and safe technique for the reduction of low to moderate corneal astigmatism during cataract surgery.
Keywords: astigmatism, cataract surgery, femtosecond laser, clear corneal incision
INTRODUCTION
The main objective of modern cataract surgery is to achieve a good unaided vision. Postoperative astigmatism is the main cause of unsatisfactory visual acuity after cataract surgery[1]–[2]. About one-third to nearly half of eyes having cataract surgeries have corneal astigmatism greater than 1.0 diopter (D), and 8% to 13% have corneal astigmatism greater than 2.0 D[3]. Preexisting corneal astigmatism is one of the sources of corneal astigmatism after surgery, and another important source is surgically induced astigmatism (SIA). If SIA can neutralize preexisting corneal astigmatism, satisfactory visual quality may be achieved after surgery. Various techniques have been introduced, including on-axis opposite clear corneal incisions or single clear corneal incision, limbal relaxing incisions (LRIs), femtosecond laser-assisted arcuate keratotomy (FS-AK), toric intraocular lens (IOL) implantation, and refractive surgery after cataract surgery. On-axis incisions are a basic and useful method for correcting corneal astigmatism between 1.00 and 3.00 D[4]. The drawbacks of manual on-axis incisions include the variability in incision location, depth, and length.
Femtosecond laser-assisted cataract surgery is now increasing in popularity due to its ability to produce precise, reproducible incisions and capsulotomies. Femtosecond laser technology has increased the safety and efficacy of corneal astigmatism management at the time of or after cataract surgery, keratoplasty, and glaucoma surgery[5]. FS-AK is proven to be effective and safe in treating astigmatism during cataract surgery. To our knowledge, no study has evaluated the use of femtosecond-assisted steepest-meridian clear corneal incisions combined with cataract surgery in eyes with low to moderate corneal astigmatism. The central 3-mm zone of the cornea is crucial to our daytime vision. The effects of relaxing incisions placed in the steepest meridian of the 3-mm corneal zone are still unclear. The purpose of this study was to determine the efficacy and safety of single or paired steepest-meridian clear corneal incisions created with the femtosecond laser in the management of preexisting corneal astigmatism at the time of cataract surgery.
SUBJECTS AND METHODS
Ethical Approval
The study design was a prospective cohort study set in the Department of Ophthalmology, Affiliated Hospital of Nantong University and was conducted in accordance with the ethical norms and standards in the Declaration of Helsinki and written informed consent was obtained from all subjects. The study protocol was approved by the Ethical Committee of Affiliated Hospital of Nantong University.
Study Design and Participant
This study included age-related cataract patients who underwent femtosecond laser-assisted cataract surgery. All patients had low to moderate regular total corneal astigmatism (range: +0.75 to +2.50 D) based on Scheimpflug tomography (Pentacam, Oculus Optikgeräte GmbH). Ophthalmological assessment was performed before cataract operation. Eyes with corneal pathology, complicated cataracts, posterior segment pathology, or a systemic condition associated with abnormal wound healing (e.g., collagen vascular disease, diabetes mellitus) were excluded. For all visual and refractive assessment results, patients with ocular complications or target refractions other than emmetropia were excluded. The right eye was selected for analysis in cases who had operated on both eyes.
Surgical Technique
A color photograph of each patient's eye was taken by the VERION Image Guided System (Alcon Laboratories, Inc., Fort Worth, TX, USA) preoperatively. Femtosecond laser-assisted cataract surgery was performed using the Alcon LenSx laser system. Topical anesthesia was applied in all cataract surgery. All operations were performed by a single experienced surgeon (Guan HJ). Femtosecond laser-assisted capsulotomy, lens fragmentation and steepest-meridian clear cornea incisions were performed. Steepest-meridian clear corneal incision parameters were calculated based on a personal nomogram (Table 1) according to total corneal K readings of the central 3-mm zone obtained from Pentacam and the individual surgeon's SIA values. Single or paired clear corneal incisions were performed based on the total corneal astigmatism value (Figure 1). The Verion Digital Marker was used to facilitate incision alignment. A 1.0-mm side-port incision was made 110 degrees away clockwise to the main incision. All incisions were single-plane and penetrating. If there was a opposite clear corneal incision, it was opened to enhance the relaxing effect. At the end of surgery, the clear corneal wounds were closed by stromal hydration.
Table 1. Nomogram for femtosecond laser-assisted steepest-meridian clear corneal incisions.
| Preoperative corneal cylinder (D) | Clear corneal incision size and number |
|
| On the steep meridian of 3-mm zone | Opposite incision on the steep meridian of 3-mm zone | |
| 0.75-1.00 | 2.4 | - |
| 1.01-1.25 | 2.4 | 2.4 |
| 1.26-1.50 | 2.8 | 2.8 |
| 1.51-1.75 | 3.0 | 3.0 |
| 1.76-2.00 | 3.0 | 3.2 |
| 2.01-2.25 | 3.0 | 3.4 |
| 2.26-2.50 | 3.0 | 3.6 |
mm
Figure 1. Intraoperative photographs of femtosecond laser-assisted paired steepest-meridian clear corneal incisions.
A: Total corneal astigmatism measured by the Pentacam preoperatively; B: Preoperative planning of 2.4 mm paired steepest-meridian clear corneal incisions; C: Creating corneal incisions by laser emission; D: Paired 2.4 mm steepest-meridian clear corneal incisions performed by femtosecond laser.
After femtosecond laser treatment, the patient was transferred to another operation bed for the remaining phacoemulsification. Ultrasound phacoemulsification was performed using the Centurion Vision System (Alcon Laboratories, Inc., Fort Worth, TX, USA). A suitable sleeve was selected to accommodate the main incision in order to have better fluidics and anterior chamber stability. The Hoffer Q formula was used for eyes with an axial length shorter than 22.00 mm and the SRK/T for longer eyes. All patients were treated with topical tobramycin–dexamethasone eye drops (Alcon Laboratories, Inc.) 4 times daily during the first postoperative month.
Postoperative Follow-up
The follow-up visits were scheduled at 1 and 3mo after surgery. The uncorrected distant visual acuity (UDVA), best corrected distant visual acuity, and refraction were recorded. Corneal keratometry was performed using the Pentacam.
The astigmatic changes were measured using the Alpins method[6]. Target induced astigmatism (TIA) is defined as the intended induced astigmatic change (by magnitude and axis) by the surgery. SIA is the amount and axis of astigmatism change induced by the surgery actually. Difference vector (DV) is the change (by magnitude and axis) that would enable the initial surgery to achieve the original target on the second attempt. The DV is an absolute measure of success and is preferably 0. The astigmatic correction index (CI) is the ratio of SIA to TIA. The CI is preferably 1.0. It is greater than 1.0 if an overcorrection occurs and less than 1.0 if there is an undercorrection. The magnitude of error (ME) is the arithmetic difference between the magnitudes of the SIA and TIA, positive for overcorrections and negative for undercorrection. The angle of error (AE) is the angle described by the vectors of the achieved correction versus the intended correction. It is positive if the achieved correction is on an axis counter-clockwise (CCW) to its intended axis and negative if the achieved correction is clockwise (CW) to its intended axis. The index of success (IOS), calculated by dividing the DV by the TIA, is a relative measure of success and is preferably 0. The flattening effect (FE) is the amount of astigmatism reduction achieved by the effective proportion of the SIA at the intended meridian. The flattening index (FI), calculated by dividing the FE by the TIA, is preferably 1. Torque is the amount of astigmatic change induced by the SIA that have been ineffective in reducing astigmatism. The coupling ratio is described by the amount of flattening in the incised meridian divided by amount of steepening in the opposite meridian, is preferably 1. The coefficient of adjustment is defined as the inverse of correction index.
Distance visual acuity was measured using the Chinese standard logarithmic visual chart and converted to logarithm of minimal angle of resolution (logMAR) units or the Snellen fraction. Excel software (Microsoft Corp.) was used for data entry and graphic representation.
Statistical Analysis
SPSS (version 17.0, SPSS; Chicago, IL, USA) was used for statistical analysis. Differences with a P value less than 0.05 were considered statistically significant. Descriptive statistics were computed for each of the variables and comparative analyses included Student t tests.
RESULTS
One hundred and thirty-eight eyes from 138 patients were included in this prospective study, 116 eyes were used for further analysis of vision and refraction. Table 2 represents the patient baseline demographics and ocular variables. The mean amount of corneal astigmatism was 1.31±0.41 D before surgery and 0.69±0.34 D at 3mo after surgery, indicating astigmatism decreased by 47%. Postoperatively, 40% of eyes attained a corneal astigmatism of less than or equal to 0.50 D (Figure 2). No statistical difference was found between preoperative and postoperative corneal average K readings. There were no postoperative surgery-related adverse events such as wound leaking, or infections. There was a significant statistical difference among the preoperative and postoperative corneal cylinder (P<0.01).
Table 2. Patient demographics and ocular biometric parameters.
| Parameters | Mean±SD (range) |
| Age, y | 59.46±13.33 (24-81) |
| Male | 49% |
| Right | 53% |
| Corrected distant visual acuity, logMAR | 0.76±0.29 (0.1 to 1.3) |
| Anterior chamber depth, mm | 2.81±0.26 (1.54 to 3.89) |
| Axial length, mm | 24.25±2.58 (19.12 to 30.24) |
| Preoperative corneal keratometry, D | 42.49±1.69 (39.20 to 48.70) |
| Postoperative corneal keratometry, D | 42.29±1.47 (39.20 to 48.40) |
| Preoperative corneal cylinder, D | 1.31±0.41 (0.8 to 2.5) |
| Postoperative corneal cylinder, D | 0.69±0.34 (0.1 to 2.43) |
Figure 2. Preoperative and postoperative corneal astigmatism.
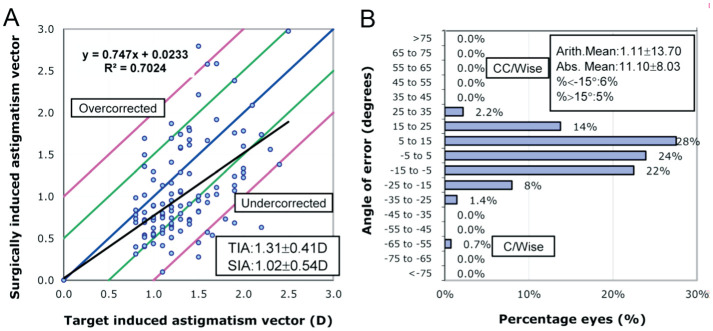
The results of Alpins vector analysis were recorded in Table 3. Figures 3A shows the the TIA versus SIA graph. The CI (ideal value 1.00) was 0.72±0.36, and the mean ME (ideal value 0.00) was -0.29±0.51, which means slight undercorrection. Thirty three eyes (23.9%) had an astigmatism correction of greater than 100%, 19 eyes (13.8%) had an astigmatism correction of greater than 120%. The arithmetic mean error of angle was 1.11±13.70, indicating a small amount of overall axis misalignment. However, the absolute mean angle of error was 11.10±8.03, suggesting a misalignment of 11 degrees at individual level. Figures 3B shows 82% of eyes had angular misalignment within ±15°. The flattening index was 0.73±0.35, representing a large proportion of SIA is effective to reduce astigmatism at the intended meridian. The index of success was 0.48±0.20 compared to the ideal value of 0, indicated a success rate of 52% in correction of astigmatism. The coupling ratio was 0.60±0.48.
Table 3. Results of vector analysis.
| Parameters | Mean±SD (range) |
| Target induced astigmatism, D | 1.31±0.41 (0.8 to 2.5) |
| Surgically induced astigmatism, D | 1.02±0.54 (0.10 to 2.98) |
| Difference vector, D | 0.69±0.34 (0.1 to 2.0) |
| Correction index | 0.72±0.36 (0.09 to 1.88) |
| Percentage of astigmatism corrected | 71.89±35.76 (9.09 to 188.18) |
| Coefficient of adjustment | 1.62±1.29 (0.53 to 10.99) |
| Index of success | 0.48±0.20 (0.11 to 1.29) |
| Magnitude of error | -0.29±0.51 (-1.98 to 1.30) |
| Absolute angle of error | 11.10±8.03 (0.0 to 61.26) |
| Arithmetic angle of error | 1.11±13.70 (-61.26 to 27.81) |
| Flattening effect | 0.93±0.53 (-0.17 to 2.97) |
| Flattening index | 0.73±0.35 (-0.14 to 1.86) |
| Torque effect | 0.05±0.43 (-1.25 to 1.40) |
| Percentage of astigmatism reduction an intended axis | 72.48±35.12 (-14.45 to 186.02) |
Figure 3. The TIA versus SIA and astigmatism angles of error graphs of patients treated with femtosecond laser-assisted steepest-meridian clear corneal incisions.
SIA: Surgically induced astigmatism; TIA: Target induced astigmatism; Abs.: Absolute; Arith.: Arithmetic; Ax: Axis; CC/Wise: Counterclockwise; C/Wise: Clockwise.
Standard graphs for refractive results of cataract surgery have been shown in Figure 4. Figure 4A shows the cumulative preoperative corrected distant visual acuity (CDVA) and postoperative UDVA. Best corrected visual acuity of all eyes reached or exceeded 20/40 after surgery, indicating that the technique was safe. Preoperative mean CDVA expressed in logMAR units improved from 0.62±0.38 to postoperative UCVA 0.16±0.13 (P<0.01). There was no requirement of refractive correction for about 48% patients to have clear distant vision (Figure 4B). Nearly 54% of patients attained a postoperative refractive cylinder of less than 0.50 D (Figure 4C). Figure 4D shows 93% of eyes achieved a postoperative spherical equivalent ±1.0 D.
Figure 4. Visual and refractive outcomes of patients treated with femtosecond laser-assisted steepest-meridian clear corneal incisions.
A: Cumulative percentages of postoperative Snellen visual acuity (UDVA and CDVA); B: Number of lines difference between UDVA and CDVA; C: Postoperative refractive astigmatism; D: Spherical equivalent refractive accuracy. CDVA: Corrected distance visual acuity; UDVA: Uncorrected distance visual acuity.
DISCUSSION
Lever and Dahan[7] first reported the paired opposite clear corneal incision technique. Although many studies have confirmed that the steepest meridian clear corneal incision can reduce the pre-existing astigmatism, the amount of astigmatism reduction varies according to the size and location of incisions and the number of incisions[8]–[11]. Femtosecond laser technology provided a more precise and reproducible surgical incision[12]. As an integral part of laser-assisted cataract surgery, incisions created by femtosecond laser are easily programmed and rapidly created without additional cost. To our knowledge, there is no experience of using femtosecond laser-assisted steepest-meridian clear corneal incisions to correct low to moderate corneal astigmatism. In our study, preoperative corneal astigmatism was reduced form 1.31±0.41 to 0.69±0.34 D after surgery, proving the effectiveness of steepest meridian clear corneal incision on astigmatism correction again. Moreover, 40% of eyes attained a corneal astigmatism of less than or equal to 0.50 D and 54% of eyes attained a postoperative refractive cylinder of less than 0.50 D in our study, which means that about half of the patients will not suffer from the loss of visual quality due to astigmatism.
The effect of correction of astigmatism is affected by various factors. One factor is the ability to accurately estimate corneal power. Pentacam-Scheimpflug showed the better precision (repeatability and reproducibility) than all other modalities[2]. In our study, the Pentacam device was used to measure preoperative and postoperative total corneal astigmatism. When the posterior corneal astigmatism was neglected, 16.6% of the patients had a difference of 0.50 D between the anterior corneal astigmatism and the total corneal astigmatism, while 3.8% of the patients had a difference of more than 10 degrees in the location of the steep meridian between the anterior corneal astigmatism and the total corneal astigmatism[13]. Therefore, total corneal astigmatism must be considered when correcting corneal astigmatism, measuring only the anterior corneal curvature can lead to inaccurate evaluation of the total corneal astigmatism. Another factor affecting astigmatism correction is the precise location of astigmatism axis, including the accurate measurement of astigmatism axis and accurate positioning axis in the eye. Tognetto et al[14] found that toric IOL axis rotation greater than 10 degrees affected the image quality seriously. Modern femto-cataract lasers coupling by the Verion preoperative assessment system can match the preoperative high-resolution image with the eye intraoperatively using scleral vessels, limbal vessels, and iris features, resulting in more accurate axis location and better correction results[15]. Corneal biomechanical properties such as corneal hysteresis and corneal resistance factor have been proven to be independent predictors of SIA[16], which means there will be individual differences even with the same surgical nomogram.
To achieve zero astigmatism is likely to be the ultimate goal of the surgical correction of astigmatism, but unfortunately. It seems impossible to reach such a level for all patients. Reducing astigmatism to a level that visual quality is acceptable to patients would be a better option. In the current study, 39.85% of eyes had postoperative corneal astigmatism of less than or equal to 0.5 D, as compared with only 33% in the FS-AK[17]. The coefficient of adjustment was 1.60, it means an increase of 60% in the magnitude of treatment nomogram may improve our research results. The axis misalignment will reduce the effect of astigmatism correction. No systematic misalignment was found since the mean arithmetic AE was close to 0 in our study. However, at individual level, we found the mean absolute value of AE was 11.1 degrees. This value is lower than that reported for manual limbal relaxing incisions[18] and femtosecond laser intrastromal astigmatic keratotomy[3]. The CI (0.72±0.36) in our findings was lower than the value (0.86) in Chan et al's study[17]. However, we observed a higher flattening effect (0.73 vs 0.53) and better index of success (0.48 vs 0.62) in our study. This can be explained by our lower absolute AE. A coupling effect must be considered when planning astigmatism surgery. The effects of incisions on astigmatism may have impact on the spherical equivalent refraction. If the coupling ratio is 1, the equivalent refraction will not change. When the coupling ratio is greater than 1 and less than 1, the results are, respectively, a hyperopic shift and a myopic shift. We found that the coupling ratio of femtosecond laser-assisted steepest-meridian clear corneal incisions was 0.6, similar to the value 0.56 of the intrastromal astigmatic keratotomy[3]. There is usually no need for torque in astigmatism correction surgery. The mean magnitude of torque vector was 0.05±0.43 D in our study, suggesting no significant overall off-steep meridian change.
The present study had several limitations. First, the follow-up time is only 3mo, and the effect of astigmatism correction may regress with time. Day and Stevens[19] showed that there were small but statistically significant regressions in SIA between 1 and 6mo postoperatively in patients performed femtosecond laser intrastromal astigmatic keratotomy. The age of the patient and the axis of the astigmatism were not taken into consideration in our nomograms. The effect of vertical clear corneal incision on astigmatism correction is different from that of horizontal clear corneal incision given their different distance from the corneal center. Longer follow-up and more patients are needed to confirm these early results and to improve treatment nomograms. Theoretically, two clear corneal incisions may increase the chance of intraocular infection; however, no corresponding complications have been reported in the literature so far, nor has this been observed in our study.
In summary, as part of femtosecond laser-assisted cataract surgery, femtosecond laser-assisted steepest-meridian clear corneal incisions can safely and effectively correct preoperative corneal astigmatism. Longer follow-up and further understanding of the factors influencing astigmatism correction efficacy will help further improve the surgical nomogram.
Acknowledgments
Conflicts of Interest: Chen W, None; Ji M, None; Wu J, None; Wang Y, None; Zhou J, None; Zhu RR, None; Lu H, None; Guan HJ, None.
REFERENCES
- 1.Anderson DF, Dhariwal M, Bouchet C, Keith MS. Global prevalence and economic and humanistic burden of astigmatism in cataract patients: a systematic literature review. Clin Ophthalmol. 2018;12:439–452. doi: 10.2147/OPTH.S146829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta PC, Caty JT. Astigmatism evaluation prior to cataract surgery. Curr Opin Ophthalmol. 2018;29(1):9–13. doi: 10.1097/ICU.0000000000000446. [DOI] [PubMed] [Google Scholar]
- 3.Day AC, Lau NM, Stevens JD. Nonpenetrating femtosecond laser intrastromal astigmatic keratotomy in eyes having cataract surgery. J Cataract Refract Surg. 2016;42(1):102–109. doi: 10.1016/j.jcrs.2015.07.045. [DOI] [PubMed] [Google Scholar]
- 4.Bazzazi N, Barazandeh B, Kashani M, Rasouli M. Opposite clear corneal incisions versus steep meridian incision phacoemulsification for correction of pre-existing astigmatism. J Ophthalmic Vis Res. 2008;3(2):87–90. [PMC free article] [PubMed] [Google Scholar]
- 5.Vickers LA, Gupta PK. Femtosecond laser-assisted keratotomy. Curr Opin Ophthalmol. 2016;27(4):277–284. doi: 10.1097/ICU.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 6.Gu ZY, Ye MJ, Ji KK, Liao RF. Effects of astigmatic keratotomy combined with scleral tunnel incisions for the treatment of high astigmatism after penetrating keratoplasty. Exp Ther Med. 2019;17(1):495–501. doi: 10.3892/etm.2018.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lever J, Dahan E. Opposite clear corneal incisions to correct pre-existing astigmatism in cataract surgery. J Cataract Refract Surg. 2000;26(6):803–805. doi: 10.1016/s0886-3350(00)00378-3. [DOI] [PubMed] [Google Scholar]
- 8.Song WJ, Chen XY, Wang W. Effect of steep meridian clear corneal incisions in phacoemulsification. Eur J Ophthalmol. 2015;25(5):422–425. doi: 10.5301/ejo.5000575. [DOI] [PubMed] [Google Scholar]
- 9.Chiam PJ. Effect of paired opposite clear corneal incisions on with-the-rule versus against-the-rule astigmatism. Cornea. 2015;34(8):901–905. doi: 10.1097/ICO.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 10.Nemeth G, Kolozsvari B, Berta A, Laszlo M. Paired opposite clear corneal incision: time-related changes of its effect and factors on which those changes depend. Eur J Ophthalmol. 2014;24(5):676–681. doi: 10.5301/ejo.5000428. [DOI] [PubMed] [Google Scholar]
- 11.Yoon JH, Kim KH, Lee JY, Nam DH. Surgically induced astigmatism after 3.0 mm temporal and nasal clear corneal incisions in bilateral cataract surgery. Indian J Ophthalmol. 2014;62(6):753. doi: 10.4103/0301-4738.136308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mastropasqua L, Toto L, Mastropasqua A, Vecchiarino L, Mastropasqua R, Pedrotti E, di Nicola M. Femtosecond laser versus manual clear corneal incision in cataract surgery. J Refract Surg. 2014;30(1):27–33. doi: 10.3928/1081597X-20131217-03. [DOI] [PubMed] [Google Scholar]
- 13.Savini G, Versaci F, Vestri G, Ducoli P, Næser K. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg. 2014;40(10):1645–1653. doi: 10.1016/j.jcrs.2014.01.046. [DOI] [PubMed] [Google Scholar]
- 14.Tognetto D, Perrotta AA, Bauci F, Rinaldi S, Antonuccio M, Pellegrino FA, Fenu G, Stamatelatos G, Alpins N. Quality of images with toric intraocular lenses. J Cataract Refract Surg. 2018;44(3):376–381. doi: 10.1016/j.jcrs.2017.10.053. [DOI] [PubMed] [Google Scholar]
- 15.Raucau M, El Chehab H, Agard E, Lagenaite C, Dot C. Toric lens implantation in cataract surgery: Automated versus manual horizontal axis marking, analysis of 50 cases. J Fr Ophtalmol. 2018;41(1):e1–e9. doi: 10.1016/j.jfo.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Day AC, Stevens JD. Predictors of femtosecond laser intrastromal astigmatic keratotomy efficacy for astigmatism management in cataract surgery. J Cataract Refract Surg. 2016;42(2):251–257. doi: 10.1016/j.jcrs.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 17.Chan TC, Cheng GP, Wang Z, Tham CC, Woo VC, Jhanji V. Vector analysis of corneal astigmatism after combined femtosecond-assisted phacoemulsification and arcuate keratotomy. Am J Ophthalmol. 2015;160(2):250–255.e2. doi: 10.1016/j.ajo.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann C, Peter J, Ooi K, Phipps S, Cooper P, Goggin M, Queen Elizabeth Astigmatism Study Group Limbal relaxing incisions versus on-axis incisions to reduce corneal astigmatism at the time of cataract surgery. J Cataract Refract Surg. 2005;31(12):2261–2265. doi: 10.1016/j.jcrs.2005.08.046. [DOI] [PubMed] [Google Scholar]
- 19.Day AC, Stevens JD. Stability of keratometric astigmatism after non-penetrating femtosecond laser intrastromal astigmatic keratotomy performed during laser cataract surgery. J Refract Surg. 2016;32(3):152–155. doi: 10.3928/1081597X-20160204-01. [DOI] [PubMed] [Google Scholar]