Abstract
Gout is a common cause of inflammatory arthritis, typically affecting the joints of the appendicular skeleton. In this report, we present the relatively less common scenario of chronic tophaceous gout affecting the lumbar spine and pelvis, complicated by compressive neuropathy, and notable for its advanced initial presentation in a young patient. We review the pathophysiology underlying gout and discuss its clinical and laboratory presentation. We also use our case as an example to present the radiographic, CT, and MR imaging features of gout affecting the lumbar spine, which can often present a diagnostic dilemma. Finally, we discuss therapeutic options for gout resulting in spinal canal compromise, which include interventions not commonly performed for gout elsewhere in the body.
Keywords: Gout, Spine, Arthritis, Radiculopathy
Introduction
Gout is the most common inflammatory arthritis worldwide, with an increasing prevalence, currently estimated between 1% and 4% in adults [1,2]. Gout is a type of crystalline arthropathy, triggered when monosodium urate exceeds its limit of solubility in the serum and deposits in the synovial and periarticular soft tissues, forming tophi [1]. The negatively birefringent urate crystals initiate an immune complex cascade that results in inflammation and pain. Hyperuricemia, generally defined as serum uric acid levels above 6.8 mg/dL, is the strongest risk factor for developing gout, and is most often the result of hepatic overproduction or underexcretion due to renal impairment [1]. However, about 10% of people are genetically predisposed to having increased serum urate levels, and thus are at an increased risk for developing gout [2]. Acute gout attacks are monoarticular, rapid in onset, and are characterized by a warm, swollen, erythematous joint that typically resolves within days to weeks. In comparison, chronic gout is characterized by destructive polyarticular involvement, bony erosions, cartilage damage, formation of tophi, and persistent chronic pain [3]. In this case report, we present the unusual case and imaging findings of a young male with an advanced initial presentation of chronic gout, including tophus development in the lumbar spine.
Case report
A 27-year-old male with no known prior medical history initially presented to our emergency room with a chief complaint of difficulty ambulating for 1 month secondary to lower extremity and back pain. On further inquiry, he reported having had brief, periodic episodes of acute pain involving the right ankle, and both feet, knees, elbows, and hands over the previous 5 years. He also reported that his father had a history of gout. On physical exam, numerous hard, nodular masses consistent with tophi were evident, including a 1 cm tophus on the left elbow, a 3 cm tophus on the right elbow, a 4 cm tophus on the right knee, a 2 cm tophus on the left knee, and multiple subcentimeter tophi of the palms and soles bilaterally. The left elbow was found to be limited in extension. In addition, palpation of the lumbar spine elicited tenderness. Laboratory investigation was significant for hyperuricemia, with an initial uric acid level of 9.4 mg/dL. The complete blood count and basic metabolic panel were normal.
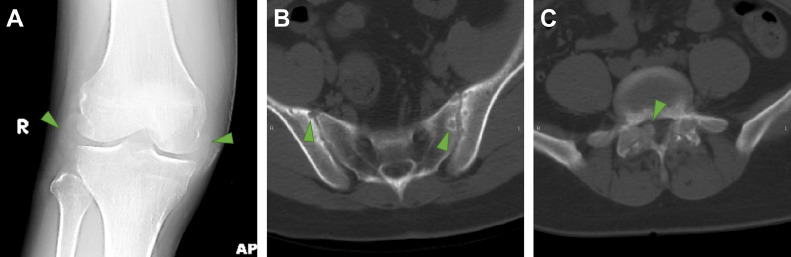
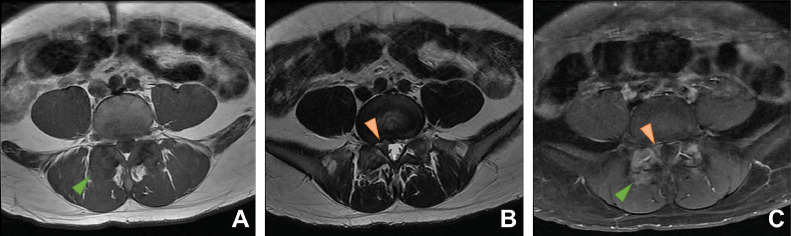
Radiographs of the knee and a CT examination of the abdomen and pelvis were obtained and are presented in Fig. 1. The large right knee tophus was visible as areas of increased radiodensity within the soft tissues surrounding the knee joint. Knee joint spacing was normal, without any discrete erosions. The abdominopelvic CT was significant for bilateral sacroiliac joint erosions. In addition, and notably in relation to the symptoms of back and leg pain, hypertrophic changes of the facet joints were seen bilaterally at L4-L5 and L5-S1, with ground-glass mineralization permeating the laminae and extending into the paraspinal soft tissues, as well as into the lateral epidural spaces, most prominently on the right at L5-S1. A contrast-enhanced MRI of the lumbar spine, shown in Fig. 2, was then performed for further evaluation and revealed heterogeneous enhancement associated with the ground-glass regions seen on the CT. Also seen was a L5-S1 disc bulge with an asymmetric protrusion in the right foraminal zone which combined with the dorsolateral epidural tophus to produce severe right sided neural foraminal stenosis and right S1 nerve impingement in the lateral recess.
Fig. 1.
Radiographic and CT findings of gout. (A) AP view of the knees demonstrates increased soft tissue density (arrowheads) along the lateral and medial aspects of the right knee joint corresponding to a clinically-evident 4 cm tophus. (B) Axial CT image at the level of the sacroiliac joints presented on bone window reveals subarticular erosions (arrowheads) along the sacroiliac joints. (C) Axial CT images at the level of the L5-S1 facet joints presented on bone window illustrates ground glass density along the superior and inferior articular processes and spinal laminae. On the right, there is notable extension into the right lateral epidural space (arrowhead).
Fig. 2.
MR imaging features of spinal gout. Axial T1-weighted (A), T2-weighted (B), and post-contrast T1-weighted fat-suppressed (C) images of the spine at the L5-S1 level depict the gouty tophi as T1 isointense, T2 hypointense material with heterogeneous patchy enhancement (green arrowheads). On the right, the medial extension of the tophus associated with the facet joint combines with a disc bulge to produce impingement of the S1 nerve root in the lateral recess (orange arrowheads).
He was prescribed naproxen, allopurinol, and colchicine and referred to follow up with our rheumatology clinic. At his follow up visit, allopurinol dosing was increased from 100 mg to 400 mg daily to target a uric acid goal of < 5 mg/dL, naproxen was continued, and oral prednisone was started. Given the involvement of the lumbar spine and nerve root compression, an aggressive approach was favored, and the patient also received intravenous pegloticase infusions every 2 weeks. During the course of his treatment, the patient also required bilateral L5-S1 facet joint and epidural space injections of local anesthetic and corticosteroid for refractory back and leg pain from his gout-related radiculopathy.
Discussion
Gout typically affects the peripheral joints of the appendicular skeleton but can also less commonly involve joints of the axial skeleton [4]. Gout can affect any level of the spine, but is most commonly reported in the lumbar region [5]. Tophi deposition in the axial elements of the spine is generally found at the facet articulation, but the ligamentum flavum, pedicle, lamina, epidural soft tissue, vertebral body, and disc space can also be affected [4,6].
There are variable and non-specific findings associated with spinal gout, which can make diagnosis challenging. On T1-weighted images, tophi have been reported as exhibiting homogenous intermediate to hypointense signal, and on T2-weighted sequences, their signal intensity is variable [7,8]. Both homogeneous and peripheral heterogeneous patterns of contrast enhancement have been described in association with gouty tophi, with the different enhancement patterns hypothesized to be due to variable vascularization of the inflammatory tissue induced by monosodium urate crystal deposition [6–8].
Reported MRI mimics for spinal gout include spondyloarthritis, infectious discitis, epidural abscess, and tumor [4,8–10]. The difficulty in discriminating gout from its mimics can sometimes lead to invasive interventions. In 1 case, a peripherally enhancing mass concerning for a spinal tumor was biopsied, with the result confirming tophaceous gout [9]. In another case, enhancement of a lumbar facet joint with medial soft tissue enhancement led to surgical exploration in order to differentiate between epidural abscess and spinal gout [10]. Correlating the CT finding of a tophus with high radiodensity, such as in our patient, with the pattern of MR enhancement may prove useful in recognizing spinal gout. Dual energy CT, if available, can also assist in the identification of urate crystals, which produce less attenuation of an 80 kVp beam than calcium does [11]. Regardless, spinal gout can present a challenging diagnosis, in large part due to its variable imaging appearances on both CT and MR imaging.
As gout can cause radiculopathy via nerve root or spinal cord compression, accurate and expedient diagnosis and treatment for the disease is important. Treatments for spinal gout and tophi primarily include pharmacologic urate acid-lowering therapies; however, in cases of nerve root or cord compression surgical intervention may be required to provide immediate decompression [12]. In less acute scenarios, minimally invasive procedures, such as epidural anesthetic and steroid injections can help manage refractory radicular pain.
Conclusion
We have presented a case of gout that is unique for its relatively early onset, advanced initial presentation, and spinal epidural involvement. We have reviewed the variable CT and MR imaging appearance of spinal gout. Recognition of these imaging features can assist the clinical workup, help minimize diagnostic delays, and guide minimally invasive or surgical therapeutic options when necessary.
Patient Consent Statement
This patient is currently lost to follow-up; however, during his presentation, he signed conditions of admission, which at our institution state an agreement to undergo procedures and treatments including imaging examinations, an agreement to have trainees participate in patient care, and an agreement to have photographs, video, and other images used for training and education purposes. In addition, we have suppressed all personally-identifiable information from the report, including all 18 HIPAA identifiers.
References
- 1.Golenbiewski J, Keenan RT. Moving the needle: improving the care of the gout patient. Rheumatol Ther. 2019;6(2):179–193. doi: 10.1007/s40744-019-0147-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryan MP, Monjazeb S, Goodwin BP, Group AR. Ulcerated tophaceous gout. Dermatol Online J. 2019;25(3) [PubMed] [Google Scholar]
- 3.Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective - A review. J Adv Res. 2017;8(5):495–511. doi: 10.1016/j.jare.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon J-W, Park K-B, Park H. Tophaceous gout of the spine causing neural compression. Korean J Spine. 2013;10(3):185–188. doi: 10.14245/kjs.2013.10.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Konatalapalli RM, Demarco PJ, Jelinek JS. Gout in the axial skeleton. J Rheumatol. 2009;36(3):609–613. doi: 10.3899/jrheum.080374. [DOI] [PubMed] [Google Scholar]
- 6.Zheng Z-F, Shi H-L, Xing Y, Li D, Jia J-Y, Lin S. Thoracic cord compression due to ligamentum flavum gouty tophus: a case report and literature review. Spinal Cord. 2015;53(12):881–886. doi: 10.1038/sc.2015.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu C-Y, Shih TT-F, Huang K-M, Chen P-Q, Sheu J-J, Li Y-W. Tophaceous gout of the spine: MR imaging features. Clin Radiol. 2002;57(10):919–925. doi: 10.1053/crad.2001.1001. [DOI] [PubMed] [Google Scholar]
- 8.Yen P-S, Lin J-F, Chen S-Y, Lin S-Z. Tophaceous gout of the lumbar spine mimicking infectious spondylodiscitis and epidural abscess: MR imaging findings. J Clin Neurosci Off J Neurosurg Soc Australas. 2005;12(1):44–46. doi: 10.1016/j.jocn.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Nakajima A, Kato Y, Yamanaka H, Ito T, Kamatani N. Spinal tophaceous gout mimicking a spinal tumor. J Rheumatol. 2004;31(7):1459–1460. [PubMed] [Google Scholar]
- 10.Barrett K, Miller ML, Wilson JT. Tophaceous gout of the spine mimicking epidural infection: case report and review of the literature. Neurosurgery. 2001;48(5):1170–1173. doi: 10.1097/00006123-200105000-00046. [DOI] [PubMed] [Google Scholar]
- 11.Desai MA, Peterson JJ, Garner HW, Kransdorf MJ. Clinical utility of dual-energy CT for evaluation of tophaceous gout. Radiogr a Rev Publ Radiol Soc North Am Inc. 2011;31(5):1365–1367. doi: 10.1148/rg.315115510. [DOI] [PubMed] [Google Scholar]
- 12.Saketkoo LA, Robertson HJ, Dyer HR, Virk Z-U, Ferreyro HR, Espinoza LR. Axial gouty arthropathy. Am J Med Sci. 2009;338(2):140–146. doi: 10.1097/MAJ.0b013e3181a3dc14. [DOI] [PubMed] [Google Scholar]