Abstract
Objectives:
Current therapies for Juvenile Fibromyalgia (JFM), such as cognitive-behavioral therapy (CBT), improve pain coping but are less effective for pain reduction or engagement in physical activity. The Fibromyalgia Integrative Training for Teens (FIT Teens) program combines CBT with specialized neuromuscular exercise training for adolescents with JFM. The current investigation examined the effects of FIT Teens vs CBT on secondary outcomes of strength and functional biomechanics, utilizing 3D Motion capture technology. This study aimed to explore improvements in strength and biomechanics in both a CBT-only group and the FIT Teens intervention.
Methods:
Forty adolescents with JFM (12–18 years) were randomized to an 8-week, group-based protocol of either FIT Teens or CBT only. Assessments occurred pre- and post- treatment. Hip and knee strength were assessed with dynamometry, dynamic postural stability was measured using the Star Excursion Balance Test, and movement biomechanics were assessed with 3D motion analyses during a Drop Vertical Jump (DVJ) task.
Results:
The FIT Teens group exhibited improvements in hip abduction strength and greater external hip rotation during the DVJ task. Some differences between the FIT Teens and CBT groups were observed in peak hip internal moment in the transverse plane. Decreased hip adduction during the DVJ was also observed in the FIT Teens group.
Discussion:
Results suggest that the FIT Teens program shows promise in improving hip abduction strength and body biomechanics, indicating improvements in stability during functional movements. These improvements may facilitate ability to initiate and maintain regular physical activity in youth with widespread musculoskeletal pain.
Keywords: Neuromuscular training, Exercise, Biomechanics, Juvenile Fibromyalgia, Cognitive-Behavioral Therapy
INTRODUCTION
Juvenile Fibromyalgia (JFM) is a debilitating condition characterized by chronic musculoskeletal (MSK) pain.1,2 JFM affects primarily female adolescents3,4 and is associated with significant impairment in functional abilities,5,6 emotional functioning5–7 and physical activity participation.8 Current therapies such as cognitive-behavioral therapy (CBT) are effective in reducing functional disability in JFM9 and improving pain coping10 but are less effective in terms of pain reduction or engagement in physical activity.11 More powerful and multi-modal interventions are needed, such as those that incorporate exercise programming.12,13 Aerobic activity and muscle strengthening exercise of at least moderate intensity two to three times a week are recommended14 and have been associated with reductions in pain.8,15 Despite the benefits of physical exercise in fibromyalgia, effects are limited due to poor adherence8,16 and the pervasiveness of a sedentary lifestyle.17–19 Prolonged sedentary activity promotes further physical deconditioning and loss of functioning,20 making it difficult for individuals with chronic pain to initiate even moderate physical activity.
Avoidance of activity and increased sedentary activity is associated with poorer physical functioning, increased muscle weakness, and increased pain sensitivity in adult fibromyalgia,21 as well as higher levels of pain in adolescents with JFM.22,23 Such deconditioning may make it more difficult for individuals with pain to initiate regular physical activity. While graded-exposure interventions have been developed to help participants gradually improve engagement in physical activity, and subsequently reduce movement related fear,24–26 it has been proposed that poor movement biomechanics may increase susceptibility to pain or injury during exercise, and may also contribute to fear of movement and exercise avoidance.27 As such, exercise interventions focused on strength and biomechanics specifically may reduce fear of exercise and its avoidance. Utilizing sophisticated motion-capture assessment methods, our research group demonstrated that adolescents with JFM show alterations in fundamental movement biomechanics, decreased strength and poorer functional performance in comparison to healthy controls.23 These patterns of movement are associated with greater risk of injury.28,29 Our work investigates whether preparatory training in fundamental movement mechanics using specialized neuromuscular training integrated with behavioral coping skills can enhance patient outcomes by addressing decreased strength and poor movement biomechanics in youth with JFM,14 which may help prepare patients for future exercise and physical activity engagement.
The Fibromyalgia Integrative Training for Teens (FIT Teens) program is an intervention designed to improve both psychological coping skills and movement competence in JFM.30,31 FIT Teens combines CBT with a tailored neuromuscular exercise training program, derived from injury prevention research in athletes, but rarely used/novel in the treatment of chronic pain.29,32 Neuromuscular training gradually improves strength and biomechanics30,33,34 through the training of multiple muscle groups, in which participants are taught how to move in less injury-prone ways and improve movement competence during functional tasks. This graded and broad training minimizes delayed onset muscle soreness through a deliberate progression of isometric, concentric, and eccentric exercises followed by full functional movements that emphasize mastery before progression to the next level. For example, participants perform varied forms of sit-ups on a BOSU ball and plank exercises to build core strength and protect their back during bending and lifting movements (see Figure 1), as well as various iterations of a squat, which builds general lower limb muscular endurance and strengthens hip muscles, which are important to keeping the knees aligned while engaged in everyday tasks (e.g., running/walking, picking up objects, lifting objects).
Figure 1 – Example of an exercise progression across all 4 levels of neuromuscular training.
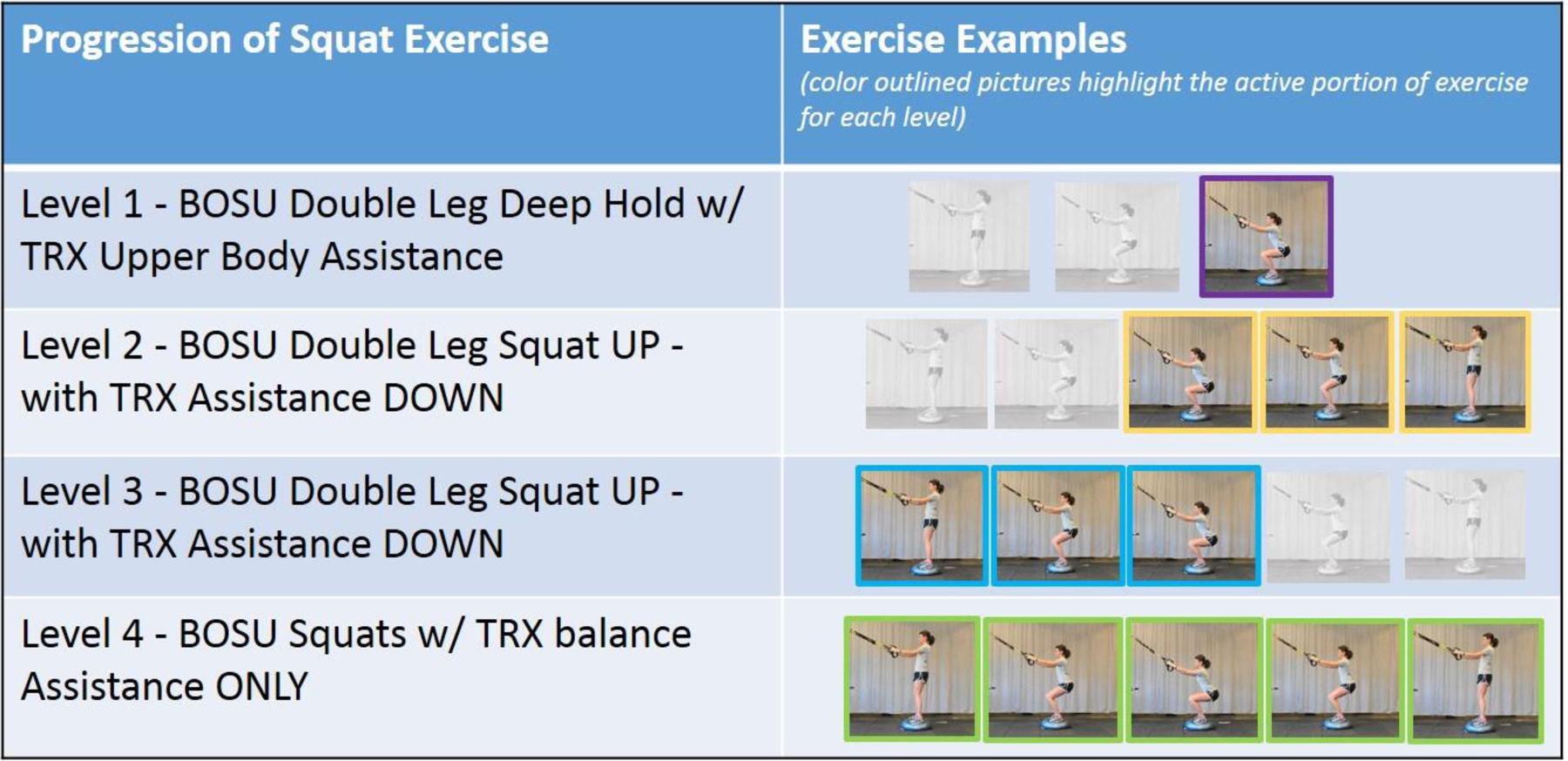
Level 1 – Isometric “holding” movements; Level 2 – Concentric “shortening” or resisting movement; Level 3 – Eccentric “lengthening” or creating movement; Level 4 – Full movement
In preliminary work, the FIT Teens program was associated with improvements in psychological outcomes, including fear of movement,30 and physical improvements in both strength and biomechanics.30,33 However, the pre-post design of the initial work did not include a control group so it was not possible to conclude that improvements were not simply due to task familiarity or time effects. The current study evaluated changes in biomechanics and knee and hip abduction strength as part of a pilot clinical trial comparing FIT Teens to a CBT-only condition. Biomechanics and strength measures were secondary outcomes collected as part of the primary pilot trial – the results of which showed FIT Teens to be promising for pain reduction (primary outcome).31 The aim of this secondary analysis was to evaluate biomechanics and strength based on 3-D motion analysis of performance in a standardized drop vertical jump (DVJ) task, strength (knee and hip dynamometry), and balance (Star Excursion Balance test) pre- and post- treatment. This analysis also aimed to explore potential changes in these areas of functioning in within a group that received CBT only and within the FIT Teens intervention.
MATERIALS AND METHODS
Participants
Adolescents (12–18 years old) with JFM (diagnosed by a pediatric rheumatologist or pain physician according to the 2010 American College of Rheumatology criteria modified for pediatric use)35 were recruited from pediatric rheumatology and pain clinics at a large Midwestern children’s hospital in the United States. Inclusion criteria were: moderate to high pain-related disability (measured by Functional Disability Inventory score ≥ 13)36 and at least moderate levels of pain (measured on a pain visual analog scale with score ≥ 4 on a 0 – 10 scale). Exclusion criteria included 1) diagnosis of a comorbid rheumatic disease (e.g., juvenile arthritis, systemic lupus erythematosus), 2) untreated major psychiatric diagnosis (e.g., major depression, bipolar disorder, and psychosis), 3) documented developmental delay, 4) any medical condition determined by their physician to be a contraindication for exercise, and 5) ongoing participation in CBT or physical therapy for pain.
Procedures
Screening and recruitment procedures are fully described in a prior publications of the primary pilot trial.6,31 Briefly, after informed consent, participants underwent a baseline assessment that included self-report questionnaires (primary outcomes, published elsewhere31) and physical assessments of balance, strength and biomechanics (secondary outcomes and the focus in this study). Using a 2-arm randomized controlled pilot trial design, participants were then group-randomized (consisting of 4–6 participants per group) to either a CBT-only group or the FIT Teens intervention.31 Randomization sequencing was obtained using random group generation in R. The study biostatistician (Peugh) maintained block randomization and concealed the group random assignment (i.e., FIT Teens or CBT) until after baseline measures had been completed; all other study personnel were blinded until this point. Post-treatment assessments were conducted within one week of the end of the 8-week treatment. At the completion of treatments, participants were provided with modest incentives – a gift basket with relaxation and stress management activities for the CBT group and a BOSU ® Balance Trainer for those in the FIT Teens group. Enrollment occurred from December 16, 2013 to April 1, 2016 and follow-up occurred from July 28, 2014 to August 31, 2016. Results of the primary trial were published in 2018.31
This study was approved by the Institutional Review Board of the pediatric hospital where the study was carried out and the parent pilot trial was registered on clinicaltrials.gov (NCT#01981096).
Strength and Biomechanical Testing Procedures
Assessments were conducted by trained master’s level biomechanists and an exercise physiologist, and they consisted of measurement of isokinetic hip and knee strength, dynamic postural stability, and 3-D motional analysis of functional tasks. 3-D motional analyses were conducted on a standardized drop vertical jump task.
Strength
Both isokinetic knee strength and hip abduction strength were assessed with the Biodex System II (Biodex Medical Systems Inc., Shirley, NY). For knee strength, participants sat in the dynamometer chair with their hips at 90° and their knees aligned with the rotation axis of the machine. A lower leg was strapped to the dynamometer arm 2 inches above the lateral malleolus. Starting at 90° knee flexion, participants extended their knee to full extension and actively flexed the knee back to the starting position at an isokinetic speed of 300°/second. Participants completed a series of exercises and were asked to exert “maximal effort.” through 10 continuous repetitions on each leg. For hip abduction strength, participants stood facing the dynamometer head, aligning the center of their hip with the axis of rotation. The testing leg was strapped to the dynamometer arm just above the knee. Participants kicked their leg out to the side, with the testing speed set to 120°/second. Peak torque normalized to body mass (Nm/kg) of each extension and flexion was recorded.37 Strength scores were based on the average peak torque across the 10 repetitions of each leg to create an overall strength score normalized to body mass (Nm/kg) for each motion (i.e., knee extension, flexion, hip abduction strength).
Dynamic postural stability
To assess stability and balance, the Star Excursion Balance Test38,39 was used. To perform this test, participants stood on one foot at the center of a grid and performed a maximal reach with the non-stance leg in the anterior, posteromedial, and posterolateral direction while maintaining balance on their single leg. The most distal reach distance of the foot in all three directions was measured in centimeters. The process was then repeated while standing on the other leg. Composite scores were calculated for each participant by dividing the sum of the maximal reach in the anterior (A), posteromedial (PM) and posterolateral (PL) directions by three times the limb length (LL) of the individual, and then multiplying by 100.40,41
Motion Capture
Functional performance assessments were conducted utilizing a 10-camera real-time high-speed 3-D motion capture and analysis system (Raptor-E; Motion Analysis Corp., Santa Rosa, CA) sampling at 240 Hz, with participants wearing 43 retroreflective markers (3 markers per segment) placed on standardized locations.23,42 Placements included bilateral lower extremities (e.g., foot, shank, and thigh) and trunk (e.g., pelvis and thorax). Additionally, ground reaction forces during movement were measured using force plates embedded into the floor sampling at 1,200 Hz (AMTI; Advanced Medical Technology, Inc., Watertown, MA). Complete methods for biomechanical and strength assessments and data processing are presented elsewhere 23,33 and are summarized below.
Drop Vertical Jump (DVJ).
Participants began the DVJ by standing on a 31-cm tall box with their feet shoulder-width apart. They were then instructed to drop off the box with both feet simultaneously and, immediately upon landing on the force plates, to perform a vertical jump with maximal effort to reach an overhead target. This procedure was modeled by the exercise physiologist and, after watching the procedure demonstrated, participants completed practice trials (typically 2–3) until they were comfortable with the test. Three trials were recorded for each participant.
Motion Capture Preprocessing.
Basic kinematic and kinetic data were computed. Cardan joint angles (kinematics) and internal joint moments of force (kinetics) were calculated for the DVJ assessment in Visual3D (C-Motion, Inc., Germantown, MD) and exported to Matlab (Mathworks; Natick, MA) for data reduction and analysis. For the DVJ, the stance phase, defined as the period of time between initial contact with the force plate to toe-off, was normalized to 101 data points (representing 0–100% of stance). Peak values during the stance phases the DVJ were extracted and averaged across trials and sides for each participant. Kinematic and kinetic waveforms were also plotted to illustrate changes in both joint angles and rotation (kinematics) and torque on those joints (kinetics) throughout the complete DVJ motion. The stance phase is depicted within the waveforms for the DVJ.
CBT and FIT Teens Interventions
After baseline assessments, participants were randomized to receive either CBT only (without any physical exercise component) or FIT Teens (CBT + neuromuscular exercise training). The components of the CBT protocol used in each group were based on our published clinical pilot trial modified for group-based delivery over 16 sessions9. The full content of the FIT Teens program has also been fully described in a previous publication.34 Briefly, sessions for each treatment arm were conducted over an 8-week period (twice per week) and consisted of 90-minute group-based sessions, co-led by a psychology post-doctoral fellow/pain psychologist and an exercise physiologist. In the CBT group, the exercise physiologist participated by reinforcing practicing of coping skills, reviewing homework completion, and conducting in-group activities. Participants were taught a variety of pain coping skills including pain education, relaxation skills, distraction, activity pacing, problem solving, and modifying negative and catastrophic thoughts about pain. While participants in the CBT-only group were encouraged to increase their participation in daily activities as part of the CBT intervention, they were not specifically instructed to engage in physical exercise. The FIT Teens intervention consisted of approximately 45 minutes of CBT, in which participants were taught the same skills as the CBT-only group but in an abbreviated format, and 45 minutes devoted to neuromuscular training.
For the FIT Teens group, CBT skills were slightly modified to integrate with the neuromuscular training component to demonstrate in-vivo application of coping skills. The neuromuscular training component of the program was based on a previously developed resistive training protocol used in injury prevention research43 and specially designed to reduce delayed muscle soreness by gradually increasing the complexity of muscle actions. In this component, exercises are tailored to each participant’s ability, allowing participants to build confidence and mastery of the exercise before moving on to more complex ones. These exercises include building from basic isometric “hold” exercises, to concentric “muscle shortening” exercises, to eccentric “muscle lengthening” exercises, and finally the full range of motion for “functional movement” (see Figure 1 for example of exercise progression and elsewhere for the full list of exercises and progressions).43 Exercises were conducted using combinations of a TRX Suspension Trainer (Fitness Anywhere LLC) to provide assistance to participants during movement, a BOSU ® Balance Trainer to encourage improved balance and coordination while completing movements, stability balls, and floor-based exercises. Throughout the training, the exercise physiologist educated participants on the role of each of the exercises and how they would be useful for the functional movements that are exhibited in daily activities (walking, jumping, bending, etc.). In addition to the progressive levels of exercise, participants were given specific instruction and feedback regarding appropriate muscle activation, form, technique, and body positioning. This not only ensured appropriate utilization of muscle groups associated with each movement, but also safeguarded against injury. Instructions frequently focused on maintaining proper lower extremity alignment with an emphasis on increasing proximal control through the hip joint and trunk, which can improve biomechanics through stabilization of the thigh and knee joints.44,45
Participants in both groups (CBT and FIT) completed post-treatment assessments on strength, balance and movement biomechanics within a week of completing the 8-week intervention.
Statistical Analysis
Rationale for the sample size for the overall pilot trial was based upon effect sizes from previous intervention studies in JFM, accounting for planned attrition (25%). The strength and biomechanics measures of this secondary analysis are entirely novel for this population and were secondary/exploratory outcomes of the study; therefore, power analyses were not available for these measures and analyses conducted in this study are largely exploratory. All data were entered and analyzed in SPSS (Version 24) statistical software. Statistical analyses are similar to those presented in our previous work.23,33 Descriptive statistics (means, standard deviations, and confidence intervals) on all biomechanics, strength and postural stability assessments were computed at pre- and post-treatment. Biomechanics measurements are based upon peak-values across the time-series of data, such that maximum values are captured, as in other studies.27 Kinematic and kinetic time-series plots for CBT and FIT Teens showing mean values with shaded areas of overlapping standard error are presented for each group, pre and post treatment, across the stance phase of the DVJ. Within group difference across treatment are explored by calculating 95% Confidence Intervals for the mean difference scores pre to post test.
RESULTS
Demographics and Baseline Characteristics
Per the primary outcomes31 of this pilot trial, 90 adolescents were screened for eligibility, and 50 of those were excluded either due to not meeting criteria (n=10), declining participation (n=28), or being lost to follow-up (n=12). Forty adolescents with JFM (M = 15.33 years, SD = 1.526; 90% female; 96% Caucasian) were randomized to either the CBT or FIT Teen’s Groups (n=20 per group). Thirty-six of these participants completed the study (nCBT = 19; nFIT Teens = 17).31 In the CBT group, one individual dropped out after being randomized to the CBT condition, and in the FIT Teens group, one individual withdrew due to parental health complications and two withdrew due to unknown reasons. At their baseline assessment, adolescents reported levels of disability in the moderate range on the Functional Disability Inventory36 (M = 25.58, SD = 7.78) and pain levels in the moderate-severe range using a pain Visual Analog Scale46 (M = 6.48, SD = 1.40). The two treatment groups did not differ in these measures at baseline. All 36 participants completed strength and balance testing at baseline and post-treatment. However, at post-treatment, 6 participants who participated as part of one CBT group did not complete the motion assessment due to unavailability of the 3-D motion capture system for facilities upgrades in the Division of Sports Medicine. Additionally, DVJ data for one FIT Teens participant could not be analyzed due to poor marker placement. Hence data for the DVJ task were only available for 16 FIT Teens participants 14 CBT participants.
Strength and Balance Descriptive Analyses, and Within Group Changes
When within group changes were evaluated, by examining confidence intervals and identifying intervals that were non-overlapping with zero, we found that the FIT Teens group demonstrated pre-post treatment improvements in knee extension strength (MDiff = 0.07 N/kg) and hip abduction strength (MDiff = 0.10 N/kg), while the CBT group did not (see Table 1). No changes were seen in balance.
Table1 –
Descriptive Statistics: Strength, Balance, Kinematic, and Kinetic Values
| CBT | FIT Teens | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | |||||||
| n | M (SD) | n | M (SD) | MDiff (SD) | MDiff CI95% | n | M (SD) | n | M (SD) | MDiff (SD) | MDiff CI95% | |
| Strength and Balance | ||||||||||||
| Balance | 20 | 82.84 (11.61) | 19 | 82.33 (8.43) | −0.24 (12.89) | (−6.46, 5.97) | 20 | 75.36 (10.92) | 17 | 79.54 (7.17) | −3.62 (11.61) | (−9.59, 2.35) |
| Knee Extensionᵻ | 19 | 0.97 (0.20) | 19 | 1.00 (0.19) | −0.03 (0.09) | (0.02, −0.08) | 20 | 0.98 (0.24) | 17 | 1.05 (0.23) | −0.10 (0.16) | (−0.18, −0.02) |
| Knee Flexionᵻ | 19 | 0.623 (0.17) | 19 | 0.66 (0.17) | −0.04 (0.15) | (−0.11, 0.03) | 20 | 0.62 (0.16) | 17 | 0.65 (0.14) | −0.02 (0.15) | (−0.10, 0.06) |
| Hip Strengthᵻ | 20 | 0.69 (0.22) | 19 | 0.68 (0.18) | 0.02 (0.16) | (−0.06, 0.10) | 19 | 0.65 (0.21) | 17 | 0.75 (0.26) | −0.10 (0.19) | (−0.20, −.001) |
| Drop Vertical Jump – Peak Kinematics* | ||||||||||||
| Hip Flexion | 14 | 53.14 (11.68) | 13 | 48.03 (12.29) | 4.30 (11.76) | (−2.81, 11.40) | 20 | 48.91 (11.81) | 16 | 50.68 (13.16) | −2.14 (7.47) | (−6.13, 1.83) |
| Hip Adduction | 14 | 2.35 (2.94) | 13 | 2.56 (3.26) | −0.18 (2.49) | (−1.69, 1.32) | 20 | 2.44 (1.07) | 16 | 2.15 (3.35) | 0.37 (1.84) | (−0.61, 1.35) |
| Hip Internal Rotation | 14 | 0.58 (5.50) | 13 | −0.59 (7.63) | 1.17 (3.90) | (−1.19, 3.53) | 20 | 0.81 (6.55) | 16 | −2.78 (6.33) | 2.91 (3.48) | (1.06, 4.77) |
| Knee Flexion | 14 | −78.18 (7.79) | 13 | −76.79 (3.34) | −1.21 (7.70) | (−5.87, 3.44) | 20 | −77.35 (11.69) | 16 | −77.05 (10.27) | −0.42 (5.13) | (−3.16, 2.31) |
| Knee Abduction | 14 | −11.98 (5.87) | 13 | −11.92 (6.51) | 0.04 (3.32) | (−1.97, 2.05) | 20 | −14.04 (8.64) | 16 | −14.67 (6.92) | 0.91 (3.83) | (−1.13, 2.95) |
| Knee Internal Rotation | 14 | 4.95 (5.99) | 13 | 6.02 (6.42) | −0.98 (3.44) | (−3.06, 1.10) | 20 | 6.57 (6.49) | 16 | 6.3 (5.69) | 0.11 (3.89) | (−1.97, 2.18) |
| Drop Vertical Jump – Peak Kinetics** | ||||||||||||
| Hip Flexion | 14 | 1.38 (0.36) | 13 | 1.31 (0.23) | 0.004 (0.11) | (−0.07, 0.07) | 20 | 1.37 (0.35) | 16 | 1.26 (0.29) | 0.03 (0.28) | (−0.12, 0.18) |
| Hip Adduction | 14 | 0.6 (0.19) | 13 | 0.62 (0.13) | −0.02 (0.14) | (−0.10, 0.07) | 20 | 0.68 (0.28) | 16 | 0.67 (.19) | 0.009 (0.23) | (−0.11, 0.12) |
| Hip Internal Rotation | 14 | 0.43 (0.12) | 13 | 0.40 (0.07) | 0.01 (0.10) | (−0.05, 0.07) | 20 | 0.42 (0.11) | 16 | 0.46 (0.14) | −0.07 (0.12) | (−0.13, −0.001) |
| Knee Flexion | 14 | −1.67 (0.29) | 13 | −1.73 (0.18) | 0.07 (0.18) | (−0.04, 0.18) | 20 | −1.92 (0.80) | 16 | −1.71 (0.36) | −0.22 (0.70) | (−0.59, 0.16) |
| Knee Abduction | 14 | −0.429 (0.23) | 13 | −0.43 (0.25) | 0.001 (0.10) | (−0.06, 0.06) | 20 | −0.55 (0.35) | 16 | −0.48 (.22) | −0.05 (0.25) | (−0.18, 0.09) |
| Knee Internal Rotation | 14 | 0.01 (0.04) | 13 | 0.01 (0.05) | 0.001 (0.02) | (−0.01, 0.02) | 20 | 0.12 (0.07) | 16 | 0.10 | 0.003 (0.07) | (−0.03, 0.04) |
Strength measures standardized to N/kg;
Peak kinematic values in degrees for participants in the CBT and FIT Teens groups during a drop vertical jump task.
Average peak kinetic values for participants in the CBT and FIT Teens groups during a drop vertical jump task in newton-meters per kilogram (Nm/kg). All available data are included in pre-assessment values, but analyses were completed only on those who completed the assessments.
Functional Performance
Peak Value Comparisons:
No pre-post treatment changes in hip or knee kinematics or kinetics were found within the CBT group. However, FIT Teens participants exhibited increases in hip internal rotation (MDiff = 3.59 degrees) and peak hip internal hip rotation moment (MDiff = 0.04 Nm/kg) (see bolded values in Table 1). No changes were observed in peak knee kinematics or kinetics.
Time-Series Plots:
Qualitative visual evaluation of the kinematic time-series plots shows differences in treatment response between the CBT and FIT Teens groups, as demonstrated by non-overlapping standard error. While the CBT group did not demonstrate significant changes pre to post (represented by non-overlapping standard errors), in hip (Figure 2) or knee (Figure 3) movement, the FIT Teens group demonstrated greater external hip rotation throughout the DVJ (Figure 2), particularly at the beginning of the stance phase. Specifically, the FIT Teens group exhibited reduced hip adduction and increased hip external rotation (Figure 2) throughout the movement noted by non-overlapping error bars in the transverse plane at the beginning (i.e., 5–10% stance) and end (i.e., 70–100% stance) of the motion. Further, the FIT Teens group showed decrease hip adduction during the middle of the stance, as shown by very slight overlap in standard error. Kinetic plots demonstrate similar relationships, most notably with increased hip moments in the frontal and transverse planes in the FIT Teens group (Figure 4). No notable changes were observed in knee kinematics or kinetics (Figure 5) for either treatment group.
Figure 2 –
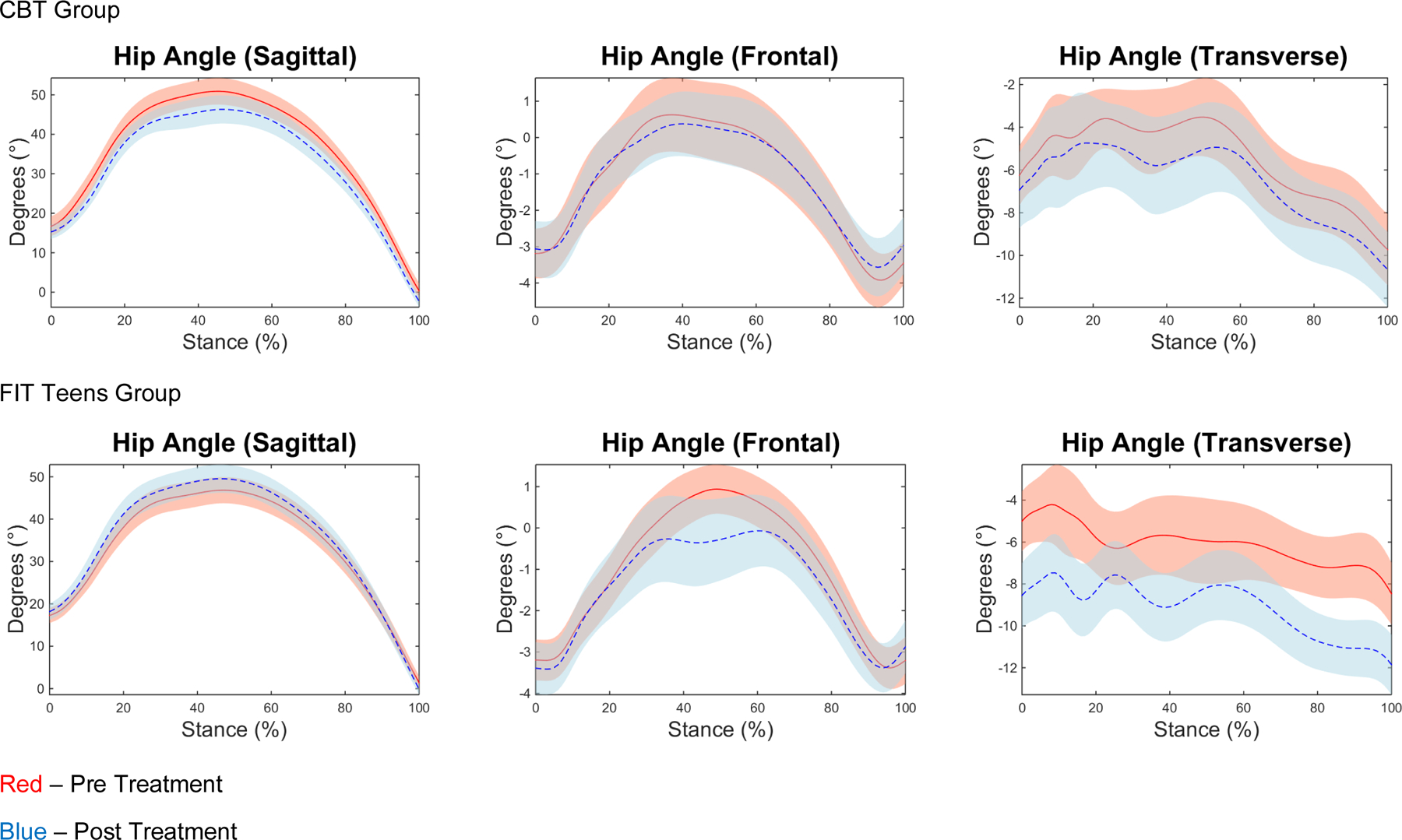
Hip Kinematic time-series plots for CBT and FIT Teens, Pre vs. Post Assessment
Figure 3 –
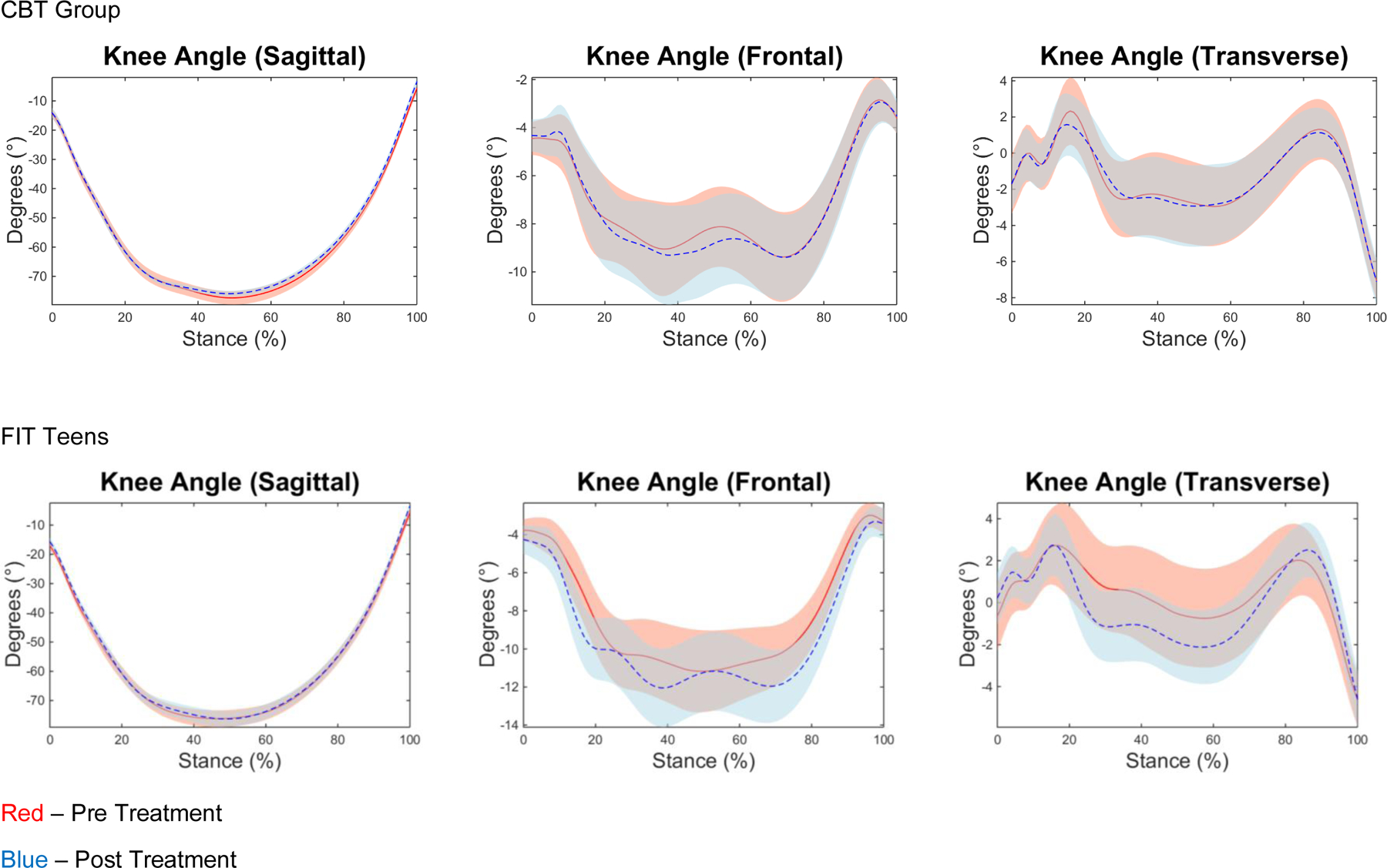
Knee Kinematic time-series plots for CBT and FIT Teens, Pre vs. Post Treatment.
Figure 4 –
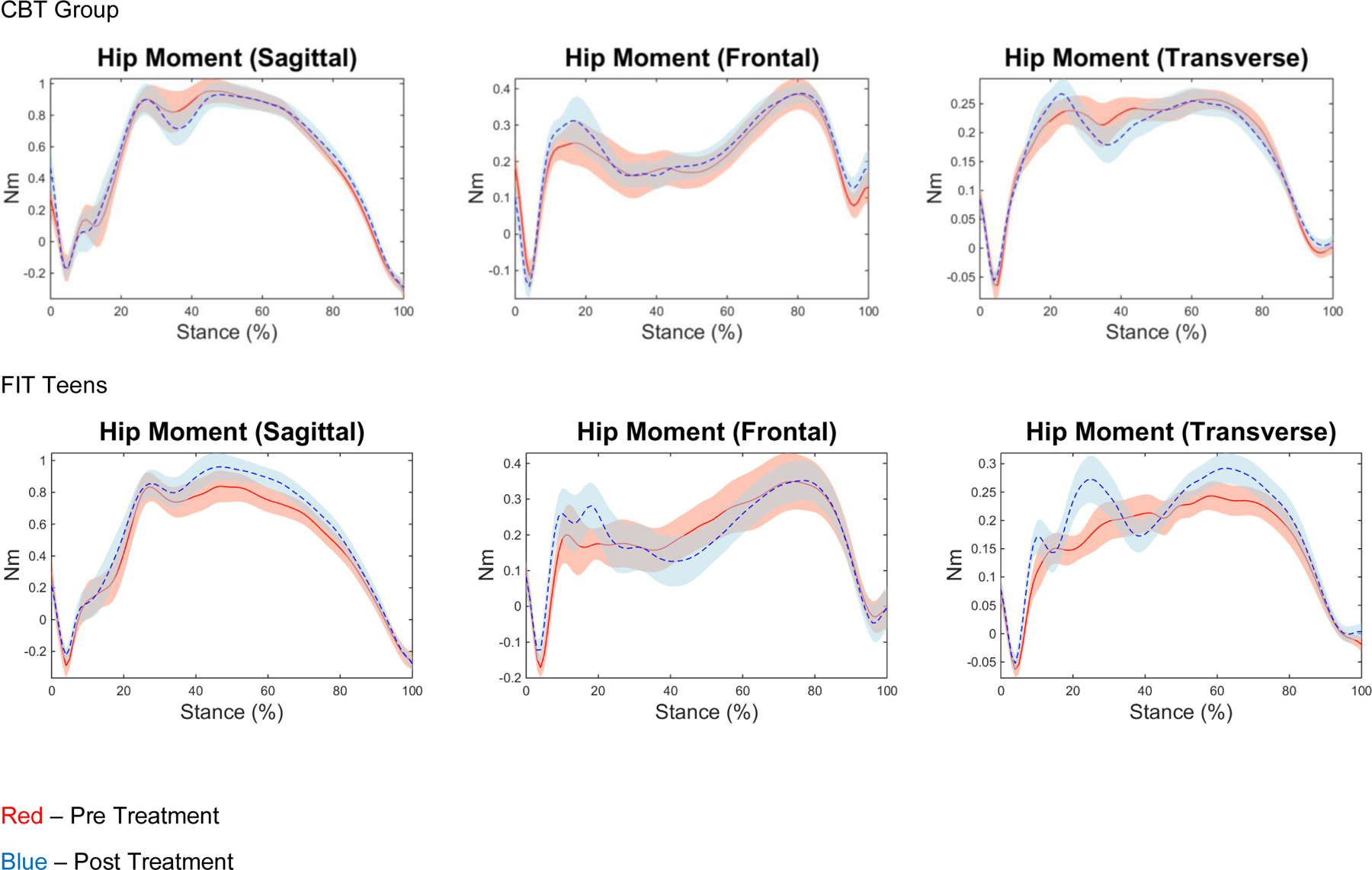
Hip Kinetic time-series plots for CBT and Fit Teens, Pre vs. Post Treatment
Figure 5 -.

Knee Kinetic time-series plots for CBT and FIT Teens, Pre vs. Post Treatment
DISCUSSION
To our knowledge, this is one of the first studies to take a technologically sophisticated approach to assessment of movement biomechanics in a chronic musculoskeletal pain condition (JFM) and evaluate what changes are possible with a combined CBT and neuromuscular exercise training program that has been specifically designed to improve fundamental movement abilities. Results of this pilot trial show promising findings with respect to objective improvements in how the body moves and its ability to absorb and exert force (i.e., biomechanics, movement competence) after treatment. These findings complement previously published primary findings of the pilot trial, which demonstrated reduced patient-reported pain and disability following the FIT Teens intervention and indicate that these improvements are accompanied by objectively measured improvements in movement biomechanics. Increased strength and confidence in movement could set the stage for JFM patients being more prepared and motivated to engage in moderate to vigorous physical exercise, which has been linked to reduced pain levels in fibromyalgia, and should allow for safer and more stable movements for functional daily living activities (e.g. sitting, walking, stair climbing, and picking up or lifting objects).33
Consistent with previous pilot work,6,23 the most prominent pre-post changes were in hip-related biomechanics that were noted to be most affected by JFM. Increases in hip neuromuscular recruitment, particularly in the transverse planes (Figures 2&4), along with evidence of kinematic improvements (i.e., improved hip and knee joint placement and orientation in the frontal and transverse planes) in the FIT Teens group, represent a shift in movement to more neutral alignment of the thighs and lower extremities upon landing and during toe-off, versus pre-treatment assessment during which their knees and thighs shifted inward (medially) in a “knock-kneed” position (Figures 2&3). Taken together, these early findings demonstrate changes in hip position and movement associated with greater knee stability; which indicates that the lower extremities are better positioned to efficiently absorb and exert force during the DVJ, with the likely result of increased muscular absorption (and exertion) of forces by the hips. These types of changes in movement have previously been related to reduced injuries in adolescents engaged in athletics.47 A central rationale underlying the use of neuromuscular training is that through gradual and graded training, movement competence is increased and injury risk is decreased while engaged in functional and everyday tasks. The targeted exercises of FIT Teens therefore appeared to be having the desired effect. After completion of treatment, the FIT Teens participants’ biomechanics, particularly their hip and knee internal rotation, began to more closely resemble movement patterns exhibited by healthy female adolescents.23
Movement based therapies have shown effectiveness on pain reduction in chronic musculoskeletal pain.48 However, specialized neuromuscular training offers advantages over other complementary techniques in that it emphasizes fundamental movements and strength building while minimizing the potential for delayed onset muscle soreness. Importantly, the specialized neuromuscular training program utilized in FIT Teens was very well-tolerated by the participants and no adverse events related to treatment were reported. FIT Teens was specifically developed for adolescents with JFM based on movement competence deficits we identified in initial pilot work27 and iteratively developed and modified based on feedback from adolescents themselves about all aspects of the program.34 The use of sophisticated motion capture technology allowed a much more fine-grained and detailed assessment of changes in movement biomechanics. This technology shows great potential as a valuable research tool in the study of musculoskeletal pain.
Limitations and Future Directions
This study includes several strengths, including the use of objective measures of biomechanics and increased methodological rigor over previous literature23 through its use of a comparison group (i.e., CBT-only); however, as this was a small pilot trial, there are several limitations that warrant future consideration. As this study presents secondary outcomes for a pilot trial that was powered to detect changes in different outcomes (pain and disability),31 the small sample size in this pilot trial, which had some unequal data loss between the treatment groups, had limited power to find statistically significant between-group differences across the measures. Much of this data loss was associated with a technology upgrade to the 3D motion capture system, during which motion capture data could not be collected. In order to prevent similar data loss in subsequent trials, any potential technology upgrades will occur between groups. Also, we encountered some challenges with marker placement due to high Body Mass Index and discomfort with marker placement. These are being kept in mind for future studies and have been written into our standard operating procedures. In combination with the fact that this study tested a neuromuscular training program, results may not be generalizable to other integrated programs that use other forms of exercise training. Additionally, as this is a small pilot study, we also report on analyses that may or may not survive replication – however, given the significant pre-post changes and novelty of 3D motion analyses in this clinical population, these are important results to include for consideration in future studies. Replication with larger sample sizes is clearly needed to more rigorously evaluate strength and biomechanical changes following FIT Teens and CBT. This must entail careful coordination with multiple sites and biomechanics labs, in order to improve and maintain high quality data collection (e.g., marker placement), and ensure that all needed equipment is in place and available for use for the duration of the study. Also, this study does not provide information on how much CBT is maximally beneficial with neuromuscular exercise training. While the two interventions are matched for time (90 minutes per session), the CBT group received twice as much CBT exposure than the FIT Teens group – thus, the CBT only group may not serve as a true control for FIT Teens.
Investigating objective biomechanics in chronic pediatric musculoskeletal pain is still a new for the field. This study prompts several areas of additional future work, including advanced analytics, and the comparative effects of other forms of physical training (such as aerobic exercise) on biomechanics. The power of biomechanics data is largely untapped, as each movements consists of thousands of data points that are collected repeatedly in a time-series fashion. As analytic techniques improve, big-data and machine learning approaches may be utilized to evaluated time-series biomechanics data in a longitudinal fashion, and to better understand how movement patterns may differ in clinical samples (e.g. JFM) compared to normative populations.
This study only evaluates biomechanical changes as a result of neuromuscular exercise training and does not include comparisons to other exercise modalities (e.g., physical therapy, aerobic activity, yoga) which should be pursued through future studies. Additionally, other studies should evaluate how biomechanics improve relative to other well described treatment outcomes such as reported pain and functional disability, the required amount of biomechanical improvement to affect functional and pain outcomes, and determining the clinical impact of improved biomechanics on functional outcomes (e.g., moderate to vigorous physical activity participation). Additionally, further study is needed on the maintenance of treatment gains for movement biomechanics. Follow-up time points are needed to determine whether treatment gains continue to be made after conclusion of the program. The utility of periodic maintenance/booster sessions following the active treatment phase could also be explored as means to maintain or augment outcomes.8,16
Conclusion
The integrated delivery of psychological coping skills and training in proper body biomechanics via the FIT Teens program has been shown to improve pain coping and reduce functional impairment and pain. This study shows promising additional benefits in objectively measured biomechanics. Specifically, the FIT Teens program may afford benefits of improved strength and biomechanics that were not apparent in pain-focused CBT only. Improvement in movement competence is a critical first step towards preparation of individuals for successful engagement in increased physical activity and regular exercise, a core treatment recommendation for patients with chronic musculoskeletal pain. Given the poor engagement and maintenance of regular exercise in JFM among youth, continued efforts are needed to develop tailored programs such as FIT Teens to enhance confidence and motivation for physical activity and exercise.
Acknowledgements:
This study was conducted with funding support from the NIH/National Institutes of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Grants R21AR063412 and K24AR056687 (PI: Kashikar-Zuck).
REFERENCES
- 1.Brattberg G Do pain problems in young school children persist into early adulthood? A 13-year follow-up. European Journal of Pain. 2004;8(3):187–199. [DOI] [PubMed] [Google Scholar]
- 2.Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014;14(10):2299–2319. [DOI] [PubMed] [Google Scholar]
- 3.Clark P, Burgos-Vargas R, Medina-Palma C, Lavielle P, Marina FF. Prevalence of fibromyalgia in children: A clinical study of Mexican children. Journal of Rheumatology. 1998;25(10):2009–2014. [PubMed] [Google Scholar]
- 4.Gerloni V, Ghirardini M, Fantini F. Assessment of nonarticular tenderness and prevalence of primary fibromyalgia syndrome in healthy Italian schoolchildren. Arthritis and Rheumatism. 1998;41(9):1405. [Google Scholar]
- 5.Kashikar-Zuck S, Lynch AM, Slater S, Graham TB, Swain NF, Noll RB. Family factors, emotional functioning, and functional impairment in juvenile fibromyalgia syndrome. Arthritis Rheum. 2008;59(10):1392–1398. [DOI] [PubMed] [Google Scholar]
- 6.Tran ST, Guite JW, Pantaleao A, et al. Preliminary outcomes of a cross-site cognitive-behavioral and neuromuscular integrative training intervention for juvenile fibromyalgia. Arthritis Care & Research. 2016. [DOI] [PMC free article] [PubMed]
- 7.Kashikar-Zuck S, Allen R, Noll R, et al. Anxiety and depressive symptoms in adolescents with juvenile fibromyalgia and their mothers. The Journal of Pain. 2005;6(3 Suppl):31. [Google Scholar]
- 8.Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity in adults with fibromyalgia: results at follow-up. J Clin Rheumatol. 2011;17(2):64–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kashikar-Zuck S, Ting TV, Arnold LM, et al. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: A multisite, single-blind, randomized, controlled clinical trial. Arthritis Rheum. 2012;64(1):297–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sil S, Arnold LM, Lynch-Jordan A, et al. Identifying treatment responders and predictors of improvement after cognitive-behavioral therapy for juvenile fibromyalgia. PAIN®. 2014. [DOI] [PMC free article] [PubMed]
- 11.Kashikar-Zuck S, Flowers SR, Strotman D, Sil S, Ting TV, Schikler KN. Physical activity monitoring in adolescents with juvenile fibromyalgia: findings from a clinical trial of cognitive-behavioral therapy. Arthritis Care Res (Hoboken). 2013;65(3):398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eccleston C, Palermo TM, Williams AC, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2014;5:CD003968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherry DD, Brake L, Tress JL, et al. The Treatment of Juvenile Fibromyalgia with an Intensive Physical and Psychosocial Program. The Journal of Pediatrics. 2015;167(3):731–737. [DOI] [PubMed] [Google Scholar]
- 14.American Pain Society. Guideline for the management of fibromyalgia syndrome pain in adults and children. Glenview, IL: American Pain Society; 2005. [Google Scholar]
- 15.Hooten WM, Qu W, Townsend CO, Judd JW. Effects of strength vs aerobic exercise on pain severity in adults with fibromyalgia: a randomized equivalence trial. Pain. 2012;153(4):915–923. [DOI] [PubMed] [Google Scholar]
- 16.Gowans SE, deHueck A. Effectiveness of exercise in management of fibromyalgia. Curr Opin Rheumatol. 2004;16(2):138–142. [DOI] [PubMed] [Google Scholar]
- 17.Kashikar-Zuck S, Flowers SR, Verkamp E, et al. Actigraphy-based physical activity monitoring in adolescents with juvenile primary fibromyalgia syndrome. J Pain. 2010;11(9):885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kop WJ, Lyden A, Berlin AA, et al. Ambulatory monitoring of physical activity and symptoms in fibromyalgia and chronic fatigue syndrome. Arthritis Rheum. 2005;52(1):296–303. [DOI] [PubMed] [Google Scholar]
- 19.Korszun A, Young EA, Engleberg NC, Brucksch CB, Greden JF, Crofford LA. Use of actigraphy for monitoring sleep and activity levels in patients with fibromyalgia and depression. J Psychosom Res. 2002;52(6):439–443. [DOI] [PubMed] [Google Scholar]
- 20.Jones K, King L, Mist S, Bennett R, Horak F. Postural control deficits in people with fibromyalgia: a pilot study. Arthritis research & therapy. 2011;13(4):R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nijs J, Roussel N, Van Oosterwijck J, et al. Fear of movement and avoidance behaviour toward physical activity in chronic-fatigue syndrome and fibromyalgia: state of the art and implications for clinical practice. Clin Rheumatol. 2013;3:3. [DOI] [PubMed] [Google Scholar]
- 22.Rabbitts JA, Holley AL, Karlson CW, Palermo TM. Bidirectional associations between pain and physical activity in adolescents. The Clinical Journal of Pain. 2014;30(3):251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sil S, Thomas S, DiCesare C, et al. Preliminary Evidence of Altered Biomechanics in Adolescents With Juvenile Fibromyalgia. Arthritis care & research. 2015;67(1):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hechler T, Dobe M, Damschen U, et al. The Pain Provocation Technique for Adolescents with Chronic Pain: Preliminary Evidence for Its Effectiveness. Pain Medicine. 2010;11(6):897–910. [DOI] [PubMed] [Google Scholar]
- 25.Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18(4):251–261. [DOI] [PubMed] [Google Scholar]
- 26.Simons LE, Kaczynski KJ. The Fear Avoidance model of chronic pain: examination for pediatric application. J Pain. 2012;13(9):827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sil S, Thomas S, DiCesare C, et al. Preliminary evidence of altered biomechanics in adolescents with juvenile fibromyalgia. Arthritis Care Res (Hoboken). 2015;67(1):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. The American journal of sports medicine. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study. The American journal of sports medicine. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 30.Tran ST, Guite JW, Pantaleao A, et al. Preliminary Outcomes of a Cross-Site Cognitive-Behavioral and Neuromuscular Integrative Training Intervention for Juvenile Fibromyalgia. Arthritis Care Res (Hoboken). 2017;69(3):413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kashikar-Zuck S, Black WR, Pfeiffer M, et al. Pilot Randomized Trial of Integrated Cognitive-Behavioral Therapy and Neuromuscular Training for Juvenile Fibromyalgia: The FIT Teens Program. J Pain. 2018. [DOI] [PMC free article] [PubMed]
- 32.Myer GD, Faigenbaum AD, Chu DA, et al. Integrative training for children and adolescents: techniques and practices for reducing sports-related injuries and enhancing athletic performance. Phys Sportsmed. 2011;39(1):74–84. [DOI] [PubMed] [Google Scholar]
- 33.Tran ST, Thomas S, DiCesare C, et al. A pilot study of biomechanical assessment before and after an integrative training program for adolescents with juvenile fibromyalgia. Pediatric Rheumatology. 2016;14(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kashikar-Zuck S, Tran ST, Barnett K, et al. A Qualitative Examination of a New Combined Cognitive-behavioral and Neuromuscular Training Intervention for Juvenile Fibromyalgia. Clin J Pain. 2015;32(1):70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ting TV, Barnett K, Lynch-Jordan A, Whitacre C, Henrickson M, Kashikar-Zuck S. 2010 American College of Rheumatology Adult Fibromyalgia Criteria for Use in an Adolescent Female Population with Juvenile Fibromyalgia. The Journal of pediatrics. 2016;169:181–187.e181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kashikar-Zuck S, Flowers SR, Claar RL, et al. Clinical utility and validity of the Functional Disability Inventory (FDI) among a multicenter sample of youth with chronic pain. Pain. 2011;152(7):1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brent JL, Myer GD, Ford KR, Paterno MV, Hewett TE. The effect of sex and age on isokinetic hip-abduction torques. Journal of sport rehabilitation. 2013;22(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gribble PA, Robinson RH, Hertel J, Denegar CR. The effects of gender and fatigue on dynamic postural control. Journal of sport rehabilitation. 2009;18(2):240. [DOI] [PubMed] [Google Scholar]
- 39.Gribble P, Hertel J, Denegar C. Chronic ankle instability and fatigue create proximal joint alterations during performance of the Star Excursion Balance Test. International journal of sports medicine. 2007;28(03):236–242. [DOI] [PubMed] [Google Scholar]
- 40.Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. J Pain. 2016;17(9 Suppl):T70–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Filipa A, Byrnes R, Paterno MV, Myer GD, Hewett TE. Neuromuscular training improves performance on the star excursion balance test in young female athletes. J Orthop Sports Phys Ther. 2010;40(9):551–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ford KR, Myer GD, Melson PG, Darnell SC, Brunner HI, Hewett TE. Land-Jump Performance in Patients with Juvenile Idiopathic Arthritis (JIA): A Comparison to Matched Controls. Int J Rheumatol. 2009;2009:478526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas SM, Sil S, Kashikar-Zuck S, Myer GD. Can Modified Neuromuscular Training Support the Treatment of Chronic Pain in Adolescents? Strength & Conditioning Journal. 2013;35(3):12–26. [Google Scholar]
- 44.Myer G, Brent J, Ford K, Hewett T. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. British journal of sports medicine. 2008;42(7):614–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myer GD, Chu DA, Brent JE, Hewett TE. Trunk and Hip Control Neuromuscular Training for the Prevention of Knee Joint Injury. Clinics in sports medicine. 2008;27(3):425–ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McGrath PJ, Walco GA, Turk DC, et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. The journal of pain : official journal of the American Pain Society. 2008;9(9):771–783. [DOI] [PubMed] [Google Scholar]
- 47.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. [DOI] [PubMed] [Google Scholar]
- 48.Mist SD, Firestone KA, Jones KD. Complementary and alternative exercise for fibromyalgia: a meta-analysis. Journal of pain research. 2013;6:247–260. [DOI] [PMC free article] [PubMed] [Google Scholar]


