Abstract
Background:
Although anterior cruciate ligament (ACL) injuries are common in female soccer players, the optimal graft option for ACL reconstruction is currently unclear.
Purpose/Hypothesis:
To compare the outcomes of female soccer players after ACL reconstruction using either hamstring tendon autograft or bone–patellar tendon–bone (BTB) autograft. We hypothesized that there would be no difference in clinical outcome scores, return to sport, or retear rates between BTB and hamstring grafts in our study cohort.
Study Design:
Case series; Level of evidence, 4.
Methods:
We performed a retrospective review of all skeletally mature adolescent female soccer players who underwent primary ACL reconstruction using either hamstring tendon or BTB autograft between 2013 and 2016. Demographic, injury, and surgical variables were documented. Outcome measures included the Lysholm score, Single Assessment Numeric Evaluation, Tegner activity score, and visual analog scales for pain and for satisfaction, as well as ability to return to sport.
Results:
Overall, 90 female soccer players met the inclusion criteria, of whom 79% (41 BTB and 30 hamstring) were available for a minimum 2-year follow-up or had a graft failure before the follow-up. The BTB group had a lower body mass index (mean ± SD, 23 ± 3 vs 25 ± 4; P = .02) and shorter postoperative follow-up time in months (mean ± SD, 37.4 vs 46.1; P ≤ .001); otherwise, no differences in demographic, injury, or surgical variables between groups were noted. Regarding outcome measures, the BTB group achieved a higher Tegner score (6.0 vs 4.2; P = .004), and there was no other difference between groups. Of the patients who did not return to soccer, 44.7% reported fear as the reason. Of the patients who did return to soccer, 31.9% sustained another ACL injury (retear or contralateral tear), with no differences in reinjury rates based on graft selection.
Conclusion:
Adolescent female soccer players undergoing ACL reconstruction had relatively high satisfaction and outcome scores independent of autograft choice. Notwithstanding, patients and families need to be counseled that less than half of patients will return to their preinjury level of sport and, if an athlete attempts to return, there is a high risk of further ACL injury.
Keywords: anterior cruciate ligament, ACL reconstruction, female soccer player, adolescent, return to sport, retear, BTB autograft, hamstring autograft
The population of adolescent female soccer players has increased over the past decade both nationally and internationally.9 Given such an increase in a population prone to anterior cruciate ligament (ACL) injuries, investigations focusing on these athletes are becoming more relevant. A few recent studies have investigated clinical outcomes and incidence of retear rate in female soccer players after ACL reconstruction (ACLR).2,6,7,9,18 However, more studies are needed to fill the gaps within previous research regarding realistic expectations for timing and level of return to sport after ACLR. Furthermore, there is a paucity of literature comparing autograft choices in the competitive athlete, particularly in the female population.
The purpose of our study was to compare graft retear rates and outcomes after ACLR using bone–patellar tendon–bone (BTB) autograft versus hamstring autograft in female soccer players aged ≤18 years with closed femoral and tibial physes. Our hypothesis was that there would be no difference in clinical outcomes between the graft options and no difference in failure rates.
Methods
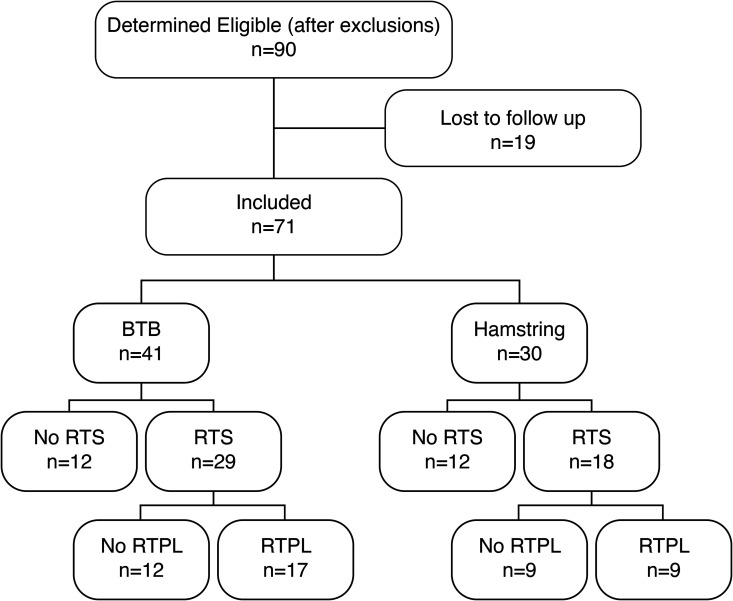
Institutional review board approval was obtained for this study. A retrospective review was performed of all patients who sustained an ACL injury while playing soccer and underwent ACLR by 1 of the 3 surgeons at our institution between 2013 and 2016. Inclusion criteria were as follows: patients had to be female and had to have reached skeletal maturity, sustained an injury while playing soccer, and received primary ACLR with either hamstring or BTB autograft. Furthermore, all patients were ≤18 years old at the time of surgery. Patients were excluded if they had sustained a multiligamentous knee injury or a previous ipsilateral ACL tear or had a previous ACLR on the same or contralateral knee. Patients also had to have a minimum follow-up of 2 years, or they had to have met the primary end point before 2-year follow-up—specifically, either retearing the ipsilateral ACL or sustaining a contralateral ACL tear (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram showing the patients who were included in the study as well as their eventual graft selection and their ultimate ability to return to sport. BTB, bone–patellar tendon–bone; RTPL, return to previous level; RTS, return to sport.
Charts were retrospectively reviewed for demographic, injury, and surgical variables. Questionnaires were filled out in clinic or during a telephone interview. Outcome measures included the Lysholm score,20 Single Assessment Numeric Evaluation,22,23 Tegner activity score,20 visual analog scale (VAS) for pain (0 = no pain, 10 = worst pain), and VAS for satisfaction (0 = very unsatisfied, 10 = very satisfied). Ability to return to soccer (yes or no), preinjury level of play (pickup, indoor, high school, club, or college), and any reason that patients could not return were also recorded (open-ended question). Patients were also asked if they sustained a reinjury to the respective or contralateral knee or if they had undergone revision ACL surgery at an outside institution.
All pre- and intraoperative data were collected retrospectively and reviewed. Preoperatively, after a thorough physical examination, all patients underwent magnetic resonance imaging (MRI) to confirm the diagnosis of an ACL tear. Skeletal maturity was defined as evidence of closed or closing physis (>50% closed) on MRI scan or radiograph. If patients did not have an MRI scan or radiograph in our system to confirm this, they were excluded from the cohort. Concomitant injuries and treatment were recorded at the time of surgery and included meniscal debridement, meniscal repair, chondroplasty, and microfracture. ACL reinjuries were defined as cases in which there was an MRI-confirmed complete or partial tear of the ACL of either the operative or the contralateral knee. In patients with no reinjury, outcome measures were obtained at 2 years after ACLR.
All surgery was performed by 1 of 3 pediatric orthopaedic surgeons at a single academic pediatric medical center. Patients had a similar single-bundle reconstruction using either a quadrupled hamstring or BTB autograft. Graft type and fixation method were based on surgeon preference. Graft choice was independent of ligamentous laxity, and no lateral extra-articular tenodesis was added in any of the cases.12 One surgeon (E.E.) used all hamstring autografts, while the 2 other surgeons (A.P., H.C.) used BTB autografts unless relative contraindications were present, such as patellofemoral disorder, Osgood-Schlatter disease, and patella alta. In general, soccer goalies preferentially received a hamstring tendon graft in an attempt to minimize any anterior knee pain with diving. Meniscal repairs or debridements were performed at the time of the reconstruction as indicated.
Postoperatively, all patients followed the same rehabilitation protocol and restrictions. Progressive weightbearing and range of motion with physical therapy were allowed immediately after surgery unless a meniscal repair was performed. In that case, knee motion was limited to 90° for 6 weeks. Patients advanced to jogging at 3 months and cutting at 6 months and returned to play after demonstrating symmetric lower extremity strength, typically between 9 and 12 months. Patients were followed clinically at approximately 1 and 6 weeks, 3 and 6 months, and 1 and 2 years postoperatively.
Statistical Analysis
Descriptive statistics were calculated for all variables. Continuous outcome data were compared between graft groups using analysis of variance. The dependent variables were evaluated for normality and homogeneity of variance. Categorical outcomes were compared between groups utilizing chi-square test. The alpha level was set at P < .05 to declare significance, and all analyses were performed utilizing SPSS Version 25 (IBM Corp).
Results
Overall, 90 patients met our inclusion criteria, of whom 71 had 2-year follow up. Of the patients lost to follow-up, there were no differences in demographic, surgical, or injury variables. Of the 71 evaluated patients, 41 had a BTB autograft and 30 had a hamstring autograft. The mean ± SD age of the cohort was 15.4 ± 1.3 years. The BTB autograft cohort had a body mass index that was significantly lower than that of the hamstring autograft cohort (23 ± 3 vs 25 ± 4; P = .02). There were no other differences in demographic, injury, or surgical variables between the groups (Table 1).
TABLE 1.
Patient Characteristicsa
| Mean ± SD or No. (%) | ||||
|---|---|---|---|---|
| All (N = 71) | BTB (n = 41) | Hamstring (n = 30) | P Value | |
| Age at surgery, y | 15.4 ± 1.3 | 15.4 ± 1.3 | 15.4 ± 1.3 | .83 |
| Body mass index | 24.0 ± 3.4 | 23.2 ± 3.0 | 25.3 ± 3.6 | .016 |
| Weight, kg | 62.1 ± 10.0 | 60.7 ± 9.3 | 64.2 ± 10.9 | .16 |
| Height, cm | 160.6 ± 6.0 | 161.5 ± 5.4 | 159.3 ± 5.4 | .15 |
| Laterality: right | 31 (43.7) | 20 (48.8) | 11 (36.7) | .371 |
| Meniscal tear requiring treatment | 30 (42.3) | 17 (41.5) | 13 (43.3) | .40 |
| Postoperative follow-up, mo | 40.8 | 37.4 | 46.1 | ≤.001 |
aBold P values indicate statistically significant difference between groups (P < .05). BTB, bone–patellar tendon–bone.
Clinical Outcome Measures
Patient-reported outcomes indicated that most patients did well, with mean Lysholm, Single Assessment Numeric Evaluation, VAS for satisfaction, and VAS for pain scores of 92.0 ± 12.0, 88.1 ± 10.4, 8.9 ± 1.6, and 1.1 ± 1.9, respectively (Table 2). These surveys demonstrated no statistical difference between graft types. However, the BTB autograft cohort did achieve a significantly higher Tegner score (6.0 ± 2.1 vs 4.2 ± 1.8; P = .004).
TABLE 2.
Clinical Outcomes at 2-Year Follow-upa
| Mean ± SD | ||||
|---|---|---|---|---|
| All (N = 71) | BTB (n = 41) | Hamstring (n = 30) | P Value | |
| SANE | 88.1 ± 10.4 | 88.9 ± 11.9 | 87.0 ± 7.6 | .10 |
| VAS: satisfaction | 8.9 ± 1.6 | 9.0 ± 1.6 | 8.7 ± 1.5 | .08 |
| VAS: pain | 1.1 ± 1.9 | 1.2 ± 2.1 | 1 ± 1.6 | .83 |
| Tegner | 5.3 ± 2.1 | 6.0 ± 2.1 | 4.2 ± 1.8 | .004 |
| Lysholm | 92.0 ± 12.0 | 92.4 ± 11.4 | 91.3 ± 13.1 | .78 |
aBold P value indicates statistically significant difference between groups (P < .05). BTB, bone–patellar tendon–bone; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale.
Return to Sport
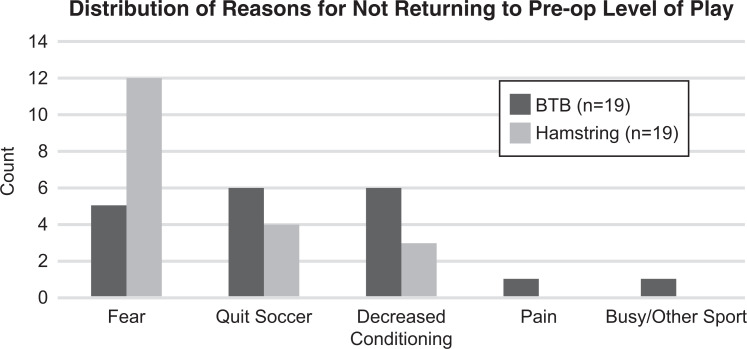
Out of the 71 patients, 47 (66%) returned to soccer at any level, and 26 (37%) returned to their preoperative level of soccer (Table 3). While the BTB autograft cohort had a greater percentage of patients return to any level of soccer as well as preinjury level of play, these values did not reach statistical significance (70.7% vs 60% [P = .35]; 41.5% vs 30% [P = .40]). The study was underpowered, as we did not have the 166 patients per group that would be necessary to achieve a power of 0.8. Of those who did not return to sport at their preoperative level of play, 38 provided rationale for why. Overall, fear was the most common reason for not returning to sport at their preoperative level of play (44.7%); however, twice as many patients in the hamstring cohort reported fear as the rationale as compared with patients in the BTB cohort. The most common rationale reported for the BTB cohort was evenly split between deconditioning and quitting soccer (Figure 2).
TABLE 3.
Return to Sporta
| Patients, No. (%) | ||||
|---|---|---|---|---|
| All (N = 71) | BTB (n = 41) | Hamstring (n = 30) | P Value | |
| Returned to soccer | 47 (66.2) | 29 (70.7) | 18 (60.0) | .35 |
| Returned to preoperative level | 26 (36.6) | 17 (41.5) | 9 (30.0) | .40 |
aBTB, bone–patellar tendon–bone.
Figure 2.
Reasons provided by athletes for why they did not return to their preoperative level of soccer. BTB, bone–patellar tendon–bone; Pre-op, preoperative.
Reinjury
For the entire cohort, including those who did not return to soccer, 16 of 71 (22.5%) patients sustained another ACL injury (retear or contralateral tear) within 2 years, with no statistical differences based on graft selection (Table 4). For the 47 athletes who returned to soccer, 15 (31.9%) sustained another ACL injury within 2 years of the index procedure (Figure 3). In this cohort of patients who returned to soccer, the hamstring autografts failed 2 times more frequently, with 4 (22.2%) failures in 18 patients versus 3 (10.3%) failures in 29 patients in the BTB autograft group, but this difference did not reach statistical significance (P = .40) (Figure 4). Of those who did not return to soccer, there was only 1 retear out of 24 patients (4.2%).
TABLE 4.
Reinjuriesa
| Patients, No. (%) | ||||
|---|---|---|---|---|
| Overall | BTB | Hamstring | P Value | |
| All patients | 71 | 41 | 30 | |
| Graft retear | 8 (11.3) | 4 (9.8) | 4 (13.3) | .71 |
| Contralateral ACL tear | 8 (11.3) | 4 (9.8) | 4 (13.3) | .71 |
| Total | 16 (22.5) | 8 (19.5) | 8 (26.7) | .48 |
| Return-to-sport cohort | 47 | 29 | 18 | |
| Graft retear | 7 (14.9) | 3 (10.3) | 4 (22.2) | .403 |
| Contralateral ACL tear | 8 (17) | 4 (13.8) | 4 (22.2) | .692 |
| Total | 15 (31.9) | 7 (24.1) | 8 (44.4) | .147 |
aACL, anterior cruciate ligament; BTB, bone–patellar tendon–bone.
Figure 3.
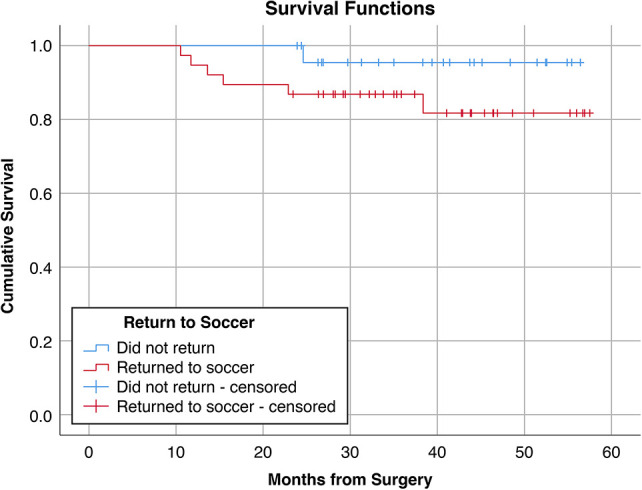
Kaplan-Meier curve depicting the ipsilateral graft failures in athletes returning to soccer as compared with those who did not return to soccer.
Figure 4.
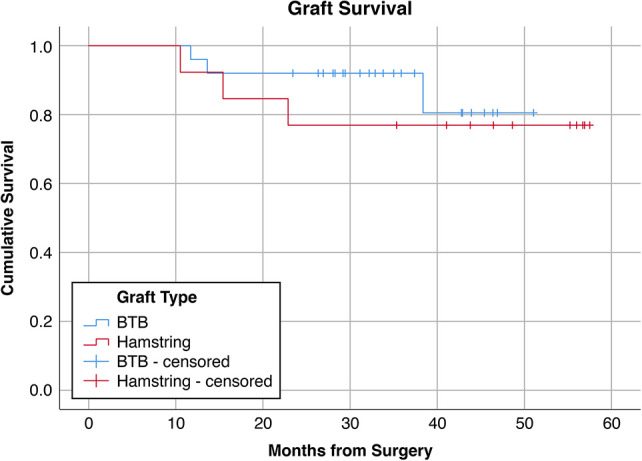
Kaplan-Meier curve depicting the ipsilateral graft failures in athletes returning to soccer who had a bone–patellar tendon–bone (BTB) autograft versus a hamstring autograft.
Meniscal Injury
Of 71 patients, there were 30 (42.3%) with meniscal tears. Of these 30, 17 (56.7%) underwent repair, and 13 (43.3%) underwent debridement. There was no difference in repair rate between the BTB and hamstring cohorts. Eighteen (60%) meniscal tears were isolated lateral tears, 7 (23.3%) were medial tears, and 5 (16.7%) were both medial and lateral tears. Of the 8 patients with a retear of the ipsilateral ACLR, only 1 (12.5%) had a meniscal tear at the time of original injury, which was debrided. This was similar to the overall retear of the ipsilateral ACLR (11.3%), as shown earlier. Patients who had their meniscus debrided, therefore, appeared to be at no higher risk for retear of the ACLR.
Discussion
According to the most recent large-scale census by Federation Internationale Football Association in 2006, approximately 29 million women play soccer worldwide, with a >50% increase in registered players since the previous census in 2000.10 This number has risen in the past 13 years throughout the world, particularly in the United States.16 The higher number of soccer players has come with a concurrent increase in injuries, with ACL tear being one of the more significant injuries that can affect an athlete’s career.
Our patient population of adolescent female soccer players is at high risk for ACL injury and reinjury owing to multiple factors. First, female soccer players have been reported to have a 2- to 4-times higher incidence rate of ACL tears as compared with male players, regardless of the level of participation.15,18,19 Additionally, they have a 3.8-times higher retear rate than do men after undergoing reconstruction and almost a 5-fold higher rate of subsequent ACL injury as compared with female soccer player controls with no previous knee injury.7,8,11 There is also a 28% rate of ACL retear after ACLR and a 34% rate of retear after returning to soccer.2
Aside from associated risks with sex and sport participation, our population is at higher risk for reinjury given its young age and the known association with higher reinjury.21 In previous studies, female soccer players had a rate of return to soccer between 46% and 67% after ACLR, demonstrating the significant effect that this injury has on an athlete’s future in the sport.6,8,18 This is a much lower rate than that seen in the general population, which is 80% in those returning to any sport after ACLR.3
At this time, it is unclear what causes this high retear rate. Functional performance testing has not been shown to differ between ACLR and control groups.8 In addition to the unexplained higher tear rates, Tegner activity scores among female soccer players have been shown to decrease at a higher rate in those with ACLR as compared with controls.6,7
Despite extensive literature on ACLR and soccer players, the optimal graft option for female soccer players is still unclear. With skeletally immature patients, a soft tissue graft is strongly recommended to avoid physeal growth disturbance.13 Regarding the donor tissue origin, there are higher failure rates in a young active population when allograft tissue is used in reconstruction.4,5,14 In skeletally mature patients, however, many autograft options are regularly used without clear benefit of one over the others. Alguacil et al1 investigated the strength of quadriceps versus hamstring tendon autografts in male soccer players; they demonstrated better isokinetic strength in quadriceps tendons at the 12-month mark but demonstrated no difference at 24 months and no clinical outcomes differences.
In this study, we found that adolescent female soccer players undergoing ACLR have relatively high satisfaction and outcome scores independent of autograft choice. We also found a significant increase in Tegner activity score in the BTB autograft group as compared with the hamstring autograft group. It is unclear why this difference existed. We did not have preoperative activity data on our patients to compare a change in pre- and postoperative function that could have offered a possible explanation for the difference.
Despite overall high satisfaction clinically, our data highlight the challenges of treating adolescent female soccer players who sustain an ACL injury. Patients and families need to be counseled that less than half of these adolescents will return to their preinjury level of sport. Additionally, if an athlete returns to playing soccer, there is a high risk of further ACL injury (31.9%) to either the operative or nonoperative knee. These findings are comparable with previously noted percentages. Similarly, the patients and families can be informed that fear of reinjury accounts for almost half (44.7%) of the patients’ reason for not returning to sport. This is consistent with a previously reported rationale in a systematic review assessing patient reasoning for not returning to play after ACLR in the adult population. Nwachukwu et al17 found that 49.6% of patients stated that fear was the primary reason why they did not return to play. Fear is a common and complex theme seen postoperatively with ACLR. As such, further consideration should be given to counseling or other methods of addressing and assisting with that fear.
While we did not find statistically significant differences of retear rates between BTB and hamstring autografts in patients who returned to soccer, we did appreciate a trend with a 2-fold higher risk, which we hypothesize might reach significance with a larger patient population. A post hoc power analysis revealed that 166 patients per group would be necessary to adequately power a future study to address this question. However, the mean follow-up was 10 months longer in the hamstring graft group, which could account for this difference. No difference between graft retear rates was seen when we assessed all patients together or the cohort of patients who did not return to soccer. This suggests that BTB autograft might offer more stability in athletes with higher-demand physical activity, as in the population returning to the previous level of sport.
There are several limitations to our study. The retrospective nonrandomized design did not allow us to account for surgeon graft preference in each situation. Three surgeons were included in this study: 1 exclusively performed ACLR using hamstring autograft, whereas the other 2 preferred BTB autograft. We could not fully control for selection bias or variation in surgical technique because of this. It is unclear how this could have affected the data; however, our demographic data were similar between the groups. Additionally, other factors were not consistently reported in patient charts, such as the presence of generalized ligamentous laxity. In our clinical practice, we do not utilize objective clinical measurements, such as KT-1000 arthrometer, so we were unable to report on this assessment tool. We also acknowledge that many other variables contribute to an athlete’s reinjury and outcomes aside from graft type; however, we chose to focus on graft type, as this is an easily controllable variable.
There were 19 patients who underwent ACLR at our institution, did not have adequate 2-year follow-up data, and were therefore excluded from our 71-patient list. While the patients lost to follow-up were 21% of our population, there were no differences in demographic, injury, or surgical data and, most importantly, in the graft type between those lost to follow-up and those who were not. It is possible that this skewed our data for failure rate and outcomes scores, although we did not see this as a likely large source of bias. In regard to comparative analysis, our study was underpowered with a small patient cohort and relatively short-term follow-up. The relatively small number of patients does not allow us to make a strong statement about which graft is best in this high-demand female patient population. Based on our experience it would take a large multicenter study group to answer this question.
The findings of our study highlight the challenges of treating adolescent female soccer players undergoing ACLR, as less than half of patients returned to preinjury level of sport. With fear being the most cited reason for not returning to sport, it is possible that female soccer players would benefit from support from a sports psychologist throughout the rehabilitation process. Conversely, the low rate of return could be a result of the patient and family electing not to return out of concern for retear. The findings highlight the importance of the surgeon setting appropriate expectations preoperatively. Finally, despite multiple studies investigating the best options for grafts, we have yet to find clear benefit of one graft over the other.
Footnotes
Final revision submitted May 28, 2020; accepted June 17, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.B. has received educational support from SportsTek. E.E. has received research support from DePuy and speaking fees from Arthrex and Ossur. H.C. has received research support from Allergan and consulting fees from OrthoPediatrics and Roche Molecular Systems. A.P. has received educational support from Arthrex and SportsTek, consulting fees from OrthoPediatrics, and speaking fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of California, San Diego (study No. 161895X).
References
- 1. Alguacil JL, Arroyo-Morales M, Martin-Gomez JL, et al. Strength recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus hamstring tendon autografts in soccer players: a randomized controlled trial. Knee. 2018;25(4):704–714. [DOI] [PubMed] [Google Scholar]
- 2. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 4. Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26:1593–1601. [DOI] [PubMed] [Google Scholar]
- 5. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362–2367. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fältstrom A, Hagglund M, Kvist J. Factors associated with playing football after anterior cruciate ligament reconstruction in female football players. Scand J Med Sci Sports. 2016;26(11):1343–1352. [DOI] [PubMed] [Google Scholar]
- 8. Fältstrom A, Hagglund M, Kvist J. Female soccer players with anterior cruciate ligament reconstruction have a higher risk of new knee injuries and quit soccer to a higher degree than knee-healthy controls. Am J Sports Med. 2019;47(1):31–40. [DOI] [PubMed] [Google Scholar]
- 9. Fältstrom A, Hagglund M, Kvist J. Functional performance among active female soccer players after unilateral primary anterior cruciate ligament reconstruction compared with knee-healthy controls. Am J Sports Med. 2017;45(2):377–385. [DOI] [PubMed] [Google Scholar]
- 10. Federation Internationale de Football Association. FIFA Big Count 2006: 270 million people active in football. Published May 2007. Accessed February 2014 https://www.fifa.com/mm/document/fifafacts/bcoffsurv/bigcount.statspackage_7024.pdf
- 11. Gans I, Retzky JS, Jones LC, Tanaka MJ. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association sports: the Injury Surveillance Program, 2004-2014. Orthop J Sports Med. 2018;6(6):2325967118777823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Getgood A, Bryant D, Firth A; Stability Group. The Stability study: a protocol for a multicenter randomized clinical trial comparing anterior cruciate ligament reconstruction with and without lateral extra-articular tenodesis in individuals who are at high risk of graft failure. BMC Musculoskelet Disord. 2019;20:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop. 2002;22:452–457. [PubMed] [Google Scholar]
- 14. Mehta VM, Mandala C, Foster D, Petsche TS. Comparison of revision rates in bone–patella tendon–bone autograft and allograft anterior cruciate ligament reconstruction. Orthopedics. 2010;33:12. [DOI] [PubMed] [Google Scholar]
- 15. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: a systemic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54(5):472–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nielsen Football fever is spreading as Major League Soccer kicks off a new season. Published April 3, 2019. https://www.nielsen.com/us/en/insights/article/2019/football-fever-is-spreading-as-major-league-soccer-kicks-off-a-new-season/ [Google Scholar]
- 17. Nwachukwu BU, Adejei J, Rauck RC, et al. How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sports Med. 2019;22;7(5):2325967119845313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sandon A, Werner S, Forssblad M. Factors associated with returning to football after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2514–2521. [DOI] [PubMed] [Google Scholar]
- 19. Stanley LE, Kerr ZY, Dompier TP, Padua DA. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in collegiate and high school sports: 2009-2010 through 2013-2014. Am J Sports Med. 2016;44(6):1565–1572. [DOI] [PubMed] [Google Scholar]
- 20. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 21. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in young athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the Single Assessment Numeric Evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000;373:184–192. [DOI] [PubMed] [Google Scholar]
- 23. Winterstein AP, McGuine TA, Carr KE, Hetzel SJ. Comparison of IKDC and SANE outcome measures following knee injury in active female patients. Sports Health. 2013;5(6):523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]