Highlights
-
•
Embryonal rhabdomyosarcoma (RMS) of the cervix.
-
•
Subtypes of embryonal RMS.
-
•
Disease of adolescence.
-
•
Fertility preservation.
-
•
Lack of standard treatment.
Keywords: Embryonal rhabdomyosarcoma, Adolescence, Fertility preservation
Abstract
Embryonal rhabdomyosarcoma (RMS) of the cervix is a rare entity, encountered mainly in the first two decades of life. The literature consists mainly of case reports and few small case series, and no standard treatment guidelines are available. As this is a disease of adolescence, fertility preservation in well selected cases is of paramount importance. We report 3 cases of cervical RMS, in adolescents highlighting the clinical presentation, diagnosis and management.
1. Introduction
Embryonal rhabdomyosarcoma (RMS) is one of the types of rhabdomyosarcomas, which are tumours of the skeletal muscle. The other types are alveolar, pleomorphic, spindle cell/sclerosing RMS (Jayi, et al., 2014, Fletcher et al., 2013). The embryonal RMS is further sub divided into sarcoma botryoides and anaplastic variant. These are highly malignant tumours originating in the embryonal mesenchyme, and they account for 4–6% of all malignancies in children and young adults (Jayi, et al., 2014, Behtash et al., 2003). The genitourinary embryonal RMS most commonly affect the vagina (Jayi, et al., 2014, Sanders et al., 2008) and only 0.5% are found on the cervix (Jayi, et al., 2014, Kriseman et al., 2012, Sanders et al., 2008). These are usually seen in the second decade of life.
Management of cervical RMS ranges from radical surgery to a more fertility sparing conservative approach, along with chemotherapy and radiotherapy. However, as this is a rare tumour there is paucity of literature consisting mainly of case reports and series and treatment is still not standardized. We report 3 cases of embryonal RMS of the cervix in adolescents, along with their clinical presentation, histopathological features, diagnosis, management tailored to individual cases.
1.1. Case 1
Fifteen years old girl presented with complaints of continuous heavy vaginal bleeding for 10 months, not responding to tranexamic acid. She had attained menarche at 14 years of age. She presented to emergency with excessive bleeding and passage of clots, haemoglobin was 4.4 g/dl, and she was transfused 4 units of red blood cells. An urgent MRI abdomen and pelvis showed a 9 × 8.5 × 7 cm polypoidal mass extruding through cervix, with high signal intensity with septations, irregular cystic elements, irregular margins; areas of restricted diffusion, no parametrial extension, and no lymphadenopathy. Uterus and adnexa were normal.
Examination under anaesthesia (EUA) was performed and it revealed a polypoid mass arising from the cervix, and biopsies were taken. Histopathology revealed rhabdomyosarcoma of botryoid subtype, desmin positive, aberrant P53 (overexpressed), hormone receptor negative, and cytokeratin AE1/AE3 negative.
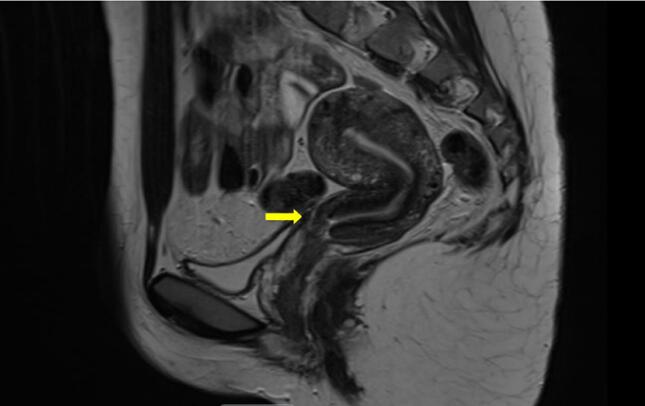
The patient received 4 cycles of neoadjuvant chemotherapy as per standard risk RMS 2005 protocol: vincristine, ifosfamide, actinomycin (VIA). There was no residual disease following chemotherapy on imaging (Fig. 1), and she underwent simple trachelectomy, with endometrial biopsy. The specimen did not show any evidence of residual disease and endometrial biopsy was negative for malignancy. Following surgery, she further received 5 cycles of adjuvant chemotherapy (VIA). The patient has been on regular follow up for the last 2 years, has remained asymptomatic, and there has been no evidence of recurrent disease on clinical examination and MRI.
Fig. 1.
Magnetic Resonance Imaging of pelvis showing no residual disease after neoadjuvant chemotherapy.
1.2. Case 2
Sixteen years old girl presented to emergency with complaints of heavy and irregular periods for 4 months, and mass protruding in the vagina. She also complained of passing a fleshy mass 1 week prior to her attendance to hospital. She attained menarche at 13 years of age, previous menstrual cycles were regular. Her family history revealed that her paternal grandfather had bowel cancer and both her paternal grandmother and aunt had breast cancer.
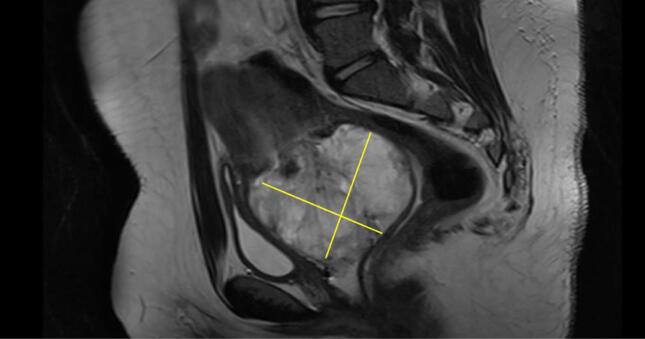
MRI revealed a polypoidal mass arising from the cervix measuring 6 cm, predominantly solid with no areas of cystic changes (Fig. 2). An emergency examination under anaesthesia revealed a 5x6 cm mass arising from the anterior lip of the cervix, and excision biopsy was taken. The histology was reported as embryonal rhabdomyosarcoma (sarcoma botryoides) of cervix, with mitotic figures >50/10hpf, positive for desmin, skeletal muscle markers (Myogenin, MyoDl ) and negative for h-Caldesmon, oestrogen and progesterone receptors (ER and PR). The postoperative MRI abdomen and pelvis did not show any evidence of residual disease.
Fig. 2.
Magnetic Resonance Imaging of pelvis showing the 6x5 cm polypoidal mass arising from the cervix and protruding into the vagina.
The patient received 4 cycles of adjuvant chemotherapy as per standard risk RMS 2005 protocol in the form of vincristine, ifosfamide, and actinomycin (VIA) 3 weekly regimen. The follow up PET CT scan was normal. Following completion of 4 cycles of chemotherapy, she underwent simple vaginal trachelectomy. There was no residual disease intraoperatively, and the histology showed normal cervix, with no evidence of cancer. She further completed 5 cycles of VIA following surgery. The patient has been on regular follow up for the last 5 years having clinical assessment and imaging. There has been no evidence of recurrent disease.
1.3. Case 3
Nineteen years old girl referred from gynaecology with history of irregular bleeding per vagina, blood stained vaginal discharge, and intermittent lower abdominal pain. She had no urinary or bowel symptoms, no loss of appetite or weight. She was sexually active and did not use any contraception. She did not have any comorbidities. On examination there was a 4x5cm infiltrative mass arising from the posterior lip of the cervix, with no vaginal or parametrial invasion. Cervical biopsy was taken which revealed a high-grade sarcoma of cervix.
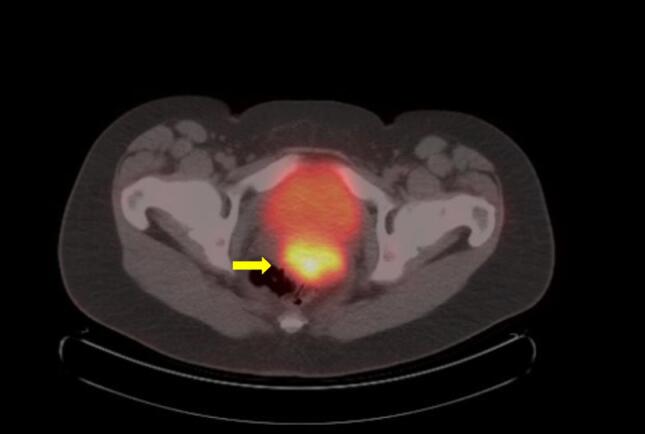
MRI abdomen and pelvis showed a 5 cm mass arising from posterior lip of cervix, heterogeneous, with mixed solid cystic areas, no parametrial invasion, and no lymphadenopathy. The PET CT scan (Fig. 3) showed a uterine mass, and there was no evidence of distant metastasis.
Fig. 3.
PET CT Scan showing increase in the F-fluorodexyglucose (FDG) uptake of the uterine mass.
In view of her histology of high-grade sarcoma, she underwent a modified radical hysterectomy, bilateral salpingectomy, and bilateral pelvic lymphadenectomy with ovarian conservation. The intraoperative findings revealed a 5 × 5 cm vascular tumour at the internal os. There was no parametrial invasion or enlarged bilateral nodes. The tumour was over 1 cm away from margin, there was no lymphovascular space invasion (LVSI), the uterus and parametrium were normal and lymph nodes were negative. Immunochemistry showed focal positivity for myogenin, MYF4, myo D1, and desmin. The final diagnosis established was cervical embryonal rhabdomyosarcoma, anaplastic variant.
The patient received a total of 9 cycles of adjuvant chemotherapy, VIA, as per standard risk of RMS 2005 protocol. Her 5 years follow up was uneventful, with no evidence of recurrent disease on clinical examination and imaging.
2. Discussion
Sarcoma botryoides accounts for 10% of the RMS cases. These embryonal tumours arise from the vagina, cervix and bladder. The outcome is favourable compared to the other subtypes- alveolar and undifferentiated. We reported 2 patients diagnosed with embryonal RMS of botryoides subtype and one of anaplastic subtype.
All of them presented with heavy bleeding per vagina, and in 2 cases there was also a cervical polypoid mass protruding through the vagina. This is in line with literature findings, according to which patients present with the sensation of a mass at the introitus, with one or more polyps which can be soft, grape-like clusters (Jayi, et al., 2014, Fletcher et al., 2013, Kriseman et al., 2012, Hemida et al., 2012, Kriseman, 2012). Bleeding and offensive discharge are the most frequent complaints (Jayi, et al., 2014, Kriseman et al., 2012).
The differential diagnosis of cervical masses in this age group consist of benign pathologies such as rhabdomyoma, pseudosarcoma botryoides (oedematous mesodermal cervical polyp), and malignancies as adenosarcoma and other small, round, blue cell tumours like neuroblastoma, rhabdomyosarcoma, non-Hodgkin's lymphoma, and the Ewing's family of tumours (Jayi, et al., 2014, Fletcher et al., 2013, Dehner et al., 2012).
The majority of the cervical RMS occur sporadically, however a small proportion was found to be associated with genetic conditions, such as Li-Fraumeni cancer susceptibility syndrome, familial pleuropulmonary blastoma tumour, neurofibromatosis Type I and Beckwith-Wiedemann syndrome (Jayi, et al., 2014, Villella, 2005, Kriseman et al., 2012, Saâdi et al., 2002, Sanders et al., 2008, Bernal et al., 2004, Villella et al., 2005). In the present series, one out of the three cases had a family history of malignancy of bowel cancer in grandfather, and breast cancer in grandmother and aunt.
The treatment is challenging as these are young women desirous of fertility preservation. Other factors taken into account in management are histologic subtype, size, site of origin, extent of disease at presentation and residual disease after treatment (Villella, 2005). Sarcoma botryoides of the cervix behaves less aggressively than sarcoma botryoides of the vagina and uterus (Jayi, et al., 2014), hence fertility sparing options can be considered in management of cervical RMS (Jayi, et al., 2014, Bernal et al., 2004, Saâdi et al., 2002). The Intergroup Rhabdomyosarcoma Study Group (IRSG) states that fertility-sparing surgery and chemotherapy is an appropriate treatment for patients with localized disease, but it is not applicable for metastatic disease (Jayi, et al., 2014, Zrara et al., 2002, Kayton et al., 2009, Villella, 2005). The most important principle for the surgical treatment in RMS is the complete resection of the primary tumour with surrounding margin of normal tissue. The options vary from cone biopsy and polypectomy to obtain a definitive diagnosis, to simple or radical trachelectomy (Jayi, et al., 2014, Kriseman et al., 2012, Bernal et al., 2004).
In the present series, two patients underwent fertility sparing surgery in form of simple trachelectomy as both the patients had undergone an excisional biopsy due to the an exophytic nature of the growth resulting in no residual tumour after biopsy and chemotherapy, and the initial histology showed cervical embryonal RMS. Both trachelectomies were performed vaginally. The literature also indicates the cone as an alternative to simple trachelectomy given the higher risk of second trimester miscarriage and preterm deliveries with the latter. However, there is a greater chance for positive margins with conisation, as well as ectocervix being left in situ. The aim was to ensure negative margins.
In the third patient, decision of radical hysterectomy was taken as the tumour was infiltrative involving the cervix and extending into the internal os and the initial biopsy results had shown a high-grade sarcoma. However, final histology did show an aggressive variant of RMS i.e. anaplastic type.
The literature suggests that lymphadenectomy is optional in patients with low risk clinical presentations, but recommended in patients with high risk clinical presentations (Elsebaie and Elsayed, 2018). RMS is a chemosensitive tumour. The cycles of chemotherapy after surgery target the lymphatic micro metastases if any. Hence we recommend that lymphadenectomy should be reserved for high risk clinical presentations.
The standard chemotherapy regimen for embryonal RMS in Europe is vincristine, isofosfamide, and actinomycin (VIA), which was given to all the three patients; 2 patients also received neoadjuvant chemotherapy prior to surgery. There is a difference in treatment protocol standard between Europe and North America, where chemotherapy consists in vincristine, actinomycin and cyclophosphamide (VAC). In IRS-IV study patients were randomised to receive chemotherapy with VAC or VAI. No significant difference in outcome was noted and the VAC was elected as gold standard by the American investigators due to the lower cost and nephrotoxicity of cyclophosphamide (European Paediatric Soft Tissue Sarcoma Study Group - RMS, 2005).
Radiotherapy is the third modality and is indicated for the local control of the tumour in cases with microscopic or macroscopic residual disease after surgery or chemotherapy (Villella, 2005).
Classical embryonal RMS most commonly present with polypoid (exophytic) growth pattern associated with more favourable prognosis (92% survival at 10 years) than diffuse intramural (endophytic) growth pattern (68% survival at 10 years). The most important prognostic factors for candidacy to fertility sparing surgery are well defined (polypoid) presentations, embryonal histology, superficial tumours, whilst deeply invasive disease, alveolar/pleomorphic histology increase the risk of treatment failure and tumour recurrence (Elsebaie and Elsayed, 2018).
Also, the extent of the disease after primary surgery is another important prognostic factor (Jayi, et al., 2014, Villella et al., 2005). The IRSG divided the status after the primary surgery in 3 groups and analysed the survival. According to this, in Clinical Group I (no residual tumour after surgery) – the survival at 5 years is greater than 90%, in Clinical Group II (microscopic residual disease) – the 5 years survival is 80%, and in Clinical Group III (macroscopic residual disease) – the 5 years survival rate is approximately 70% (Jayi, et al., 2014, Villella et al., 2005). All the three patients in the present series had no residual disease following surgery and did not show any recurrence during their long term follow up.
The latter consisted in 3 monthly follow up with MRI and CXR for the first year, 4 monthly follow up with MRI and CXR for the second and third year, and 1 yearly follow up for the fourth and fifth year.
The potential completion hysterectomy for patients who have completed their family plans has to be assessed on an individual basis. Where complete surgical clearance was achieved and the patient is compliant with her follow up, hysterectomy is not necessary providing no further recurrence.
3. Conclusion
The embryonal type of cervical RMS is the most frequent type in this age group. Cervical RMS have good prognosis as usually they present early due to clinical features of bleeding or a mass protruding through the vagina. It should be considered as differential diagnosis for continuous vaginal bleeding in a teenager and should be investigated appropriately. The patients diagnosed with RMS should be managed by multidisciplinary team at cancer centre for best outcomes. Given the young age at diagnosis, fertility sparing treatment maintaining the oncological safety is of paramount importance and is associated with long term survival.
Declaration of Competing Interest
The authors declared that there is no conflict of interest.
References
- S Jayi et al. - Embryonal rhabdomyosarcoma of the cervix presenting as a cervical polyp in a 16-year-old adolescent- a case report, Jayi et al. Journal of Medical Case Reports 2014, 8:241. [DOI] [PMC free article] [PubMed]
- Fletcher C., Bridge J., Hogendroom P., Mertrens F. IARC; Lyon: 2013. WHO Classification of Tumours of Soft Tissue and Bone. [Google Scholar]
- Behtash N., Mousavi A., Tehranian A., Khanafshar N., Hanjani P. Embryonal rhabdomyosarcoma of the uterine cervix: case report and review of the literature. Gynecol. Oncol. 2003;91:452–455. doi: 10.1016/s0090-8258(03)00539-0. [DOI] [PubMed] [Google Scholar]
- Dehner L.P., Jarzembowski J.A., Hill D.A. Embryonal rhabdomyosarcoma of the uterine cervix: a report of 14 cases and a discussion of its unusual clinicopathological associations. Mod. Pathol. 2012;25:602–614. doi: 10.1038/modpathol.2011.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriseman M.L., Wang W.-L., Sullinger J., Schmeler K.M., Ramirez P.T., Herzog C.E., Frumovitz M. Rhabdomyosarcoma of the cervix in adult women and younger patients. Gynecol. Oncol. 2012;126:351–356. doi: 10.1016/j.ygyno.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saâdi I., Errihani H., Haddadi K., Amaoui B., Benjaafar B., El Gueddari B.K. Rhabdomyosarcome botryoïde du col utérin: à propos d’un cas Sarcoma botryoïde of the uterine cervix. Canc/Radiother. 2002;6:363–365. doi: 10.1016/s1278-3218(02)00256-1. [DOI] [PubMed] [Google Scholar]
- Sanders M.A., Gordinier M., Talwalkar S.S., Moore G.D. Embryonal rhabdomyosarcoma of the uterine cervix in a 41-year-old woman treated with radical hysterectomy and adjuvant chemotherapy. Gynecol. Oncol. 2008;111:561–563. doi: 10.1016/j.ygyno.2008.07.016. [DOI] [PubMed] [Google Scholar]
- Bernal K.L., Fahmy L., Remmenga S., Bridge J., Baker J. Embryonal rhabdomyosarcoma of the cervix presenting as a cervical polyp treated with fertility-sparing surgery and adjuvant chemotherapy. Gynecol. Oncol. 2004;95:243–246. doi: 10.1016/j.ygyno.2004.06.049. [DOI] [PubMed] [Google Scholar]
- Villella J.A., Bogner P.N., Jani-Sait S.N., Block A.M., Lele S. Rhabdomyosarcoma of the cervix in sisters with review of the literature. Gynecol. Oncol. 2005;99:742–748. doi: 10.1016/j.ygyno.2005.08.048. [DOI] [PubMed] [Google Scholar]
- Hemida R., Goda H., Abdel-Hady E., El-Ashry R. Embryonal rhabdomyosarcoma of the female genital tract: 5 years’ experience. J Exp Ther Oncol. 2012;10(2):135–137. [PubMed] [Google Scholar]
- Zrara I., Mounzil C.D., Rimani M., Bouzidi A., Labraimi A., Ben O.C. Botryoide sarcoma of the uterine cervix. About one case. Gynécologie Obstétrique Fertilité. 2002;30:784–786. doi: 10.1016/s1297-9589(02)00484-8. [DOI] [PubMed] [Google Scholar]
- Kayton M.L., Wexler L.H., Lewin S.N., Park K.J., La Quaglia M.P., Abu-rustum N.R. Pediatric radical abdominal trachelectomy for anaplastic embryonal rhabdomyosarcoma of the uterine cervix: an alternative to radical hysterectomy. J. Pediatr. Surg. 2009;44:862–867. doi: 10.1016/j.jpedsurg.2008.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- J. A. Villella - Rhabdomyosarcoma of the cervix in sisters with review of the literature, Gynaeciologic Oncology 99 (2005): 742-748. [DOI] [PubMed]
- M. L. Kriseman et al - Rhabdomyosarcoma of the Cervix in Adult Women and Younger Patients, Gynecol Oncol. 2012 September; 126(3): 351–356. doi: 10.1016/j.ygyno.2012.05.008. [DOI] [PMC free article] [PubMed]
- European Paediatric Soft Tissue Sarcoma Study Group - RMS 2005, a Protocol for Nonmetastatic Rhabdomyosarcoma, Version 1.3, May 2012.
- Elsebaie M.A., Elsayed Z. Is Fertility-preservation Safe for Adult Non-Metastatic Gynecologic Rhabdomyosarcoma Patients? Systematic Review and Pooled Survival Analysis of 137 Patients. Arch. Gynecol. Obstet. 2018;297:559–572. doi: 10.1007/s00404-017-4591-6. [DOI] [PubMed] [Google Scholar]