Abstract
Meningeal tuberculoma is one of the most serious sites of tuberculosis. Its incidence varies depending on the geographical area, rare in Western countries and frequent in developing countries where it represents 5% to 10% of intracranial masses. We report the case of a 21-year-old male patient with no particular medical history from Africa and living in Europe for more than a year, is hospitalized for an isolated inaugural, generalized, afebrile seizure in whom the scanner and cerebral magnetic resonance imaging (MRI) revealed a meningeal mass with significant glove finger edema suggesting a primary brain tumor. Surgical excision and anatomopathological analysis of the excisional piece allowed the diagnosis of tuberculoma. Meningeal tuberculoma is a source of diagnostic error because its clinical and radiological expression can mimic a brain tumor. This is an etiology that should not be ignored in the face of a meningeal mass in any subject coming from or living in a region with a high endemic tuberculosis.
Keywords: Meningeal tuberculoma, Brain tumor, Scanner, MRI
Introduction
Intracranial meningeal tuberculomas represent one of the most serious sites of tuberculosis, their incidence varies depending on the context representing 0.2% of intracranial processes in Western countries and 5%-10% of intracranial masses in emerging countries [1].
TM preferentially affects the young subject.
Its meningeal pseudo-tumor form represents a diagnostic challenge, especially in the absence of immunosuppression and pulmonary involvement. We report a case of atypical clinical-radiological presentation in a 21-year-old patient and present the characteristic appearance of this pathology from a review of the literature.
Clinical observation
A 21-year-old man from Africa who has lived in Europe for a year is admitted to the emergency room with a generalized, isolated, rapidly resolving tonicoclonic convulsive seizure that resolves suddenly. The anamnesis revealed an absence of medical and surgical history and the presence of headaches. The physical examination was normal.
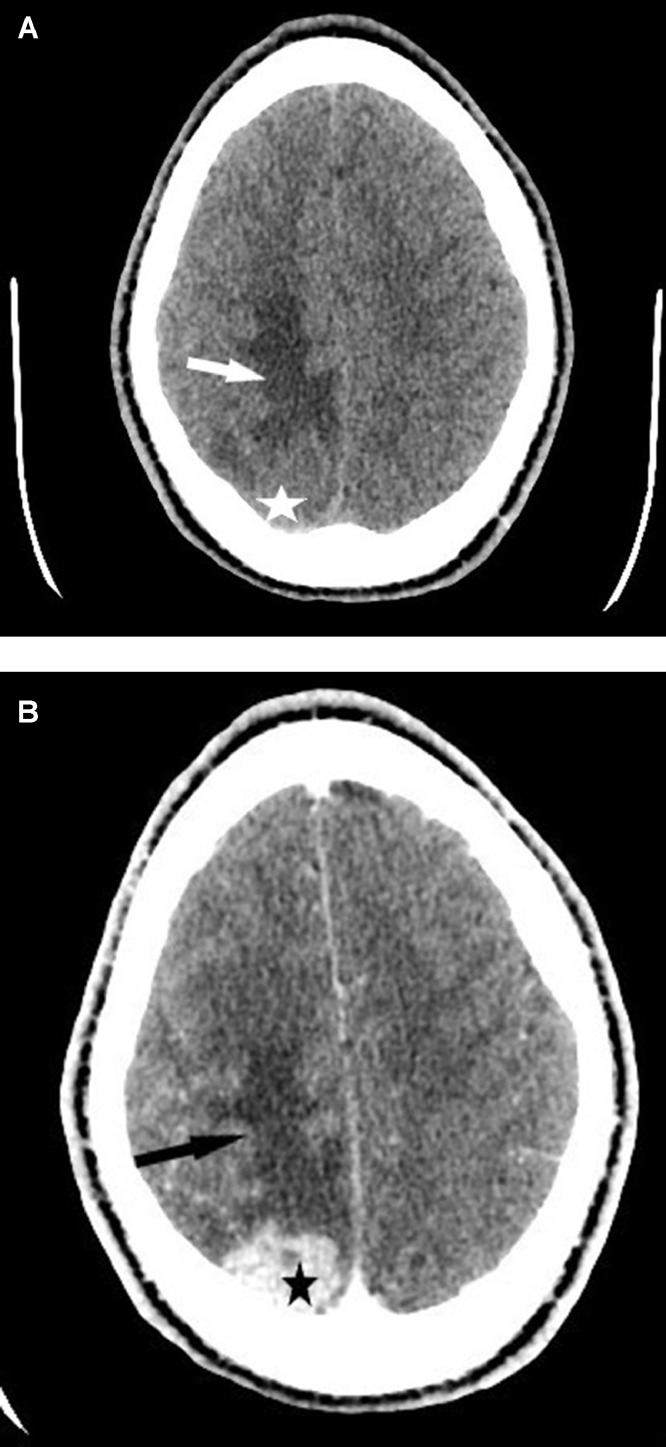
A brain encephalic scan without and with injection revealed an extra-axial right parietal tissue mass taking heterogeneous contrast at the late stage with glove-finger edema without bone reaction to the eye (Fig. 1).
Fig. 1.
Brain scan in axial section without injection of iodine contrast (A) and with injection (B) revealed an extra-axial right parietal tissue mass (star) taking contrast in a heterogeneous manner at the late stage with glove finger edema (arrow) without bone reaction facing it.
The complementary cerebral magnetic resonance imaging (MRI) confirmed the presence of this meningeal mass by specifying its base of insertion at the level of the internal graduate, its size of 32 × 17 × 25 mm, its polylobulated contours, its hypo perfused aspect compared to the adjacent brain parenchyma, and its heterogeneous contrast enhancement. with nonenhanced areas in its anterior part in the late phase, with a corticosubcortical edema in the glove finger pushing back the posterior horn of the right ventricular junction (Fig. 2).
Fig. 2.
Brain MRI. (A) Sagittal T1 slice: isosignal mass (star) surrounded by a hypointense edematous area. (B, T2 FLAIR axial slice): isointense mass (star) in the cortex surrounded by a hyperintense edematous area. (C, axial, coronal and sagittal T1 slices after injection of gadolinium).; meningeal mass of polylobulated outlines, intensely contrasting in heterogeneous ways (star) with nonenhanced areas in its anterior part (arrow head) with corticosubcortical edema (arrow) in a thimble pushing back the posterior horn of the right ventricular junction. (D) Spectrometry showed a peak in creatine choline with the presence of free lipid; without breakdown of other metabolites such as N-acetylaspartate and myoinositol.
The spectrometric analysis of this lesion revealed a peak in creatine choline with the presence of free lipid.
The characteristics of this mass suggest a tumor process such as a hemangiopericytoma or meningioma.
As part of an assessment of the extension of the disease, the patient had undergone a thoracoabdominipelvic scan and a positron emission tomography (PET) scan which did not show any notable abnormality apart from multiple lumboaortic lymphadenopathy (Fig. 3).
Fig. 3.
Thoracoabdominopelvic CT scan showing multiple coeliomesenteric abdominal lymphadenopathy (arrow).
The biological assessment (complete blood count (CBC), creactive protein (CRP), renal and hepatic assessment, lactate deshydrogenase (LDH), and human immunodeficiency virus (HIV) serology) performed was normal.
The patient had received symptomatic treatment with corticosteroids, anticonvulsants and analgesics.
Given the patient's young age, the peripheral, accessible (extra parenchymal) nature of this lesion and especially the extent of the edema, the patient had a direct surgical approach with a sample. Extemporaneous pathological examination was not clear between an inflammatory fibrotic lesion and a malignant meningioma. Complete tumor excision was performed and anatomopathological analysis of the operative specimen suggested tuberculous infection by the presence of epitheloid giganto granuloma with necrosis without proliferation of tumor cells.
The postoperative consequences were simple. The patient was put on anti-tuberculosis treatment with recovery. A control MRI was performed 5 days after the postoperative surgical procedure (Fig. 4) showing the poroencephalic cavity with reduction of the edema in relation to the total excision of the lesion with the cranial flap facing it.
Fig. 4.
Postoperative control brain MRI. (A) axial flair slice showing a reduction in edema on D5 postoperative (arrow). (B) T1 axial slice after injection of gadolinium showed the excisional encephalic pore cavity facing the postoperative flap (arrow head).
Discussion and literature review
Tuberculosis is a ubiquitous granulomatosis caused by the tubercle bacillus or koch bacillus. One of the most serious extrapulmonary locations is central nervous system involvement. The most common cerebromeningeal lesions are leptomeningitis and tuberculomas [1].
Transmission of the tubercle bacillus occurs primarily through the air. A tuberculoma is a mass of granulomatous tuberculosis tissue that has been contained and limited by the host's immune system. It presents itself as an intracranial process.
Tuberculoma results from hematogenous spread from a primary focus, usually pulmonary. Etiopathogenically, there is the absence of acid-fast bacilli in tuberculoma, the mycobacteria only have the role of triggering the cell-mediated immune reaction. Several tubers form and then merge to form an often lobulated mass, sometimes at a distance from the primary infection. This explains the absence of Koch's Bacillus (BK) in the samples and a normal chest radiological examination [1,2].
Consequently, the absence of manifestations on pulmonary imaging should not exclude the possible existence of cerebral tuberculomas. The computed tomography scan of our patient was strictly normal, with no lesions suggestive of tuberculosis.
On the other hand, multiple abdominal adenomegalies were discovered as part of the extension workup. This lymph node site could constitute the latent focus of tuberculosis in our patient.
Tuberculomas are clinically manifested most often by progressive, focused neurological damage associated with meningeal signs [2]. Isolated inaugural comitial crises of sudden onset as in our case are rarer. An alteration of consciousness can also be noted, ranging from obnubilation to deep coma [1,2], most of which progresses in a context of altered general condition and fever.
Tuberculomas occur frequently in immunocompromised patients with signs of tuberculosis infiltration [1,2]. Contrary to the usual clinical picture, our nonimmunocompromised patient presented exclusively with a sudden onset feverish attack and headache.
Tuberculoma can localize in any part of the neuraxis.
The preferential encephalic locations are intraparenchymal at the level of the periventricular white and gray matter junction and in the posterior fossa. They can affect the gray nuclei and the midbrain.
Very rarely the tuberculoma can be located in the meningeal spaces [3] as in our case. Our patient had an extraparenchymal meningeal lesion.
Tuberculoma is often solitary as in our case, but the multiple form is suggestive of tuberculosis etiology. It consists of a sowing of annular or nodular lesions often grouped in a focus, or of coalescing lesions giving a multiloculated lesion.
Pathologically, these lesions begin as a conglomerate of microgranuloma which merges to form a mature, noncaseified tuberculoma, followed by caseous necrosis [2].
Tuberculomas take on different aspects on the scanner and MRI depending on the stage of development and the presence or absence of caseous necrosis [3].
On the scanner, before injection of contrast product, tuberculoma presents as a solid-type lesion. After injection, the enhancement takes place either globally or in a ring. The presence of calcification, a central hypodense zone and a peripheral ring, called the Target sign, is pathognomonic of tuberculoma.
Noncaseified tuberculomas appear hypointense in T1 sequence and hypersignal in T2 sequence relative to the cerebral parenchyma and are intensely and homogeneously enhanced after injection of contrast product in T1 sequence.
The caseified tuberculomas with a solid center appear in hypo or iso signal in sequence in both T1 and T2 and are often associated with perilesional edema.
Caseified tuberculomas with a necrotic center appear in hypointense in the T1 sequence and in hyper signal in the T2 sequence. The injection of gadolinium finds a nodular or annular enhancement.
The diffusion and spectroscopy sequences are currently very useful for an early and noninvasive diagnostic approach of cerebral tuberculomas, especially in patients without systemic signs of tuberculosis.
They can distinguish tuberculomas from other primary or secondary infectious and tumor lesions [3], [4], [5].
The diffusion sequence highlights the tuberculoma as a hypersignal regardless of its T2 signal, with ADC numbers always low [3].
The spectroscopy can be useful to differentiate tuberculomas from other infectious lesions, particularly neurocysticercosis. Indeed, some authors have found an elevation of the lipid peak, an increase in choline and a decrease in N-acetylaspartate and creatinine compared to neurocysticercosis.
In our case, the mass could not be analyzed on the diffusion sequence because of its peripheral and juxtaosseous location in the brain, generating artefacts.
The spectrometry had shown a peak in creatine choline with the presence of free lipid; no peak in N-acetylaspartate. This aspect was not suggestive of tuberculoma and made suspect a primary tumor such as a menigioma or a hemangiopericytoma.
The tuberculoma most often takes on a nonspecific appearance which may suggest a tumor or inflammatory pathology [4].
The definitive diagnosis is based on the histological analysis of a stereotaxic biopsy sample or on a surgical excision piece.
The CSF or polymerase chain reaction is a useful and effective addition in the diagnosis of CNS tuberculosis. A combination of polymerase chain reaction and MRI can make it possible to make a diagnosis of neurotuberculosis [2,4].
Histological analysis of our patient's surgical excisional part made it possible to establish the diagnosis of tuberculoma while ruling out a tumor process.
Our patient had subsequently benefited from antituberculosis treatment with a favorable outcome.
Tuberculosis is a notifiable disease and well-codified medical treatment. Meningeal tuberculomas are treated like tuberculous meningitis according to the protocol (2SRHZ/7RH).
Conclusion
Meningeal tuberculoma is a form of tuberculosis whose clinical and radiological expression may mimic tumor lesion in immunocompetent subjects without associated systemic signs. Its diagnosis is based on anatomopathological examination and a stereotaxic biopsy sample or surgical excision of the brain lesion. Meningeal tuberculoma should be suspected in the presence of any solitary extraparenchymal brain lesions in a subject who has stayed in a region of highly endemic tuberculosis.
References
- 1.Muralidhar K., Katti MK. Pathogenesis, diagnosis, treatment, and outcome aspects of cerebral tuberculosis. Med Sci Monit. 2004;10:215–229. [PubMed] [Google Scholar]
- 2.Semlali S., El Kharras A., Mahi M., Hsaini Y., Benameur M., Aziz N. The imaging aspects of tuberculosis of the central nervous system. J Radiol. 2008;89:209–220. doi: 10.1016/s0221-0363(08)70396-2. [DOI] [PubMed] [Google Scholar]
- 3.Nouira K., Allani R., Abdelmalek R., Azaiez O., Laamari L., Benmessaoud M contribution of MRI in the diagnosis of tuberculosis of the central nervous system. La Presse Médicale 2008; 37: 634–642. [DOI] [PubMed]
- 4.Suslu H.T., Bozbuga M., Bayindir C. Cerebral tuberculoma mimicking high grade glial tumor. Turkish Neurosurg. 2011;21:427–429. doi: 10.5137/1019-5149.JTN.2947-10.0. [DOI] [PubMed] [Google Scholar]
- 5.Batra A., Tripathi R.P. Diffusion-weighted magnetic resonance imaging and magnetic resonance spectroscopy in the evaluation of focal cerebral tubercular lesions. Acta Radiol. 2004;45:679–688. doi: 10.1080/02841850410001169. [DOI] [PubMed] [Google Scholar]