Abstract
Objectives:
We estimate the proportion of family caregivers assisting older adults during Medicare home health who have an identified need for activity-specific training and identify characteristics associated with caregiver training needs.
Design:
Nationally representative retrospective cohort study.
Setting and Participants:
1,758 (weighted n=8,477,990) Medicare beneficiaries who participated in the National Health and Aging Trends Study (NHATS) and received Medicare-funded home health care between 2011–2016.
Measures:
Older adult and caregiving network characteristics before home health (sociodemographic factors, caregiver assistance, older adult health and function) were drawn from NHATS; characteristics during home health (family caregiver training needs, older adult health and function) were drawn from home health patient assessments. Weighted proportions of family caregivers with an identified need for activity-specific training were estimated. Weighted, multivariable logistic regressions modelled associations between older adult/caregiving network characteristics and family caregivers’ identified activity-specific training needs during home health.
Results:
More than 1 in 3 (35.7%) family caregivers assisting older adults during Medicare home health had an identified training need with at least one caregiving activity. Rates of need for training varied widely, from 8.6% among caregivers helping with advocacy to 48.2% among caregivers helping with medical procedures. In weighted analyses that adjusted for older adults’ health and function, family caregivers were less likely to have identified training needs when assisting older adults with ongoing disability or who received caregiver assistance prior to home health admission.
Conclusions and Implications:
Findings highlight the pervasiveness of family caregivers’ training needs, particularly with medically-oriented activities, and indicate that escalations in older adults’ care needs are linked to caregiver training needs. Therefore, transitions of care may present critical opportunities to connect family caregivers with training resources.
Keywords: Older adult, family caregiver, home health, home care services, Medicare
Brief Summary:
More than 1 in 3 family caregivers of older adults receiving home health were identified as having training needs. Developing strategies to better support family caregivers could improve quality and efficiency of home health care.
Introduction:
Family and unpaid caregivers are an important source of care for older adults with disabilities and/or chronic illness1–3 and emerging literature suggests that family caregiver characteristics affect older adults’ ability to remain safely in the community, avoiding unplanned healthcare utilization.4–8 There is mounting evidence that providing training for family caregivers may reduce caregiver burden and improve older adult health outcomes.1,9–13 Yet, the majority of family caregivers report feeling unprepared for their caregiving role1 and fewer than 1 in 10 report receiving role-related training.14 Little is known regarding what proportion of family caregivers need training across care delivery settings, how training need varies by caregiving activity, and what characteristics are associated with training needs.
Family caregiver training is especially important within the context of Medicare-funded home health care, through which eligible beneficiaries receive skilled nursing, rehabilitation therapy, and personal care aide services in their homes. The home health patient population exhibits significant social and medical vulnerability,15 and home health clinicians and staff are only present in the home environment intermittently. As a result, home health providers commonly rely on family caregivers to help meet patient care needs: in 87% of Medicare-funded home health episodes, home health clinicians report a need for family caregiver assistance.16 The Centers for Medicare and Medicaid Services (CMS) recently mandated that home health clinicians assess caregivers’ ability to provide assistance and offer training as needed.17 However, there is limited information available to guide providers’ efforts in designing and implementing family caregiver training programs.
This study provides the first evidence regarding family caregiver training needs during Medicare home health. We rely on a unique dataset that combines a nationally representative survey of older adults with linked Medicare home health patient assessments. Study objectives include quantifying the scope of family caregivers’ training needs during home health and identifying characteristics, beyond those already captured in home health patient assessments, that may assist home health providers in recognizing caregivers most in need of access to training. To achieve these objectives, we estimate the proportion of family caregivers identified by home health clinicians as requiring activity-specific training during a Medicare home health episode and examine characteristics prior to home health that are associated with caregivers’ identified training needs. Given prior work linking assistance with select medically-oriented activities to greater information-seeking among caregivers,18 as well as the inherent complexity of nursing and medical tasks, we hypothesized that family caregivers would be more likely to need training related to medically-oriented activities. Findings are relevant to home health providers’ efforts to comply with new CMS requirements and to ongoing efforts to better support family caregivers of older adults within care delivery settings.1,11,19–21
Methods:
Data Sources
Data for this study were drawn from the National Health and Aging Trends Study (NHATS) and the Outcomes and Assessment Information Set (OASIS). NHATS is an annual, nationally representative survey of Medicare beneficiaries ages 65 and older that collects comprehensive information on participants’ sociodemographic characteristics, health and functional status, and support from family and unpaid caregivers during in-person interviews.22 OASIS is a standardized patient assessment completed by home health clinicians (either a registered nurse (RN) or physical therapist (PT)) and submitted to CMS at regular intervals during a Medicare funded home health episode. OASIS includes information regarding the home health patient’s clinical and functional status, plan of care, and receipt of family caregiver assistance.
Study Cohort
The study included 1,758 (weighted n=8,477,990) community-dwelling older adults who participated in the 2011 NHATS and received home health care within one year of the baseline (2011) or a subsequent follow-up interview (2012–2015). To construct this dataset, we pooled NHATS data from 2011–2015 with linked OASIS data from 2011–2016 and matched each participant’s OASIS Start of Care filing for their index home health episode with the immediately preceding NHATS interview. We exclusively examined the index home health episode; therefore, each participant appears in the dataset only once. We excluded NHATS participants who did not receive home health care during the observation period, as well as those living in congregate settings (i.e. assisted living facilities), due to the availability of supports that may substitute for or otherwise affect family caregiving. This study was deemed exempt from human subjects review by the Institutional Review Board at the authors’ primary institution.
Measures
Older Adult Characteristics
From NHATS, we identified older adults’ sociodemographic characteristics (age, sex, race, educational attainment, Medicaid-enrollment), living arrangement (living alone), caregiving patterns (presence of a paid caregiver, hours of care/month, types of assistance received), dementia status, and health status (number of chronic conditions, fall in prior year). Types of caregiver assistance received include assistance with household, mobility, or self-care tasks due to health or functional issues and assistance with medication management. Dementia status was determined from self-reported physician diagnosis of Alzheimer’s or dementia, proxy respondent responses to a dementia screening tool, and older adult performance on cognitive tests in the NHATS, as described previously by Kasper et al (2013).23
From the OASIS, we identified measures of older adults’ health and care needs (post-acute status, cognitive impairment, functional impairment, and clinical severity) during home health. We characterized an individual as post-acute if they received inpatient acute or post-acute care in the 14 days prior to the home health episode. Cognitive impairment was measured via home health clinician assessment of the older adult: we considered older adults to have no cognitive impairment if the home health clinician noted that they were “alert and oriented…comprehend and recall task direction independently” and some cognitive impairment otherwise.24 We drew measures of functional impairment and clinical severity from Health Insurance Prospective Payment System (HIPPS) codes.24,25 HIPPS codes are used for home health payment risk adjustment25,26 and identify home health patients as having little or no, moderate, or significant functional impairment and clinical severity.
Identified Need for Caregiver Training
Family caregiver identified training needs are drawn from home health clinician reports during the home health episode that are documented in the OASIS. Home health clinicians who may complete an OASIS patient assessment include Registered Nurses (RN) or Physical Therapists (PT). In our sample, 88.5% of assessments were completed by an RN. The type of assessor (RN vs PT) was not significantly associated with whether the family caregiver had an identified training need in any caregiving activity.
Across seven activities, home health clinicians document whether an older adult needs family caregiver assistance, whether they receive this assistance, and whether the caregiver needs training/supervision in order to provide this assistance.24 We constructed binary indicators of whether the family caregiver had an identified training need with each activity, limiting the sample to cases in which home health clinicians identified the older adult as both requiring and receiving family caregiver assistance with that activity. OASIS specifies seven potential caregiving activities, including assisting with:
Medical procedures (treatments or procedures such as changing wound dressings or home exercise programs),
Equipment management (oxygen, intravenous/infusion equipment, enteral/parenteral nutrition, or ventilator therapy equipment),
Medication management (managing and taking oral, inhaled, or injectable medications),
Self-care tasks (transfer/ambulation, bathing, dressing, toileting, eating/feeding),
Patient supervision (monitoring to ensure patient’s safety),
Household chores (meals, housekeeping, laundry, telephone, shopping, finances),
Advocacy (facilitating patient’s participation in appropriate medical care).
Statistical Analysis
We first assessed the proportion of family caregivers assisting during Medicare home health who had an identified training need, both for any activity and by specific activity. In prior work, we found that the proportion of home health patients who needed caregiver assistance varied by activity: 84.7% required assistance with household chores, 82.5% with advocacy, 80.3% with self-care tasks, 65.2% with medication management, 56.9% with patient supervision, 37.1% with medical procedures, and 20.4% with equipment.16
We model family caregivers’ identified training need with each of the seven specific activities described in the OASIS using weighted, multivariable logistic regression. We limited analyses to home health episodes in which clinicians reported that the patient needed and received family caregiver assistance with the given activity. Models test each characteristic individually while adjusting for measures of older adult care needs/health status during the home health episode (older adult post-acute status, cognitive impairment, functional impairment, and clinical severity). We adjust for these measures as family caregivers were more likely to have identified training needs across multiple caregiving activities if helping an older adult who was post-acute, cognitively impaired, or had greater functional impairment or clinical severity during the episode (Table 1). All analyses used survey weights and design variables to account for non-probability sampling and to produce nationally representative estimates. Analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Table 1.
Older Adult Characteristics During Home Health Associated with Family Caregivers’ Identified Training needs during Home Health, by Caregiving Activity(n=1,758 unweighted, n=8,477,990 weighted)*
| Older adult characteristics (measured during home health): | Family caregiver has identified training need with: | ||||||
|---|---|---|---|---|---|---|---|
| Medically-oriented activities | Functional activities | ||||||
| Medical procedures | Equipment management | Medication management | Self-care tasks | Patient supervision | Household chores | Advocacy | |
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Post-acute entry to home health | 1.13 (0.73, 1.74) | 2.65 (1.57, 4.47) | 1.11 (0.81, 1.52) | 1.54 (1.08, 2.19) | 1.36 (0.92, 2.03) | 1.78 (1.15, 2.76) | 1.91 (1.07, 3.41) |
| Cognitive impairment | 1.59 (1.04, 2.44) | 1.61 (0.89, 2.91) | 1.56 (1.14, 2.12) | 1.98 (1.47, 2.68) | 1.73 (1.15, 2.60) | 1.84 (1.20, 2.84) | 2.23 (1.34, 3.73) |
| Functional impairment | |||||||
| Little or no | REF | REF | REF | REF | REF | REF | REF |
| Moderate | 1.42 (0.72, 2.83) | 2.10 (0.53, 8.30) | 1.81 (1.01, 3.25) | 3.05 (1.68, 5.52) | 2.73 (1.03, 7.24) | 2.85 (1.20, 6.75) | 1.19 (0.54, 2.63) |
| Significant | 3.03 (1.38, 6.65) | 3.62 (0.90, 14.66) | 2.61 (1.31, 5.17) | 5.54 (2.69, 11.43) | 4.11 (148, 11.42) | 5.56 (2.13, 14.53) | 2.95 (1.21, 7.19) |
| Clinical severity | |||||||
| Low | REF | REF | REF | REF | REF | REF | REF |
| Moderate | 1.55 (0.83, 2.89) | 1.12 (0.47, 2.66) | 1.45 (0.97, 2.16) | 1.49 (1.02, 2.17) | 1.24 (0.74, 2.06) | 1.24 (0.76, 2.03) | 1.29 (0.69, 2.41) |
| Significant | 1.65 (0.92, 2.97) | 1.60 (0.73, 3.53) | 1.78 (1.20, 2.65) | 1.32 (0.91, 1.93) | 1.14 (0.74, 1.77) | 1.65 (0.98, 2.79) | 1.53 (0.81, 2.88) |
Linked National Health and Aging Trends Study (NHATS) and Outcome and Assessment Information Set (OASIS) data for Medicare beneficiaries receiving family caregiver assistance during a home health episode, 2011–2016.
Results:
Among a nationally representative sample of older adults receiving home health between 2011–2016, the average age was 79.5 years, 39.7% were male, 21.2% were non-white, and 16.9% were Medicaid-enrolled (Table 2). Of family caregivers assisting home health patients with any care activity, 35.7% required training (Figure 1). Among those assisting with any medically-oriented activity (medical procedures, equipment management, medication management) 36.8% required training and among those assisting with any functional activity (self-care tasks, patient supervision, household chores, advocacy) 25.9% required training. The proportion of family caregivers who required training with individual activities ranged from 8.6%, for training related to advocacy, to 48.2%, for training related to medical procedures.
Table 2.
Characteristics of Community-Dwelling Older Adults Receiving Medicare Home Health between 2011–2016(n=1,758 unweighted, n=8,477,990 weighted)*
| Characteristics | % (n) or Mean ± SE |
|---|---|
| Measured prior to home health | |
| Age | 79.5 ± 0.23 |
| Male sex | 39.7% (663) |
| Non-white race | 21.2% (618) |
| Medicaid enrolled | 16.9% (362) |
| Medicare Advantage enrolled | 30.8% (544) |
| Education: | |
| High school or less | 58.3% (1,108) |
| Some college | 41.7% (637) |
| Lives alone | 34.0% (618) |
| Has paid caregiver | 16.9% (321) |
| Hours/month of caregiver assistance | 105.2 ± 5.47 |
| Received caregiver assistance with: | |
| Household tasks, mobility, or self-care | 59.5% (1,133) |
| Medication management | 16.8% (371) |
| Probable dementia | 17.7% (397) |
| 2+ chronic conditions† | 17.9% (446) |
| Fell in past year | 44.4% (787) |
| Hospitalized in past year | 30.1% (560) |
| Measured during home health | |
| Post-acute admission | 72.2% (1,182) |
| Cognitive impairment | 42.0% (829) |
| Functional impairment | |
| None/low | 16.6% (265) |
| Moderate | 62.8% (1,114) |
| High | 20.7% (379) |
| Clinical severity | |
| Low | 27.0% (476) |
| Moderate | 43.1% (743) |
| High | 29.9% (539) |
Data are drawn from National Health and Aging Trends Study (NHATS) and linked Outcomes and Assessment Information Set (OASIS) and Medicare claims data for Medicare beneficiaries receiving family caregiver assistance during a home health episode between 2011–2016. Percentages are weighted to account for NHATS survey design and to produce nationally representative estimates.
Chronic conditions include heart attack in previous year, heart disease, high blood pressure, diabetes, lung disease, and stroke in previous year.
Figure 1. Rates of Identified Training need among Family Caregivers Assisting during Medicare Home Health, by Caregiving Activity*,†.
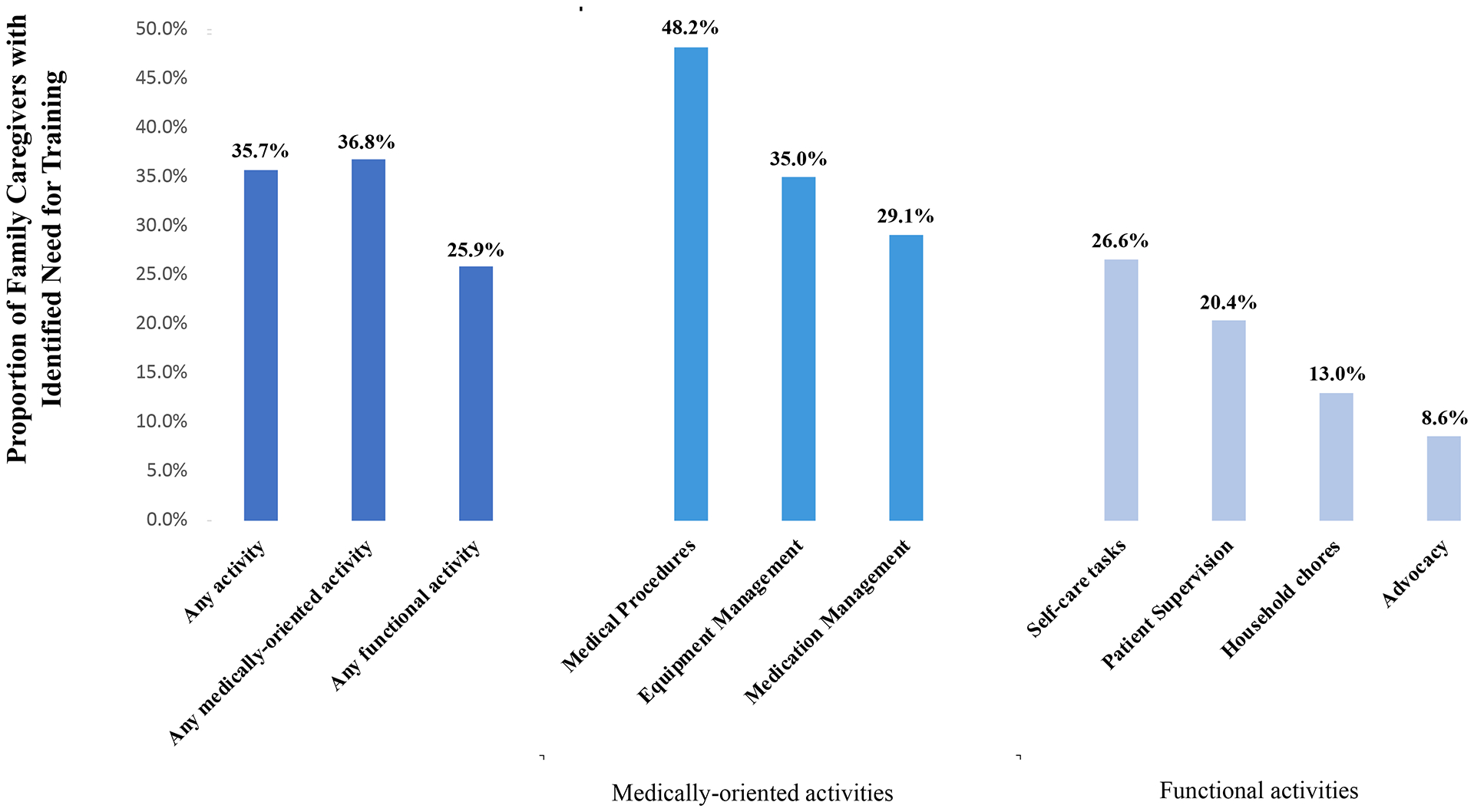
* Data drawn from National Health and Aging Trends Study (NHATS) and linked Outcomes and Assessment Information Set (OASIS) data for 1,758 Medicare beneficiaries receiving family caregiver assistance during a home health episode between 2011–2016. † Percentages weighted to account for National Health and Aging Trend Study (NHATS) survey design and produce nationally-representative estimates.
Family caregivers were less likely to have identified training needs during home health if assisting an older adult with greater ongoing care needs and/or greater reliance on family caregiver assistance prior to home health, after adjusting for care needs/health status during home health (Table 3). If the older adult had probable dementia prior to home health, family caregivers were less likely to have identified training needs with medically-oriented activities, including: medical procedures (aOR (Adjusted Odds Ratio): 0.42; CI (95% confidence interval): 0.23, 0.79), equipment management (aOR: 0.32; CI: 0.16, 0.65), and medication management (aOR=0.61; CI: 0.41, 0.91). If the older adult had two or more chronic conditions present prior to home health, family caregivers were less likely to have an identified training need with medical procedures (aOR: 0.53; CI: 0.34, 0.82), medication management (aOR=0.56; CI: 0.40, 0.91), self-care tasks (aOR: 0.50; CI:0.36, 0.71), and household chores (aOR: 0.46; CI: 0.28, 0.76).
Table 3.
Older Adult Characteristics Prior to Home Health Associated with Family Caregivers’ Identified Training needs during Home Health, by Caregiving Activity(n=1,758 unweighted, n=8,477,990 weighted)*
| Older adult characteristics (measured prior to home health): | Family caregiver has identified training need with: | ||||||
|---|---|---|---|---|---|---|---|
| Medically-oriented activities | Functional activities | ||||||
| Medical procedures | Equipment management | Medication management | Self-care tasks | Patient supervision | Household chores | Advocacy | |
| aOR‡(95% CI) | aOR‡(95% CI) | aOR‡(95% CI) | aOR‡(95% CI) | aOR‡(95% CI) | aOR‡(95% CI) | aOR‡(95% CI) | |
| Age | 1.01 (0.98, 1.03) | 1.02 (0.98, 1.06) | 0.99 (0.97, 1.01) | 1.02 (0.99, 1.04) | 0.99 (0.96, 1.01) | 1.00 (0.97, 1.03) | 0.99 (0.97, 1.02) |
| Male sex | 1.01 (0.68, 1.49) | 1.23 (0.74, 2.06) | 0.81 (0.58, 1.12) | 1.13 (0.84, 1.54) | 1.11 (0.67, 1.85) | 1.37 (0.91, 2.06) | 1.17 (0.76, 1.80) |
| Non-white race | 0.81 (0.46, 1.41) | 0.73 (0.39, 1.37) | 1.01 (0.68, 1.51) | 0.78 (0.53, 1.15) | 0.91 (0.61, 1.36) | 0.97 (0.66, 1.42) | 0.81 (0.51, 1.29) |
| Medicaid enrolled | 0.99 (0.53, 1.88) | 0.73 (0.36, 1.48) | 1.06 (0.70, 1.60) | 0.70 (0.46, 1.05) | 0.73 (0.43, 1.24) | 0.79 (0.46, 1.37) | 0.73 (0.39, 1.36) |
| Medicare Advantage enrolled | 0.86 (0.55, 1.33) | 1.09 (0.57, 2.06) | 1.18 (0.81, 1.70) | 1.12 (0.79, 1.59) | 1.39 (0.88, 2.19) | 0.96 (0.62, 1.51) | 1.12 (0.68, 1.83) |
| Education: | |||||||
| High school or less | REF | REF | REF | REF | REF | REF | REF |
| Some college | 1.54 (1.04, 2.30) | 2.38 (1.23, 4.63) | 0.98 (0.68, 1.43) | 1.12 (0.77, 1.63) | 1.04 (0.69, 1.57) | 1.05 (0.72, 1.53) | 0.92 (0.59, 1.43) |
| Lives alone | 1.15 (0.76, 1.75) | 1.69 (0.94, 3.03) | 1.34 (1.01, 1.78) | 1.15 (0.81, 1.65) | 1.15 (0.77, 1.71) | 1.14 (0.80, 1.63) | 1.10 (0.72, 1.66) |
| Has paid caregiver | 0.86 (0.53, 1.39) | 1.15 (0.52, 2.55) | 0.83 (0.57, 1.23) | 0.83 (0.60, 1.16) | 0.49 (0.29, 0.82) | 0.73 (0.46, 1.15) | 0.40 (0.17, 0.95) |
| Hours/month of caregiver help | 0.99 (0.99, 1.00) | 0.99 (0.99, 0.99) | 1.00 (0.99, 1.00) | 0.99 (0.99,1.00) | 1.00 (0.99, 1.00) | 0.99 (0.99, 1.00) | 1.00 (0.99, 1.00) |
| Types of caregiver help: | |||||||
| Household, mobility, or self-care tasks | 0.55 (0.33, 0.93) | 0.35 (0.20, 0.63) | 0.63 (0.44, 0.90) | 0.69 (0.50, 0.96) | 0.53 (0.36, 0.76) | 0.58 (0.38, 0.87) | 0.56 (0.34, 0.92) |
| Medication management | 0.33 (0.18, 0.63) | 0.25 (0.12, 0.53) | 0.47 (0.33, 0.65) | 0.63 (0.42, 0.94) | 0.46 (0.30, 0.69) | 0.67 (0.43, 1.02) | 0.49 (0.29, 0.81) |
| Probable dementia | 0.42 (0.23, 0.79) | 0.32 (0.16, 0.65) | 0.61 (0.41, 0.91) | 0.67 (0.45, 1.00) | 0.63 (0,41, 0.99) | 0.73 (0.47, 1.15) | 0.47 (0.24, 0.90) |
| 2+ chronic conditions‡ | 0.53 (0.34, 0.82) | 0.59 (0.30, 1.13) | 0.56 (0.40, 0.78) | 0.50 (0.36, 0.71) | 0.67 (0.41, 1.09) | 0.46 (0.28, 0.76) | 0.77 (0.44, 1.37) |
| Fell in past year | 0.60 (0.37, 0.96) | 0.64 (0.40, 1.03) | 0.85 (0.61, 1.18) | 0.92 (0.65, 1.29) | 0.75 (0.49, 1.14) | 0.95 (0.65, 1.40) | 0.79 (0.55, 1.13) |
Linked National Health and Aging Trends Study (NHATS) and Outcome and Assessment Information Set (OASIS) data for Medicare beneficiaries receiving family caregiver assistance during a home health episode, 2011–2016.
Adjusted Odds Ratio. Adjusted for characteristics measured during home health episode: post-acute entry into home health, cognitive impairment, functional impairment, and clinical severity.
Chronic conditions include heart attack in previous year, heart disease, high blood pressure, diabetes, lung disease, and stroke in previous year.
Family caregivers were approximately half as likely to have identified training needs with each of the medically-oriented and functional activities if the older adult received caregiver assistance prior to home health. Particularly strong relationships were observed between prior assistance with medication management and caregivers’ identified training need with medically-oriented activities: family caregivers were less likely to have identified training needs related to medical procedures (aOR: 0.33; CI: 0.18, 0.63), equipment management (aOR: 0.25; CI: 0.12, 0.53), and medication management (aOR=0.47; CI: 0.33, 0.65) if the older adult had been receiving caregiver assistance with medication management prior to home health. Intensity of caregiving prior to home health (hours/month of family caregiver assistance) was not significantly associated with caregivers’ identified training needs during the home health episode. However, if a paid caregiver was present prior to home health, family caregivers were less likely to have an identified training need with patient supervision (aOR: 0.49; CI: 0.29, 0.82) and advocacy (aOR: 0.40; CI: 0.17, 0.95).
Discussion:
Home health clinicians identified more than one-third of family caregivers assisting during Medicare home health as requiring training related to their caregiving activities. Family caregivers’ identified training need was greatest for medically-oriented activities: nearly half of family caregivers assisting with medical procedures required training, while about one in three assisting with equipment or medication management required training. Caregivers were less likely to be identified as requiring training if assisting an older adult with ongoing care needs and caregiving support; these relationships were strongest for medically-oriented activities. Findings suggest that there are significant training needs among family caregivers assisting during Medicare home health, that rates of training need differ by caregiving activity, and that greater reliance on caregiver assistance prior to the home health episode is associated with family caregivers being better prepared and less in need of additional support during home health.
Our findings may inform the development and prioritization of training resources directed to family caregivers in the home health context. While numerous caregiver training models have been developed, implementation studies have been limited to the ambulatory setting10,11,27–29 and interventions focus largely on the management of dementia-related behavioral symptoms.10,27–29 Thus, available resources may be less applicable to the specific training needs observed in the home health setting, with respect to greater training needs for medically-oriented activities and older adults without dementia. Importantly, standardized family caregiver assessments were not used to guide access to these interventions.10,11,27–29 However, results of this study suggest that systematically soliciting information, beyond what is currently collected in the OASIS, could be a valuable tool for home health providers to guide training resources to caregivers most in need of this support. Information regarding contextual factors prior to home health, and especially caregivers’ prior experiences of providing assistance, may help providers in prioritizing access to training.
We find that caregivers are more likely to need training if there has been a recent escalation in the older adult’s care needs, such as those commonly observed during care transitions surrounding acute health events. During care transitions, family caregivers are often required to assist with new activities or provide more intensive support;30–32 in particular, caregivers often assume greater responsibility for medically-oriented activities.30 In our analyses, caregivers were most likely to have an identified training need on medically-oriented activities. While this finding may be related to our reliance on a measure of clinician-reported training needs, prior work has found that assisting with these types of activities is linked to greater caregiving intensity and burden.2,33 There is already wide acknowledgement of the need to improve provider engagement with family caregivers during care transitions.34–38 Our findings suggest that these transitions may also offer an important opportunity to connect family caregivers with training resources. Structural factors such as narrow reimbursement opportunities for time spent interacting with caregivers31,36 represent existing threats to caregivers’ access to training during transitions of care that could be remedied by strengthening legislation such as the CARE Act34 to require clinician communication with and support of family caregivers during critical episodes of care.
As public payers, including Medicare, Medicaid, and Veterans Affairs (VA), expand access to community-based services,39–42 and as demographic trends lead to more older adults aging in place with complex health and functional needs,3,43,44 more older adults will experience significant shifts in care needs that occur wholly within the community. These changes are not care transitions in the traditional sense, but represent key inflection points in the care trajectory where access to training may be needed. The VA’s Helping Invested Families Improve Veterans’ Experiences Study (HI-FIVES) is an example of how access to training can be linked to changes in need that occur while the older adult ages in place.11 Caregivers are approached for inclusion in HI-FIVES following an escalation in the older adult’s use of home- and community-based long-term services and supports.45 Integrated health care systems could similarly identify changes in utilization or referral patterns which indicate an intensification of the older adult’s care needs and use these as opportunities to assess existing caregiver(s), offering training resources as appropriate. Improving access to training for these family caregivers may contribute to improved health outcomes and reduced utilization1,9,10 for high-need, community-dwelling older adults.
Limitations
This work is subject to several limitations. First, we are constrained to the information available in the NHATS and OASIS and as a result, cannot determine whether the family caregivers evaluated in the OASIS were also providing assistance at the time of NHATS interview. However, it is reasonable to assume that one of the established caregivers identified in the NHATS would continue in their caregiving role during a home health episode occurring within one year. Second, measures of caregiver assistance and training needs during the home health episode are drawn from home health clinician reports in the OASIS. Research on the reliability and validity of OASIS items is generally sparse,46 and no available research tests the psychometric properties of these measures in particular. Nonetheless, the OASIS represents the most comprehensive source of information on home health episodes nationwide. Third, we limit our sample to index home health episodes and therefore our findings may not be reflective of later episodes in a sustained period of home health utilization.
Conclusions and Implications:
We found that a high proportion of family caregivers assisting during Medicare home health episodes are identified as needing activity-specific training and that rates of identified training need vary by caregiving activity and older adult characteristics. Caregivers were more likely to require training during the home health episode if assisting an older adult who had experienced lower levels of previous assistance, suggesting that shifts in older adults’ care needs may present important opportunities for providers to connect family caregivers with training supports, which can improve well-being and outcomes for both family caregivers and older adults.1,9–12 Future research is warranted which examines the relationship of family caregiver training to older adult health care utilization and outcomes in community settings.
Acknowledgements:
Authors thank Dr. Judith Kasper for sharing her expertise regarding development of the National Health and Aging Trends Study (NHATS) complex survey weights. This work was supported by the National Institute on Aging under Grant R01AG047859 and by the Agency for Health Care Research and Quality under Grant T32HS0000029.
Funding sources: This work was supported by the National Institute on Aging under Grant R01AG047859 and by the Agency for Health Care Research and Quality under Grant T32HS0000029.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
Authors have no conflicts of interest to report.
REFERENCES
- 1.National Academies of Sciences, Engineering, and Medicine. (2016). Families Caring for an Aging America. Washington, DC: The National Academies Press; 10.17226/23606. [DOI] [PubMed] [Google Scholar]
- 2.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A National Profile of Family and Unpaid Caregivers Who Assist Older Adults With Health Care Activities. JAMA Intern Med. 2016;176(3):372–379. doi: 10.1001/jamainternmed.2015.7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Favreault M, Dey J. Long-term services and supports for older Americans: Risk and financing research brief. Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services; Washington, DC; 2016. [Google Scholar]
- 4.Hass Z, DePalma G, Craig BA, Xu H, Sands LP. Unmet Need for Help With Activities of Daily Living Disabilities and Emergency Department Admissions Among Older Medicare Recipients. Gerontologist. 2017;57(2):206–210. doi: 10.1093/geront/gnv142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accounting for Social Risk Factors in Medicare Payment. Washington, DC: National Academies of Science, Engineering, and Medicine; 2017. [PubMed] [Google Scholar]
- 6.Castillo EM, Brennan JJ, Howard J, et al. Factors Associated With Geriatric Frequent Users of Emergency Departments. Ann Emerg Med. 2019; 74 (2), 270–275. doi: 10.1016/j.annemergmed.2018.12.013 [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE. Hospitalization in older persons: not just a medical outcome, a social outcome as well: comment on “Elder abuse as a risk factor for hospitalization in older persons”. JAMA Intern Med. 2013;173(10):919. [DOI] [PubMed] [Google Scholar]
- 8.Wolff JL, Mulcahy J, Roth DL, et al. Long-Term Nursing Home Entry: A Prognostic Model for Older Adults with a Family or Unpaid Caregiver. J Am Geriatr Soc. 2018;66(10):1887–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuckols TK, Keeler E, Morton S, et al. Economic Evaluation of Quality Improvement Interventions Designed to Prevent Hospital Readmission: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177(7):975–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teri L, Logsdon RG, McCurry SM, Pike KC, McGough EL. Translating an Evidence based Multicomponent Intervention for Older Adults With Dementia and Caregivers. Gerontologist. 2018; doi: 10.1093/geront/gny122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Houtven CH, Smith VA, Lindquist JH, et al. Family Caregiver Skills Training to Improve Experiences of Care: a Randomized Clinical Trial. J Gen Intern Med. 2019; 34 (10), 2114–2122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hepburn KW, Tornatore J, Center B, Ostwald SW. Dementia family caregiver training: affecting beliefs about caregiving and caregiver outcomes. J Am Geriatr Soc. 2001;49(4):450–457. [DOI] [PubMed] [Google Scholar]
- 13.Terracciano A, Artese A, Yeh J, Egderton L, et al. Effectiveness of Powerful Tools for Caregivers on Caregiver Burden and on Care Recipient Behavioral and Psychological Symptoms of Dementia: A Randomized Controlled Trial. J Am Med Dir Assoc. 2019. doi: 10.1016/j.jamda.2019.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burgdorf J, Roth DL, Riffin C, Wolff JL. Factors Associated with Receipt of Training Among Caregivers of Older Adults. JAMA Intern Med. 2019; 179(6):833–835. doi: 10.1001/jamainternmed.2018.8694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Home Health Chartbook 2018:Prepared for the Alliance for Home Health Quality and Innovation. Alliance for Home Health Quality and Innovation & Avalere Health; 2018. Available from: http://ahhqi.org/images/uploads/AHHQI_2018_Chartbook_09.21.2018.pdf. Accessed 9/12/2019. [Google Scholar]
- 16.Burgdorf J, Arbaje A, & Wolff JL. Older Adult Factors Associated With Identified Need for Family Caregiver Assistance During Home Health Care Home Health Care Management & Practice. 2019; doi: 10.1177/1084822319876608 [DOI] [Google Scholar]
- 17.Medicare and Medicaid Program: Conditions of Participation for Home Health Agencies. Washington, DC: Centers for Medicare and Medicaid Services; 2017. Available from: https://www.federalregister.gov/documents/2017/01/13/2017-00283/medicare-and-medicaid-program-conditions-of-participation-for-home-health-agencies. Accessed 2/5/2020. [Google Scholar]
- 18.Noureldin M, Murawski MM, Mason HL, Hyner GC, Plake KS. The association between family caregivers’ involvement in managing older adults’ medications and caregivers’ information-seeking behavior. J Am Pharm Assoc (2003). 2017;57(2):170–177.e171. [DOI] [PubMed] [Google Scholar]
- 19.Wolff JL, Feder J, Schulz R. Supporting Family Caregivers of Older Americans. N Engl J Med. 2016;375(26):2513–2515. [DOI] [PubMed] [Google Scholar]
- 20.Jennings LA, Reuben DB, Evertson LC, et al. Unmet needs of caregivers of individuals referred to a dementia care program. J Am Geriatr Soc. 2015;63(2):282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berg-Weger M, Tebb S. Caregiver Well-Being: Is it On Your Radar? J Am Med Dir Assoc. 2015;16(11):908–910. doi: 10.1016/j.jamda.2015.08.017 [DOI] [PubMed] [Google Scholar]
- 22.Freedman VA, Kasper JD. Cohort Profile: The National Health and Aging Trends Study (NHATS). Int J Epidemiol. 2019. doi: 10.1093/ije/dyz109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kasper J, Freedman V, Spillman B. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Technical Paper #5. Baltimore, MD: Johns Hopkins University School of Public Health;2013. [Google Scholar]
- 24.Outcome and Assessment Information Set Guidance Manual. Washington, DC: Centers for Medicare and Medicaid Services;2016. [Google Scholar]
- 25.Definition and Uses of Health insurance Prospective Payment System Codes (HIPPS Codes). Washington, DC: CMS Division of Institutional Claims Processing;2010. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ProspMedicareFeeSvcPmtGen/Downloads/hippsuses.pdf. Accessed 2/5/2020. [Google Scholar]
- 26.Home Health Care Services Payment System. Washington, DC: Medicare Payment Advisory Commission;2016. Available from: http://www.medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_17_hha_final.pdf. Accessed 2/5/2020. [Google Scholar]
- 27.Nichols LO, Martindale-Adams J, Burns R, Zuber J, Graney MJ. REACH VA: Moving form translation to system implementation. Gerontologist. 2016; 56(1):135–144. [DOI] [PubMed] [Google Scholar]
- 28.Burns R, Nichols LO, Martindale-Adams J, Graney MJ, Lummus A. Primary care interventions for dementia caregivers: 2-year outcomes from the REACH study. Gerontologist. 2003; 43(4):547–555. [DOI] [PubMed] [Google Scholar]
- 29.Nicols LO, Chang C, Lummus A, et al. The cost-effectiveness of a behavior intervention with caregivers of patients with Alzheimer’s disease. J Am Geriatr Soc. 2008; 56(3):413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson M, Kelly K, Kaplan A. Family caregiving and transitional care: a critical review. San Francisco, CA: Family Caregiver Alliance;2012. Available from: https://www.caregiver.org/family-caregiving-and-transitional-care-critical-review-2012. Accessed 2/5/2020. [Google Scholar]
- 31.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood). 2010;29(1):116–124. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell SE, Laurens V, Weigel GM, et al. Care Transitions From Patient and Caregiver Perspectives. Ann Fam Med. 2018;16(3):225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giovannetti ER, Wolff JL, Xue Q-L, et al. Difficulty assisting with health care tasks among caregivers of multimorbid older adults. J Gen Intern Med. 2012;27(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coleman EA. Family caregivers as partners in care transitions: The caregiver advise record and enable act. J Hosp Med. 2016;11(12):883–885. [DOI] [PubMed] [Google Scholar]
- 35.Arbaje A, Kansagara D, Salanitro A. Regardless of age: Incorporating principles from geriatric medicine to improve care transitions for patients with complex needs. J Gen Intern Med. 2014; 29 (6), 932–9. doi: 10.1007/s11606-013-2729-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Transitional Care Management Services. Medicare Learning Network. Washington, DC: Centers for Medicare and Medicaid Services; 2016. Available from: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. Accessed 2/5/2020. [Google Scholar]
- 37.Jones J, Nowels CT, Sudore R, Ahluwalia S, Bekelman DB. The future as a series of transitions: qualitative study of heart failure patients and their informal caregivers. J Gen Intern Med. 2015;30(2):176–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stolee P, Elliott J, Byrne K, et al. A Framework for Supporting Post-acute Care Transitions of Older Patients With Hip Fracture. J Am Med Dir Assoc. 2019;20(4):414–419.e411. [DOI] [PubMed] [Google Scholar]
- 39.Fact Sheet: 2019 Medicare Advantage and Part D Rate Announcement and Call Letter. Centers for Medicare and Medicaid Services; 2018. Available from: https://www.cms.gov/newsroom/fact-sheets/2019-medicare-advantage-and-part-d-rate-announcement-and-call-letter. Accessed 7/17/2019. [Google Scholar]
- 40.Ryan J, Coulter Edwards B. Rebalancing Medicaid Long-Term Services And Supports. Health Affairs Policy Brief. September 17, 2015. doi: 10.1377/hpb20150917.439553 [DOI] [Google Scholar]
- 41.Karuza J, Gillespie SM, Olsan T, et al. National Structural Survey of Veterans Affairs Home-Based Primary Care Programs. J Am Geriatr Soc. 2017;65(12):2697–2701. [DOI] [PubMed] [Google Scholar]
- 42.Independence at Home Demonstration. Centers for Medicare and Medicaid Services. Available at: https://innovation.cms.gov/initiatives/independence-at-home/. Accessed 8/27/2019.
- 43.Freedman VA, Spillman BC. Disability and care needs among older Americans. Milbank Q. 2014;92(3):509–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knickman JR, Snell EK. The 2030 problem: caring for aging baby boomers. Health Serv Res. 2002;37(4):849–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Houtven CH, Oddone EZ, Hastings SN, et al. Helping Invested Families Improve Veterans’ Experiences Study (HI-FIVES): study design and methodology. Contemp Clin Trials. 2014;38(2):260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O’Connor M, Davitt J. The Outcome and Assessment Information Set (OASIS): A Review of Validity and Reliability. Home Health Care Services Quarterly. 2012;31(4):267–301. [DOI] [PMC free article] [PubMed] [Google Scholar]


