Abstract
Uterine arteriovenous malformation (AVM) is a rare condition that may lead to a life-threatening state. The urgency of diagnosis and treatment for uterine AVM should be emphasized. This case report describes a 42-year-old woman with a vaginal hemorrhage. In the previous month, the patient also had a hemorrhage after induced abortion that required a bilateral artery suture hemostasis of the uterus. On ultrasound, there was a lesion suspected by acquired AVM. Magnetic Resonance Angiography and Digital Subtraction Angiography was indicated to confirm the diagnosis. The patient was successfully treated by uterine artery embolization. After 6 months, the re-examined result showed no lesion of AVM.
Keywords: Arteriovenous malformation, Uterine artery embolization, Vaginal bleeding, Ultrasound, Uterus, Uterine artery
Background
Uterine arteriovenous malformation (AVM) is a rare condition with less than 150 reported cases, which may lead to a life-threatening state by causing vaginal hemorrhage [1]. The uterine AVM is congenital or acquired but in most cases, they are acquired [2]. The color Doppler ultrasound is popularly used in diagnosing uterine AVM as the first-hand test while digital subtraction angiography is the golden standard. At Tu Du hospital, one of the leading centers in Gynecology & Obstetrics in Vietnam, we have recorded a few cases of uterine AVM, however, the diagnosing and treatment of this condition is still complicated for physicians. The right way in approaching patients with uterine AVM is necessary to avoid deadly complications such as severe hemorrhage. By this case report, we expect to contribute our experience to the knowledge of uterine AVM.
Case report
A 42-year-old patient, G4 P 1-0-2-1, visited our faculty to abort a 15-week and 2-day fetus with birth defects. The patient underwent hemorrhage after the induced abortion. She was treated with emergency bilateral artery suture hemostasis of the uterus. During the surgery, the volume of blood loss was approximately 1500 mL, and 6 units of blood were transfused. One month later, the patient presented abnormal vaginal bleeding. The ultrasound showed some irregular features: myometrial heterogeneous mixed echogenicity, multiple dilated tubular structures spreading throughout the uterine muscle, thin and intact endometrium, and no image of abnormal mass. The color Doppler showed many areas of increased vascularity, dilated blood vessels, aliasing, and indistinction of arteries and veins. The diagnosis by ultrasound is the uterine AVM. Magnetic resonance angiography and digital subtraction angiography were indicated to confirm the diagnosis before treatment by artery embolization. MRA showed an abnormal tangle of blood vessels with early contrast enhancement. DSA showed an abnormal blood vessel tangle with early contrast enhancement, which is a typical lesion feature of uterine AVM. Microcatheter was inserted into the uterine artery branch then embolized with 2 coils: 7 mm and 5 mm, another microcatheter was inserted into 2 diseased artery branches of the inner pelvic artery and then embolized with a 1.5 mm coil, glue (1 tube of 0.5 mL glue, 1 mL lipiodol), and gel foam. After the procedure, the size of the blood tangle declined approximately 70% and blood flow returned slowly. During and after treatment, there had been no serious complications. After the treatment by uterine artery embolization, the symptoms and features of uterine AVM had decreased and completely disappeared 6 months later.
Discussion
The uterine AVM was first described by Dubreuil and Loubat in 1926 [3], featured by the increased vascularity with a direct arteriovenous fistula, bypassing the capillaries. There are 2 types of uterine AVM: congenital or acquired. The congenital uterine AVM is known as a result of abnormal embryonic blood vessel development that leads to the abnormality in the differentiation of capillaries and the connection of arteries and veins [4]. The arteriovenous fistula in congenital uterine AVM may include many arteries and veins that can encroach on surrounding structures [5]. The acquired uterine AVM is the most commonly reported type. Patients with acquired uterine AVM usually have the anamnesis of abortion, cesarean, or pelvic surgery. The typical abnormality in acquired uterine AVM is the connection between one artery and one vein, which is different from congenital uterine AVM. The acquired uterine AVM may relate to infection, retained products of conception, gestational trophoblastic disease, gynecological malignancies and exposure to diethylstilboestrol [6].
Clinical features
The most common symptom of uterine AVM is vaginal bleeding from mild to severe grade. It usually occurs in women who are of reproductive age, postpartum, or have had uterine intervention [7]. The congenital or acquired uterine AVM may have the same features on imaging results. The medical history is important to distinguish these 2 types of lesions. The severe hemorrhage often occurs in congenital uterine AVM and does not respond to normal treatment while patients with acquired uterine AVM often have had surgical interventions. The symptoms may appear gradually or suddenly. The mechanism of hemorrhage in uterine AVM can be the rupture of the endothelium of blood vessels during abortions or menstruation (2).
Imaging features of uterine AVM
The 2D gray-scale ultrasound showed the non-specific images [1,8]: Thick uterine muscle, mixed echogenic areas with the multiple tubular or "spongy" anechoic or hypoechoic areas within the myometrium, and mixed echogenic mass in the uterus that may be mistaken with retained products of conception.
The Doppler ultrasound showed an increased vascularity area in the uterine muscle with aliasing of a high-velocity flow [1,2].
In uterine AVM, the pulse wave Doppler ultrasound demonstrates the high velocity flows with low impedance. Following recent studies, the average velocity of flows in uterine AVM is 136 cm/s with an average RI = 0.3 [2]).
MRA is a non-invasive and valuable technique that results in good compatibility with the DSA (gold standard) in diagnosing and treating uterine AVM. The characteristic appearances of uterine AVM on spin-echo sequences of MRI are multiple serpiginous flow-related signal voids within the lesion, enlarged uterus, mass with indistinct margins, localized or diffusive ill-defined transition zone [2,9].
DSA is the gold standard in diagnosing AVM and also an interventional treatment technique. For this reason, the indication of DSA required the patient's consent. The defining feature of uterine AVMs on DSA is brisk early filling of numerous enlarged veins emerging from a nidus or nest of abnormal vessels after arterial contrast injection [1,2].
Planning and treatment for patients with AVM
There are 5 main factors [2] that needed to be considered in planning and treatment for patients with AVM including hemodynamic state, size and location of the lesions, degree of bleeding, age, and the desire for future fertility.
Depending on each patient's status and desires, there are different treatment options such as hormone therapy, uterine artery embolization, or even hysterectomy [2].
Conclusion
The uterine AVM is a rare condition that may lead to a life-threatening state by causing severe hemorrhage. The recognizable features of uterine AVM are increased vascularity, squiggly and dilated blood vessels. These blood vessels are usually localized in uterine muscles. To detect uterine AVM lesions, the radiologists need to combine patients’ anamnesis and the result of ultrasound imaging. The other imaging diagnostic tools (MRA, DSA) can be used to confirm the diagnosis to build a suitable treatment plan for patients. The ultrasound is easy to use and accurate, which becomes the first-hand test in diagnosing uterine AVM. The MRA is a non-invasive technique that results in good compatibility with the DSA (gold standard) in diagnosing and treating uterine AVM. Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6
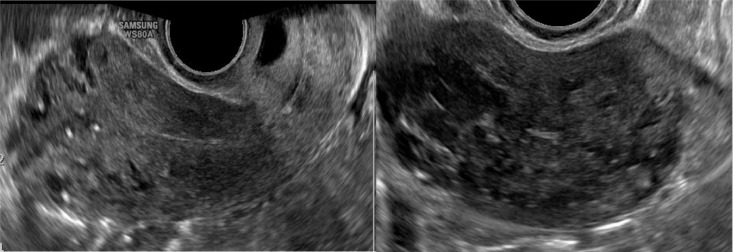
Fig. 1.
The 2D transvaginal ultrasound. On the sagittal and transverse plane, myometrial heterogeneous mixed echogenicity, thin endometrium, and no image of mass in the uterine cavity is shown.
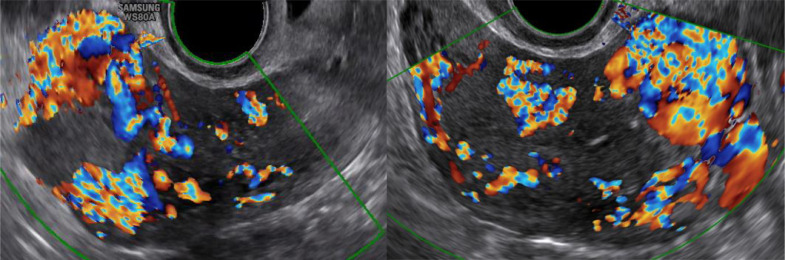
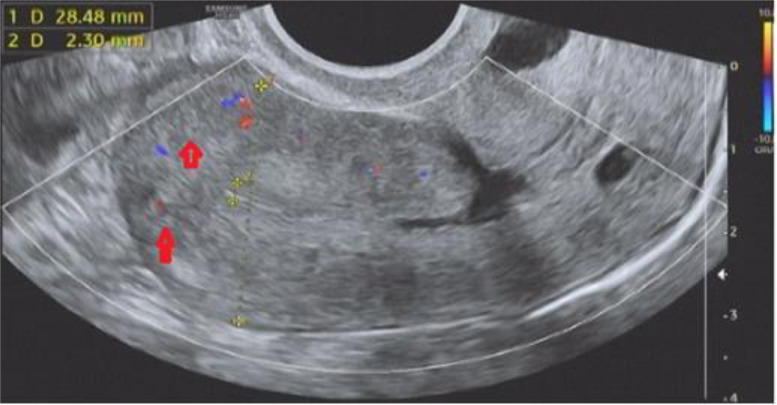
Fig. 2.
The color Doppler transvaginal ultrasound. On the sagittal and transverse plane, the increased vascularity on the entire uterine muscle, squiggly and dilated blood vessels with aliasing are seen.
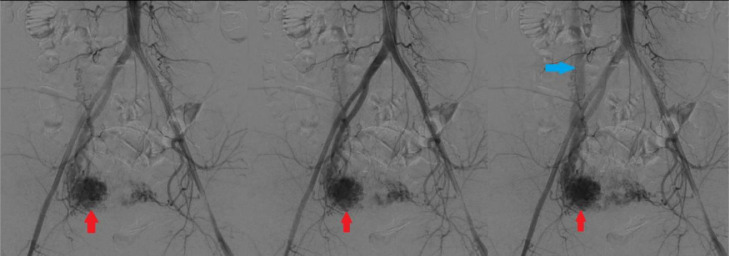
Fig. 3.
The MRA volume rendering technique demonstrated that the squiggly and dilated tangle of blood vessels appeared early (red arrows) with an early draining vein (blue arrow).
Fig. 4.
On DSA, the squiggly and dilated tangle of blood vessels appeared early (red arrows) with an early draining vein (blue arrow).
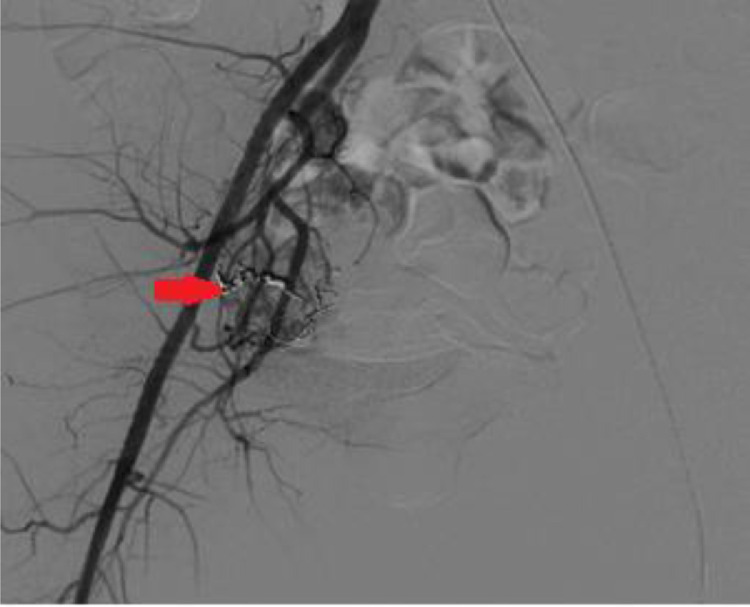
Fig. 5.
The post-embolization image shows the coil in the blood vessel (red arrow) with the decreasing of squiggly blood vessels and no early draining vein.
Fig. 6.
Ultrasound after 6 months of uterine artery embolization. The increased vascularity areas are almost disappeared. Remaining hyperechoic areas (Arrowheads).
References
- 1.Divya Sridhar, Robert L V. Diagnosis and treatment of uterine and pelvic arteriovenous malformations. 2018
- 2.Thangam ma Kati Mada Annaiah SKS. Uterine arteriovenous malformations: clinical implications. 2015.
- 3.Fleming H, Ostor A, Pickel H FD. Arteriovenous malformations of the uterus. Obs Gynaecol. 1989;73(2):209–213. [PubMed] [Google Scholar]
- 4.Polat P, Suma S, Kantarcy M, Alper F LA. Colour Doppler ultrasound in the evaluation of uterine vascular abnormalities. Radiographics. 2002;22:47–53. doi: 10.1148/radiographics.22.1.g02ja0947. [DOI] [PubMed] [Google Scholar]
- 5.Grivell R, Reid K MA. Uterine arteriovenous malformations: a review of the current literature. Obs Gynecol Surv. 2005;60(11):761–767. doi: 10.1097/01.ogx.0000183684.67656.ba. [DOI] [PubMed] [Google Scholar]
- 6.Sellers Francisco. Ana Palacios-Marqués, Belen Moliner and RB. Case report. Uterine Arteriovenous Malformation. 2013 doi: 10.1136/bcr-2012-008443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aziz N, Lenzi TA, Jeffrey RB Jr LD. Postpartum uterine arteriovenous fistula. Obs Gynecol. 2004;103:8. doi: 10.1097/01.AOG.0000123241.44401.01. [DOI] [PubMed] [Google Scholar]
- 8.Hickey M FI. Clinical implications of disturbances of uterine vascular morphology and function. Baillieres Best Pr Res Clin Obs Gynaecol. 2000;14:51. doi: 10.1053/beog.2000.0136. [DOI] [PubMed] [Google Scholar]
- 9.Sridhar D, Fleming H, Polat P, Grivell R, Sellers F, Aziz N. Arteriovenous malformations of the uterus. Acta Radiol. 2009;50:9. [Google Scholar]