Highlights
-
•
Atrial fibrillation is associated with peripheral embolism.
-
•
Renal artery embolism is reported in rare instances.
-
•
Clinical suspicion in high risk patient and urgent treatment is key to success.
Keywords: Case report, Renal segmental artery embolism, Popliteal artery embolism, Atrial fibrillation, Thrombolysis
Abstract
Introduction
Renal artery embolism is uncommon cause of flank or back pain. Of all embolic episodes in patients with atrial fibrillation, 2–4% are renal artery embolism. Early thrombolysis within 90 min has favorable renal outcome. Long term anticoagulation can prevent recurrent embolic episodes. Two different embolic phenomenon within short span in same patient is not described in literature.
Presentation of case
We describe fifty-year-old female with rheumatic heart disease with atrial fibrillation presented as renal segmental artery emboli with popliteal artery emboli within seven-day interval.
Discussion
Embolic phenomenon is well known in atrial fibrillation. High index of suspicion in patient with risk factors of thromboembolism with appropriate use of contrast enhanced computed tomography can help early diagnosis. Renal artery embolism is managed with anticoagulation or thrombolysis based on duration of presentation. Peripheral artery embolism can be diagnosed with Doppler ultrasonography. Thrombus can be removed with endovascular procedure or open surgical technique. Holistic patient management includes cardiac workup and treatment of factors predisposing to embolization.
Conclusion
Early identification and urgent treatment is key to the management of embolic episode in patient with atrial fibrillation. Long term prophylaxis can prevent further episodes.
1. Introduction
Renal artery embolism is uncommon cause of flank or back pain whose diagnosis is often delayed [1,2]. Atrial fibrillation is often associated with thromboembolic phenomenon and risk of embolism to renal artery, mesenteric artery and peripheral arteries is increased in these group of patients [3,4]. High index of suspicion in patient with risk factors of thromboembolism with appropriate use of imaging can help early diagnosis. Urgent treatment with anticoagulation or thrombolysis or endovascular aspiration is key to the management of embolic episode in patient with atrial fibrillation [5,6]. Long term prophylaxis can prevent further episodes and treatment of cause can address the problem. This case report has been reported in line with the SCARE 2018 criteria [7].
2. Case report
A fifty-year-old female presented to Emergency Room of our Institute with complaint of right flank pain and vomiting for 5 days. Pain was moderate to severe, non-radiating, constant intensity, relieved partially with oral pain killers. She had no burning micturition, no fever, no decrease in urine output, no hematuria, no abdominal fullness or lump. No past history of stone disease, no history of any abdominal surgery. Her bowel and bladder habit were normal. Patient was known case of Rheumatic heart disease with Severe MS status post Percutaneous Trans-Septal Mitral commissurotomy (PTMC) done 12 years ago. Patient was lost to follow up for last 3 years. No significant family history. She was not taking any medications for last 3 years.
On examination, her pulse was 62/min, irregularly irregular, Blood pressure was 86/59 mmHg with normal saturation at room air. Abdominal examination showed tenderness on right flank region and cardiac examination showed normal heart sounds with diastolic murmur. Laboratory investigations showed normal total leukocyte count, platelet count and hemoglobin level was 12gm/dl. Her renal function test was normal and Ultrasonography of abdomen showed fatty liver with normal both kidneys and empty urinary bladder. Contrast Enhanced Computed Tomography of abdomen showed abrupt cutoff of posterior division of right main renal artery with approximately 9.7 × 3.8 cm sized well-defined hypo-dense area in posterior aspect of right kidney involving all poles suggestive of thrombo-embolism of right posterior renal artery (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Axial section of Contrast Enhanced Computed Tomography (CECT) showing well-defined hypo dense area in posterior aspect of right kidney.
Fig. 2.
Coronal CECT abdomen and pelvis image showing infract of posterior aspect of right kidney (shown by arrow).
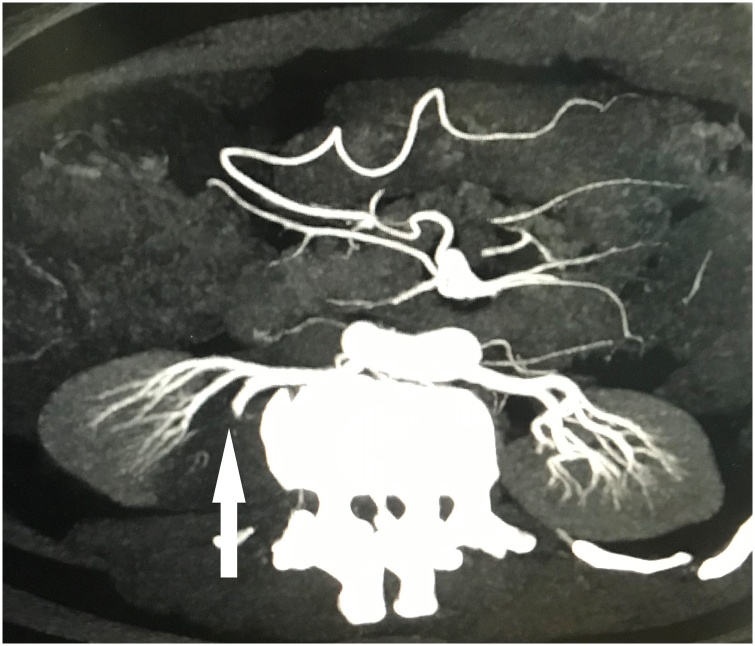
Fig. 3.
Renal arterial reconstruction image showing abrupt cut-off of right posterior renal artery (shown by arrow).
Acute right renal posterior segmental artery embolism was diagnosed and cardiac consultation was done. In view of late presentation, conservative management was planned against the active vascular intervention. Patient was admitted and started on intravenous heparin and overlapped with warfarin. Echocardiography showed features suggestive of Rheumatic heart disease with severe mitral stenosis with moderate mitral regurgitation with dilated left atrium with no mass or vegetation in left atrium. Her final diagnosis was Atrial Fibrillation with Rheumatic Heart disease with Right renal posterior segmental arterial thromboembolism. She was managed conservatively. Her serum creatinine rose during initial admission days which subsequently was normal and was discharged on warfarin, metoprolol and verapamil. Her INR was 2.5 on discharge. Seven days later she again presented to Emergency Room with right lower limb pain and numbness of 4 h duration. On examination Right lower limb was cold compared to left limb, sensations were lost below knee, and right dorsalis pedis, anterior tibial and posterior tibial artery pulsation were absent. Urgent arterial Doppler of right lower limb showed sluggish flow and echogenic content in distal aspect of popliteal artery, monophasic low velocity flow in anterior tibial artery and no flow in posterior tibial artery and dorsalis pedis artery. Her INR was 1.8. Fresh Frozen plasma was arranged and Urgent popliteal artery embolectomy was done and revascularization of limb was established. Patient had uneventful recovery and was continued with warfarin, metoprolol and verapamil. Her renal function test was within normal limits and she had no abdominal and limb pain.
3. Discussion
Acute renal artery embolism (RAE) is one of the uncommon cause of acute flank pain and risk factors of thromboembolism, is the clue to suspect such an uncommon pathology [1,2]. Hoxie and Coggin, were first to report about renal artery embolism in 1940 in postmortem study and some clinical subjects. Since then some case series have been published and different clinical presentations and treatment options have been described. Hazanov N. et al. in 2004 described their experience of eighteen years with forty-four cases of atrial fibrillation and renal infraction [7]. Risk factors include atrial fibrillation (most common), ischemic heart disease, mitral valve disease, aortic valve disease, cardiomyopathy, previous thromboembolism. Other non-cardiac sources of emboli are thrombi on unstable aortic plaques, valvular vegetations in infective endocarditis, and paradoxical emboli in the setting of a patent foramen ovale [[1], [2], [3]].
Clinical presentation of RAE is variable, and includes sudden onset severe abdominal, flank or back pain. Vomiting and fever is also present in half of patients. Signs of extra-renal embolism may also be present at times. Laboratory investigations may provide evidence of renal insufficiency, infraction and hematuria. Serum markers like C-reactive protein (CRP), Lactate dehydrogenase (LDH) are associated indirectly with renal infraction with variable specificity and sensitivity [7,8].
Imaging modality of choice for diagnosis of flank pain is unenhanced Computed Tomography scan. However, if renal artery embolism is suspected, Computed Tomography (CT) renal angiography or Magnetic Resonance(MR) angiography is widely used [7]. These imaging can identify renal parenchymal area of decrease or absent contrast enhancement. The standard management of RAE is urgent anticoagulation with or without thrombolysis. Patients are typically anticoagulated with intravenous heparin and oral warfarin. This measure prevents further embolic episodes. Thrombolysis can be done with medical or surgical measure. Surgical thrombus removal is associated with higher morbidity and mortality. Medical thrombolysis can be systemic or local intra-arterial. Local intra-arterial thrombolysis is associated with lesser systemic bleeding and is much favorable option. Thrombolysis is useful only if it is done within the ischemic time frame which kidney can withstand without permanent damage. There is no consensus regarding acceptable ischemia time [9], but ranges between 90–180 min, but useful dictum is the lesser the duration of ischemia, the better outcome [10,11]. Renal outcome of embolism is usually favorable if only segmental artery is involved and it is unilateral. Some may develop transient deranged kidney function test, but gradually it will improve [12]. However, only few patients who require dialysis, mortality is higher in them. Another important management aspect is treatment of the cause, and prevention of recurrent thromboembolism to various organs. Peripheral artery thrombo-embolism can be treated with endovascular or open surgical technique.
Recurrent episodes of thromboembolism are an uncommon clinical situation and are difficult to manage. High index of clinical suspicion and elaborate history and examination has a central role in diagnosing embolism.
4. Conclusion
Early identification and urgent treatment is key to the management of embolic episode in patient with atrial fibrillation. Long term prophylaxis can prevent further episodes.
Conflicts of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical approval taken from Institutional review committee.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Study concept or design- Purushottam Parajuli, Bhoj Raj Luitel, Suman Chapagain, Manish Man Pradhan, Sujeet Poudyal, Pawan Raj Chalise and Uttam Kumar Sharma.
Data collection- Purushottam Parajuli, Diwas Gnyawali, Prem Raj Sigdel, Durga Pandit, Bipin Guragain, Sampanna Chudal, Rupesh Verma.
Writing paper- Purushottam Parajuli, Bhoj Raj Luitel, Suman Chapagain, Manish Man Pradhan, Sujeet Poudyal, Pawan Raj Chalise and Uttam Kumar Sharma.
Registration of research studies
N/A.
Guarantor
Dr Purushottam Parajuli.
References
- 1.Mesiano P., Rollino C., Beltrame G., Ferro M., Quattrocchio G., Fenoglio R., Pozzato M., Cecere P., Forneris G., Bazzan M., Macchia G., Roccatello D. Acute renal infarction: a single center experience. J. Nephrol. 2017;30(February (1)):103–107. doi: 10.1007/s40620-015-0259-0. Epub 2016 Jan 7. PMID: 26743079. [DOI] [PubMed] [Google Scholar]
- 2.Bourgault M., Grimbert P., Verret C., Pourrat J., Herody M., Halimi J.M., Karras A., Amoura Z., Jourde-Chiche N., Izzedine H., François H., Boffa J.J., Hummel A., Bernadet-Monrozies P., Fouque D., Canouï-Poitrine F., Lang P., Daugas E., Audard V. Acute renal infarction: a case series. Clin. J. Am. Soc. Nephrol. 2013;8(March (3)):392–398. doi: 10.2215/CJN.05570612. Epub 2012 Nov 30. PMID: 23204242; PMCID: PMC3586969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oh Y.K., Yang C.W., Kim Y.L., Kang S.W., Park C.W., Kim Y.S., Lee E.Y., Han B.G., Lee S.H., Kim S.H., Lee S.H., Lim C.S. Clinical characteristics and outcomes of renal infarction. Am. J. Kidney Dis. 2016;67(February (2)):243–250. doi: 10.1053/j.ajkd.2015.09.019. Epub 2015 Nov 4. PMID: 26545635. [DOI] [PubMed] [Google Scholar]
- 4.Frost L., Engholm G., Johnsen S., Møller H., Henneberg E.W., Husted S. Incident thromboembolism in the aorta and the renal, mesenteric, pelvic, and extremity arteries after discharge from the hospital with a diagnosis of atrial fibrillation. Arch. Intern. Med. 2001;161(January (2)):272–276. doi: 10.1001/archinte.161.2.272. PMID: 11176743. [DOI] [PubMed] [Google Scholar]
- 5.Law Y., Chan Yc, Cheng Sw. Aspiration thrombectomy of acute atrial fibrillation-related renal artery thromboembolism in a patient with horseshoe kidney. Ann. Vasc. Surg. 2016;36(October):289.e5–289.e10. doi: 10.1016/j.avsg.2016.02.030. Epub 2016 Jun 25. PMID: 27354320. [DOI] [PubMed] [Google Scholar]
- 6.Yousif A., Samannan R., Abu-Fadel M. Unilateral acute renal artery embolism: an index case of successful mechanical aspiration thrombectomy with use of penumbra indigo aspiration system and a review of the literature. Vasc. Endovascular Surg. 2018;52(July (5)):391–394. doi: 10.1177/1538574418764052. Epub 2018 Mar 19. PMID: 29554859. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Hazanov N., Somin M., Attali M., Beilinson N., Thaler M., Mouallem M., Moar Y., Zaks N., Malnick S. Acute renal embolism. Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine. 2004;83:292–299. doi: 10.1097/01.md.0000141097.08000.99. [DOI] [PubMed] [Google Scholar]
- 9.Bolderman R., Oyen R., Verrijcken A., Knockaert D., Vanderschueren S. Idiopathic renal infarction. Am. J. Med. 2006;119(April (4)) doi: 10.1016/j.amjmed.2005.06.049. 356.e9-12, PMID: 16564787. [DOI] [PubMed] [Google Scholar]
- 10.Koivuviita N., Tertti R., Heiro M., Manner I., Metsärinne K. Thromboembolism as a cause of renal artery occlusion and acute kidney injury: the recovery of kidney function after two weeks. Case Rep. Nephrol. Urol. 2014;4(April (1)):82–87. doi: 10.1159/000362538. PMID: 24847350; PMCID: PMC4025054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gluck G., Croitoru M., Deleanu D., Platon P. Local thrombolytic treatment for renal arterial embolism. Eur. Urol. 2000;38:339–343. doi: 10.1159/000020303. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg D., Menes T., Rimon U., Salomon O., Halak M. Acute renal artery occlusion: presentation, treatment, and outcome. J. Vasc. Surg. 2016;64(October (4)):1026–1032. doi: 10.1016/j.jvs.2016.04.043. Epub 2016 Jun 23. PMID: 27345378. [DOI] [PubMed] [Google Scholar]